Abstract
Purpose
Prior studies have reported improved gait performance and kinematics after total ankle arthroplasty (TAR) compared to ankle arthrodesis (AAD). Given these findings, AAD has been primarily considered as a salvage procedure that may lead to adjacent joint degeneration.
Methods
A total of 101 TAR and 40 screw arthrodeses were enrolled in a retrospective study with a prospectively designed follow-up examination that included gait analysis and outcome assessment with the AOFAS hindfoot score and FAOS questionnaire.
Results
Significant asymmetry in gait and reduced range of motion compared to normal remained after both procedures. Subjective outcome improved after both procedures, and pain was significantly better after TAR. Limited functional gains after TAR and joint degeneration to the same degree after both procedures was seen in the mid-term. Hindfoot fusion seemed to have a greater impact on postoperative function than ankle arthrodesis.
Conclusion
Considering only minor functional gains of TAR compared to AAD the implantation of current TAR designs in large patient series may be questioned.
Keywords: Total ankle arthroplasty, Ankle arthrodesis, Comparative analysis, Gait analysis, Clinical outcome
Introduction
Ankle arthrodesis (AAD) for treatment of ankle osteoarthritis was reported to relieve pain and improve function, but was still considered a salvage procedure that caused alterations in gait [1], a significant decrease of the sagittal plane motion of the hindfoot [2] and a shift of the ground reaction force [3]. Furthermore, premature deterioration of other foot joints with substantial arthritic changes was found in the foot as a long-term result [4]. On the other hand, significant improvements including subjective outcome, more normal ankle function, gait kinematics and gait kinetics were observed following total ankle replacement (TAR) [5, 6]. In cadaveric studies it was suggested that modern prosthetic designs are even able to achieve close to normal kinematics [7]. Since kinematic models vary, direct comparison of functional results and their impact on clinical outcome is necessary to identify potential advantages of one method over another. A few studies have directly compared the effects of TAR against AAD, showing improvement after both procedures and a more natural ankle joint function after TAR [8–11]. Those studies however have only limited numbers of patients and short observation periods. Therefore, the aim of the present study was to compare radiological, subjective, and functional outcomes of a larger consecutive patient series after TAR and AAD. It was hypothesized that patients with TAR would show improved gait patterns compared to AAD patients after a longer observation period, theoretically related to protection of adjacent hindfoot joints from premature degeneration due to improved ankle range-of-motion in TAR.
Patients and methods
All consecutive patients that had undergone AAD or TAR between January 2000 and December 2012 entered into the study. The Hintegra® TAR (Newdeal, Lyon, France) was used in all cases. Investigations included a radiographic analysis of the adjacent joints with regard to osteoarthritis progression, a standardised clinical investigation, assessment of subjective outcome with the AOFAS (American Orthopaedic Foot and Ankle Society), FAOS (Foot and Ankle Outcome Score) and VAS (visual analogue scale), an instrumented gait analysis and a detailed retrospective analysis of medical records. The local ethical board approved the project and all participating patients provided informed consent prior to participation.
Patients
One-hundred-one TAR and 40 AAD patients were identified. Patients were excluded if they had diagnoses other than primary or posttraumatic osteoarthritis, fixation other than screw arthrodeses, a follow-up (FU) period of less than six months and revision surgery following the definition of Henricson et al. [12]. Hence, gait analysis was performed in 52 patients after TAR and in ten patients after AAD, with 14 of the 52 TAR patients also receiving an arthrodesis of the hindfoot (HFA). None of the ten patients receiving gait analysis after AAD had an additional hindfoot fusion. An additional 16 patients (62 total after TAR, 16 total after AAD) took part in the clinical investigation including the questionnaires. It was assumed that an arthrodesis of one or more of the three hindfoot joints (TN talo-navicular, CC calcaneo-cuboideal, ST subtalar joint) would lead to a blockade of the hindfoot movement, therefore these patients were analysed as a consistent group. Subsequently three groups of patients were analysed: (1) TAR without hindfoot arthrodesis (TAR-alone), (2) TAR with arthrodesis of one or more hindfoot joints (TAR-HFA) and (3) patients with AAD.
Gait analysis
Sixteen retro-reflective spherical surface markers were placed according to conventional gait model description [13]. Patients walked a 9.5-metre walkway at their self selected walking speed. Marker trajectories were recorded using a six camera Vicon V460 system at 120Hz (Vicon, Oxford, UK). Anterio-posterior, medio-lateral and vertical ground reaction forces (GRF) were recorded with a biomechanical force platform (AMTI OR6-7-1000, Watertown, MA) embedded in the walkway. Data were collected and analysed using the Vicon workstation V4.6 and polygon, multimedia reporting software including the plug-in gait model (version V3.1). Temporal-spatial measurements included gait velocity, cadence, stride length, step length for operative and non-operative side, double support as a percentage of the gait cycle and limp index (total support time (single + double) for ipsilateral foot divided by the total support time for the contralateral foot; equal to unity for a symmetric gait). Joint kinematics were measured ten times per patient and included sagittal plane range of motion of hip, knee and ankle joint and frontal plane measurement of pelvic obliquity, frontal hip and knee angle. Kinetic parameters were calculated for sagittal hip, knee and ankle moments as well as frontal hip, knee and ankle moments.
Clinical examination and questionnaires
A standardised clinical exam including range of motion (RoM) measurement was performed by use of a goniometer aligned to the longitudinal axis of the shank and the plantar pedis of the hindfoot. The examining surgeon also analysed the patient according to the AOFAS hindfoot scale. Self-reported assessment of symptoms, stiffness, pain, function, activities of daily living, quality of life, sports and recreational activities were recorded with the FAOS by the patients alone. Pain was quantified with the VAS scale. Additionally, pre-operative status was retrieved with use of the FAOS and VAS.
Radiological analysis
Standard AP and lateral X-rays of the ankle joint and foot were taken in a standing position pre-operatively and at each routine follow-up examination including the recent examination. All patients with a minimum radiological follow-up of six months were included. Twenty-three of the remaining patients from the TAR group and six patients from the AAD group had a hindfoot fusion before or at the time of the index operation. Hence, a total series of 55 TAR patients and 22 AAD patients were enrolled in the radiological analysis of degenerative changes of the adjacent joints (CC, TN, ST). They were graded for both groups according to the fives scales of the Kellgren and Lawrence radiographic criteria for assessment of osteoarthritis [14] pre-operatively and at last follow-up.
Statistics
Due to the small sample sizes and skewed distribution non-parametric tests were chosen for analyses. Statistical analysis was performed with the SPSS 20.0 statistical software package (IBM Corporation, Armond, NY, USA). Quantitative, normally distributed variables are described as mean and standard deviation. In cases with two independent samples the Mann–Whitney U-test was chosen. For dependent samples the Wilcoxon test for paired samples was used. Chi-square tests were used to check two nominal variables for independence. For correlations either Pearson or Spearman correlation coefficients were used, depending on whether the variables involved were normally distributed or not. In cases where more than two independent groups were compared, the Kruskal-Wallis H-test was used. We chose a significance level of 0.05.
Results
Gait analysis
Temporal-spatial analysis (Table 1) did not show significant differences in cadence, stride length or walking velocity between AAD and both TAR groups, indicating all three procedures had the same overall effect on gait performance. The limp index was significantly smaller on the operated side compared to the non-operated side for all groups, suggesting a shorter stance time on the operated side using each procedure. Single support time was longer for the non-operated side in all groups, but less asymmetric after both TAR procedures. Step length was significantly longer for the operated side after TAR-alone, but not for TAR-HFA or AAD patients. While all groups showed temporal-spatial asymmetry, the asymmetry was greater in arthrodesis patients.
Table1.
Temporal-spatial results
| Measure | TAR-alone op | TAR-alone nop | p-value (Wilcoxon) | TAR-HFA op | TAR-HFA nop | p-value (Wilcoxon) | AAD op | AAD nop | p-value (Wilcoxon) | TAR-alone op vs TAR-HFA op vs AAD opp-value (Kruskal-Wallis) |
|---|---|---|---|---|---|---|---|---|---|---|
| Cadence (steps/min) | 106.6 (±10.9) | - | 109.8 (±12.7) | - | 107.6 (±13.2) | - | 0.64 | |||
| Single support (sec) | 0.43 (±0.04) | 0.45 (±0.04) | 0.002 | 0.41 (±0.03) | 0.43 (±0.04) | 0.1 | 0.39 (±0.05) | 0.46 (±0.07) | 0.01 | 0.08 |
| Double support (sec) | 0.26 (±0.09) | 0.26 (±0.1) | 0.54 | 0.27 (±0.09) | 0.26 (±0.09) | 0.41 | 0.28 (±0.14) | 0.28 (±0.14) | 0.26 | 0.96 |
| Limp index (sec/sec) | 0.98 (±0.04) | 1.03 (±0.05) | 0.002 | 0.98 (±0.04) | 1.03 (±0.03) | 0.03 | 0.92 (±0.07) | 1.09 (±0.09) | 0.01 | 0.09 |
| Step length (m) | 0.52 (±0.11) | 0.5 (±0.11) | 0.003 | 0.51 (±0.1) | 0.45 (±0.09) | 0.33 | 0.53 (±0.12) | 0.47 (±0.16) | 0.26 | 0.76 |
| Stride length (m) | 1.03 (±0.21) | - | 1.01 (±0.18) | - | 1.01 (±0.26) | - | 0.87 | |||
| Walking speed (m/s) | 0.92 (±0.23) | - | 0.93 (±0.22) | - | 0.91 (±0.26) | - | 0.96 | |||
Values are given as mean ± SD. TAR-alone op = patients after total ankle replacement alone at the operated side; TAR-alone nop = patients after TAR alone at the non-operated side; TAR-HFA op = patients after total ankle replacement and hind-foot arthrodesis at the operated side; TAR-HFA nop = patients after TAR and hind-foot arthrodesis at the non-operated side; AAD op = patients after ankle arthrodesis at the operated side; AAD nop = patients after ankle arthrodesis at the non-operated side
Kinematic analysis (Table 2) showed a significant difference between the three procedures on the operated side in total ankle RoM, minimum knee flexion angle, knee flexion at initial contact, and minimum knee extension moment in stance. Sagittal ankle RoM was significantly reduced on the operated side after all procedures, but to the highest amount after AAD. AAD also led to significantly less knee flexion throughout stance period on the operated side, specifically at initial contact, toe off and at the point of minimum knee flexion in stance. For AAD there was also a significantly greater knee RoM during the gait cycle, and a significantly lower maximum ankle dorsiflexion in stance on the operative side compared to the non-operated side. Significant differences in these same kinematic variables were not seen in either TAR group, except that there was significantly lower maximum dorsiflexion in stance in the TAR alone group on the operative side. For the kinetic variables the TAR-alone group showed a slightly reduced knee extension moment minimum on the operative side compared to the non-operative side and a reduced maximum ankle plantar-flexor moment.
Table 2.
Kinematic and kinetic results
| Measure | TAR-alone op | TAR-alone nop | p-value (Wilcoxon) | TAR-HFA op | TAR-HFA nop | p-value (Wilcoxon) | AAD op | AAD nop | p-value (Wilcoxon) | TAR-alone op vs TAR-HFA op vs AAD opp-value (Kruskal-Wallis) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Kinematics (degrees) | Max knee flex stance | 19.7 (±6.8) | 20.1 (±6.8) | 0.75 | 20.3 (±3.9) | 19.6 (±5.5) | 0.65 | 14.7 (±6.5) | 20.9 (±5.1) | 0.04 | 0.09 |
| Max knee flex swing | 56.8 (±8.4) | 56.4 (±8.4) | 0.54 | 57.9 (±7.7) | 55.7 (±8.8) | 0.35 | 57.1 (±8.2) | 58.8 (±7.3) | 0.39 | 0.77 | |
| Min knee flex | 6.0 (±5.5) | 6.8 (±5.3) | 0.53 | 4.2 (±3.7) | 4.2 (±4.8) | 0.97 | −0.9 (±6.5) | 8.0 (±2.3) | 0.01 | 0.008 | |
| Knee flex toe off | 33.5 (±5.5) | 33.4 (±7.1) | 0.86 | 32.5 (±4.6) | 34.2 (±6.8) | 0.42 | 29.1 (±7.4) | 37.7 (±4.2) | 0.007 | 0.24 | |
| Knee flex initial contact | 11.7 (±4.6) | 10.8 (±6.1) | 0.2 | 11.3 (±5.8) | 8.7 (±5.1) | 0.15 | 7.8 (±2.9) | 13.6 (±4.2) | 0.02 | 0.04 | |
| Total knee RoM | 50.9 (±10.6) | 49.6 (±9.1) | 0.21 | 53.8 (±10.0) | 51.4 (±8.2) | 0.15 | 58.0 (±8.6) | 50.8 (±7.8) | 0.03 | 0.15 | |
| Max ankle dorsiflexion in stance | 10.4 (±5.3) | 13.1 (±3.8) | 0.005 | 12.3 (±4.1) | 13.6 (±2.6) | 0.12 | 5.5 (±8.3) | 14.9 (±4.8) | 0.005 | 0.09 | |
| Max ankle plantar-flexion in stance | 6.1 (±7.0) | 9.7 (±7.7) | 0.003 | 3.2 (±5.8) | 7.2 (±4.3) | 0.01 | 6.0 (±8.0) | 4.6 (±8.8) | 0.65 | 0.44 | |
| Total ankle RoM | 17.3 (±4.3) | 23.1 (±6.3) | <0.001 | 16.9 (±4.4) | 22.2 (±4.0) | 0.006 | 11.6 (±3.2) | 20.4 (±4.5) | 0.005 | 0.002 | |
| Moments (Nm/kg) | Max gait cycle knee | 0.24 (±0.16) | 0.34 (±0.28) | 0.2 | 0.3 (±0.17) | 0.29 (±0.15) | 0.72 | 0.17 (±0.07) | 0.32 (±0.14) | 0.03 | 0.28 |
| Min stance knee | −0.3 (±0.12) | −0.3 (±0.21) | 0.35 | −0.32 (±0.14) | −0.34 (±0.07) | 0.91 | −0.5 (±0.21) | −0.31 (±0.1) | 0.01 | 0.03 | |
| Min swing knee | −0.19 (±0.07) | −0.21 (±0.11) | 0.01 | −0.2 (±0.07) | −0.19 (±0.05) | 1.0 | −0.21 (±0.06) | −0.27 (±0.5) | 0.07 | 0.92 | |
| Max ankle plantar-flexor moment | 1.26 (±0.23) | 1.4 (±0.31) | 0.001 | 1.13 (±0.31) | 1.28 (±0.27) | 0.15 | 1.26 (±0.16) | 1.47 (±0.45) | 0.26 | 0.24 | |
Values are given as mean ± SD. TAR-alone op = patients after total ankle replacement alone at the operated side; TAR-alone nop = patients after TAR alone at the non-operated side; TAR-HFA op = patients after total ankle replacement and hind-foot arthrodesis at the operated side; TAR-HFA nop = patients after TAR and hind-foot arthrodesis at the non-operated side; AAD op = patients after ankle arthrodesis at the operated side; AAD nop = patients after ankle arthrodesis at the non-operated side
Clinical examination and questionnaires
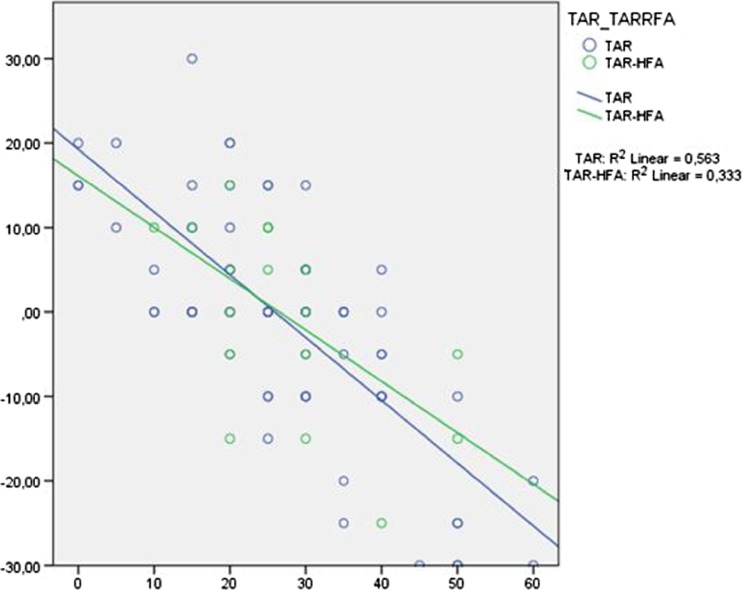
Mean clinical ankle RoM did not differ significantly pre-operatively between TAR-alone, TAR-HFA and AAD patients (27.5 vs. 26.9 vs. 25.6 degrees, p = 0.87). Mean postoperative RoM was significantly worse for TAR-HFA compared to TAR-alone (19.4° vs. 27.3, p = 0.03) but did not differ from the pre-operative status in the TAR-alone group. There was however a significant linear correlation between pre-operative RoM and the difference to the postoperative status for both TAR groups, illustrating that patients with a higher pre-operative joint mobility lost motion whereas patients with lower pre-operative RoM gained motion (Fig. 1).
Fig. 1.
Linear correlation between pre-operative RoM and the difference to the postoperative status
Mean global AOFAS outcome score did not differ between the three groups postoperatively. The TAR-alone group showed a significant better outcome with regard to the AOFAS-function subscore compared to the TAR-HFA and AAD groups. There were no significant statistical differences between the three groups for the subgroups pain and alignment. Assessment of pain with the VAS revealed significant improvement of pain without differences between the three groups pre- and postoperatively. Patients’ self reported symptoms, activity of daily living, sports and quality of life improved significantly after both interventions, again without significant differences between the three groups. Only self-reported pain assessed with the FAOS revealed significantly less pain pre-operatively for AAD patients and a significant better outcome after TAR (Table 3).
Table 3.
Results and p-values of the clinical evaluation with visual analogue scale (VAS), AOFAS hindfoot score and FAOS questionnaire (ADL = activities of daily living; QOL = quality of life). TAR-alone showed a significant better outcome in the AOFAS subscore function and AAD patients had significantly more pain at a mean of 4.4 years after the intervention than both groups of TAR patients
| Measure | VAS pre-OP | VAS post-OP | AOFAS pain | AOFAS function | AOFAS alignment | AOFAS global |
|---|---|---|---|---|---|---|
| TAR-alone | 8.4 (±1.3) | 3.3 (±2.4) | 25.6 (±12.4) | 36.4 (±10.6) | 8.8 (±2.6) | 70.9 (±23.4) |
| TAR-HFA | 7.9 (±1.8) | 3.1 (±2.3) | 27.2 (±9.6) | 30.6 (±10.0) | 9.7 (±1.6) | 67.5 (±17.1) |
| AAD | 8.1 (±1.3) | 2.6 (±2.2) | 30.9 (±7.0) | 29.6 (±8.7) | 7.8 (±3.8) | 68.3 (±15.5) |
| p-value (Kruskal-Wallis) |
0.67 | 0.61 | 0.48 | 0.02 | 0.48 | 0.39 |
| pre-OP | FAOS pain | FAOS symptoms | FAOS ADL | FAOS sports | FAOS QOL | |
| TAR-alone | 29.5 (±15.7) | 34.2 (±21.5) | 37.5 (±20.6) | 17.4 (±16.0) | 13.6 (±10.2) | |
| TAR-HFA | 26.3 (±11.6) | 31.6 (±26.9) | 36.8 (±22.5) | 19.7 (±13.2) | 12.7 (±14.5) | |
| AAD | 39.4 (±17.4) | 32.3 (±17.6) | 36.9 (±21.7) | 20.8 (±15.2) | 17.9 (±14.5) | |
| p-value (Kruskal-Wallis) |
0.04 | 0.72 | 0.99 | 0.41 | 0.35 | |
| post-op | FAOS pain | FAOS symptoms | FAOS ADL | FAOS sports | FAOS QOL | |
| TAR-alone | 68.9 (±17.4) | 63.0 (±22.4) | 71.7 (±20.5) | 46.9 (±23.8) | 41.5 (±23.9) | |
| TAR-HFA | 71.8 (±22.2) | 63.4 (±22.4) | 70.0 (±24.4) | 42.8 (±24.5) | 43.9 (±28.6) | |
| AAD | 47.9 (±20.4) | 70.6 (±23.2) | 69.6 (±22.0) | 40.3 (±23.5) | 43.2 (±26.1) | |
| p-value (Kruskal-Wallis) | 0.001 | 0.48 | 0.94 | 0.53 | 0.94 | |
Radiological analysis
An increase of one or more scales in the adjacent joints around the ankle according to the Kellgren and Lawrence criteria [14] was seen in 80.7 % of TAR patients after a mean observation period of 4.2 (±2.03) years and 64.9 % of the AAD patients after 3.4 (±3.67) years. CC-degeneration was seen in 27.7 % after TAR and 17.1 % after AAD. TN-degeneration was seen in 49.9 % vs. 34.3 % of the patients and ST-degeneration was found in 53.1 % vs. 48.7 %, respectively. Those differences were not significant (Fisher’s exact test: for CC = 0.2, TN = 0.06, ST = 0.82). An increase of degeneration with time was clearly seen as well after TAR as after AAD.
Discussion
Patients in both the arthrodesis and arthroplasty groups reportedly improve in various parameters of gait when compared with their own pre-operative function [7, 8]. For joint replacement it was suggested that functional results may approximate those of healthy subjects [7], which seemed to be the most powerful arguments for the choice of an arthroplasty in comparison to an arthrodesis despite higher complication and reoperation rates [15, 16]. Nevertheless, comparative studies showed that neither group functioned as well as normal subjects [8, 9, 11, 17].
Although the design of modern TAR systems is meant to theoretically allow a normal RoM [7], no improvement of total postoperative RoM compared to pre-operative values was seen in our TAR-alone patients and also reported in other studies with mean values between 24 and 28 degrees, respectively [18, 19]. Hindfoot fusion led to a significantly worse clinically assessed RoM after TAR in our patient series. Excluding those patients, the Hintegra® implant showed a mean postoperative RoM of 27° which correlated significantly with symptoms, sports and pain. The motion of the normal ankle joint in the sagittal plane averages 70° of motion, but during the stance phase of the gait cycle RoM is said to be limited to 25° [20]. In our patient series mean ankle RoM as assessed with gait analysis was 17° after TAR and 12° for AAD patients. Similar ankle RoM was reported by Singer et al. who concluded that dorsal ankle motion in the sagittal plane was primarily responsible for better gait patterns after TAR [17]. This slight improvement in ankle RoM after TAR also appears associated with increased knee flexion in stance compared to AAD. Similar to an earlier study, sign of knee hyperextension at terminal stance was also seen in the AAD group in this study [20]. Compensatory motion at the subtalar and midtarsal joints contribute to the amount of ankle dorsiflexion obtained by goniometric measurements and gait analysis [21] and RoM even seems to increase with time after arthrodesis [22]. A compensatory increase of the combined subtalar and medial column motion of 11 % was reported with time after tibiotalar fusion, which also had a positive association of quality of life with increased compensatory motion of the hindfoot and midfoot [22]. In our study, the TAR-alone group showed a significant better outcome of the AOFAS-function subscore compared to the TAR-HFA and AAD groups. These results may indicate that a fusion of the hindfoot has a greater impact on function than fusion of the ankle joint.
Impact of ankle fusion on gait is hyperextension of the knee and increased stress on the adjacent hindfoot joints that might enhance osteoarthritic changes of those joints [20], which is one major argument for implantation of TAR. A clearly increased degeneration of the adjacent joints with time was seen in our patients after AAD but also after TAR in the medium-term without significant differences between the two groups. Deterioration of the arthritic changes in the subtalar joint was already previously reported in 15 % of patients five years after TAR [23]. At a mean follow up of nine years after arthrodesis, progressive osteoarthritis of the contiguous joints was also appreciated in other studies, however rarely becoming symptomatic in these patients [24]. It has not yet been shown that long-term results after ankle replacement are superior with regard to adjacent joint degeneration, which might also be seen as a long-term complication after joint replacement.
This is to our knowledge the largest study comparing functional and radiological results after TAR and AAD in the literature. It is furthermore the first study analysing the effect of hindfoot fusion on gait of patients with TAR. There are however several weaknesses of this study. Pre-operative gait analysis data are missing and it is unclear whether baseline measurements were comparable between the two groups. The treatment groups were not randomised and the minimal differences between the two treatment groups may therefore be underestimated. Pre-operative FAOS was obtained after elective surgery, which was believed to be a poor predictor of the patient’s pre-operative condition and to overestimate the benefit of surgery. This however is the case for both procedures and has no impact on the main messages of the present study, namely, the remaining implications on gait after both procedures and challenging the rationale of the implantation of present ankle designs such as prevention of osteoarthritis of the adjacent hindfoot joints.
Taking into account the comparably high revision rates of approximately 10 % at five years [25] and the limited functional gains after TAR as highlighted in our study, further use of those implants in large patient series should be reconsidered. Further studies are needed comparing functional results and osteoarthritic changes of the adjacent joints after TAR and AAD in the long term. As a consequence of this study, the rate of ankle replacements versus arthrodeses dropped significantly at our institution, especially in the younger patients.
Acknowledgments
Conflict of interest
None.
References
- 1.Fuentes-Sanz A, Moya-Angeler J, Lopez-Oliva F, Forriol F. Clinical outcome and gait analysis of ankle arthrodesis. Foot Ankle Int. 2012;33:819–827. doi: 10.3113/FAI.2012.0819. [DOI] [PubMed] [Google Scholar]
- 2.Wu WL, Su FC, Cheng YM, Huang PJ, Chou YL, Chou CK. Gait analysis after ankle arthrodesis. Gait Posture. 2000;11:54–61. doi: 10.1016/S0966-6362(99)00049-1. [DOI] [PubMed] [Google Scholar]
- 3.Beyaert C, Sirveaux F, Paysant J, Molé D, André JM. The effect of tibio-talar arthrodesis on foot kinematics and ground reaction force progression during walking. Gait Posture. 2004;20:84–91. doi: 10.1016/j.gaitpost.2003.07.006. [DOI] [PubMed] [Google Scholar]
- 4.Coester LM, Saltzman CL, Leupold CL, Pontarbelli W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg. 2001;83-A:219–228. doi: 10.2106/00004623-200102000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Brodsky JW, Polo FE, Coleman SC, Bruck N. Changes in gait following the Scandinavian total ankle replacement. J Bone Joint Surg. 2011;93-A:1890–1896. doi: 10.2106/JBJS.J.00347. [DOI] [PubMed] [Google Scholar]
- 6.Noelle S, Egidy CC, Cross MB, Gebauer M, Klauser W. Complication rates after total ankle arthroplasty in one hundred consecutive prostheses. Int Orthop. 2013;37:1789–1794. doi: 10.1007/s00264-013-1971-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Valderrabano V, Nigg BM, von Tscharner V, Stefanyshyn DJ, Goepfert B, Hintermann B. Gait analysis in ankle osteoarthritis and total ankle replacement. Clin Biomech. 2007;22:894–904. doi: 10.1016/j.clinbiomech.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 8.Piriou P, Culpan P, Mullins M, Cardon JN, Pozzi D, Judet T. Ankle replacement versus arthrodesis: A comparative gait analysis study. Foot Ankle Int. 2008;29:3–9. doi: 10.3113/FAI.2008.0003. [DOI] [PubMed] [Google Scholar]
- 9.Hahn ME, Wright ES, Segal AD, Orendurff MS, Ledoux WR, Sangeorzan BJ. Comparative gait analysis of ankle arthrodesis and arthroplasty: initial findings of a prospective study. Foot Ankle Int. 2012;33:282–289. doi: 10.3113/FAI.2012.0282. [DOI] [PubMed] [Google Scholar]
- 10.Rouhani H, Favre J, Aminian K, Crevoisier X. Multi-segment foot kinematics after total ankle replacement and ankle arthrodesis during relatively long-distance gait. Gait Posture. 2012;36:561–566. doi: 10.1016/j.gaitpost.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 11.Flavin R, Coleman SC, Tenenbaum S, Brodsky JW (2013) Comparison of gait after total ankle arthroplasty and ankle arthrodesis. Foot Ankle Int 34(10):1340–1348 [DOI] [PubMed]
- 12.Henricson A, Carlsson A, Rydholm U. What is a revision of total ankle replacement? Foot Ankle Surg. 2011;17:99–102. doi: 10.1016/j.fas.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 13.Davis RB, Õunpuu S, Tyburski D, Gage JR. A gait analysis data collection and reduction technique. Hum Movement Sci. 1991;10:575–587. doi: 10.1016/0167-9457(91)90046-Z. [DOI] [Google Scholar]
- 14.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krause FG, Windolf M, Bora B, Penner MJ, Wing KJ, Younger ASE. Impact of complications in total ankle replacement and ankle arthrodesis analyzed with a validated outcome measurement. J Bone Joint Surg. 2011;93-A:830–839. doi: 10.2106/JBJS.J.00103. [DOI] [PubMed] [Google Scholar]
- 16.SooHoo NF, Zingmond DS, Ko CY. Comparison of reoperation rates following ankle arthrodesis and total ankle arthroplasty. J Bone Joint Surg. 2007;89-A:2143–2149. doi: 10.2106/JBJS.F.01611. [DOI] [PubMed] [Google Scholar]
- 17.Singer S, Klejman S, Pinsker E, Houck J, Daniels T (2013) Ankle arthroplasty and ankle arthrodesis: gait analysis compared with normal controls. J Bone Joint Surg 95(24):e191(1–10) [DOI] [PubMed]
- 18.Ajis A, Henriquez H, Myerson M. Postoperative range of motion trends following total ankle arthroplasty. Foot Ankle Int. 2013;34:645–656. doi: 10.1177/1071100713481433. [DOI] [PubMed] [Google Scholar]
- 19.Queen RM, De Biasio JC, Butler RJ, DeOrio JK, Easley ME, Nunley JA. J. Leonard Goldner Award 2011: changes in pain, function, and gait mechanics two years following total ankle arthroplasty performed with two modern fixed-bearing prostheses. Foot Ankle Int. 2012;33:535–542. doi: 10.3113/FAI.2012.0535. [DOI] [PubMed] [Google Scholar]
- 20.Michael JM, Golshani A, Gargac S, Goswami T. Biomechanics of the ankle joint and clinical outcomes of total ankle replacement. J Mech Behav Biomed Mater. 2008;1:276–294. doi: 10.1016/j.jmbbm.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 21.Conley KA, Geist K, Shaw JN, Labib SA, Johanson MA. The effect of goniometric alignment on passive ankle dorsiflexion. Range of motion among patients following ankle arthrodesis or arthroplasty. Foot Ankle Spec. 2012;5:175–179. doi: 10.1177/1938640012444731. [DOI] [PubMed] [Google Scholar]
- 22.Sealey RJ, Myerson MS, Molloy A, Gamba C, Jeng C, Kalesan B. Sagittal plane motion of the hindfoot following ankle arthrodesis: a prospective analysis. Foot Ankle Int. 2009;30:187–196. doi: 10.3113/FAI.2009.0187. [DOI] [PubMed] [Google Scholar]
- 23.Wood PL, Deakin S. Total ankle replacement: the results in 200 ankles. J Bone Joint Surg. 2003;85-B:334–341. doi: 10.1302/0301-620X.85B3.13849. [DOI] [PubMed] [Google Scholar]
- 24.Hendrickx RP, Stufkens SA, de Bruijn EE, Sierevelt IN, van Dijk CN, Kerkhoffs GM. Medium- to long-term outcome of ankle arthrodesis. Foot Ankle Int. 2011;32:940–947. doi: 10.3113/FAI.2011.0940. [DOI] [PubMed] [Google Scholar]
- 25.Labek G, Todorov S, Iovanescu L, Stoica CI, Böhler N. Outcome after total ankle arthroplasty—results and findings from worldwide arthroplasty registers. Int Orthop. 2013;37:1677–1682. doi: 10.1007/s00264-013-1981-7. [DOI] [PMC free article] [PubMed] [Google Scholar]