Abstract
Purpose
External fixation is the recommended stabilization method for both open and closed fractures of long bones in forward surgical hospitals. Specific combat surgical tactics are best performed using dedicated external fixators. The Percy Fx© (Biomet) fixator was developed for this reason by the French Army Medical Service, and has been used in various theatres of operations for more than ten years.
Methods
The tactics of Percy Fx© (Biomet) fixator use were analysed in two different situations: for the treatment of French soldiers wounded on several battlefields and then evacuated to France and for the management of local nationals in forward medical treatment facilities in Afghanistan and Chad.
Results
Overall 48 externals fixators were implanted on 37 French casualties; 28 frames were temporary and converted to definitive rigid frames or internal fixation after medical evacuation. The 77 Afghan patients totalled 85 external fixators, including 13 temporary frames applied in Forward Surgical Teams (FSTs) prior to their arrival at the Kabul combat support hospital. All of the 47 Chadian patients were treated in a FST with primary definitive frames because of delayed surgical management and absence of higher level of care in Chad.
Conclusion
Temporary frames were mostly used for French soldiers to facilitate strategic air medical evacuation following trauma damage control orthopaedic principles. Definitive rigid frames permitted achieving treatment of all types of war extremity injuries, even in poor conditions.
Keywords: External fixation, War trauma, Damage control orthopaedic, Combat
Introduction
External fixation is considered to be the best primary form of long-bone fracture stabilization for soldiers treated on the battlefield [1–8]. The severity of combat-related extremity injuries and austerity of combat environments require a sequential management, with damage control surgery prior to evacuation out of the combat zone for definitive treatment in specialized surgical centers [9]. Combat Trauma Damage Control Orthopaedic (TDCO) procedures are based on temporary external fixation with goals of controlling the hemorrhage, restoring limb perfusion, soft-tissue debridement and achieving bone stability without disruption of the resuscitation process [10, 11]. Precise fracture reduction or rigid frames are not expected. The main objective is transportation out of the combat zone while decreasing pain and shock, and minimizing complications such as infection, damage of the soft-tissues, blood vessels and nerves [11, 12]. Once patients are evacuated to a high level of care facilities, definitive bone stabilization requires more secure and stable external fixation or internal fixation when soft-tissue envelope allows it [13].
In current armed conflicts, many local military or civilian nationals (including children) are also managed in forward surgical hospitals. Because host-nation medical services are not available or capable of performing complex reconstruction procedures, definitive treatment is performed by deployed surgeons with specific goals due to the limitation of soft tissue coverage means, internal fixation material and possibility of hospitalisation [14]. Definitive external fixation is often required for these patients because of contaminated wounds after delayed evacuation due to intra-theatre transportation difficulties or secondary transfer from local facilities [15]. To achieve bone union and bone reconstruction procedures stable and versatile external fixators should be available in the field hospitals.
These combat surgical tactics are best performed using specific external fixators. In 1979, the French Army Medical Service (FAMS) created the first external fixator dedicated to war purposes, disasters or low-resources setting—the Fixateur Externe du Service de Santé des Armées (FESSA) [8, 16]. Afterward, several military external fixation frames were developed [3, 7]. Characteristics of these war external fixators should include: appropriate rigidity, stability and stiffness of the construction; simple application, even for non specialized surgeons; insuring permanent good access to the wound; sterile package ready for use in the field; and acceptable price [6, 7]. In 2000, the trauma department of the Percy Military Hospital (Clamart, France) improved the FESSA concept creating the Percy Fx© (Biomet) external fixator, designed to achieve lower manufacturing cost for single use and to meet the North Atlantic Treaty Organization (NATO) standardization agreement [17–19]. The Percy Fx© (Biomet) fixator has now been used by French military surgeons for more than ten years, for primary and definitive treatment of combat-related extremity injuries on various theatres of operations all over the world.
The Percy Fx© (Biomet) external fixator
General characteristics
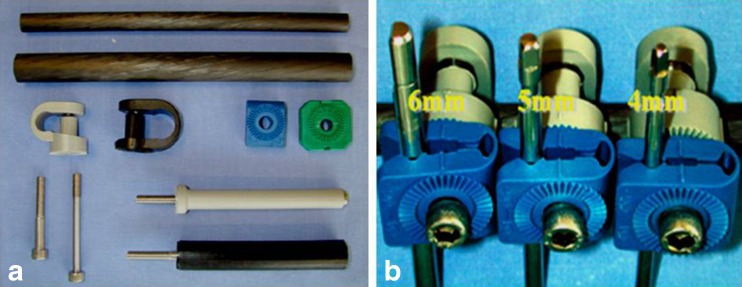
The fixator is composed of carbon tubes (diameters of 18 mm and 12 mm) and fiberglass composite parts: collars, lateral tubes and pin clamps. Pins clamps and collars are used for binding tubes and pins, tightened together with a hexagonal screw (Fig. 1). Each pin clamp allows a rotation of 360°. All components bear notches for easy assembly. This system authorizes a great variety of configurations: various types of frames can be obtained with various numbers and diameters of pins and tubes [20, 21]. This fixator is designed for single use with a sterile package, but it can be resterilized by humid heat and reused, which contributes to lowering costs [18]. Surgical tools are limited to a hexagonal stamp spanner, metal protecting tubes and guiding pins.
Fig. 1.
Components of the Percy Fx© (Biomet) fixator: 18/12 mm carbon tubes, collars and lateral tubes; PF1 (blue) and PF2 (green) pin clamps; hexagonal screws (a). PF1 clamps receiving pins of various diameter (b)
The main characteristics of the Percy Fx© (Biomet) fixator are:
Versatility: this equipment is adapted to trauma care, easy to assemble, and can be used for all fractures on both upper and lower extremity;
Modularity: pins are independent from the main frame, in order to be able to rectify assemblies, and are of various diameters (3, 4, 5 or 6 mm) for single plan frames or epiphyseal fixations;
Interoperability: with the possibility to replace various fixators used in NATO nations without ablation of the pins;
Small number of parts: for easy stock management and lower manufacturing costs;
Comfort: light, X-ray transparent and non magnetic system [17].
Conditions of use
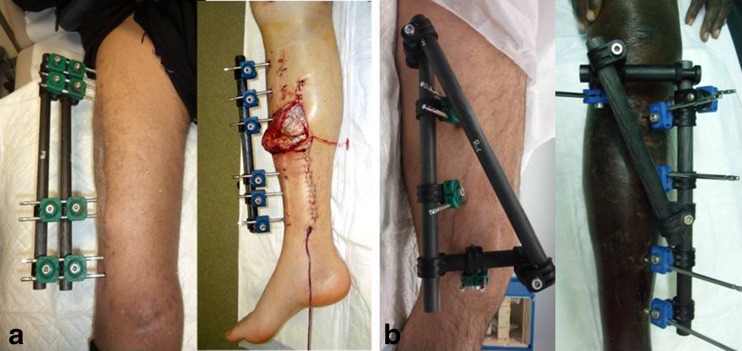
The Percy Fx© (Biomet) fixator can be used either as a transportation fixator for temporary stabilization of long bone shaft fractures and spanning fixation in peri-articular injuries, or as a definitive fixator capable to achieve bone union (Fig. 2 and Fig. 3).
Fig. 2.
Examples of spanning fixation of the wrist (a), elbow (b) and ankle (c)
Fig. 3.
Femoral and tibial diaphyseal frames (a) and metaphyseal frames around the knee (b)
The transportation configuration used for TDCO procedures involves unilateral frames with one tube and 2 × 2 half pins [7, 22, 23]. In adults, an 18-mm diameter tube is preferred for the lower extremity and a 12-mm diameter tube recommended for the upper extremity. The position and number of pins significantly modifies the result, e.g. spaced and independent pins increase stiffness [20, 21]. This fixator also permits adaptation of the diameter of pins to the diameter of the bone and to the magnitude of stresses (higher at the lower extremity). These single plan/single tube frames place the Percy Fx© (Biomet) fixator in the medium range of existing equipment in terms of stability [20, 21].
Various definitive configurations can be obtained with various numbers and diameters of pins and tubes, e.g. single or double tubes monoplane frames for diaphyseal fractures, or triangular double planes frames with epiphyseal fixation for metaphyseal fractures [23] (Fig. 3). Biomechanical studies showed that the frame stiffness with double planes or double tubes is comparable to the stiffest fixators. The modular system is a flexible solution to adapt the frames to the constraints (bone contact, loss of substance, patient’s weight, bone diameter, etc.) and to propose a gradual reduction in stiffness [20, 21, 24].
French military medical service experience
Tactical use of a combat external fixator depends on the operational setting and varies according to different factors: severity of soft tissue wounds, associated injuries in polytraumatized patients, need for a rapid evacuation out of the combat zone, caring for local nationals, and working in an isolated facility with limited resources [9, 11, 13]. We analysed the Percy Fx© (Biomet) fixator used by surgeons of FAMS in three different situations using the OPEX surgical database (Service de Santé des Armées).
Treatment of French soldiers
Between 2004 and 2013, 37 French soldiers were treated with the Percy Fx© (Biomet) fixator on various theatres of operations: Kosovo (one case), Iraq (two cases), Afghanistan (25 cases) and Africa (nine cases) including Chad, Ivory Coast, Mali and Central African Republic. All patients were males with a mean age of 30.6 ± 8.3 years. Mechanisms of injury were dominated by solid blast due to the use of Improvised Explosive Devices (IEDs) (Fig. 4). Damage control procedures were performed in level 2 or level 3 Medical Treatment Facilities (MTFs) before strategic evacuation to military hospitals (level 4 MTF) in France. Overall 48 Percy Fx© (Biomet) fixators were implanted for 30 open injuries and 18 closed injuries (Fig. 5 and Table 1).
Fig. 4.
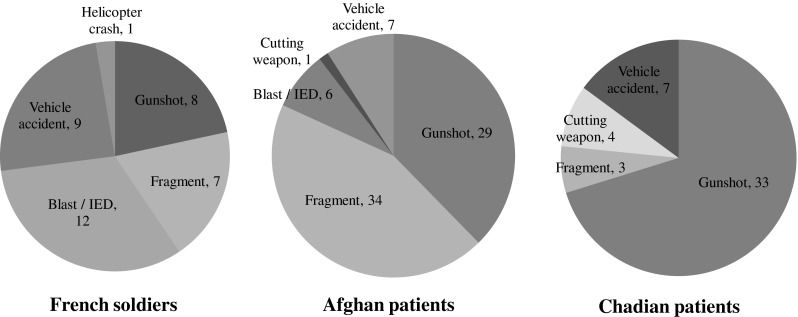
Distribution of injury mechanism (n)
Fig. 5.
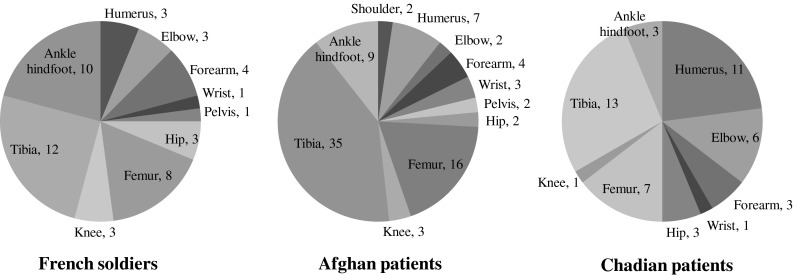
Distribution of external fixation anatomical location (n)
Table 1.
Tactical use of the Percy Fx© (Biomet) fixator
| Fixator | French soldiers, n = 37 (48 fixators) | Afghan patients, n = 77 (85 fixators) | Chadian patients, n = 47 (48 fixators) |
|---|---|---|---|
| Temporary frame (TDCO), n | 28 | 13 | 0 |
| Conversion to definitive frame, n | 14 | 9 | – |
| Conversion to internal fixation, n | 14 | 4 | – |
| Primary definitive frame, n | 20 | 72 | 48 |
| Minimal osteosynthesis, n | 10 | 6 | 1 |
Treatment of local nationals
Afghanistan
Between 2009 and 2012, 77 military or civilian Afghan patients were treated with the Percy Fx© (Biomet) fixator for a combat-related injury at the Kabul International Airport (KaIA) Combat Support Hospital (CSH). There were 71 males and six females, with a mean age of 29.4 ± 14 years, including nine children younger than 16 years of age. Mechanisms of injury were dominated by gunshot and fragment wounds (Fig. 4). Most of these patients were first managed in a Forward Surgical Team (FST, level 2 MTF) prior to definitive treatment in the KaIA CSH (level 3 MTF). An overall of 85 Percy Fx© (Biomet) fixators were implanted for 76 open injuries and nine closed injuries (Fig. 5 and Table 1).
Chad
Between 2008 and 2011, 47 military or civilian Chadian patients were treated with the Percy Fx© (Biomet) fixator for a combat-related injury in a FST deployed in N’Djamena. There were 46 males and one female, with a mean age of 28.5 ± nine years, including one child. Gunshot wound was the main injury mechanism (Fig. 4). All of these patients were directly admitted to this FST which was the higher level of care within the whole country. The mean delay time to admission was seven ± 7.8 days and varied from 12 hours to four weeks according to the patient provenance. An overall of 48 Percy Fx© (Biomet) fixators were exclusively implanted for open injuries (Fig. 5 and Table 1).
TDCO for French soldiers
Most of the French soldiers were injured by IED attacks against armoured vehicles, which explains the high proportion of closed injuries in this cohort [25]. These patients received state-of-the art treatment at different levels of the battlefield medical support. Temporary external fixation was the most common procedure for both open and closed injuries. Transportation fixators were dominated by tibial shaft and ankle spanning frames due to the predominance of lower extremity injuries in the solid blast trauma [25]. Conversely, 20 frames were right away definitive. Most of these cases were stable patients with isolated open tibial fractures for whose primary ideal external fixation could be performed in the absence of associated injury.
Conversion to definitive external fixation
Transition from temporary to definitive external fixation is required when conversion to internal fixation is unsuitable or impossible due to early infectious complications [13, 26]. For example, several authors recommended secondary circular (or hybrid) external fixation for open tibial fractures in the military setting [12, 26]. In this cohort, conversion to definitive external fixation was performed using the primary frames thanks to the modularity of the Percy Fx© (Biomet) fixator. Temporary diaphyseal frames were augmented by additional pins (2 × 3) and often required two tubes in a single plane. Some spanning frames for metaphyseal fractures were converted to double plane frames with epiphyseal fixation. In every case, placement of primary pins was crucial to limit additional trauma and early pin complications. Casper and Philips [22] caution against temporary frames because of their instability leading to infection and pin loosening. That is the reason why improvement of fracture reduction and conversion to a definitive frame should be performed as soon as possible (mean delay of eight ± seven days from the injury in this cohort). Minimal osteosynthesis was mainly associated with enhancing reduction of articular injuries, especially at the ankle or hindfoot level after blast injury (Fig. 6) [13, 27].
Fig. 6.
Bifocal femoral fracture (diaphyseal and epiphyseal) treated by a spanning external fixator associated with minimal osteosynthesis
Conversion to internal fixation
Definitive formal open reduction and internal fixation were performed in 14 cases after removal of the transportation fixator. Early conversion to internal fixation seems to be associated with improved bone healing and functional recovery in combat-related injuries [26, 28]. In a previous study, we found that conversion to internal fixation permitted reduction of the time to bone union compared to definitive external fixation [13]. However, secondary internal fixation remains a controversial issue in the war setting due to the risk of infectious complications [26, 28]. In this cohort, indications for secondary internal fixation were limited to highly selected cases according to current recommendations: five upper extremity diaphyseal fractures, four peri-articular injuries, four closed femoral shaft fractures and one pelvic ring fracture [26, 29]. All were early conversions (mean delay to 8.2 ± six days from the injury) and no infectious complication occurred.
Care for local nationals
In regions of conflict, military surgeons are often asked to provide care to local civilian patients for both diplomatic and humanitarian reasons [14]. Several factors complicate this assistance: limitations in hospitalization capabilities and medical supplies in forward MTFs; the lack of medical care system in the host country; uncertainty of the follow-up care [6]. Dougherty et al. [6] caution against the use of external fixation in local patients when the follow-up is uncertain: “device application should not be undertaken in a combat zone without reasonable assurance as to safe follow-up care and proper removal of the fixator”. Rowley [30], reporting the experience of the International Red Cross Committee (ICRC) experience in Kenya and Afghanistan, found that plaster casting permitted shorter hospitalization stay and fewer complications compared to external fixation. However, even in an austere environment where pin track infection and loosening seem to be more frequent, the use of external fixation has uncontestable advantages: to facilitate soft-tissue management of severe open injuries; to maintain acceptable reduction of unstable closed fractures when plaster casting or skeletal traction failed (especially for femoral fractures); and to permit early mobilization of adjacent joints [6–8, 12, 31].
Afghan patients managed in the KaIA CSH were soldiers, policemen and civilians victims of terrorism or collateral damage. Most of them presented fragment wounds due to mortar, rocket or various explosive devices. Tibial and femoral fractures were predominant with frequent bilateral lower limb injuries. TDCO procedures were performed in patients first managed in a FST prior to their arrival to the KaIA CSH and/or in unstable patients due to associated injuries. Definitive external fixation was required for highly contaminated wounds. Early conversion to internal fixation was performed in only four selected cases: two closed femoral shaft fractures, one closed pelvic ring fracture and one open radial shaft fracture. Once definitive surgical treatment was achieved, policemen and military patients were transferred to the Police or Military National Hospitals for rehabilitation and follow-up care. Conversely, the majority of civilian patients were fully managed in the KaIA CSH, including for rehabilitation and physical therapy, until bone union was obtained and the Percy Fx© (Biomet) fixator removed.
Most of the Chadian patients treated in the N’Djamena FST were soldiers wounded by gunshot during internal conflicts against various rebel groups. Humeral and tibial open fractures were predominant. Few explosive weapons were employed in these combats. However, many patients arrived with contaminated or infected wounds after difficult and extended medical evacuations in this extensive desert region: all of them were evacuated by road means in poor conditions after minimal primary care. There were no unstable polytraumatized patients in this cohort, because they died before they reached the FST. No TDCO procedures were performed because of the absence of unstable patients and the impossibility for further evacuation to higher level of care facilities. External fixation frames were immediately definitive, and no internal fixation was performed for these open injuries managed lately. As reported by Labeeu et al. [8] during the Rwandese war, we found that the use of the Percy Fx© (Biomet) fixator in this cohort was limited by two frequent complications: pin tract infection and loosening (whose rate was impossible to determine) due to unsatisfactory hygiene conditions; knee joint stiffness in cases of femoral fractures because of fascia lata contractures and impossibility for appropriate physiotherapy.
Future direction
Lerner et al. [12] recommend the use a staged protocol of external fixation for severe high-energy war injuries, with temporary unilateral tubular stabilization followed by definitive circular or hybrid fixation. The Ilizarov fixator offers specific advantages for definitive treatment of combat-related injuries: stability of peri-articular fractures with the possibility of early controlled motion; gradual correction of fracture displacement or malunions; compression in the fracture site for nonunions; restoration of bone defects by distraction osteogenesis [12].
In our experience, nonunions and bone defects are rather managed with adequate soft tissue coverage and secondary bone grafting [13]. Furthermore, the Ilizarov technique requires a careful follow-up for compression or distraction procedures, which is seldom possible in low-resources and/or war settings. However, we believe that hybrid fixators are particularly interesting for metaphyseal and peri-articular fractures, especially at the knee or ankle level. These devices represent an alternative to metaphyseal frames using pins, for which application is difficult and does not permit further axial corrections, or to internal fixation which remains risky for combat-related injuries [12, 13, 32]. At the present time, the FAMS is developing carbon ring receiving tension wires devoted to adaptation for Percy Fx© tubes in order to realize metaphyseal hybrid frames. This customized hybrid Percy Fx© (Biomet) fixator could be used for definitive stabilization of war injuries in high level trauma centres as well as in forward MTFs treating local nationals.
Conclusion
External fixation is the method of choice for the treatment of extremities injuries in war conditions. Modern TDCO procedures are based on a staged protocol of bone stabilization, including transportation external fixators applied on the battlefield, then converted to definitive stable frames or internal fixation (in selected cases) after evacuation out of the combat zone.
The Percy Fx© (Biomet) fixator is a versatile and modular device appropriate for both temporary and definitive stabilization of lower or upper extremity fractures. Simple transportation frames are easy to apply by any surgeon with minimal training. Definitive frames only require additional pins and tubes, in order to improve fracture reduction and increase fixator stiffness, without removal of the primary pins.
Since its conception, this external fixator was used by French surgeons on various theatres of operations all over the world. Transportation frames were mostly used to facilitate strategic evacuation of French casualties. Definitive rigid frames permitted achieving treatment of all types of war injuries, even for local nationals managed in forward MTFs in Afghanistan and Chad.
Development of a hybrid frame using a carbon ring will permit increasing the Percy Fx© (Biomet) fixator modularity, and to simplify definitive stabilization of metaphyseal or peri-articular injuries.
Acknowledgments
Conflict of interest
Sylvain Rigal: co-designer of the Percy Fx© (Biomet) external fixator.
The other authors declare that they have no conflict of interest.
References
- 1.Rich NM, Metz CW, Jr, Hutton JE, Jr, Baugh JH, Hughes CW. Internal versus external fixation of fractures with concomitant vascular injuries in Vietnam. J Trauma. 1971;11:463–476. doi: 10.1097/00005373-197106000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Mechelany E, Karrat K. External fixation device in treatment of severe injuries of the extremities caused by war projectiles: continuous series of 500 cases. Rev Chir Orthop Reparatrice Appar Mot. 1978;64(Suppl 2):36–40. [PubMed] [Google Scholar]
- 3.Bosse MJ, Holmes C, Vossoughi J, Alter D. Comparison of the Howmedica and Synthes military external fixation frames. J Orthop Trauma. 1994;8:119–126. doi: 10.1097/00005131-199404000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Has B, Jovanovic S, Wertheimer B, Mikolasević I, Grdic P. External fixation as primary and definitive treatment of open limb fractures. Injury. 1995;26:245–248. doi: 10.1016/0020-1383(95)90010-U. [DOI] [PubMed] [Google Scholar]
- 5.Dougherty PJ, Silverton C, Yeni Y, Tashman S, Weir R. Conversion from temporary external fixation to definitive fixation: shaft fractures. J Am Acad Orthop Surg. 2006;14:S121–S127. doi: 10.5435/00124635-200600001-00028. [DOI] [PubMed] [Google Scholar]
- 6.Reis ND, Zinman C, Besser MIB. A philosophy of limb salvage in war: use of the fixateur externe. Mil Med. 1991;156:505–520. [PubMed] [Google Scholar]
- 7.Koržinek K, Delimar D, Tripković B. External fixator for war purposes: the CMC fixator. Mil Med. 1999;164:358–360. [PubMed] [Google Scholar]
- 8.Labeeu F, Pasuch M, Toussaint P, Van Erps S. External fixation in war traumatology: report from the Rwandese war (October 1, 1990 to August 1, 1993) J Trauma. 1996;40(3):223–227. doi: 10.1097/00005373-199603001-00048. [DOI] [PubMed] [Google Scholar]
- 9.Andersen RC, Ursua VA, Valosen JM, Shawen SB, Davila JN, Baechler MF, Keeling JJ. Damage control orthopaedics: an in-theatre perspective. J Surg Orthop Adv. 2010;19:13–17. [PubMed] [Google Scholar]
- 10.Rigal S, Barthélémy R, Mathieu L, Barbier O. Indications of Trauma Damage Control Orthopaedics (TDCO) E-Mem Acad Natle Chir. 2013;12:45–49. [Google Scholar]
- 11.Possley DR, Burns TC, Stinner DJ, Murray CK, Wenke JC, Hsu JR, and the Skeletal Trauma Research Consortium Temporary external fixation is safe in a combat environment. J Trauma. 2010;69(1):135–139. doi: 10.1097/TA.0b013e3181e44fcb. [DOI] [PubMed] [Google Scholar]
- 12.Lerner A, Fodor L, Soudry M. Is staged external fixation a valuable strategy for war injuries to the limbs? Clin Orthop Relat Res. 2006;448:217–224. doi: 10.1097/01.blo.0000214411.60722.f8. [DOI] [PubMed] [Google Scholar]
- 13.Mathieu L, Bazile F, Barthélémy R, Duhamel P, Rigal S. Damage control orthopaedics in the context of battlefield injuries: the use of temporary external fixation on combat trauma soldiers. Orthop Traumatol Surg Res. 2011;97:852–859. doi: 10.1016/j.otsr.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 14.Klem C, Sniezek JC, Moore B, Davis MR, Coppit G, Schmalbach C. Microvascular reconstructive surgery in Operations Iraqi and Enduring Freedom: the US military experience performing free flaps in a combat zone. J Trauma Acute Care Surg. 2013;75(Suppl 2):228–232. doi: 10.1097/TA.0b013e318299da23. [DOI] [PubMed] [Google Scholar]
- 15.Mathieu L, Marty A, Ramaki A, Najib A, Ahmadzai W, Fugazzotto DJ, Rigal S, Shirzai N. Current issues with lower extremity amputations in a country at war: experience from the National Military Hospital. Eur J Trauma Emerg Surg. 2013 doi: 10.1007/s00068-013-0334-y. [DOI] [PubMed] [Google Scholar]
- 16.Meyrueis JP, Mine J, Rochat G, Mayaudon JL, Tripon P. A comparative mechanical study of types of external fixator. Rev Chir Orthop Reparatrice Appar Mot. 1980;66:317–321. [PubMed] [Google Scholar]
- 17.Di Schino M, Steenman C, Rigal S, Dalzoto G, Evrard P, Le Guilloux P, Bauer B. Development and specifications of the “Percy” external fixator. Med Arm. 2000;28:633–638. [Google Scholar]
- 18.Di Schino M, Steenman C, Rigal S, Dalzotto G, Evrard P, Gueugnon G, Poichotte A, Le Guilloux P. Description of the “Percy” external fixator. Med Arm. 2000;28:639–641. [Google Scholar]
- 19.No author listed (1998) Essential requirements of orthopaedic external fixation devices. NATO standardization agreement (STANAG)
- 20.Gueugnon G, Evrard P, Diop A, Poichotte A, Rigal S, Di Schino M, Lavaste F. Biomechanical study of the “Percy” external fixator: equipment, methods and results. Med Arm. 2000;28:643–653. [Google Scholar]
- 21.Gueugnon G, Evrard P, Diop A, Lavaste F, Rigal S, Di Schino M. Biomechanical study of the “Percy” external fixator: discussion. Med Arm. 2000;28:655–668. [Google Scholar]
- 22.Clasper JC, Philips SL. Early failure of external fixation in the management of war injuries. J R Army Med Corps. 2005;151:81–86. doi: 10.1136/jramc-151-02-04. [DOI] [PubMed] [Google Scholar]
- 23.Barbier O, Rigal S, Mathieu L. Principe de la fixation externe en traitement définitif. Montpellier: Sauramps Médical eds; 2012. [Google Scholar]
- 24.Fabre A, Sockeel P, Cadot P, Van Gaver E, Sene M, Di Schino M. Prospective clinical study of the “Percy” external fixator: 24 cases. Med Arm. 2000;28:679–688. [Google Scholar]
- 25.Kang DG, Lehman RA, Carragee EJ. Wartime spine injuries: understanding the improvised explosive device and biophysics of blast trauma. Spine J. 2012;12:849–857. doi: 10.1016/j.spinee.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 26.Murray CK, Hsu JR, Solomkin JS, Keeling JJ, Andersen RC, Ficke JR, Calhoun JH. Prevention and management of infections associated with combat related extremity injuries. J Trauma. 2008;64(Suppl 3):239–251. doi: 10.1097/TA.0b013e318163cd14. [DOI] [PubMed] [Google Scholar]
- 27.Pukljak D. External fixation—minimal osteosynthesis: indications, role, and place in war surgery. J Trauma. 1997;24:453–458. doi: 10.1097/00005373-199708000-00012. [DOI] [PubMed] [Google Scholar]
- 28.Mody RM, Zapor M, Hartzell JD, Robben PM, Waterman P, Wood-Moris R, et al. Infectious complications of damage control orthopaedics in war trauma. J Trauma. 2009;67:758–761. doi: 10.1097/TA.0b013e3181af6aa6. [DOI] [PubMed] [Google Scholar]
- 29.Bhandari M, Zlowodzki M, Tonetta P, III, Schimdt A, Templeman DC. Intramedullary nailing following external fixation in femoral and tibial shaft fractures. J Orthop Trauma. 2005;19:140–144. doi: 10.1097/00005131-200502000-00012. [DOI] [PubMed] [Google Scholar]
- 30.Rowley DI. The management of war wounds involving bone. J Bone Joint Surg. 1996;78B:706–709. [PubMed] [Google Scholar]
- 31.Padhi NR, Padhi P. Use of external fixators for open tibial injuries in the rural third world: panacea of the poor? Injury. 2007;38:150–159. doi: 10.1016/j.injury.2006.08.053. [DOI] [PubMed] [Google Scholar]
- 32.Carmack DB. Conversion from temporary external fixation to definitive fixation: periarticular injuries. J Am Acad Orthop Surg. 2006;14:S128–S130. doi: 10.5435/00124635-200600001-00029. [DOI] [PubMed] [Google Scholar]