Abstract
Purpose
Carrying out osteosynthesis is challenging, and controlling for results and complications is necessary to define the limits of acceptable complications. Within the context of sudden-onset disasters, comparing internal with external osteosynthesis remains controversial.
Methods
The most recent and significant Médecins Sans Frontières (MSF) experience with osteosynthesis was following the earthquake in Haiti in 2010: 353 external fixators were used in the 12 months following the catastrophe, 62 of which were used in the first month. Carrying out internal osteosynthesis was possible two weeks following the earthquake.
Results
The most common indication for open tibial fracture was Gustillo grade 2 or 3. Conversion rate from external to internal osteosynthesis remains anecdotal for several practical reasons. Advantages and drawbacks of external fixators are discussed in the context of precarious situations frequently encountered by MSF.
Conclusions
External osteosynthesis as a primary and definitive treatment for open fractures, especially of the leg, remains the most frequently used and best-adapted procedure in the context of sudden-onset disasters, even though not ideal.
Keywords: External fixation, Sudden-onset disaster, Humanitarian surgery
Introduction
Joint replacement, arthroscopy and osteosynthesis are the three most important breakthroughs in orthopaedic surgery in the last 60 years. Internal osteosynthesis has definitively and dramatically improved fracture healing and functional outcome. Médecins Sans Frontières (MSF) introduced internal osteosynthesis in a level-3 hospital several years ago and again following recent natural disasters. Under any circumstance, osteosynthesis is challenging, and controlling for results and complications is essential to define the limits of complication acceptance [1].
The most recent and significant experience for MSF was during the earthquake in Haiti in 2010. For 20 years, MSF has conducted a trauma centre, including a burn unit and rehabilitation facility. On 12 January 2010, an earthquake of magnitude 7 on the Richter scale struck Haiti, resulting in an estimated 220,000 deaths and 300,000 injuries. The epicentre was 25 km west of Port Au Prince, and almost all medical structures were severely damaged and affected. The specific context of Haiti in terms of poverty and urban violence made it extremely difficult to treat the injured. Between days one and three, MSF teams operated in the streets with minimal equipment; soon, however, conditions became marginally better when, on day four, MSF managed to create an operating theatre (OT) in a shipping container, which proved extremely challenging due to wind, rain and flies. On day 12, our inflatable hospital was functional, and teams could begin carrying out appropriate surgical care, including internal osteosynthesis.
Materials and methods
During the first three months, 248 patients were treated for orthopaedic trauma related to the earthquake, representing 259 fractures. Only 192 files were correctly documented. Average patient age was 29 years; 55 % were women. Not surprisingly, and as previous statistics show, there was a large number of open tibial and closed femoral fractures (Table 1).
Table 1.
Fracture location and type
| Closed (%) | Open (%) | Total | |||
|---|---|---|---|---|---|
| Humerus | 6, (67) | 3 (33) | 9 | ||
| Forearm | 11 (79) | 3 (21) | 14 | ||
| Femur | 70 (89) | 9 (11) | 79 | ||
| Tibia/fibula | 21 (23) | 69 (77) | 90 | ||
| Total | 108 (56) | 84 (44) | 192 | ||
Fractures were initially treated according to location and type. The most common intervention was external fixation (36 %) followed by nailing (19 %), plating (13 %), traction (11 %), amputation (11 %) and mini osteosynthesis (Table 2). MSF surgical experience is significantly linked to violent acts, such as those wounded in war or by SOD. In such contexts, external fixation of open fractures generally remains the rule. Table 3 shows the number of external fixations since MSF introduced data collection.
Table 2.
Treatment according to fracture type
| K wire | EF | Plate | Nail | Amputation | Traction | Other | |
|---|---|---|---|---|---|---|---|
| Closed | 15 | 6 | 28 | 44 | 26 | 1 | |
| Open 1 | 2 | 12 | 1 | 2 | 1 | ||
| Open 2 | 23 | 3 | 3 | 1 | |||
| Open 3Aa | 2 | 18 | 1 | 2 | |||
| Open 3Ba | 1 | 20 | 1 | ||||
| Open 3Ca | 6 | 1 | |||||
| NR | 7 | 4 | 1 | 21 | 3 | 3 | |
| Total | 20 (8 %) | 92 (36 %) | 32 (13 %) | 50 (19 %) | 28 (11 %) | 30 (11 %) | 7 (2 %) |
NR not reported, K wire Kirschner wire, EF external fixation
aGustillo grade
Table 3.
Number of external fixations per year in Médecins Sans Frontières (MSF) programmes
| Year | Number |
|---|---|
| 2007 | 730 |
| 2008 | 803 |
| 2009 | 695 |
| 2010 | 775 (Haiti: 352) |
| 2011 | 757 |
| 2012 | 651 |
Discussion
Von Shreeb et al. [2] conceptualised the characteristics of patient flow following sudden-onset disasters (SOD), distinguishing three phases that vary in duration.
The first phase—very short, approximatively three to four days—corresponds with the blackout period faced by all medical facilities. Total chaos reigns. There is no coordinated internal management, and external aid remains nonexistent, and medical facilities must cope the best they can with the ever-increasing flow of victims.
During the second phase, which can last several weeks, victim flow rate rapidly declines; external aid arrives.
The third phase, several weeks after the SOD, corresponds to managing surgery to alleviate complications from the initial treatment and reinstitution of elective surgery. At this stage, external aid has often left (Fig. 1).
Fig. 1.
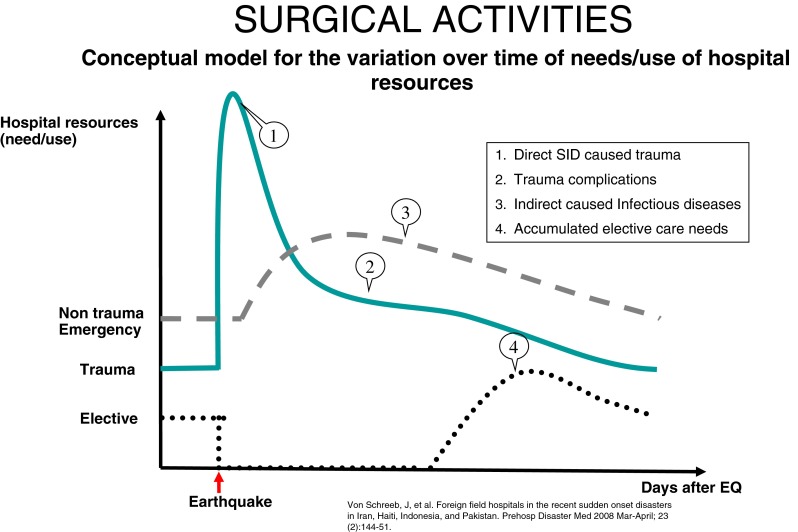
Conceptual model for variation of patient flow over time
Data collection and follow up
A major difficulty with this type of work is data collection and recording data. Data collection must take into account not only initial trauma management but also its follow-up until consolidation, which thus far has been insufficient at all stages. Disorganisation and patient movement may explain the difficulties encountered in the initial phase; also, data collection in such conditions is not a top priority, particularly for local caregivers. In Haiti, follow-up was extremely difficult, and complication rates were most probably underestimated.
Correctly setting an external fixator
Surgery by an MFS team following SOD is most often performed by general surgeons who, compared with orthopaedic surgeons, have relatively little knowledge of principles and techniques regarding appropriate bone fixation. Unilateral, uniplanar and, rarely, biplanar setups are recommended. Pins are inserted by hand; dynamisation is not possible. Plastic surgeons, who became involved for the first time in such disasters, are familiar with using local rotational flaps, helping transform fractures from to closed.
External fixation as definitive treatment
External fixation as definitive treatment for fractures has not been widely documented [3, 4] and remains disputed. Compared with intramedullary nailing, external fixation is associated with a higher incidence of malunion and nonunion: 26 % and 13 %, respectively, reported by Kimel [5], and 24 % and 20 %, respectively, by Gianoudis et al. [6]. However, other teams have published more promising results. Betsios et al. [7], in a series of 220 open and closed tibial fractures, consolidated 87 %. Vijay [8] recorded a success rate of 90 % for open tibial fractures Gustillo grades 3A and 3B. Some teams proposed osteosynthesis in the 15 days after setting an external fixator. This procedure is only possible if the patient is operated in a level 3 centre or if patients can be moved to such centres. External fixation is to be considered the definitive treatment in most cases of open fractures. MSF protocols are strict concerning fracture treatment. External fixation can only be used on open fractures; the only exception is pelvic fixation associated with life-threatening haemorrhaging, with a preference for EIAI fixation. In some trauma centres where a C-arm is available in the operating theatre, it may be used for joint fractures, especially for ankle traction.
Converting external fixators into internal fixators
As soon as we set up a level 3 hospital on day 12 following the disaster, we tried to convert external fixators into internal fixations. The electrical blackout period lasted three to four days, during which time we were unable to perform standard surgical care. A huge workload continued several weeks after power was restored. Conversion to internal fixation should be carried out before three weeks [9], but wound coverage must be appropriately performed, so very few patients could take advantage of a definitive internal osteosynthesis; this procedure was possible only for five patients. Intermedullary nailing was the choice for osteosynthesis.
Avoiding shortage of external fixators
We set 64 external fixators in the first 30 days, 13 the following month and 13 in the third month. The initial phase and often the second phase following an SOD are critical, because stocks are difficult to come by, and the care structure therefore needs to manage its stock of external fixators. With regards to Haiti, we had to give priority to specific indications, i.e. open tibial fractures; femoral or upper-limb fractures were first treated with traction and then with a posterior plaster splint.
Coping with complications
Early or late complications were not recorded systematically, particularly the incidence of infection (fractures; pins in external fixators). A major problem encountered following the Haiti earthquake was the overwhelming number of dressings required. The presence of a plastic surgeon in the initial and secondary phases would have allowed a number of open fractures to be covered and would most certainly have reduced the workload of changing dressings. The idea that early closure reduces the chance of infection and nonunion cannot be assumed. In our practice, war and SOD wounds should be treated in the same way: debridement and secondary closure at day five. This clearly means that external fixation remains our gold treatment in open fractures until consolidation and as our only tool for septic or nonunion complications.
Amputation vs external fixation
This area of surgery has often been debated and argued. The two main reasons for amputation following the Haiti disaster were either limbs that were irreparably shattered, or very late fasciotomy that developed massive infections within closed fractures from the beginning. In civilian studies, functional outcomes for severe injuries are not significantly different in patients who have undergone limb salvage compared with amputation. Long-term functionality is more dependent upon social factors than upon injury severity.
Conclusions
Our experience following the Haiti earthquake revealed that despite a relatively positive structure (surgical team onsite, swift setup of level 3 structure), the rate of conversion from external to internal osteosynthesis remains anecdotal and extremely difficult to manage. External osteosynthesis remains the most widely practiced and best adapted in the context of SOD for open fractures, especially of the leg, even though not ideal. Further information we gleaned from the earthquake in Haiti is that plastic surgeons can be very useful when treating definitive wounds by creating a flap that does not require frequent redressing and virtually elimates the need for late fasciotomy. Although many surgeons believe late fasciotomy is of value, we dispute that belief. Last but not least, data collection is a problem at all times and at all levels. It is obvious there is a long way to go in the development of a stronger emergent response to SOD.
References
- 1.Awais S, Saeed A. Study of the severity of musculoskeletal injuries and triage during the 2005 Pakistan earthquake. Int Orthop. 2013;37(8):1443–1447. doi: 10.1007/s00264-013-2013-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Von Shreeb J, Riddez L, Samnegård H. Foreign field hospitals in the recent sudden onset disasters in Iran, Haiti, Indonesia, and Pakistan. Prehosp Disaster Med. 2008;23(2):144–151. doi: 10.1017/s1049023x00005768. [DOI] [PubMed] [Google Scholar]
- 3.Liu L, Tan G, Luan F, Tang X, Kang P, Chongqi T, Pei F. The use of external fixation combined with vacuum sealing drainage to treat open comminuted fractures of tibia in the Wenchuan earthquake. Int Orthop. 2012;36(7):1441–1447. doi: 10.1007/s00264-011-1404-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schuind F, Andrianne Y, Burny F (2013) Treatment of forearm fractures by Hoffman external fixation. A study of 93 patients. Clin Orthop Relat Res (266):197–204 [PubMed]
- 5.Kimel RB. Results of treatment using the Hoffman external fixator for fractures of the tibia diaphysis. J Trauma. 1982;22:960–965. doi: 10.1097/00005373-198211000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Gianoudis PV, Papakostidis C, Roberts C. A review of the management of open fractures of the tibia and femur. J Bone Joint Surg (Br) 2006;88-B:281–289. doi: 10.1302/0301-620X.88B3.16465. [DOI] [PubMed] [Google Scholar]
- 7.Betsios M, Savvidou O, Kovanis J, Alexandropoulos P, Papagelopoulos P. External fixation as a primary and definitive treatment for tibia diaphyseal fractures. Strateg Trauma Limb Reconstr. 2009;4:81–87. doi: 10.1007/s11751-009-0062-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vijay C. Management of open type IIIA and type IIIB fractures tibia with LRS External Fixator. Internet J Orthop Surg. 2010;18:2. [Google Scholar]
- 9.Bhandari M, Zlowodski M, Tornetta P, Schmidt A, Templeman DC. Intramedullary nailing following external fixation in femoral and tibial shaft fractures. J Orthop Trauma. 2005;19(2):140–144. doi: 10.1097/00005131-200502000-00012. [DOI] [PubMed] [Google Scholar]


