Abstract
Purpose
This prospective randomized pilot study reports our institutional experience and early results using Sonoma Wrx (Sonoma Orthopedic Products, Santa Rosa, CA) in the treatment of extra-articular and simple intra-articular distal radius fractures.
Material and methods
A total of 64 patients, were enrolled in the study. They were considered eligible if they had; unstable extra-articular distal radius fractures and simple intra-articular distal radius fractures suitable for closed reduction (AO types; A2.2, A2.3, A3.1 C2.1, C2.2). Patients in group I received intramedullary fixation using the Sonoma Wrx® device and patients in group II received standard volar locking plate fixation. Radiographic criteria of acceptable healing were used for evaluation.
Results
Two groups were similar in terms of baseline characteristics. Mean time of operation was significantly shorter in Group 1 vs. in group 2 (36.81 ± 7.11 vs. 48.97 ± 5.9 minutes, p = 0.001). Time to healing of the fracture was not different between two groups (5.45 ± 1.09 vs. 5.70 ± 1.04 weeks for Group 1 vs. 2, respectively p = 0.36). Overall complications occurred in 9 patients in group 1 and in 15 patients in group 2 (p = 0.17). Follow-up was completed in all patients with a median time of 12 months and 13 months in group 1 and 2, respectively. On radiographic evaluation radial inclination, radial height and volar tilt were not significantly different between group 1 and 2, respectively. There were no significant differences between two groups in regard to wrist rotational degrees measured in last follow-up visit.
Conclusion
Sonoma Wrx Device is reliable and effective in terms of achieving satisfactory outcomes in treatment of distal radius fractures. It may be reasonable to use this device to prevent complications that are related to extensive soft tissue dissection.
Keywords: Distal radial fracture, Intramedullary nail, Volar locking plate, Complications
Introduction
Distal radius fractures account for 44 % of all types of hand and forearm fractures [1]. Incidence of distal radius fractures increase in two distinct age groups in which the injury occurs by two distinct mechanisms: high energy falls during sports activities in young and low energy falls in elderly patients with various risk factors. Closed reduction and cast stabilization is the accepted treatment in most cases, especially in low-demand elderly patients [2–4], whereas operative treatment provides better anatomical stabilization of the wrist and earlier improvement of functions in patients who had professional expectations.
Volar locking plate fixation has increasingly gained popularity in surgical treatment of distal radius fractures since it provides better functional outcomes than dorsal plating [5, 6]. However, the volar approach has its own disadvantages, such as large soft tissue dissection, tendon injury, hardware irritation and pain. Intramedullary nailing has been introduced as a contemporary technique in patients undergoing surgery for distal radius fractures. Limiting soft tissue irritation and providing earlier wrist motion, this technique may be an alternative to known methods for unstable fractures. Several devices were introduced with promising outcomes in treatment of extra-articular and simple intra-articular distal radius fractures [7–10]. However, to our knowledge, there has been no comparative clinical study reporting outcomes regarding the use of Sonoma Wrx (Sonoma Orthopedic Products, Santa Rosa, CA) in treatment of extra-articular and simple intra-articular distal radius fractures. This prospective randomized pilot study reports our institutional experience and early results using this novel technique.
Material and methods
The study was approved by the local ethics committee. All patients gave consent to take part in the research. The study was undertaken on a prospective basis and study participants were considered eligible if they had unstable extra-articular distal radius fractures and simple intra-articular distal radius fractures suitable for closed reduction (AO types; A2.2, A2.3, A3.1 C2.1, C2.2). Operative fixation was considered as indicated in the presence of radial shortening >3 mm, dorsal tilt >10 degrees and intra-articular step-off >2 mm following cast fixation. Patients who had stable fractures that were suitable for cast fixation, previous wrist or distal radius injury or deformity, open fractures, accompanying ulnar fractures were not considered eligible for the study.
A total of 64 patients were enrolled in the study between December 2012 and October 2013. Baseline characteristics of the patients were given in Table 1. On the day of admittance, patients’ demographic and clinical data were recorded and an independent orthopaedist performed physical examination and initial radiographic evaluation. Patients were randomly allocated into two treatment arms using a computerized random number generator. Patients in group 1 received intramedullary fixation using the Sonoma Wrx® device and patients in group 2 received standard volar locking plate fixation.
Table 1.
Baseline patient characteristics
| Variable | Group 1 (flexible nail) (N = 31) | Group 2 (volar plaque) (N = 33) | P value |
|---|---|---|---|
| Age (years) | 47.90 ± 15.27 | 45.64 ± 14.48 | 0.54 |
| Male gender | 6 (19.4 %) | 6 (18.2 %) | 0.90 |
| Right sided fracture | 15 (48.4 %) | 14 (42.4 %) | 0.63 |
| Mechanism of injury | |||
| Fall | 19 (61.3 %) | 22 (66.7 %) | 0.65 |
| Vehicle accident | 6 (19.4 %) | 7 (21.2 %) | 0.85 |
| Sports injury | 5 (16.1 %) | 4 (12.1 %) | 0.72 |
| Assault injury | 1 (3.2 %) | 0 (0.0 %) | 0.48 |
| Concomitant injury | |||
| None | 24 (77.4 %) | 24 (72.7) | 0.66 |
| Calcaneus fracture | 1 (3.2 %) | 1 (3 %) | 1.0 |
| Humerus fracture | 1 (3.2 %) | 2 (6.1 %) | 1.0 |
| Lumbar vertebral fracture | 1 (3.2 %) | 0 (0.0 %) | 0.48 |
| Shoulder fracture | 2 (6.5 %) | 1 (3.0 %) | 0.60 |
| Femur fracture | 2 (6.5 %) | 3 (9.1 %) | 1.0 |
| Malleolus fracture | 0 (0.0 %) | 2 (6.1 %) | 0.50 |
| Type of fracture | |||
| A2.2 | 5 (16.1 %) | 5 (15.2 %) | 1.0 |
| A2.3 | 7 (22.6 %) | 10 (30.3 %) | 0.48 |
| A3.1 | 14 (45.2 %) | 10 (30.3 %) | 0.22 |
| C2.1 | 2 (6.5 %) | 4 (12.1 %) | 0.67 |
| C2.2 | 3 (9.7 %) | 4 (12.1 %) | 1.0 |
Values given as n (%) unless otherwise noted
Surgical technique
Sonoma Wrx® Wrist fracture repair device
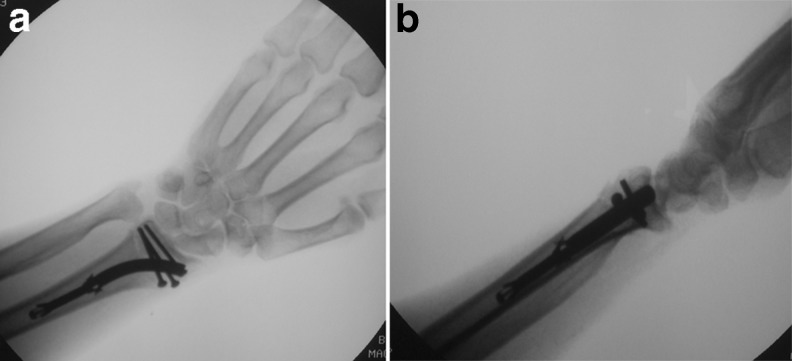
All operations were performed with the patients under regional or general anaesthesia and the procedures were undertaken by one of three experienced surgeons. The operation was performed by using the technique provided by the manufacturer. A proximal arm tourniquet was applied and index and middle fingers were placed in traction. Then, we made a 2–3 cm incision over the radial styloid and we exposed the superficial branch of radial nerve using blunt dissections. Care was taken to avoid injury to this nerve. Using sharp dissections, we exposed the radial styloid between first and second dorsal extensor compartments. We placed a temporary K wire just beneath the subchondral bone and then we inserted a 3-mm S-shaped awl about 3–5-mm proximal to the radial styloid to create an entry hole. Then the awl was advanced through the radius body while stability of the reduction was controlled under fluoroscopy guidance. An appropriate size hub nail was selected according to the size of S-shaped awl that could be inserted. The channel was reamed, and then the Sonoma Wrx device was inserted. After insertion, using appropriate drivers, the grippers on the device were actuated and the device was deployed to provide solid fixation. The fixation was confirmed by fluoroscopy and the actuation driver was removed. Then, we inserted appropriate sized proximal and buttress screws and confirmed the fixation of the fracture in anteroposterior and lateral radiographic views (Fig. 1). Before skin closure, stability of the distal radio-ulnar joint was examined in pronation, supination and rotation.
Fig. 1.
Loss of degrees compared to healthy side
Volar locked plating
An arm tourniquet was applied and open reduction was performed using the volar approach. The plate was placed and locking screws were inserted. The position of the plate and correct reduction were confirmed using radiographic views. Range of motion and fracture stability were examined before skin closure.
Postoperative care
All arms were placed in volar splints for approximately seven to ten days after the operation. Immediate forearm, wrist and thumb movements were encouraged. Patients were allowed to perform strenuous tasks and weight bearing once radiographic fracture union was achieved.
Follow-up
Patients were invited to outpatient visit after the first month and every three months after the operation. The latest follow-up examination included radiographic evaluation and assessment of rotational capability of the affected wrist in comparison with the contralateral side. Anteroposterior and lateral radiographs were assessed by an independent radiologist. Radial inclination, volar tilt and radial height were measured in both healthy and affected wrists to evaluate acceptable healing. Graham’s [11] radiographic criteria of acceptable healing were used for evaluation. Range of wrist motions (palmar flexion, dorsal flexion, radial deviation, ulnar deviation, supination and pronation) was measured with a goniometer. The difference between the degree of movement between the healthy and affected sides was defined as loss of range of motion. Subjective and objective data were combined in Stewart’s scoring system [12] and Gartland and Werley [13] scoring system for each patient.
Statistical analyses
All statistical analyses were performed using SPSS (SPSS version 16.0 Inc., Chicago, IL, USA) packaged software. Visual histograms and analytical methods (Kolmogorov-Simirnov/Shapiro-Wilk’s test) were used for determination of normal distribution. Continuous variables were defined by the mean ± standard deviations. Parametric data were compared using independent sample t test, and non-parametric data were compared using Mann Whitney test. Categorical variables were compared using chi-square test or Fisher’s exact test where appropriate. A p-value of less than 0.05 was considered to be statistically significant.
Results
There were no significant differences between two groups in regard to baseline demographics, mechanism of injury and classification of fracture type (Table 1). No crossover occurred between treatment arms during the pre-operative stage, and all patients were operated on as planned. Three patients who had concomitant humerus fractures received an initial closed reduction and cast fixation before the operation. Patients with other concomitant fractures were treated appropriately before the operation for distal radius fracture was undertaken. Mean time from injury to operation was 3.45 ± 1.45 days and 3.61 ± 1.40 days in group 1 and group 2, respectively (p = 0.66). Mean time of operation was significantly shorter in group 1 than it was in group 2 (36.81 ± 7.11 min vs. 48.97 ± 5.9 min, p = 0.001). Time to healing of the fracture was not different between two groups (5.45 ± 1.09 vs. 5.70 ± 1.04 weeks for group 1 vs. 2, respectively; p = 0.36). Although, loss of palmar flexion was significantly higher in group 2 than that found in group 1, the difference was not of functional and clinical importance (<10 degrees).
Overall complications occurred in nine patients in group 1 and in 15 patients in group 2 (p = 0.17) (Table 2). Tendon damage occurred in one patient from group 2 and this patient received an additional operation for tendon transfer. Mild symptoms of carpal tunnel syndrome were observed in three patients in group 2 without requiring further interventions. Paresthesia of the radial nerve occurred in three patients in group 1 whereas such complication was not encountered in any one of the group 2 patients (p = 0.10). These three patients were those whom we operated on earlier during the study course and such complication has not occurred in the last 20 patients. The symptoms in these three patients were transient and improved without treatment. Patients who had skin infection (two patients in group 1 and four patients in group 2) responded well to administration of parenteral antibiotics and those who had tenosynovitis (three patients in group 1 and two patients in group 2) also responded well to analgesics and anti-inflammatory drugs.
Table 2.
Postoperative complications
| Complication | Group 1 flexible nail (N = 31) | Group 2 volar plaque (N = 33) | P value |
|---|---|---|---|
| Overall | 9 (29.0 %) | 15 (45.5 %) | 0.17 |
| Tendon rupture | 0 (0.0 %) | 1 (3.0 %) | 1.0 |
| Carpal tunnel syndrome | 0 (0.0 %) | 3 (9.1 %) | 0.23 |
| Sudek atrophy | 0 (0.0 %) | 2 (6.1 %) | 0.49 |
| Radial nerve paraesthesia | 3 (9.7 %) | 0 (0.0 %) | 0.10 |
| Pain at wrist | 1 (3.2 %) | 3 (9.1 %) | 0.61 |
| Infection | 2 (6.5 %) | 4 (12.1 %) | 0.67 |
| Tenosynovitis | 3 (9.7 %) | 2 (6.1 %) | 0.66 |
Values given as n (%)
Follow-up was completed in all patients with a median time of 12 months (range nine to 17 months) and 13 months (range ten to 19 months) in groups 1 and 2, respectively. On radiographic evaluation radial inclination (19.58 ± 2.65 degrees vs. 19.79 ± 2.59 degrees, p = 0.75), radial height (8.55 ± 2.04 mm vs. 8.33 ± 2.31 mm, p = 0.69) and volar tilt (9.61 ± 1.45 degrees vs. 9.39 ± 1.65 degrees, p = 0.57) were not significantly different between grosup 1 and 2, respectively. Table 3 shows rates for fulfilling Graham’s criteria for acceptable healing. We achieved similar rates in two groups. There were no significant differences between two groups with regard to wrist rotational degrees measured in last follow-up visit (palmar flexion: 70.32 ± 11.48 vs. 66.03 ± 10.71, p = 0.12; dorsal flexion: 65.19 ± 12.08 vs. 66.09 ± 11.98, p = 0.76; radial deviation 21.13 ± 6.7 vs. 21.67 ± 6.77, p = 0.75; ulnar deviation: 38.71 ± 7.18 vs. 39.09 ± 6.55, p = 0.82; supination: 85.32 ± 7.40 vs. 85.91 ± 6.78, p = 0.74; and pronation: 82.10 ± 9.01 vs. 81.97 ± 8.74, p = 0.95, for groups 1 and 2, respectively). Figure 2 shows loss of motion with healthy wrist was considered as the base of reference in each individual patient. Stewart and Gartland and Werley scores are given in Table 4.
Table 3.
Fulfilling rates of the radiographic healing criteria defined by Graham et al. [10]
| Variable | Group 1 flexible nail (N = 31) | Group 2 volar plaque (N = 33) | P value |
|---|---|---|---|
| Radial inclination ≥15 degrees | 30 (96.8 %) | 32 (97.0 %) | 0.96 |
| Radial shortening <5 mm vs. healthy wrist | 29 (93.5 %) | 29 (87.9 %) | 0.67 |
| Volar tilt <20 degrees | 31 (100.0 %) | 33 (100.0 %) | 1.0 |
Values given as n (%)
Fig. 2.
Fluoroscopic images of intramedullary nail
Table 4.
Stewart and Gartland and Werley [12] scores of patients
| Variable | Group 1 flexible nail (N = 31) | Group 2 volar plaque (N = 33) | P value |
|---|---|---|---|
| Stewart score | |||
| Mean | 1.52 ± 0.62 | 1.45 ± 0.66 | 0.57 |
| Excellent | 17 (54.8 %) | 21 (63.6 %) | 0.47 |
| Good | 12 (38.7 %) | 9 (27.3 %) | 0.33 |
| Fair | 2 (6.5 %) | 3 (9.1 %) | 1.00 |
| Gartland and Werley score | |||
| Mean | 1.77 ± 0.84 | 1.64 ± 0.82 | 0.46 |
| Excellent | 14 (45.2 %) | 18 (54.5 %) | 0.45 |
| Good | 11 (35.5 %) | 10 (30.3 %) | 0.66 |
| Fair | 5 (16.1 %) | 4 (12.1 %) | 0.73 |
| Poor | 1 (3.2 %) | 1 (3.0 %) | 1.0 |
Values given as mean ± SD or n (%)
Discussion
We achieved satisfactory outcomes using a novel intramedullary fixation device in patients with unstable distal radius fractures. In this study, two groups were similar in terms of acceptable healing criteria [11]. We demonstrated that the technique seems non-inferior to the standard treatment (i.e. volar locking plating) in terms of radiographic and functional outcomes. In addition, it takes shorter time to implant the intramedullary device, although this finding is subject to criticism since the difference we found between the two groups (about ten to 15 minutes) does not seem to be of clinical significance. However, operative times that we had using the new device were not longer than those we had in volar locking plating which we have already been familiar with. Therefore, we think that the novel technique seems to offer a steep learning curve. The number of patients was limited to draw a conclusion regarding the superiority of any technique over the other in terms of postoperative complications. However, the fact that the Sonoma Wrx device requires a smaller incision than that is made when implanting a volar locking plate seems to be its major advantage without taking further risk of complications.
There have been no clinical studies comparing the reliability and effectiveness of the technique described here. Rhee et al. reported [14] their preliminary results in six patients aged between 42 and 81 years. Mean range of motion parameters they reported in a mean of 17.4 weeks were slightly lower than those we found in about one-year follow-up (wrist flexion = 46 degrees, wrist extension = 56 degrees, radial deviation = 18 degrees, ulnar deviation = 27 degrees, pronation = 89 degrees and supination = 82 degrees). Mean time to healing they reported was longer (ten weeks, range six to 20 weeks) than that we reported herein. They reported similar values for mean radial height (11 mm, range 9–14 mm) and mean radial inclination (24 degrees, range 18–29 degrees) to those we found; whereas they found a lower mean volar tilt (3 degrees, range –4 to 10 degrees) than that found in our patients.
Recent studies regarding other types of intramedullary nail fixation devices reported satisfactory results. Gradi et al. [15] reported in a prospective randomized trial that they achieved similar clinical outcomes in patients who received either volar locking plates or Targon DR intramedullary fixation device for treatment of distal radius fractures. Postoperative complications occurred rarely and the authors could not draw a definitive conclusion within this context. Safi et al. [16] compared MICRONAIL intramedullary nailing device with volar plating and they found better clinical outcomes six weeks after the operation, whereas one-year results of two techniques were similar. The authors concluded that, since this technique requires minimal invasiveness and provides better stability, it allows for early active rehabilitation. Using the Sonoma Wrx device, we found no significant differences in terms of both postoperative healing and complications.
Injury to the superficial branch of the radial nerve is one possible complication during implantation of intramedullary nail fixation devices that is introduced over the radial styloid. Safi et al. [16] encountered this complication in one out of 31 patients they treated using the MICRONAIL device whereas Gradi et al. [15] found it in seven out of 55 patients they treated using the Targon DR device. We experienced that this complication would be prevented with increasing familiarity with the technique.
The Sonoma Wrx Device stands out with two particular features: flexible insertion of the distal intramedullary portion of the nail which is then converted into a solid part when the final position is achieved and actuation of the grippers provides increased stabilization within radius shaft [14]. We conclude that the Sonoma Wrx Device is reliable and effective in terms of achieving satisfactory clinical outcomes in treatment of distal radius fractures. It may be reasonable to use this device to prevent complications that are related to extensive soft tissue dissection. However, further study is needed to establish its safety and usefulness in various age groups and in presence of different clinical scenarios. This pilot study is subject to criticism due to low number of patients, exclusion of cases with complex fractures and lack of early radiographic data.
Acknowledgments
Conflict of interest
None of the authors have financial relationships and there has been no conflict of interest to declare.
References
- 1.Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg (Br.) 2001;26:908–915. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 2.Young BT, Rayan GM. Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. Hand Surg Am. 2000;25:19–28. doi: 10.1053/jhsu.2000.jhsu025a0019. [DOI] [PubMed] [Google Scholar]
- 3.Arora R, Gabl M, Gschwentner M, Deml C, Krappinger D, Lutz M. A comparative study of clinical and radiologic outcomes of unstable colles type distal radius fractures in patients older than 70 years: nonoperative treatment versus volar locking plating. J Orthop Trauma. 2009;23:237–242. doi: 10.1097/BOT.0b013e31819b24e9. [DOI] [PubMed] [Google Scholar]
- 4.Cui Z, Pan J, Yu B, Zhang K, Xiong X. Internal versus external fixation for unstable distal radius fractures: an up-to-date meta-analysis. Int Orthop. 2011;35:1333–41. doi: 10.1007/s00264-011-1300-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walenkamp MM, Bentohami A, Beerekamp MSH, Peters RW, van der Heiden R, Goslings JC, Schep NW. Functional outcome in patients with unstable distal radius fractures, volar locking plate versus external fixation: a meta-analysis. Strategies Trauma Limb Reconstr. 2013;8:67–75. doi: 10.1007/s11751-013-0169-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Protopsaltis TS, Ruch DS. Volar approach to distal radius fractures. J Hand Surg (Br.) 2008;33:958–965. doi: 10.1016/j.jhsa.2008.04.018. [DOI] [PubMed] [Google Scholar]
- 7.Ilyas AM, Thoder JJ. Intramedullary fixation of displaced distal radius fractures: a preliminary report. J Hand Surg (Br.) 2008;33:1706–1715. doi: 10.1016/j.jhsa.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 8.Capo JT, Hashem J, Orillaza NS, Tan V, Warburton M, Bonilla L. Treatment of extra-articular distal radial malunions with an intramedullary implant. J Hand Surg (Br.) 2010;35:892–899. doi: 10.1016/j.jhsa.2010.02.032. [DOI] [PubMed] [Google Scholar]
- 9.Orbay JL, Touhami A, Orbay C. Fixed angle fixation of distal radius fractures through a minimally invasive approach. Tech Hand Up Extrem Surg. 2005;9:142–148. doi: 10.1097/01.bth.0000173374.97406.70. [DOI] [PubMed] [Google Scholar]
- 10.Schmelzer-Schmied N, Wieloch P, Martini AK, Daecke W. Comparison of external fixation, locking and non-locking palmar plating for unstable distal radius fractures in the elderly. Int Orthop. 2009;33:773–8. doi: 10.1007/s00264-007-0504-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Graham TJ. Surgical correction of malunited fractures of the distal radius. J Am Acad Orthop Surg. 1997;5:270–281. doi: 10.5435/00124635-199709000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Stewart HD, Innes AR, Burke FD. Functional cast-bracing for Colles’ fractures. a comparison between cast-bracing and conventional plaster casts. J Bone Joint Surg (Br) 1984;66:749–53. doi: 10.1302/0301-620X.66B5.6389558. [DOI] [PubMed] [Google Scholar]
- 13.Gartland JJ, Jr, Werley CW. Evaluation of healed Colles’ fractures. J Bone Joint Surg Am. 1951;33:895–907. [PubMed] [Google Scholar]
- 14.Rhee PC, Shin AY. Minimally invasive flexible insertion and rigid intramedullary nail fixation for distal radius fractures. Tech Hand Up Extrem Surg. 2012;16:159–65. doi: 10.1097/BTH.0b013e31825c83e7. [DOI] [PubMed] [Google Scholar]
- 15.Gradl G, Mielsch N, Wendt M, Falk S, Mittlmeier T, Gierer P, Gradl G. Intramedullary nail versus volar plate fixation of extra-articular distal radius fractures. two year results of a prospective randomized trial. Injury. 2014;45:3–8. doi: 10.1016/j.injury.2013.10.045. [DOI] [PubMed] [Google Scholar]
- 16.Safi A, Hart R, Těknědžjan B, Kozák T. Treatment of extra-articular and simple articular distal radial fractures with intramedullary nail versus volar locking plate. J Hand Surg Eur. 2013;38:774–9. doi: 10.1177/1753193413478715. [DOI] [PubMed] [Google Scholar]