Abstract
Purpose
Pre-operative donation of autologous blood has been widely used in elective joint replacement procedures to avoid the risks of allogeneic blood transfusions. However, the high percentage of wasted autologous blood questions the general efficacy of pre-operative autologous blood donation (PABD) for all patients undergoing hip replacement. This study prospectively investigates the impact of a targeted pre-operative autologous blood donation protocol for anaemic patients on allogeneic and overall transfusion rates in 2,350 unilateral primary total hip arthroplasty procedures.
Methods
Patients with pre-operative haemoglobin less than 12.5 g/dL were advised to donate one unit of autologous blood seven to 15 days prior to the date of surgery. The targeted protocol was followed by 2,251 patients: 280 out of 367 anaemic patients donated while 1,971 out of 1,983 non-anaemic patients did not donate.
Results
Results showed a significantly lower rate of allogeneic transfusion for anaemic patients who predonated than anaemic patients who did not (13 % vs. 37 % respectively, p < 0.001). Overall transfusion rates for patients who followed the protocol (n = 2,251) were found to be 0.17 units/patient compared to previously reported numbers of 0.75 units/patient when routine donation was used. Among the 2,251 patients who followed the protocol, only 140 patients (6 %) had their autologous blood wasted, in contrast to values reported in the literature ranging from 14 % up to 50 %.
Conclusions
Targeted PABD reduces the need for allogeneic blood transfusion in anaemic patients and significantly reduces the overall number of transfusions compared to routine pre-operative autologous donation.
Keywords: Anaemia, Total hip arthroplasty, Blood management, Preoperative autologous blood donation, Allogeneic, Transfusion
Introduction
Pre-operative donation of autologous blood has been widely used in elective orthopaedic surgeries to avoid the risks of allogeneic blood transfusions. Inherent risks of allogeneic blood include the risk of transfusion reactions, infection transmission, as well as a higher risk of postoperative infections and complications attributed to transfusion-related immunomodulation [1, 2]. The high percentage of wasted autologous blood questions the general efficacy of pre-operative autologous blood donation (PABD) [3, 4]. Wastage rates up to 50 % have been reported in a previous study involving 9,482 patients undergoing total joint arthroplasty [5].
The role of pre-operative haemoglobin (Hb) in estimating transfusion needs has been established in several studies [3, 6–8]. Blood management strategies rely on optimization of pre-operative haemoglobin levels through iron supplementation with or without erythropoietin, hypotensive anaesthesia, blood salvage, pharmacologic agents, as well as pre-operative autologous blood donation [9–14]. Patients with haemoglobin above 13 g/dL have a transfusion risk five times lower than those in the 11–13 g/dL range and are associated with the highest percentage of wasted autologous blood [15]. A previous study from our centre comparing routine PABD for all patients to a control group revealed that while PABD reduces the allogeneic blood exposure for anaemic patients, it has no effect in non-anaemic patients [16]. Subsequently, targeted autologous blood donation based on pre-operative haemoglobin levels was introduced at the authors’ institution.
The present study aims to compare targeted autologous blood donation to the previously reported protocol of routine PABD for all patients by answering the following questions: (1) What is the incidence of allogeneic blood transfusion in non-anaemic patients when pre-operative donation is abandoned? (2) Is autologous blood donation effective in anaemic patients? (3) What is the impact of targeted blood donation on overall transfusion rates?
Materials and methods
Prospectively, 2,252 patients were pre-operatively screened by the Blood Preservation Center between October 2009 and May 2013. Patients underwent 2,350 unilateral primary total hip replacements by 13 surgeons at the authors’ institution and were enrolled into the Blood Preservation Center by the individual surgeons’ private offices. All procedures were performed utilizing a standardized posterior approach with hypotensive spinal–epidural anaesthesia. A total of 995 males and 1,355 females with an average age of 64 years (range, 18–94 years) were enrolled. The average BMI was 25 kg/m² (range, 11.7–51.5 kg/m²). The study was approved by the Institutional Review Board.
Patients were divided by pre-operative haemoglobin level, utilizing 12.5 g/dL as a cutoff. Although the World Health Organization defines anaemia differently for males and females (less than 13 g/dL and 12 g/dL, respectively), this threshold was based on previous data from our institution showing significantly less benefit from autologous blood donation and more units wasted with haemoglobin values greater than 12.5 g/dL [8]. Patients with a hemoglobin level of 12.5 g/dL or more were considered non-anaemic and were not asked to donate blood prior to surgery. Patients with a pre-operative haemoglobin level less than 12.5 g/dL were advised to donate one unit of autologous blood. Patients were asked to donate seven to–15 days prior to the date of surgery, and no patient was allowed to donate less than seven days prior to the procedure. Gender, age, BMI, pre-operative Hb, date of pre-operative Hb measurement, date of autologous blood donation, number of autologous transfusions, number of allogeneic transfusions, time of transfusion, postoperative Hb levels until date of discharge, and in-house complications were recorded. Patients with bleeding disorders were excluded and patients whose actual blood management deviated from the standard protocol were analysed as separate groups.
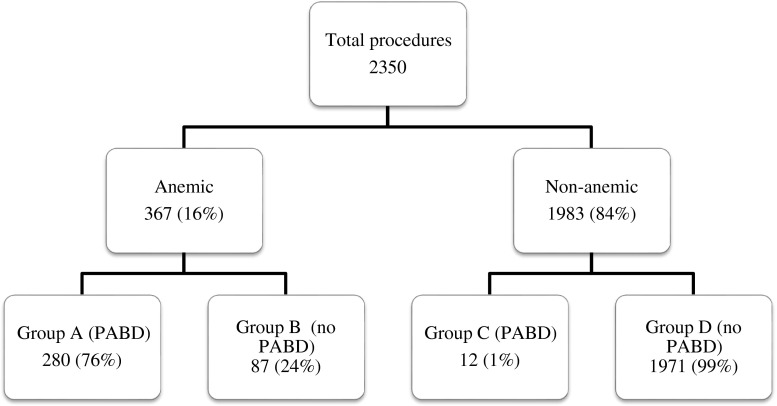
Of 367 (16 %) total hip arthroplasty (THA) procedures performed in anaemic patients, 280 (76 %) followed the protocol and donated one unit of autologous blood (group A), while 87 (24 %) chose not to donate (group B). Patients in the anaemic groups A and B had a mean pre-operative haemoglobin level of 11.7 g/dL and 11.5 g/dL, respectively. Of 1,983 procedures performed in non-anaemic patients, pre-operative donation of an autologous unit took place in 12 cases (1 %) (group C), while 1,971 (99 %) followed protocol by not donating (group D). The mean pre-operative Hb for the non-anaemic patients was 13.4 g/dL and 14.1 g/dL for groups C and D, respectively. Patients received one allogeneic transfusion if their haemoglobin level dropped below 8.0 g/dL and the patient displayed clinical symptoms of anaemia (tachycardia and/or hypotension) despite intravenous fluid boluses. The decision to transfuse autologous blood was made at the discretion of the anaesthesiologist and medical attending, and strict transfusion guidelines were not enforced for the administration of autologous blood (Fig. 1).
Fig. 1.
Patient distribution by number of total hip arthroplasty procedures according to targeted PABD protocol
All four groups were similar in terms of age and BMI (Table 1). Groups A and D represent the targeted blood centre algorithm. Overall, 2,251 total hip arthroplasties (96 %) followed the protocol while 99 (4 %) did not.
Table 1.
Demographics of patients enrolled in the current study
| Demographic | Group A | Group B | Group C | Group D | Total |
|---|---|---|---|---|---|
| Number | 280 | 87 | 12 | 1971 | 2350 |
| Male/female | 34/246 | 25/62 | 5/7 | 931/1040 | 995 (42 %)/1355 (58 %) |
| Mean age (years) | 64.9 ± 15.0 (21–94) | 68.9 ± 14.0 (29–93) | 62.2 ± 12.0 (33–80) | 63.4 ± 12.0 (18–91) | 63.8 ± 12.0 (18–94) |
| Mean BMI (kg·m−2) | 23.0 ± 6.0 (12.8–44.8) | 23.1 ± 5.4 (13.1–39.0) | 24.4 ± 6.1 (17.5–28.6) | 25.5 ± 6.2 (11.7–51.5) | 25.1 ± 6.2 (11.7–51.5) |
No patient with a haemoglobin level less than 10 g/dL donated, and such patients usually have their procedures postponed until the anaemia is investigated and treated. Data were analysed using a standard two-tailed t test (Microsoft Excel, Microsoft Corporation, Redmond, WA, USA, Microsoft Office Professional Plus 2010 Version 14.0.6 for Windows 7). A p-value of less than 0.05 was considered statistically significant. No patients elected to drop out of the study at any time (Table 1).
Results
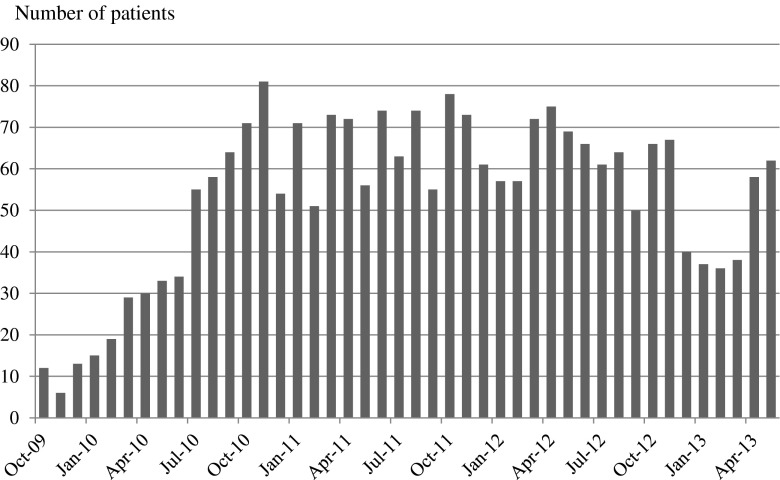
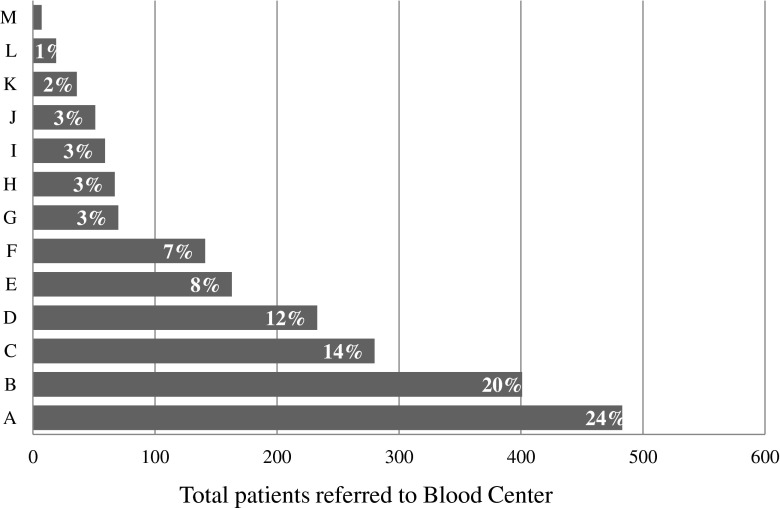
Over the three-year study period an increasing number of patients were enrolled by the Blood Preservation Center (Fig. 2). Significant variability could be observed among the different surgeons’ tendency to refer their patients to the Blood Preservation Center (Fig. 3).
Fig. 2.
Monthly distribution of number of procedures performed on patients who enrolled between October 2010 and May 2013
Fig. 3.
Number of cases referred to the Blood Preservation Center per surgeon from October 2010 till May 2013
Autologous blood donation significantly reduced the need for allogeneic blood in anaemic patients (13 % group A vs. 37 % group B; p < 0.001). Although it did increase overall transfusion rates among the patients who donated, the difference was not statistically significant (0.66/patient group A vs. 0.54/patient group B; p = 0.27). The allogeneic transfusion rate for non-anaemic patients in group D was low (8 %). Only 12 non-anaemic patients donated autologous blood (group C) and none of them required allogeneic blood (Table 2).
Table 2.
The average of any transfusion for patients who followed the targeted algorithm was found to be 0.17
| Pre-op | Number of THAs per group | THA procedures with autologous transfusion | THA procedures with allogeneic transfusion | Total allogeneic units | Average allogeneic transfusion per patient | Average overall transfusion per patient | Autologous units wasted |
|---|---|---|---|---|---|---|---|
| Anaemic | Group A (n = 280) | 140 (50 %) | 36 (13 %) | 44 | 0.16 | 0.66 | 50 % |
| Group B (n = 87) | 0 | 32 (37 %) | 47 | 0.54 | 0.54 | 0 | |
| Non-anaemic | Group C (n = 12) | 5 (42 %) | 0 | 0 | 0 | 0.42 | 58 % |
| Group D (n = 1,971) | 0 | 162 (8 %) | 206 | 0.10 | 0.10 | 0 |
Anaemic patients in groups A and B had similar discharge haemoglobin levels of 9.4 g/dL (range: 7.4 to 11.6 g/dL), with an average drop of 2.3 g/dL and 2.1 g/dL from pre-operative levels, respectively. In contrast, non-anaemic patients displayed an average drop in hemoglobin of 3.5 g/dL and were discharged with an average hemoglobin level of 10.6 g/dL (range: 8.4 to 14.5) g/dL). No significant difference in length of stay was detected between the different groups.
Discussion
Pre-operative autologous blood donation is appealing because it reduces the risk associated with allogeneic blood transfusions [11]. It has also been stipulated to precede surgical blood loss as a trigger for reticulocytosis [17]. However, the high percentage of wasted autologous blood in primary total joint arthroplasty has led surgeons to question its efficacy. A Cochrane review evaluated pre-operative donation in different surgical disciplines including orthopaedic procedures. The study revealed a 68 % reduction in exposure to allogeneic blood in the PABD group at the expense of a 24 % higher overall transfusion rate (allogeneic and/or autologous) [18]. This has been attributed to donation-induced anaemia as well as a tendency to transfuse autologous blood more liberally. The Orthopedic Surgery Transfusion Hemoglobin European Overview (OSTHEO) study examined transfusion practices involving 2,640 total hip and 1,305 total knee arthroplasty patients (including primary unilateral and bilateral procedures as well as revisions). Of the 49 % of patients who participated in PABD, 13 % subsequently received allogeneic transfusions [12].
The current study has a number of limitations. Strict transfusion guidelines were not enforced for autologous blood transfusions. The increase in blood volume during hypotensive anaesthesia likely has an effect on postoperative hemoglobin levels and might account for higher than expected transfusion rates in non-anaemic patients. Moreover, although the same surgical technique was used, the fact that multiple surgeons contributed to the patient series remains a possible source of bias.
Pre-operative haemoglobin levels are an important predictor for postoperative transfusion requirements [19]. Keating et al. showed that the application of a universal autologous donation protocol in patients with a haemoglobin greater than 13 g/dL resulted in 66 % of the blood being wasted [8]. Potential complications of autologous blood include bacterial contamination, febrile non-hemolytic transfusion reactions, and technical or clerical errors with the handling of samples. The benefit of PABD for non-anaemic patients undergoing primary unilateral total hip replacement has been questioned in the literature [16, 20, 21]. In light of the fact that the cost of donating, storing, and transfusing autologous blood is similar to that of allogeneic blood, the cost-efficacy of PABD is primarily a function of the number of units discarded [22].
In a previously published study, our centre compared overall transfusion rates between a routine PABD group and control group in which no patient donated, reporting 0.75 transfusions per patient versus 0.22, respectively [16]. The PABD group had a significantly higher overall transfusion rate. However, 11.8 % of the anaemic patients (Hb ≤ 12.5 g/dL) who donated autologous units received allogeneic blood transfusions, as opposed to 52.6 % of anaemic patients who did not donate. The study suggested maximizing the benefit and minimizing the cost of PABD by offering it to anaemic patients only. The present study supports these recommendations by showing that the implementation of target blood management is feasible in the private practice environment, although it is largely influenced by the surgeon’s dedication to enroll patients during the initial visit in the office. Ideally, pre-operative patient screening and autologous blood donation are handled independently of the surgeon’s office by the hospital as part of the routine pre-operative medical examination. The average transfusion per patient (autologous and allogeneic) for the groups that followed the protocol (groups A and D) was found to be 0.17 while the previously reported number was 0.75 with routine PABD for all patients. Among 2,251 patients who followed the protocol, only 140 patients (6 %) had their autologous blood wasted. This compares well to values reported in the literature ranging from 14 % [12] up to 50 % [5] (Fig. 3).
The overall transfusion rate in non-anaemic patients might be rather high compared to the literature suggesting that hypotensive anaesthesia has an impact on transfusion rates [15, 16]. In fact, Hb levels used as transfusion triggers were likely affected by the fluids administered intra-operatively to stabilize the blood pressure during hypotensive anaesthesia.
The results of the present study support the use of targeted autologous blood donation in patients undergoing primary THA. Several blood management modalities are available for use in total hip arthroplasty. Selecting patients at highest risk for postoperative transfusion maximizes the efficacy of pre-operative blood donation and significantly reduces the overall number of transfusions as well as the number of autologous units wasted as compared to a routine predonation protocol for all patients. Targeted PABD effectively reduces the need for allogeneic blood transfusion in anaemic patients.
Acknowledgments
The authors would like to thank Michele Prigo, MA, CHES, Coordinator of the Blood Preservation Center, for her effort in enrolling patients as well as the surgeon members of the blood preservation centre who changed their practice routine and enrolled patients into the protocol.
Members of the blood preservation center
Dr. Michael Alexiades, Dr. Mathias Bostrom, Dr. Charles Cornell, Dr. Alejandro Gonzales Della Valle, Dr. Mark Figgie, Dr. David Mayman, Dr. Douglas Padgett, Dr. Michael Parks, Dr. Amar Ranawat, Dr. Chitranjan Ranawat, Dr. Thomas Sculco, and Dr. Geoffrey Westrich
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Friedman R, Homering M, Holberg G, Berkowitz SD. Allogeneic blood transfusions and postoperative infections after total hip or knee arthroplasty. J Bone Joint Surg Am. 2014;96(4):272–278. doi: 10.2106/JBJS.L.01268. [DOI] [PubMed] [Google Scholar]
- 2.Newman ET, Watters TS, Lewis JS, Jennings JM, Wellman SS, Attarian DE, Grant SA, Green CL, Vail TP, Bolognesi MP. Impact of perioperative allogeneic and autologous blood transfusion on acute wound infection following total knee and total hip arthroplasty. J Bone Joint Surg Am. 2014;96(4):279–284. doi: 10.2106/JBJS.L.01041. [DOI] [PubMed] [Google Scholar]
- 3.Hatzidakis AM, Mendlick RM, McKillip T, Reddy RL, Garvin KL. Preoperative autologous donation for total joint arthroplasty. An analysis of risk factors for allogenic transfusion. J Bone Joint Surg Am. 2000;82(1):89–100. doi: 10.2106/00004623-200001000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Parvizi J, Chaudhry S, Rasouli MR, Pulido L, Joshi A, Herman JH, Rothman RH. Who needs autologous blood donation in joint replacement? J Knee Surg. 2011;24(1):25–31. doi: 10.1055/s-0031-1275404. [DOI] [PubMed] [Google Scholar]
- 5.Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am. 1999;81(1):2–10. doi: 10.2106/00004623-199901000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Salido JA, Marin LA, Gomez LA, Zorrilla P, Martinez C. Preoperative hemoglobin levels and the need for transfusion after prosthetic hip and knee surgery: analysis of predictive factors. J Bone Joint Surg Am. 2002;84-A(2):216–220. doi: 10.2106/00004623-200202000-00008. [DOI] [PubMed] [Google Scholar]
- 7.de Andrade JR, Jove M, Landon G, Frei D, Guilfoyle M, Young DC. Baseline hemoglobin as a predictor of risk of transfusion and response to Epoetin alfa in orthopedic surgery patients. Am J Orthop (Belle Mead NJ) 1996;25(8):533–542. [PubMed] [Google Scholar]
- 8.Keating EM, Meding JB, Faris PM, Ritter MA. Predictors of transfusion risk in elective knee surgery. Clin Orthop Relat Res. 1998;357:50–59. doi: 10.1097/00003086-199812000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Aggarwal AK, Shashikanth VS, Marwaha N. Platelet-rich plasma prevents blood loss and pain and enhances early functional outcome after total knee arthroplasty: a prospective randomised controlled study. Int Orthop. 2014;38(2):387–395. doi: 10.1007/s00264-013-2136-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buljan M, Nemet D, Golubic-Cepulic B, Bicanic G, Tripkovic B, Delimar D. Two different dosing regimens of human recombinant erythropoietin beta during preoperative autologous blood donation in patients having hip arthroplasty. Int Orthop. 2012;36(4):703–709. doi: 10.1007/s00264-011-1367-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Munoz M, Garcia-Erce JA, Villar I, Thomas D. Blood conservation strategies in major orthopaedic surgery: efficacy, safety and European regulations. Vox Sang. 2009;96(1):1–13. doi: 10.1111/j.1423-0410.2008.01108.x. [DOI] [PubMed] [Google Scholar]
- 12.Rosencher N, Kerkkamp HE, Macheras G, Munuera LM, Menichella G, Barton DM, Cremers S, Abraham IL. Orthopedic Surgery Transfusion Hemoglobin European Overview (OSTHEO) study: blood management in elective knee and hip arthroplasty in Europe. Transfusion. 2003;43(4):459–469. doi: 10.1046/j.1537-2995.2003.00348.x. [DOI] [PubMed] [Google Scholar]
- 13.Sharrock NE, Salvati EA. Hypotensive epidural anesthesia for total hip arthroplasty: a review. Acta Orthop Scand. 1996;67(1):91–107. doi: 10.3109/17453679608995620. [DOI] [PubMed] [Google Scholar]
- 14.Sukeik M, Alshryda S, Haddad FS, Mason JM. Systematic review and meta-analysis of the use of tranexamic acid in total hip replacement. J Bone Joint Surg. 2011;93(1):39–46. doi: 10.1302/0301-620X.93B1.24984. [DOI] [PubMed] [Google Scholar]
- 15.Millett PJ, Porramatikul M, Chen N, Zurakowski D, Warner JJ. Analysis of transfusion predictors in shoulder arthroplasty. J Bone Joint Surg Am. 2006;88(6):1223–1230. doi: 10.2106/JBJS.E.00706. [DOI] [PubMed] [Google Scholar]
- 16.Boettner F, Altneu EI, Williams BA, Hepinstall M, Sculco TP (2009) Nonanemic patients do not benefit from autologous blood donation before total hip replacement. HSS J 6(1):66–70. doi:10.1007/s11420-009-9145-4 [DOI] [PMC free article] [PubMed]
- 17.Sculco TP. Global blood management in orthopaedic surgery. Clin Orthop Relat Res. 1998;357:43–49. doi: 10.1097/00003086-199812000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Henry DA, Carless PA, Moxey AJ, O’Connell D, Forgie MA, Wells PS, Fergusson D (2002) Pre-operative autologous donation for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev (2):CD003602. doi:10.1002/14651858.CD003602 [DOI] [PMC free article] [PubMed]
- 19.Callaghan JJ, Spitzer AI. Blood management and patient specific transfusion options in total joint replacement surgery. Iowa Orthop J. 2000;20:36–45. [PMC free article] [PubMed] [Google Scholar]
- 20.Billote DB, Glisson SN, Green D, Wixson RL. A prospective, randomized study of preoperative autologous donation for hip replacement surgery. J Bone Joint Surg Am. 2002;84-A(8):1299–1304. doi: 10.2106/00004623-200208000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Jakovina Blazekovic S, Bicanic G, Hrabac P, Tripkovic B, Delimar D. Pre-operative autologous blood donation versus no blood donation in total knee arthroplasty: a prospective randomised trial. Int Orthop. 2014;38(2):341–346. doi: 10.1007/s00264-013-2185-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Etchason J, Petz L, Keeler E, Calhoun L, Kleinman S, Snider C, Fink A, Brook R. The cost effectiveness of preoperative autologous blood donations. N Engl J Med. 1995;332(11):719–724. doi: 10.1056/NEJM199503163321106. [DOI] [PubMed] [Google Scholar]