Abstract
Purpose
For femoral neck fractures, recent scientific evidence supports cemented hemiarthroplasty (HA) over uncemented HA and suggests that total hip arthroplasty (THA) should be performed more frequently. We report the current surgical trends in treating femoral neck fractures in Finland.
Methods
The study was conducted using the Finnish National Hospital Discharge Register and included all Finns at least 50 years of age who underwent surgery for femoral neck fractures from 1998 through 2011. Age- and sex-specific incidence rates and annual proportion of each treatment method were calculated.
Results
During 1998–2011, a total of 49,514 operations for femoral neck fracture were performed in Finland. The proportion of uncemented HA increased from 8.1 % in 2005 to 22.2 % in 2011. During the same time, the proportion of cemented HA decreased from 63.9 to 52.5 %, internal fixation decreased from 23.2 to 16.1 % and THA increased from 4.9 to 9.2 %.
Conclusions
Between 2005 and 2011, the proportion of uncemented HA for femoral neck fractures increased markedly in Finland, while cemented HA and internal fixation declined. During this time, the use of THA nearly doubled. The current evidence-based guidelines for treatment of femoral neck fractures were mainly followed, but the increase in uncemented HA procedures contradicts recent scientific evidence.
Keywords: Hip fracture, Population-based, Treatment, Internal fixation, Arthroplasty
Introduction
Hip fractures are a common injury in elderly adults leading to increased mortality, loss of function and consumption of social and community health care services [1, 2]. Approximately 7,500 persons sustain hip fractures annually in Finland. Based on a recent Finnish study, the age-adjusted incidence of hip fracture has continuously declined, especially in women, but the rapid ageing of the population will result in an increase in the total number of hip fractures in the near future [3]. Based on a Scandinavian study, femoral neck fractures represent 60 % of all hip fractures [4].
Treatment of femoral neck fracture is aimed at normal ambulation without weight-bearing restrictions. Non-displaced or impacted (Garden I or II) fractures should be stabilised surgically, because without fixation there is a 12–33 % risk of fracture displacement prior to healing [5–7]. Desirable reduction and internal fixation reduce this risk to approximately 5 %, thus clearly supporting surgical treatment [8]. For non-displaced femoral neck fractures, hemiarthroplasty (HA) is associated with increased mortality and a higher complication rate compared with internal fixation [9].
Arthroplasty and internal fixation also represent possible surgical methods for the treatment of displaced femoral neck fractures (Garden III or IV). The literature supports the use of the former method; in patients older than 60 years, HA reportedly results in fewer re-operations compared with internal fixation [10]. HA is also the most cost-effective surgical treatment available [11].
Cemented HA is associated with better mobility and less pain compared with traditional uncemented HA [12]. A recently published randomised trial regarding a modern uncemented stem had the same visual analogue scale score for cemented vs uncemented HA, but a higher Oxford Hip Score and less pain in flexion to 45° for a cemented stem at six weeks after surgery [13]. In addition, the uncemented stem was also associated with an increased number of intra- and post-operative fractures during the two year follow-up. In contrast, another recent randomised trial between cemented and uncemented HA showed no difference in mortality, disposition or need for assistance with ambulation during a one year follow-up [14].
A patient’s physiological age and an assessment of physical health and previous activity level may be more important than chronological age in the decision-making between different surgical treatment options for femoral neck fractures [15]. Clearly, HA is the most common procedure performed for the treatment of displaced femoral neck fractures. Recent data, however, suggest that total hip arthroplasty (THA) is a better alternative for previously independent and healthy subjects [16, 17].
As noted above, four surgical treatment options are available for patients with a femoral neck fracture (internal fixation, cemented HA, uncemented HA and THA), but the optimal approach remains under debate. The aim of this study was to assess the incidence of surgical procedures for femoral neck fractures in Finland and to evaluate whether the proportions of different treatment methods have changed from 1998 through 2011.
Materials and methods
For the purpose of this study, data on femoral neck fracture patients were obtained from the Finnish National Hospital Discharge Register (NHDR). The Finnish NHDR is a mandatory national register for all hospitals encompassing private, public and other institutions. The data in the NHDR includes variables such as patient identification number; sex; domicile of the subject; duration and type of hospital stay; external cause for injury; primary, secondary and tertiary diagnosis; and all procedures performed during the stay. The coverage and accuracy of the NHDR injury data are excellent [18, 19].
In this study, all patients 50 years of age or older with femoral neck fracture code S72.0 (10th version of International Classification of Diseases, ICD-10, 1994) and valid surgical procedure code between 1 January 1998 and 31 December 2011 were included. The surgical procedures were identified by using the Finnish version of the Nordic Medico-Statistical Committee (NOMESCO) Classifications’ procedure codes and the following procedures were established: uncemented HA, cemented HA, THA and internal fixation (Table 1).
Table 1.
The procedure (NOMESCO) codes used in the study
| Code | Procedure |
|---|---|
| NFB10 | Primary partial prosthetic replacement of hip joint not using cement |
| NFB20 | Primary partial prosthetic replacement of hip joint using cement |
| NFB30 | Primary total prosthetic replacement of hip joint not using cement |
| NFB40 | Primary total prosthetic replacement of hip joint using hybrid technique |
| NFB50 | Primary total prosthetic replacement of hip joint using cement |
| NFJ50 | Internal fixation of fracture of neck of femur with nail or screw |
| NFJ52 | Internal fixation of fracture of upper femur with screws and side plate |
| NFJ54 | Internal fixation of fracture of upper femur with intramedullary nail |
| NFJ64 | Other internal fixation of other parts of femur |
To calculate the incidence ratios of surgically treated femoral neck fractures, the annual mid-population of Finland was obtained from the Official Statistics of Finland, a statutory electronic population register of the country. The rates of surgically treated femoral neck fractures (per 100,000 persons) were based on the entire adult (50-year-old and older) population of Finland rather than sample- or cohort-based estimates and thus 95 % confidence intervals were not calculated. The population was categorised into five age-based classes (50–59, 60–69, 70–79, 80–89 and ≥90) for further analyses. No exclusion criteria were used other than age under 50 years. Statistical analyses were performed using IBM SPSS Statistics version 21.
Results
During the study period between 1998 and 2011, a total of 49,514 patients 50 years of age and older underwent surgery for femoral neck fracture. The mean patient age was 79.2 years (range 50–106) and 35,376 of them (71.4 %) were women. Patients aged 80–89 years comprised the largest group (21,822; 44.1 %). During the entire study period, the most common surgical procedure was cemented HA (28,613; 57.8 %), followed by internal fixation (11,189; 22.6 %), uncemented HA (6618; 13.4 %) and THA (3094; 6.2 %).
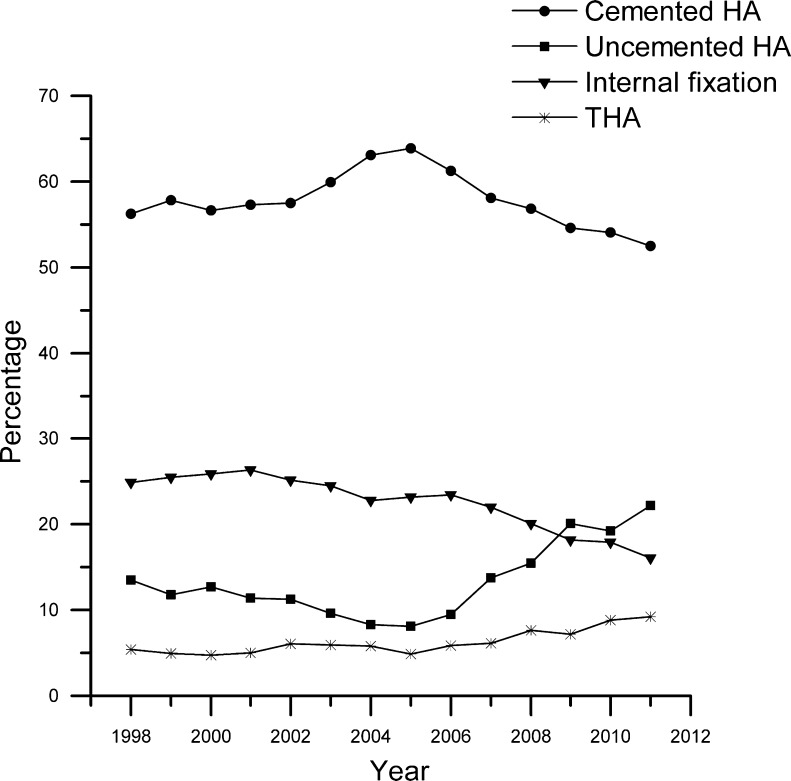
From 1998 through 2005, there was a modest decline in uncemented HA procedures (from 13.5 to 8.1 %) and a slight increase in cemented HA procedures (from 56.2 to 63.9 %). No major changes were noted in internal fixation (from 24.9 to 23.2 %) or THA (from 5.4 to 4.9 %) procedures during the same time period (Fig. 1).
Fig. 1.
Percentage distribution of femoral neck fracture procedures in Finland from 1998 through 2011. HA hemiarthroplasty, THA total hip arthroplasty
From 2005 through 2011, the proportions of uncemented HA and THA procedures increased from 8.1 to 22.2 % and from 4.9 to 9.2 %, respectively. In contrast, the proportions of cemented HA and internal fixation procedures decreased from 63.9 to 52.5 % and 23.2 to 16.1 %, respectively (Fig. 1).
Age-specific results from 1998 through 2011
A separate analysis of the youngest age group (50–59 years) revealed only minor changes in the use of uncemented HA and cemented HA. The proportion of internal fixation procedures, however, declined from 62.9 to 40.3 %, while the proportion of THA procedures increased from 15.7 to 29.6 %. No marked changes occurred in the proportion of uncemented HA (from 6.3 to 9.7 %) or cemented HA (from 15.1 to 20.4 %) procedures.
Persons aged 60–69 years showed a substantial proportional decline in internal fixation (from 39.2 to 23.7 %) and an increase in THA (from 14.1 to 29.9 %). The proportions of cemented HA (from 38.1 to 34.3 %) and uncemented HA (from 8.6 to 12.1 %) remained unaltered.
In patients 70–79 years of age, there was an increase in the proportions of uncemented HA procedures from 14.6 to 24.1 % and in THA procedures from 6.3 to 11.4 %, whereas there was a decrease in cemented HA procedures from 55.2 to 47.0 % and in internal fixation from 23.9 to 17.5 %.
In patients aged 80–89 years, uncemented HA procedures nearly doubled from 14.4 to 25.3 %, while there were no marked changes in cemented HA (from 63.0 to 60.1 %) and THA (from 2.5 to 2.9 %) procedures. Internal fixation was used less frequently in 2011 (11.8 %) than in 1998 (20.2 %).
In the oldest age group (90+ years), there was a moderate increase in uncemented HA from 14.5 to 21.4 % and a decrease in internal fixation from 16.6 to 12.2 %. The incidence of cemented HA (from 67.4 to 64.6 %) and THA (from 1.5 to 1.7 %) procedures did not change markedly.
Discussion
Our nationwide study showed that the proportion of uncemented HA procedures for the treatment of femoral neck fractures increased nearly threefold from 8.1 to 22.2 % from 2005 to 2011, while the proportion of cemented HA procedures declined. The increased proportion of uncemented HA procedures was mainly due to the increase in patients over 70 years of age. This finding is interesting, although not consistent with the evidence from previous randomised controlled trials favouring cemented HA. The reason for the shift from cemented HA to uncemented HA procedures remains unknown. We may speculate that the shorter operation time and reduced cardiovascular effects associated with uncemented HA are contributing factors to this shift [20, 21]. Better implant availability and more active marketing systems for modern uncemented stems may have also contributed to the change.
Accumulating evidence indicates that assessment of a patient’s physiological age is essential in deciding between the procedures [15]. A patient’s medical co-morbidities and previous activity level should also be taken into account. Each procedure has limitations and its own spectrum of complications, and some complications are associated with poor bone quality and osteoporosis. In the case of an old fragile patient with a non-displaced femoral neck fracture, the surgeon must choose between internal fixation and HA. In chronologically or physiologically young patients, internal fixation should be used to retain the indigenous hip joint, especially in previously symptomless patients.
In cases of displaced femoral neck fracture, patient characteristics are important. In a prospective study of 60 cognitively impaired patients older than 70 years, displaced femoral neck fractures treated by cemented HA provided a safe option with better health-related quality of life and less risk for re-operation compared to internal fixation [22]. A recent randomised controlled trial revealed that HA has predictable and good long-term results after femoral neck fracture and is the treatment of choice compared with internal fixation [23]. In displaced fractures, results of HA in the worst cases have been reported to be better than those of internal fixation in the best cases [24]. While younger healthy patients should be treated with internal fixation or THA to avoid further complications related to HA over time, older fragile patients who have significant medical co-morbidities should be treated with HA [25].
HA is the most common treatment for displaced femoral neck fractures in elderly adults. The Cochrane Review published in 2010 concluded that patients with cemented HA experienced less pain at one year or later and had improved post-operative mobility compared with patients having uncemented HA, while mortality and surgical complications were not significantly different between these groups [26]. A recent systematic review concluded that cemented HA reduces the risk of residual pain and provides better functional outcomes [27]. Furthermore, cemented HA was not associated with higher mortality, re-operation or complications. Also, the latest meta-analysis concluded that the available evidence indicates that cemented HA procedures can achieve better hip function, lower residual pain and less implant-related complications with no increased risk of mortality, cardiovascular and cerebrovascular complications, general complications, local complications or re-operation rate in elderly patients with femoral neck fractures [28]. A point worth noting, however, is that most of the randomised controlled trials included in the systematic review and meta-analysis were conducted using traditional uncemented stems and thus the results cannot be directly generalised to the newer stems.
Recently published randomised trials provide somewhat contradictory answers to the question of whether to use cemented or uncemented implants. A five year follow-up of a randomised trial with modern stems demonstrated a higher hip score for uncemented HA, but also increased risk of later femoral fractures [29]. Furthermore, two randomised controlled trials conducted by comparing modern uncemented and cemented stems concluded that both methods lead to equivalent functional results [14, 21]. In patients 70 years or older, uncemented and cemented HAs were comparable with regard to pain, but implant-related complications were significantly lower in patients treated with cemented HA [13]. Thus, according to the latest available data, we suggest that functional outcomes of modern-design uncemented and cemented stems are similar, but implant-related complications are higher in uncemented HA.
Another important finding was the increased use of THA for the treatment of femoral neck fracture from 4.9 to 9.2 %. This increase was especially observable in younger patients aged 50–69 years. In patients 80 years of age or older, there was no such change. A recent meta-analysis revealed no difference in mortality, infections or general complications between patients undergoing HA and THA, but demonstrated a significant increase in the dislocation rate for THA. Based on the evidence, patients may benefit from THA compared with HA, despite an increased dislocation rate [17, 30]. The latest systematic review indicated that THA may lead to better patient-related outcomes in fit patients, but has a higher dislocation rate compared to HA [16].
Our data showed an increased use of THA for femoral neck fractures, especially in younger patients. At the same time, internal fixation became less popular. It appears that active young patients should be treated with internal fixation especially in cases of non-displaced fractures, but poor reduction and posteroinferior displacement of the femoral head increase the rate of nonunion [31]. Therefore, THA may have a role in the treatment of femoral neck fractures in younger age groups if the fracture is highly displaced and the potential for anatomic reduction with suitable internal fixation is excluded.
Our third finding showed a decrease in use of internal fixation from 24.9 to 16.1 % annually from 1998 to 2011. Patients aged 50–79 years accounted for the major decrease in the incidence and proportion of internal fixation procedures. Thus, internal fixation has limitations for femoral neck fracture treatment, especially in older adults. First, elderly patients with osteoporosis and poor bone quality demonstrate a higher risk of nonunion [32]. Second, internal fixation is an appropriate treatment method for non-displaced Garden I and II femoral neck fractures only [33]. Third, complication and re-operation rates are markedly higher in older patients treated with internal fixation [33–35]. It is unclear why the trend toward internal fixation procedures is decreasing, especially in younger patients. We suspect that the improved THA survivorship and the potential risk of early re-operation related to internal fixation play a role.
A limitation of our study was that we were not able to assess a detailed classification of the femoral neck fractures or patients’ physical activity. Thus, we could draw no conclusion about whether the surgical method or implant used was according to current treatment concepts. A major strength of the study was that true nationwide data were used, as medical treatment in Finland is equally available to everyone and the study population comprised the entire Finnish adult population over the age of 50 years. Thus, with coverage of an entire country, including all hospitals, the changes in the trends of a treatment method obviously represent the general opinion of all actively practising orthopaedic surgeons in Finland. A second strength was that during the study period there were no changes in diagnostics, ICD coding or hospital registry. Finally, another strength of this study is that the coverage and accuracy of the NHDR injury codes are excellent [18, 19].
In conclusion, the age-adjusted incidence and proportion of uncemented HA procedures performed for femoral neck fractures increased considerably in Finland between 2005 and 2011, whereas the use of cemented HA and internal fixation procedures declined during the same period. During the same period, the use of THA nearly doubled, although the procedure was yet rather uncommon in 2011. Thus, the current evidence-based guidelines for treatment of femoral neck fractures were mainly followed in Finland, although the increased use of uncemented HA contradicts recent scientific evidence.
Acknowledgments
This study was supported by the Competitive State Research Financing of Seinäjoki Central Hospital, grant number VTR 111.
Conflict of interest
The authors declare that they have no conflict of interest.
Contribution of authors
MH and VM were in charge and contributed to all stages of the study. SN contributed to the data interpretation. MN contributed to writing the final manuscript. PK and HP contributed to the study design, data collection, data interpretation and writing the final manuscript. All authors read and approved the final manuscript.
References
- 1.Diamantopoulos AP, Hoff M, Skoie IM, et al. Short- and long-term mortality in males and females with fragility hip fracture in Norway. A population-based study. Clin Interv Aging. 2013;8:817–823. doi: 10.2147/CIA.S45468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nikitovic M, Wodchis WP, Krahn MD, Cadarette SM. Direct health-care costs attributed to hip fractures among seniors: a matched cohort study. Osteoporos Int. 2013;24:659–669. doi: 10.1007/s00198-012-2034-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Korhonen N, Niemi S, Parkkari J, et al. Continuous decline in incidence of hip fracture: nationwide statistics from Finland between 1970 and 2010. Osteoporos Int. 2013;24:1599–1603. doi: 10.1007/s00198-012-2190-8. [DOI] [PubMed] [Google Scholar]
- 4.Lönnroos E, Kautiainen H, Karppi P, et al. Increased incidence of hip fractures. A population based-study in Finland. Bone. 2006;39:623–627. doi: 10.1016/j.bone.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 5.Garden RS. Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg Br. 1961;43:647–666. [Google Scholar]
- 6.Bentley G. Treatment of nondisplaced fractures of the femoral neck. Clin Orthop Relat Res. 1980;152:93–101. [PubMed] [Google Scholar]
- 7.Holmberg S, Kalén R, Thorngren KG. Treatment and outcome of femoral neck fractures. An analysis of 2418 patients admitted from their own homes. Clin Orthop Relat Res. 1987;218:42–52. [PubMed] [Google Scholar]
- 8.Conn KS, Parker MJ. Undisplaced intracapsular hip fractures: results of internal fixation in 375 patients. Clin Orthop Relat Res. 2004;421:249–254. doi: 10.1097/01.blo.0000119459.00792.c1. [DOI] [PubMed] [Google Scholar]
- 9.Parker MJ, White A, Boyle A. Fixation versus hemiarthroplasty for undisplaced intracapsular hip fractures. Injury. 2008;39:791–795. doi: 10.1016/j.injury.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 10.Rogmark C, Johnell O. Primary arthroplasty is better than internal fixation of displaced femoral neck fractures: a meta-analysis of 14 randomized studies with 2,289 patients. Acta Orthop. 2006;77:359–367. doi: 10.1080/17453670610046262. [DOI] [PubMed] [Google Scholar]
- 11.Waaler Bjørnelv GM, Frihagen F, Madsen JE, et al. Hemiarthroplasty compared to internal fixation with percutaneous cannulated screws as treatment of displaced femoral neck fractures in the elderly: cost-utility analysis performed alongside a randomized, controlled trial. Osteoporos Int. 2012;23:1711–1719. doi: 10.1007/s00198-011-1772-1. [DOI] [PubMed] [Google Scholar]
- 12.Parker MI, Pryor G, Gurusamy K. Cemented versus uncemented hemiarthroplasty for intracapsular hip fractures: a randomised controlled trial in 400 patients. J Bone Joint Surg Br. 2010;92:116–122. doi: 10.1302/0301-620X.92B1.22753. [DOI] [PubMed] [Google Scholar]
- 13.Taylor F, Wright M, Zhu M. Hemiarthroplasty of the hip with and without cement: a randomized clinical trial. J Bone Joint Surg Am. 2012;94:577–583. doi: 10.2106/JBJS.K.00006. [DOI] [PubMed] [Google Scholar]
- 14.DeAngelis JP, Ademi A, Staff I, Lewis CG. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: a prospective randomized trial with early follow-up. J Orthop Trauma. 2012;26:135–140. doi: 10.1097/BOT.0b013e318238b7a5. [DOI] [PubMed] [Google Scholar]
- 15.Lowe JA, Crist BD, Bhandari M, Ferguson TA. Optimal treatment of femoral neck fractures according to patient’s physiologic age: an evidence-based review. Orthop Clin North Am. 2010;41:157–166. doi: 10.1016/j.ocl.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 16.Burgers PTPW, Van Geene AR, Van den Bekerom MPJ, et al. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures in the healthy elderly: a meta-analysis and systematic review of randomized trials. Int Orthop. 2012;36:1549–1560. doi: 10.1007/s00264-012-1569-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yu L, Wang Y, Chen J. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures: meta-analysis of randomized trials. Clin Orthop Relat Res. 2012;470:2235–2243. doi: 10.1007/s11999-012-2293-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mattila VM, Sillanpää P, Iivonen T, et al. Coverage and accuracy of diagnosis of cruciate ligament injury in the Finnish National Hospital Discharge Register. Injury. 2008;39:1373–1376. doi: 10.1016/j.injury.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 19.Sund R. Quality of the Finnish Hospital Discharge Register: a systematic review. Scand J Public Health. 2012;40:505–515. doi: 10.1177/1403494812456637. [DOI] [PubMed] [Google Scholar]
- 20.Parvizi J, Holiday AD, Ereth MH, Lewallen DG. The Frank Stinchfield Award. Sudden death during primary hip arthroplasty. Clin Orthop Relat Res. 1999;369:39–48. doi: 10.1097/00003086-199912000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Figved W, Opland V, Frihagen F, et al. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures. Clin Orthop Relat Res. 2009;467:2426–2435. doi: 10.1007/s11999-008-0672-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hedbeck C-J, Inngul C, Blomfeldt R, et al. Internal fixation versus cemented hemiarthroplasty for displaced femoral neck fractures in patients with severe cognitive dysfunction: a randomized controlled trial. J Orthop Trauma. 2013;27:690–695. doi: 10.1097/BOT.0b013e318291f544. [DOI] [PubMed] [Google Scholar]
- 23.Støen RØ, Lofthus CM, Nordsletten L, et al. Randomized trial of hemiarthroplasty versus internal fixation for femoral neck fractures: no differences at 6 years. Clin Orthop Relat Res. 2014;472:360–367. doi: 10.1007/s11999-013-3245-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bjørgul K, Reikerås O. Hemiarthroplasty in worst cases is better than internal fixation in best cases of displaced femoral neck fractures: a prospective study of 683 patients treated with hemiarthroplasty or internal fixation. Acta Orthop. 2006;77:368–374. doi: 10.1080/17453670610046271. [DOI] [PubMed] [Google Scholar]
- 25.Inngul C, Hedbeck C-J, Blomfeldt R, et al. Unipolar hemiarthroplasty versus bipolar hemiarthroplasty in patients with displaced femoral neck fractures. A four-year follow-up of a randomised controlled trial. Int Orthop. 2013;37:2457–2464. doi: 10.1007/s00264-013-2117-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parker MJ, Gurusamy KS, Azegami S (2010) Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev 6:CD001706. doi:10.1002/14651858.CD001706.pub4 [DOI] [PubMed]
- 27.Luo X, He S, Li Z, Huang D. Systematic review of cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures in older patients. Arch Orthop Trauma Surg. 2011;132:455–463. doi: 10.1007/s00402-011-1436-9. [DOI] [PubMed] [Google Scholar]
- 28.Li T, Zhuang Q, Weng X, et al. Cemented versus uncemented hemiarthroplasty for femoral neck fractures in elderly patients: a meta-analysis. PLoS One. 2013;8:e68903. doi: 10.1371/journal.pone.0068903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Langslet E, Frihagen F, Opland V, et al. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: 5-year followup of a randomized trial. Clin Orthop Relat Res. 2014;472:1291–1299. doi: 10.1007/s11999-013-3308-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bensen AS, Jakobsen T, Krarup N. Dual mobility cup reduces dislocation and re-operation when used to treat displaced femoral neck fractures. Int Orthop. 2014 doi: 10.1007/s00264-013-2276-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Upadhyay A, Jain P, Mishra P, et al. Delayed internal fixation of fractures of the neck of the femur in young adults. A prospective, randomised study comparing closed and open reduction. J Bone Joint Surg Br. 2004;86:1035–1040. doi: 10.1302/0301-620X.86B7.15047. [DOI] [PubMed] [Google Scholar]
- 32.Hedström M. Are patients with a nonunion after a femoral neck fracture more osteoporotic than others? BMD measurement before the choice of treatment? A pilot study of hip BMD and biochemical bone markers in patients with femoral neck fractures. Acta Orthop Scand. 2004;75:50–52. doi: 10.1080/00016470410001708090. [DOI] [PubMed] [Google Scholar]
- 33.Murphy DK, Randell T, Brennan KL, et al. Treatment and displacement affect the reoperation rate for femoral neck fracture. Clin Orthop Relat Res. 2013;471:2691–2702. doi: 10.1007/s11999-013-3020-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dai Z, Li Y, Jiang D. Meta-analysis comparing arthroplasty with internal fixation for displaced femoral neck fracture in the elderly. J Surg Res. 2011;165:68–74. doi: 10.1016/j.jss.2009.03.029. [DOI] [PubMed] [Google Scholar]
- 35.Viberg B, Overgaard S, Lauritsen J, Ovesen O. Lower reoperation rate for cemented hemiarthroplasty than for uncemented hemiarthroplasty and internal fixation following femoral neck fracture: 12- to 19-year follow-up of patients aged 75 years or more. Acta Orthop. 2013;84:254–259. doi: 10.3109/17453674.2013.792033. [DOI] [PMC free article] [PubMed] [Google Scholar]