Abstract
Purpose
In order to prevent recurrent deformity, overcorrection in Blount’s disease has been a common practice by most paediatric orthopaedic surgeons. However, some patients have persistent valgus alignment resulting in awkward deformity. The femoro-tibial angle (FTA) was measured in this series of cases to determine the necessity of such practice.
Method
During 1998–2010, patients with Blount’s disease stage 2 by Langenskiold, aged from 30 to 40 months who had failed from bracing and underwent valgus osteotomy were included. Seventeen legs had postoperative FTA 7–13° (group 1) and 48 legs had postoperative FTA more than 13° (group 2). ROC curve was used to determine the appropriate FTA that was suitable to prevent recurrence.
Results
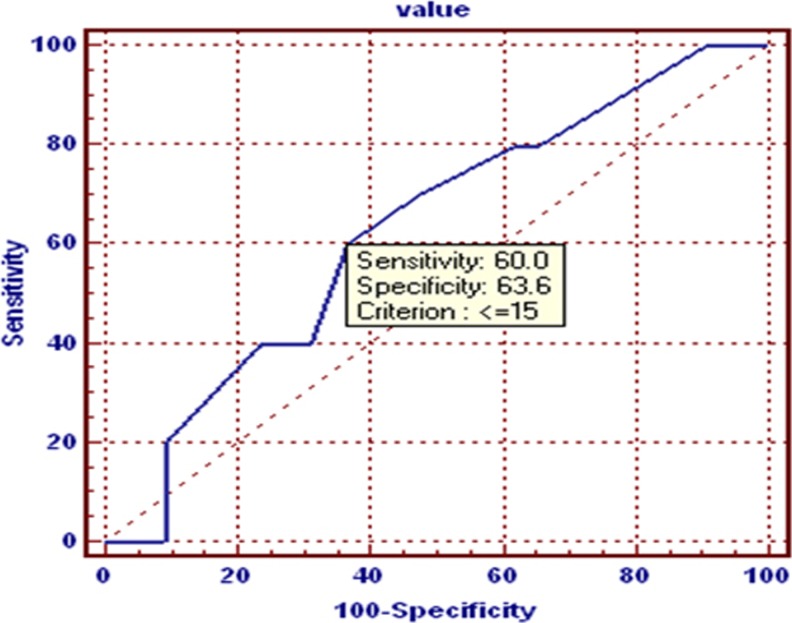
Four legs had recurrence (28.6 %) in group 1 and six legs (12.5 %) had recurrence in group 2. Chi-square test between two groups were not statistically significant in recurrence (p = 0.434). Age and BMI were not statistically significant between recurrent and non-recurrent groups. The ROC curve shows that overcorrection more than 15° did not show benefit to prevent the recurrence in Blount’s stage 2.
Conclusion
Our study showed that the overcorrection group had non-statistically significant recurrence compared to the non-overcorrection group, and overcorrection more than valgus 15° has no benefit to prevent recurrence.
Keywords: Blount’s disease, Corrective valgus osteotomy, Recurrence, Langenskiöld
Introduction
Early treatment of infantile Blount disease generally includes bracing, although the effectiveness of bracing continues to be controversial [1]. Surgical management is recommended if the correction by bracing does not occur [2]. Currently, the recommendation of progressive infantile Blount disease is a proximal tibial osteotomy. Excessive valgus position of the osteotomy is primarily used [3, 8]. This position minimizes the compression force across the disorganized physis and provides time for normal growth to resume. In a best-case scenario, symmetrical growth would resume when the tibia is back in physiological alignment. The degree of overcorrection is determined by the surgeon’s judgment, but it is generally 5–10° more valgus angulation than in the normal child’s age. Overcorrection in such cases could cause persistent or even increase in the valgus deformity. The recurrence of Blount’s disease is diagnosed when the FTA is more than 10° varus at the follow up. A mechanical axis of greater than 10° of varus creates force on the medial side of the knee joint and probably predisposes the patient to early osteoarthritis. Tibial realignment is usually recommended for these patients.
Early surgical intervention during initial stages of the disease will decrease incidence of recurrence of deformity and decreased symptoms and knee pathology at skeletal maturity. Blount [5] and Langenskiöld [10] both stated that, if performing correction of the varus deformity to a physiologic valgus position before the age of eight years in Langenskiöld stages I–IV would result in permanent cure for the patient. More recent reports by Smith [6], Hofmann et al. [7], Schoenecker et al. [8], Ferriter and Shapiro [9] noted a varying frequency of recurrence of varus deformity after initial surgery and suggested that surgical correction should be performed at an early age.
The corrective osteotomy performed in children at more than three years of age and Langenskiold stage 3 have high rate of recurrence. In this study we selected children with Langenskiold stage 2 who had failed from conservative treatment. In Blount disease, recurrent deformity can still occur regardless of initially successful surgery [11, 13, 16–18]. It is currently unknown whether overcorrection into valgus as is recommended would prevent this problem. Causes of recurrent varus are probably multifactorial and can be also associated with increasing obesity, age and staging. The main purpose of this study was to examine the correlation of recurrence and the degree of surgical correction. Another purpose was to find the proper degrees for overcorrection which could prevent the recurrence.
Materials and methods
After approved by the hospital research ethical committee, the charts and radiographs of 65 legs diagnosed with Blount disease stage 2 by Langenskiöld who had failed from brace treatment between 1998 and 2010 were reviewed. Children included in the data collection did not have any other orthopaedic or medical problems that were related to their lower extremities, no previous treatment, and had at least four years follow-up visit with full-length lower extremity radiographs. There were 38 patients, of which 27 were bilateral and 11 unilateral. The surgical procedures were Dome osteotomy of the proximal tibia and fibula in all patients. The patient age, sex, BMI, affected side, Langenskiöld stage, pre- and postoperative FTA, FTA of every visit, MDA (metaphyseal-diaphyseal angle) and method of treatment were recorded. Initial radiograph of the lower extremity was classified by Langenskiöld staging [10]. The FTA at the time of initial correction and every follow up were measured. Full-length standing anteroposterior (AP) radiographs of bilateral lower extremities, standing AP and lateral radiographs of bilateral knees were obtained. The mechanical axis and FTA were calculated from full-length standing AP. Degenerative articular changes were noted. Initial and final alignment were recorded for each osteotomy. The charts were reviewed for complications. FTA and MDA [4] were measured on serial long–leg standing radiographs to determine the pre-operative degree of deformity and subsequent recurrence after follow up. Care was taken to rotate the limbs while standing so that a true anterior-posterior radiograph of the knee could been taken despite tibial torsion being present. Although this assignment was made, we recognized that there were problems with reproducibility with this stage. In this series we determined the recurrence of varus deformity as FTA more than 10°. Data analysed by using ROC curve (receiver operating characteristic) and chi-square with P < 0.05 were considered significant.
Results
The patients were divided into two groups based on postoperative femorotibial angle (FTA). Group 1 (17 osteotomies) had postoperative FTA valgus from 7 to 13°, and group 2 (48 osteotomies) had postoperative FTA valgus more than 13°. The mean pre-operative MDA was 17.5 + 4.4 in group 1 and 17.4 + 4.4 in group 2 (p value 0.938). The mean pre-operative FTA was 19.5 + 6.2 in group 1 and 16.1 + 4.6 in group 2 (p value 0.022). BMI was 27.7 ± 4.6 in group 1 and 24.9 ± 4.6 in group 2 (p value 0.035) . The average age of the patients at surgery was 34 months (range 30–40 months). All patients were Langenskiöld stage 2 (Tables 1 and 2).
Table 1.
Results of statistical analysis between recurrence and non-recurrence groups
| Patient characteristics | No recurrence (n = 55) | Recurrence (n = 10) | p-value |
|---|---|---|---|
| Age | 2.2 ± 0.4 | 2.3 ± 0.5 | 0.615 |
| BMI | 25.8 ± 4.9 | 24.6 ± 3.8 | 0.448 |
| Height | 93.3 ± 8.2 | 95.2 ± 10.0 | 0.532 |
| Weight | 22.7 ± 6.2 | 23.1 ± 9.2 | 0.859 |
Table 2.
Statistical analysis between two groups
| Patient characteristics | Group1 | Group 2 | P value |
|---|---|---|---|
| Age (years) | 2.2 ± 0.4 | 2.3 ± 0.4 | 0.710 |
| BMI (kg/m2) | 27.7 ± 4.6 | 24.9 ± 4.6 | 0.035 |
| Recurrence (number %) | 4 (23.5 %) | 6 (12.5 %) | 0.434 |
| FTA (pre-op) | 19.5 ± 6.2 | 16.1 ± 4.6 | 0.022 |
| MDA (pre-op) | 17.5 ± 4.4 | 17.4 ± 4.4 | 0.938 |
| FTA F/U 2 months (post-op) | 8.3 ± 2.2 | 18.2 ± 2.9 | < 0.001 |
| MDA F/U 2 months (post-op) | 8.2 ± 3.0 | 13.2 ± 3.7 | < 0.001 |
| FTA F/U 36 months (post-op) | 6.4 ± 1.5 | 10.8 ± 6.7 | < 0.001 |
| MDA F/U 36 months (post-op) | 3.0 ± 2.2 | 6.5 ± 4.0 | < 0.007 |
After postoperative correction at two-months follow up, FTA in group 1 ranged from 5 to 10° with a mean of 8.3 ± 2.2 and MDA in group 1 ranged from 3 to 12° with mean of 8.2 ± 3.0. FTA in group 2 ranged from 12 to 28° with a mean of 18.2 ± 2.9, MDA in group 2 ranged from 5 to 22° with a mean of 13.2 ± 3.7.
At 36-months follow up FTA in group 1 ranged from 4–9° with a mean of 6.4 ± 1.5 and MDA in group 1 ranged from 1 to 7° with mean of 3.0 ± 2.2. FTA in group 2 ranged from −10 to 21° with a mean of 10.8 ± 6.7, and MDA in group 2 ranged from −2 to 16° with a mean of 6.5 ± 4.0 (Table 2).
Interobserver agreement was done by two of the authors; intraclass correlation coefficient (ICC) was 0.7 and intraobserver (ICC) was 0.8.
There was no statistically significant difference between weight, BMI, preoperative MDA and preoperative FTA in the recurrent and non-recurrent groups (Table 1).
At four years of follow-up, four legs (28.6 %) had recurrence in group 1, and six legs (12.5 %) had recurrence in group 2. There was no significant difference in recurrence between these two groups. From ROC curve analysis, overcorrection more than 15° does not show any benefit in preventing the recurrence in Blount’s disease stage 2 (Fig. 1).
Fig. 1.
Receiver operating characteristic (ROC) curve for appropriate degrees of overcorrection in Blount’s disease
Discussion
The rate of recurrence of varus deformity in Blount disease has been found to be in the range of 30–100 %. Studies have shown that the rate of recurrence of varus deformity may be decreased by performing the initial surgery at an early age [13, 14]. Many reports documented a high rate of recurrence of varus deformity after proximal tibial and fibular osteotomy for infantile Blount disease [2, 3, 6]. The only two prognostic features which can be identified in evaluating the recurrence deformity are the patient’s age and Langenskiöld staging at the initial osteotomy [8]. Ferriter and Shapiro [9] found a clear difference, such that there was a recurrence rate of 76 % in limbs operated initially at age older than 4.5 years versus 31 % recurrence rate before 4.5 years. Many reports concluded that (a) operative treatment should be performed before the age of four years on patients with progressive clinical and radiographic evidence of Blount disease, (b) surgical correction should be performed when radiographic stage shows the patient had Blount disease corresponding to Langenskiöld stage I or II, (c) a single corrective osteotomy performed early on the affected limb could result in permanent correction which could significantly decrease the incidence of a symptomatic and painful knee at maturity, and (d) failure to correct the tibia vara early will result in permanent physeal damage and development of degenerative intra-articular knee pathology, including meniscal tears and degenerative articular cartilage changes [12, 14–17].
We agree with Ferriter and Shapiro [9] that, although increasing stage and increasing age correlated with increased recurrence, the increasing stage of the disease appears to be the most important prognostic factor. Based on our data, we believe that increasing stage relates directly to physeal damage of the proximal tibial, so if we believe that the increase of the recurrence is related to the increasing age and stage, do we need to do overcorrection in the early stage of Blount? Overcorrection into valgus is recommended by many surgeons who explained that this will place the mechanical axis of the leg within the lateral compartment of the knee, optimally unloading the medial proximal tibia to allow it to grow [3, 8]. From our data, the recurrence of patients in group 1 (postoperative FTA 7–13°) was 23.5 %; in group 2 (postoperative FTA more than 13°) it was 12.5 %. Although the rate of recurrence was less in postoperative FTA of more than 13°, the statistical difference was non-significant. The data from this study also demonstrate that FTA with more than 15° of overcorrection has no benefit in preventing the recurrence. To the best of our clinical judgment, the patients in both groups had a similar severity of disease and age. In both groups, the loss of correction or recurrence of varus deformity was not found to be correlated with the degree of overcorrection. We did not find any correlation between the amount of overcorrection to a valgus position and the recurrence.
Acknowledgments
The authors would like to thank Miss Siranart Kumpravat for her assistance in statistical analysis and staff of the Orthopaedic Research unit is also gratefully acknowledged.
References
- 1.Richards BS, Katz DE, Sims JB (1998) Effectiveness of brace treatment in early infantile Blount’s disease. J Pediatr Orthop 18:374–380 [PubMed]
- 2.Zionts LE, Shean CJ (1998) Brace treatment of early infantile tibia vara. J Pediatr Orthop 18:102–109 [PubMed]
- 3.Green WB. Infantile tibia vara. J Bone Joint Surg Am. 1993;75:130–143. doi: 10.2106/00004623-199301000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Levine AM, Drennan JC. Physiological bowing and tibia vara. The metaphyseal-diaphyseal angle in the measurement of bowleg deformities. J Bone Joint Surg Am. 1982;64:1158–1163. [PubMed] [Google Scholar]
- 5.Blount WP. Tibia vara, osteochondrosis deformans tibiae. Curr Pract Orthop Surg. 1966;3:141–156. [PubMed] [Google Scholar]
- 6.Smith CF. Current concepts review tibia vara (Blount’s disease) J Bone Joint Surg Am. 1982;64:630–632. [PubMed] [Google Scholar]
- 7.Hofmann A, Jones RE, Herring JA. Blount’s disease after skeletal maturity. J Bone Joint Surg Am. 1982;64:1004–1009. [PubMed] [Google Scholar]
- 8.Schoenecker PL, Meade WC, Pierron RL, et al. Blount’s disease: a retrospective review and recommendations for treatment. J Pediatr Orthop. 1985;5:181–186. doi: 10.1097/01241398-198505020-00012. [DOI] [PubMed] [Google Scholar]
- 9.Ferriter P, Shapiro F (1987) Infantile tibia vara: factors affecting outcome following proximal tibia osteotomy. J Pediatr Orthop 7:1–7 [PubMed]
- 10.Langenskiöld A (1981) Tibia vara: osteochondrosis deformans tibiae Blount’s disease. Clin Orthop 158:77–82 [PubMed]
- 11.Jones JK, Gill L, John M, Goddard M, Hambleton IR (2009) Outcome analysis of surgery for Blount disease. J Pediatr Orthop 29(7):730–735 [DOI] [PubMed]
- 12.Synder M, Vera J, Harcke HT, Bowen JR. Magnetic resonance imaging of the growth plate in late-onset tibia vara. Int Orthop. 2003;27:217–222. doi: 10.1007/s00264-003-0467-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gonzàlez-Herranz P. Recurrence of varus deformity after proximal tibial osteotomy in Blount disease: long-term follow-up. J Pediatr Orthop. 2005;25(1):130. doi: 10.1097/01241398-200501000-00028. [DOI] [PubMed] [Google Scholar]
- 14.Bs D, Volk AG, Smith CF. Infantile Blount disease: long-time follow-up surgically treated patients at skeletal maturity. J Pediatr Orthop. 1996;16:469–475. doi: 10.1097/01241398-199607000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Hayek S, Seger E, Ezra E, et al. Serrated W/M osteotomy: results using a new technique for the correction of infantile tibia vara. J Bone Joint Surg (Br) 2000;82:1026–1029. doi: 10.1302/0301-620X.82B7.10507. [DOI] [PubMed] [Google Scholar]
- 16.Bathfield CA, Beighton PH. Blount disease. A review of etiological factors in 110 patients. Clin Orthop. 1978;135:29–33. [PubMed] [Google Scholar]
- 17.Chotigavanichaya C, Salinas G, Green T, Moseley CF, Otsuka N. Recurrence of varus deformity after proximal tibial osteotomy in blount disease: long-term follow-up. JPO. 2002;22:638–641. [PubMed] [Google Scholar]
- 18.Sabharwal S. Blount disease. J Bone Joint Surg Am. 2009;91(7):1758–1776. doi: 10.2106/JBJS.H.01348. [DOI] [PubMed] [Google Scholar]