Abstract
Purpose
To evaluate how often manipulation under anesthesia (MUA) can achieve functional flexion ≥ 90 degrees and identify predictor for successful outcome of MUA for stiff total knee arthroplasty (TKA).
Methods
Demographic data, range of motion, and surgical and anesthetic information of 143 MUAs were retrospectively analyzed from 2000 to 2011.
Results
One-hundred thirty-six out of 143 patients (95 %) improved mean range of motion (ROM) from pre-MUA 62 ± 17° to final ROM 101 ± 21° (p < 0.001). Flexion ≥ 90 degrees was achieved in 74% (106/143) of patients. Regional anesthesia was identified as predictor of successful MUA outcome (p = 0.007, OR: 8.5, 95 % CI: 1.2-66.7).
Conclusions
Although the proportion of patients regaining flexion ≥ 90 degrees following MUA was less than those patients with simple overall ROM increase, the functional flexion ≥ 90 degrees was achieved in the vast majority of patients with stiff TKA following MUA.
Keywords: Total knee arthroplasty, Stiffness, Manipulation under anesthesia, Range of motion, Prognostic factors
Introduction
The main objectives of total knee arthroplasty (TKA) are to achieve a painless, stable, functional knee. In terms of functionality, TKA can improve range of motion (ROM) in patients with significant pre-operative limited joint motion [1]. However, despite advancements in surgical technique, implant design and perioperative management, post-TKA stiffness occurs with an incidence ranging from 1.8 % to 23 % [2–4]. It has been shown that aetiology of stiffness is multifactorial [5, 6] and that treatment is challenging. Stiffness may be defined as an inadequate range of motion (ROM) that results in functional limitations in daily activities. However, there is no consensus in the literature about the precise definition of functional ROM. In general, 90° of flexion has been considered as minimum functional recovery after primary TKA, as failure of recovering 90° flexion may jeopardise various daily activities. A biomechanical study demonstrated that 83° of flexion is required for going up and down stairs and 93° for sitting [7]. Of several treatment options for stiff TKA, manipulation under anesthesia (MUA) has been considered the first-line treatment after failure of nonoperative measurements, such as dynamic splint and physical therapy. A number of studies reported successful improvement in ROM ranging from 26° to 44° [8–11] following MUA. In a review article, Fitzsimmons et al. [12] reported that gained ROM by MUA ranges from 30° to 47° [12]. However, the majority of studies reported overall ROM gain following manipulation procedure, but limited information is available regarding successful ROM recovery achieving flexion ≥ 90° [9, 13]. We aimed to investigate how often functional final flexion ≥ 90° can be achieved following MUA for stiffness after primary TKA and any potential factors that can predict successful outcome after MUA procedures.
Materials and methods
This study was approved by the hospital institutional review board. The authors’ institution-based registry database was queried to identify study patients from 2000 to 2011, and 154 patients were identified as having undergone MUA for stiffness after primary TKA. Of these, 11 patients were excluded due to insufficient information for perioperative ROM; the remaining 143 were included for analysis. There were 59 men and 84 women with a mean age of 60.2 (range, 37–83) years at the time of MUA. Six patients had bilateral TKA and required manipulation of both knees. Diagnoses for primary TKA were osteoarthritis (n = 125), posttraumatic arthritis (n = 12), osteonecrosis (n = 1), septic knee sequelae (n = 1), rheumatoid arthritis (n = 2) and unknown (n = 2). Diabetes mellitus was diagnosed in 19 patients. Mean time interval between primary TKA and MUA was 8.6 (range, two to 40) weeks; 126 (74 %) underwent MUA within 12 weeks and the remaining 37 (26 %) after 12 weeks. Three patients received MUA 40 weeks after primary TKA when they underwent another joint replacement surgery for contralateral knee or hip joints. Mean follow-up was 23.4 (range, one to 110) months. There were three case of failed MUA that underwent an additional procedure one month post-MUA, accounting for the minimum follow-up period of 1 month in this study. All MUAs were performed by the same surgeons who performed the primary TKA, except in the case of three patients who received primary TKA at an outside hospital and were referred to our institution. MUA was indicated when knee flexion was < 90° at four to eight weeks post-TKA. Before proceeding with manipulation, physical examination and careful radiographic examination were performed to confirm that stiffness was not related to surgical factors, such as component malposition or oversizing, loose bodies or retained cement.
Under general anesthesia (n = 120) with adequate muscle relaxation or regional anesthesia (epidural 18, spinal 5), ROM and joint stability were first examined. Manipulation was performed by flexing the ipsilateral hip to 90°. Holding the proximal leg, steadily, gradually increasing pressure on the proximal tibia was applied to flex the knee joint until audible breakage of adhesion was heard. When the audible or palpable separation no longer occurred, the maximally flexed joint was maintained for a minute. When there was flexion contracture, the knee was carefully manipulated into extension. Putting the heel on a bolster, gentle, firm downward pressure was applied on top of the joint. A final ROM was measured after the procedure. Manipulation was performed as a same-day procedure (n = 97) or under hospitalisation (n = 46). When the procedure was performed under hospitalisation, a continuous passive-motion machine was applied, along with a local ice pack. Patients received outpatient physical therapy until their clinic visit at four to six weeks.
Flexion and extension angles were measured with a pocket goniometer either by the surgeon, arthroplasty fellows or an orthopaedic nurse practitioner before TKA, before and after MUA and at each clinic visit. Final ROM was defined as the arc of motion measured at the latest clinic follow-up or at the time immediately prior to additional procedures following failed MUA. Treatment success was defined as final flexion ≥ 90° (success group). and failure as final flexion < 90° (failure group).
Data were collected for demographics, ROM and surgical and anaesthetic information. Potential contributing factors included age, gender, body mass index (BMI), medical comorbidity including diabetes mellitus, ROM (before TKA, before and after MUA and at follow-up), interval between TKA and MUA, type of anaesthesia for MUA, type of implant (cruciate retaining versus posterior stabilised) and post-MUA hospitalisation.
Statistical analysis was performed using paired t tests to assess mean changes in ROM, independent groups t tests to compare continuous variables (age, BMI, TKA operative time, interval between TKA and MUA) and Fisher’s exact tests to compare proportions between groups. Median follow-up was compared using the Mann–Whitney U test. Multivariate logistic regression analysis was performed to determine independent predictors of MUA outcome using nine covariates in the model to control for confounding. IBM SPSS Statistics (version 21.0, IBM, Armonk, NY) was used for analysis. Two-tailed p < 0.05 was considered statistically significant.
Results
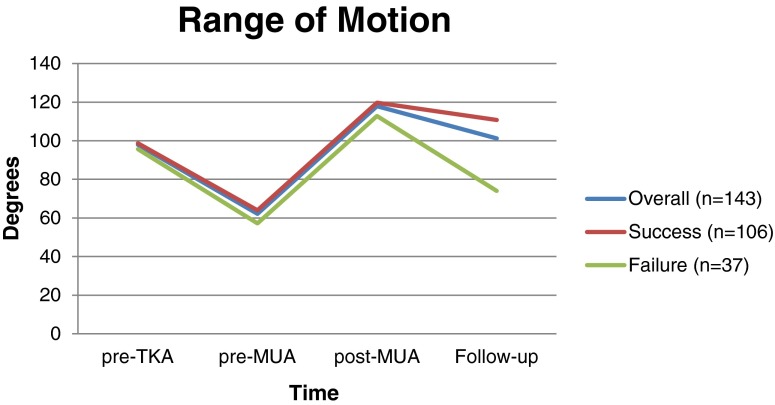
At the latest follow-up, 95.2 % of patients (136/143) showed significant improvement of ROM—from 62 ± 17° pre-MUA to 101 ± 21° at latest follow-up with 39° increments (p < 0.001). Seven patients (4.8 %, 7/143) did not improve following MUA, resulting in the same (n = 1) or decreased (n = 6) final ROM compared with pre-MUA ROM. The success rate to achieve final flexion of ≥ 90° was 74 % (106/143); 106/143 MUAs achieved final flexion ≥ 90°, with ROM improvement from 63 ± 16° pre-MUA to 110 ± 12° at latest follow-up (p < 0.001, success group,). The remaining 37 MUAs (26 %) failed to achieve satisfactory final flexion of 90° despite a ROM increase from 57 ± 18° pre-MUA to 74 ± 16° at latest follow-up (p < 0.001, failure group,) (Fig. 1).
Fig. 1.
Change of mean range of motion (ROM) at each time point: prior to total knee arthroplasty (TKA), prior to manipulation under anaesthesia (MUA), immediately after MUA and at latest follow-up
There was no difference between groups in patient age, BMI, operation time for primary TKA, and interval between TKA and MUA; however, median follow-up was significantly shorter in the failure group (Table 1). By univariate analysis, a successful outcome was observed in 21/23 (91 %) patients who had regional anaesthesia versus 85/120 (71 %) who had general anaesthesia (p = 0.04). Multivariate logistic regression analysis confirmed a significant association (p = 0.007) between type of anaesthesia and MUA outcome independent of the other eight variables tested, with patients undergoing regional anaesthesia faring significantly better than those undergoing general anaesthesia (Table 2). No complications occurred as a result of manipulation procedures in either group.
Table 1.
Comparison between success and failure groups
| Variable | Success (n = 106) | Failure (n = 37) | P value |
|---|---|---|---|
| Age at MUA (years) | 60.0 ± 9.6 | 60.7 ± 9.4 | 0.69 |
| BMI (kg/m2) | 30.7 ± 5.6 | 30.3 ± 7.0 | 0.72 |
| TKA operative time (min) | 101.1 ± 27.7 | 95.3 ± 25.3 | 0.28 |
| interval between TKA and MUA (weeks) | 8.3 ± 6.9 | 9.4 ± 7.1 | 0.41 |
| Follow-up, months, median (IQR) | 18.5 (8–41) | 8 (2–12) | 0.001* |
BMI body mass index, IQRinterquartile range, ± standard deviation
*Statistically significant
Table 2.
Analysis of factors associated with outcome of MUA for TKA stiffness
| Variable | Success (n = 106) | Failure (n = 37) | Univariate | Multivariate logistic regression | ||
|---|---|---|---|---|---|---|
| P value | P value | Odds ratio | 95 % CI | |||
| Age (years) | 0.87 | 0.54 | – | – | ||
| ≤65 | 73 (69 %) | 26 (70 %) | ||||
| >65 | 33 (31 %) | 11 (30 %) | ||||
| Gender | 0.78 | 0.9 | – | – | ||
| Female | 63 (59 %) | 21 (57 %) | ||||
| Male | 43 (41 %) | 16 (43 %) | ||||
| BMI, kg/m2 | 0.58 | 0.55 | – | – | ||
| <30 | 60 (57 %) | 19 (51 %) | ||||
| ≥30 | 46 (43 %) | 18 (49 %) | ||||
| Diabetes mellitus | 0.61 | 0.45 | – | – | ||
| Yes | 15 (14 %) | 4 (11 %) | ||||
| No | 91 (86 %) | 33 (89 %) | ||||
| Pre-TKA ROM (°) | 0.42 | 0.23 | – | – | ||
| <90 | 32 (30 %) | 11 (30 %) | ||||
| ≥90 | 67 (63 %) | 21 (57 %) | ||||
| Unknown | 7 (7 %) | 5 (13 %) | ||||
| Interval from TKA to MUA | 0.24 | 0.16 | – | – | ||
| ≤12 weeks | 94 (89 %) | 30 (81 %) | ||||
| >12 weeks | 12 (11 %) | 7 (19 %) | ||||
| Anaesthesia | 0.04* | 0.007* | 8.5 | 1.2-66.7 | ||
| General | 85 (80 %) | 35 (95 %) | ||||
| Regional | 21 (20 %) | 2 (5 %) | ||||
| Implant | 0.72 | 0.96 | – | – | ||
| Cruciate retaining | 94 (89 %) | 32 (86 %) | ||||
| Posterior stabilized | 12 (11 %) | 5 (14 %) | ||||
| Post-MUA hospital stay | 0.24 | 0.16 | – | – | ||
| Yes | 37 (35 %) | 9 (24 %) | ||||
| No | 69 (65 %) | 28 (76 %) | ||||
MUA manipulation under anaesthesia, TKA total knee arthroplasty, BMI body mass index, ROM range of motion, CI confidence interval
*Statistically significant
Discussion
MUA improves ROM for stiff TKA with a success rate rate of > 90 % [4, 8, 9, 11, 13, 14]. However, the majority of studies report overall ROM improvement, and limited information is available regarding success rate in achieving flexion ≥ 90° [9, 13]. Given the fact that functionality is also one of the goals of joint replacement, recovering functional ROM is an important factor in evaluating MUA outcomes after primary TKA. Currently, there is no consensus of the definition for successful MUA, as patient satisfaction may vary according to pre-operative ROM, activity requirement or regional life style [15, 16]. Non-Western populations, who perform frequent squatting, kneeling or sitting cross-legged activities, clearly demand a greater ROM [16]. However, in general, 90° of knee flexion is considered as functional recovery for performing activities of everyday living, such as going up and down stairs or sitting on a chair.
In this study, in which we report results in one of the largest patient populations undergoing MUA for stiffness following TKA, treatment success—defined as achievement of ≥ 90° of flexion—was 74 % (106/143). This was lower than those of other previous reports that also evaluated their results based on final achievement of 90° of flexion. In the literature, Cates and Schmidt [9] reported 20 of 23 patients (87 %) regained at least 90° of flexion by manipulation. Esler et al. [13] reported that ten of 47 (21.3 %) patients were unable to flex to 90° after MUA. However, these studies included relatively small number of patients. In addition, direct comparison of these results is difficult due to heterogeneous criteria of variables. Specifically in regard to procedure indication and timing, several studies [4, 11, 14, 17] suggested 90 days as time criteria between TKA and MUA; however, other studies suggested early MUA as being that performed within three weeks [10, 18], 30 days [19], eight weeks [9] and 75 days [8] following TKA. In our study, we applied a 12-week cutoff for evaluating MUA timing, as most authors recommend a time interval < three months following initial surgery [4, 9, 15, 19, 20].
Many factors have been suggested as possible risk factors for failed MUA, including diagnosis of rheumatoid arthritis [3], late manipulation [8, 9], diabetes mellitus [8, 11], less pre-TKA ROM [4, 19, 21], cruciate-retaining implant [8] and prior operation history [17, 19]. However, other studies reported contradictory findings related to possible risk factors of MUA outcome [4, 10, 14, 17, 22]. Namba and Inacio [14] reported that both early and late manipulation could improve flexion. Yeoh et al. [22] reported that there was no difference in ROM gain between knees with a pre-TKA ROM < 90° and > 90°. In our study, although many of these potential factors regarding MUA outcome were not found to be associated with final ROM recovery, regional anaesthesia was identified as positive predictor of successful outcome. This may in part be because regional anaesthesia would have contributed to optimal pain control in the early postprocedure period. This finding is in agreement with a previous study in which a modified technique was used for repeated MUA [23]. The study used epidural anaesthesia continued for postoperative analgesia, hospital stay of one to three days, continuous passive motion for two to three days and daily physical therapy; reported successful results were observed in 74 % of patients.
Our study has a number of limitations. First was the relatively short follow-up period in the failure group. This was because many failed MUA patients immediately underwent next-step procedures, including repeated MUA or revision arthroplasty. Second, during the study periods, there was no standardised protocol for managing stiff TKA among different surgeons, which might have affected treatment outcomes. However, indications and techniques for MUA were consistent among surgeons.
In summary, findings of our study demonstrate that although the proportion of patients regaining flexion ≥ 90° following MUA was less than in patients with overall ROM increase, functional recovery with flexion ≥ 90° was achieved in the majority of patients (74 %) with stiff TKA following MUA. Using regional anaesthesia was identified as a predictor of improved MUA outcome. Further studies are required to characterise clinical patient factors that may optimise ROM recovery in TKA patients.
Acknowledgments
Conflict of interest
None.
References
- 1.Debette C, Lustig S, Servien E, Lording T, Villa V, Demey G, Neyret P. Total knee arthroplasty of the stiff knee: three hundred and four cases. Int Orthop. 2014;38:285–289. doi: 10.1007/s00264-013-2252-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anania A, Abdel MP, Lee YY, Lyman S, Gonzalez Della Valle A. The natural history of a newly developed flexion contracture following primary total knee arthroplasty. Int Orthop. 2013;37:1917–1923. doi: 10.1007/s00264-013-1993-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fox JL, Poss R. The role of manipulation following total knee replacement. J Bone Joint Surg Am. 1981;63:357–362. [PubMed] [Google Scholar]
- 4.Keating EM, Ritter MA, Harty LD, Haas G, Meding JB, Faris PM, Berend ME. Manipulation after total knee arthroplasty. J Bone Joint Surg Am. 2007;89:282–286. doi: 10.2106/JBJS.E.00205. [DOI] [PubMed] [Google Scholar]
- 5.Gonzalez Della Valle A, Leali A, Haas S. Etiology and surgical interventions for stiff total knee replacements. Hss J. 2007;3:182–189. doi: 10.1007/s11420-007-9053-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lutzner J, Kirschner S, Gunther KP, Harman MK. Patients with no functional improvement after total knee arthroplasty show different kinematics. Int Orthop. 2012;36:1841–1847. doi: 10.1007/s00264-012-1584-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Laubenthal KN, Smidt GL, Kettelkamp DB. A quantitative analysis of knee motion during activities of daily living. Phys Ther. 1972;52:34–43. doi: 10.1093/ptj/52.1.34. [DOI] [PubMed] [Google Scholar]
- 8.Bawa HS, Wera GD, Kraay MJ, Marcus RE, Goldberg VM. Predictors of Range of Motion in Patients Undergoing Manipulation After TKA. Clin Orthop Relat Res. 2013;471:258–263. doi: 10.1007/s11999-012-2591-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cates HE, Schmidt JM. Closed manipulation after total knee arthroplasty: outcome and affecting variables. Orthopedics. 2009;32:398. doi: 10.3928/01477447-20090511-10. [DOI] [PubMed] [Google Scholar]
- 10.Ellis TJ, Beshires E, Brindley GW, Adams RL, Preece C. Knee manipulation after total knee arthroplasty. J South Orthop Assoc. 1999;8:73–79. [PubMed] [Google Scholar]
- 11.Mohammed R, Syed S, Ahmed N. Manipulation under anaesthesia for stiffness following knee arthroplasty. Ann R Coll Surg Engl. 2009;91:220–223. doi: 10.1308/003588409X359321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fitzsimmons SE, Vazquez EA, Bronson MJ. How to treat the stiff total knee arthroplasty?: a systematic review. Clin Orthop Relat Res. 2010;468:1096–1106. doi: 10.1007/s11999-010-1230-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Esler CN, Lock K, Harper WM, Gregg PJ. Manipulation of total knee replacements. Is the flexion gained retained? J Bone Joint Surg Br. 1999;81:27–29. doi: 10.1302/0301-620X.81B1.8848. [DOI] [PubMed] [Google Scholar]
- 14.Namba RS, Inacio M. Early and late manipulation improve flexion after total knee arthroplasty. J Arthroplasty. 2007;22:58–61. doi: 10.1016/j.arth.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 15.Maloney WJ. The stiff total knee arthroplasty: evaluation and management. J Arthroplasty. 2002;17:71–73. doi: 10.1054/arth.2002.32450. [DOI] [PubMed] [Google Scholar]
- 16.Mulholland SJ, Wyss UP. Activities of daily living in non-Western cultures: range of motion requirements for hip and knee joint implants. Int J Rehabil Res. 2001;24:191–198. doi: 10.1097/00004356-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Scranton PE., Jr Management of knee pain and stiffness after total knee arthroplasty. J Arthroplasty. 2001;16:428–435. doi: 10.1054/arth.2001.22250. [DOI] [PubMed] [Google Scholar]
- 18.Yercan HS, Sugun TS, Bussiere C, Ait Si Selmi T, Davies A, Neyret P. Stiffness after total knee arthroplasty: prevalence, management and outcomes. Knee. 2006;13:111–117. doi: 10.1016/j.knee.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Ipach I, Mittag F, Lahrmann J, Kunze B, Kluba T. Arthrofibrosis after TKA - Influence factors on the absolute flexion and gain in flexion after manipulation under anaesthesia. BMC Musculoskelet Disord. 2011;12:184. doi: 10.1186/1471-2474-12-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghani H, Maffulli N, Khanduja V. Management of stiffness following total knee arthroplasty: A systematic review. Knee. 2012;19:751–759. doi: 10.1016/j.knee.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 21.Rubinstein RA, Jr, DeHaan A. The incidence and results of manipulation after primary total knee arthroplasty. Knee. 2010;17:29–32. doi: 10.1016/j.knee.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 22.Yeoh D, Nicolaou N, Goddard R, Willmott H, Miles K, East D, Hinves B, Shepperd J, Butler-Manuel A. Manipulation under anaesthesia post total knee replacement: long term follow up. Knee. 2012;19:329–331. doi: 10.1016/j.knee.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 23.Pariente GM, Lombardi AV, Jr, Berend KR, Mallory TH, Adams JB. Manipulation with prolonged epidural analgesia for treatment of TKA complicated by arthrofibrosis. Surg Technol Int. 2006;15:221–224. [PubMed] [Google Scholar]