Abstract
Gait analysis is an objective tool that has been used to assess and monitor treatment for many musculoskeletal conditions. Recently, it has been used to assess the impact of femoro-acetabular impingement (FAI) on the hip and lower limb movements. There have been a fairly limited number of studies published so far reporting unexpected and inconsistent results, which calls for more research to be conducted in this arena. In the light of the limited data available, it has been challenging to reconcile the contradictions in some of these results, and therefore no coherent conclusions could be drawn. In this short article, we attempt to explain some of the abnormal kinematic and kinetic patterns associated with FAI by highlighting similarities between the gait seen in early osteoarthritis (OA) and that of FAI. We also propose an approach for future research in this field and emphasise the importance of quantifying early OA in FAI based on magnetic resonance imaging (MRI) scans and the amount of chondral damage seen during open or arthroscopic surgery.
Keywords: Kinematics, Kinetics, Femoro-acetabular impingement
Introduction
Femoro-acetabular impingement (FAI) is a pathomechanical condition caused by an altered osseous morphology of the acetabulum and or the head-neck junction of the femur [1–3]. This leads to a pathological abutment and a point or regional loading of the femoral neck or head-neck junction against the acetabulum [4–6]. This reduces the free arc of hip motion [7] and causes articular or soft tissue damage around the acetabular rim [8, 9] which may eventually result in irreversible labral and chondral damage [8, 10], thereby ultimately progressing on to osteoarthritis (OA) [11–13]. Based on the morphological bony anomalies contributing to the impingement process, two distinct types of FAI have been described [6]. The pincer type is caused by bony anomalies associated with the acetabulum such as excessively retroverted acetabulum or an acetabular protrusion, whilst the cam type is caused by mis-shaped head-neck junction of the femur causing a prominence at the femoral head-neck junction leading to impingement. In many cases patients have a combination of cam and pincer FAI [6, 9, 14]. Therefore, surgical intervention by an open, arthroscopic or combined techniques [15–17] aims to reduce the severity of the impingement, relieve pain and possibly increase motion.
Since FAI impairs hip motion, obtaining objective and accurate assessment of hip biodynamics is vital in understanding the impact of this condition. Gait analysis has been used as an objective and quantitative technique for the evaluation of normal and pathological patterns of locomotion in many musculoskeletal conditions [18, 19]. It has also been used for the prescription of treatment as well as evaluating the effect of different interventions in pathological states [20–23]. Therefore, it could potentially provide an alternative objective assessment tool for FAI.
Patients with FAI were thought to have normal gait pattern because it can be difficult to identify small kinematic abnormalities by clinically appraising gait unless an antalgic gait is present [24]. For example, normal hips abduct during the swing phase in order to swing the foot around the contralateral leg (foot) and adduct during the stance phase in order to shift the centre of gravity directly above the supporting leg [25]. Small differences in these movements can be difficult to appreciate during clinical assessment. However, using modern gait analysis techniques have allowed investigators to acquire precise measurements highlighting subtle discrepancies in the joint kinematics that are not readily visible to the clinician’s eye [22, 26].
The potential impact of FAI on gait was initially highlighted in a computer-based study by Rab [27] on slipped capital femoral epiphysis (SCFE) which resembles FAI. The author simulated a virtual restriction in the overall range of hip movements during the gait cycle, with significant reduction in hip flexion that correlated with the severity of the slip [27]. Since then, there have been a small number of clinical studies looking at gait and the overall range of hip movements in patients with FAI [20, 23, 28, 29]. These studies have compared patients with FAI to healthy control groups [28, 29] and also looked at gait parameters in patients with FAI before and after surgery [20, 23], revealing surprising and inconsistent results. It is therefore challenging to draw any logical conclusions from the limited data available in the literature. The small number of studies makes summarising their positive results fairly easy, but the aim of this article is to analyse these conflicting results and their clinical effect and with these in mind be able to propose further research in this arena.
Kinematics and kinetics in FAI
Kennedy et al. demonstrated reduced frontal (abduction and adduction) and sagittal (flexion and extension) range of movements (ROM) in hips with FAI compared to a control group during gait at a natural pace. These reductions in movements were caused by significant decrease in hip peak abduction angle and an insignificant decrease in the peak extension angle [28] respectively; these are the maximum angles recorded for hip abduction and extension (respectively) during normal pace gait. Similarly, Hunt et al. reported significantly reduced sagittal ROM caused by a significantly reduced peak extension angle [29]. However, contrary to Kennedy et al. [28], they demonstrated a significant reduction in the peak internal rotation angle and in the peak adduction angle causing insignificant reduction in the frontal plane ROM [29]. Patients with FAI often have limited internal rotation especially in flexion and also limited adduction [2, 9], and therefore from the outset it seems that this concurs more with the findings in the Hunt et al. study [29].
With regard to kinetics, Kennedy et al. reported no significant differences in all planes of movement [28]. However, Hunt et al. demonstrated reduction in the moment of hip flexion and external rotation [29]. Furthermore, Hunt et al. also demonstrated a reduction in the velocity of gait.
Surgical treatment resulted in an increased sagittal ROM and reduction in reverse hip flexion angle according to Rylander et al. [20], but no improvement could be demonstrated by Brisson et al. who looked at the effect of surgery on cam FAI [23]. Neither of these studies demonstrated any impact of surgery on the kinetics of the hip. It is worth noting that Kennedy et al. and Brisson et al. included cam FAI only [23, 28], whilst Rylander et al. and Hunt et al. included different types of FAI [20, 29] which may explain some of the differences in the results.
Are these results consistent with FAI?
Normal hip sagittal and frontal ROM during gait at a natural pace varies slightly but is centred on the average figure of 40 and 13° respectively, with little variations amongst different age groups [18, 25]. However, the total sagittal ROM of the hip joint is almost 130° and the total frontal plane ROM is approximately 80° [30]. Therefore, during normal pace gait cycle the hip only moves within 31 % of the total sagittal ROM and 16 % of the frontal ROM. Furthermore, two computer-based studies conducted by Bedi et al. [31] and Kubiak-Langer et al. [32] showed that patients with FAI had an average flexion of greater than 100° before any physical osseous impingement occurred on simulation. This is not far off the average hip flexion gained during clinical examination, which has been shown to have an average of more than 90° [33, 34]. Hence, the range of peak flexion during the normal gait cycle does not reach the threshold for physical impingement. Therefore, why should FAI have any impact on the sagittal ROM of the hip during gait at a natural pace?
The studies comparing patients with FAI to control patients have consistently demonstrated a reduction in the peak extension angle [28, 29]. Even when the overall range of sagittal movement was reduced, it was caused by this reduction in the peak extension angle. This is in total contradiction to what is expected from the impinging hip [27, 31] particularly in cam FAI. The impingement occurs around the anterior superior aspect of the acetabulum [32] and hence if FAI is ever going to have any impact on the gait then this should manifest maximum during flexion and internal rotation [27].
Furthermore, surgical resection of the cam impinging lesion did not lead to any improvement in the kinematics of the hip despite the improvement in pain [23]. Even when surgery led to an improvement in the range of motion as demonstrated by Rylander et al. [20], the change in the hip flexion angle did not correlate with pain or functional scores, depth of acetabular labrum resection or the improvement in the centre edge angle. Furthermore, there were no changes noted in the kinetics of the hip following surgical resection of the cam lesion [20, 23].
The above contradictions in the results and the inconsolable findings with our expectations raise the question whether we should attribute all the changes in the kinematics and kinetics purely to the colliding and impinging areas in the acetabulum and the femoral head-neck junction. Or is there another process (or processes) associated with FAI that may underpin the observations reported?
Some of the explanations that have been suggested for the abnormal hip kinematics in FAI, beside bony impingement, are pain inhibition and soft tissue impingement [20, 28, 29]. It is also possible that patients with FAI have subconsciously adopted impingement and pain avoidance behaviour that manifests by an altered gait pattern [23]. Another possible explanation is muscle weakness, which is poorly understood in FAI, but so far has been demonstrated in some muscle groups affecting flexion, abduction and internal rotation [35, 36]. The decrease in peak extension could also be secondary to muscle contractures or early anterior capsular tightness similar to what occurs in arthritis. The range of hip joint extension is normally less than flexion [25], and therefore even a slight reduction in extension (as a result of anterior capsule tightness or muscle contracture) could easily translate into a significant reduction in the peak extension angle during gait and hence smaller step length.
Discussion
One of the significant findings raised by Rylander et al. [20, 35] was the presence of reverse angles in almost 50 % of their cohort, and this was also noted recently by Hunt et al. [29] in one of their participants with FAI. This may hold the key for explaining some of the gait analysis results in FAI.
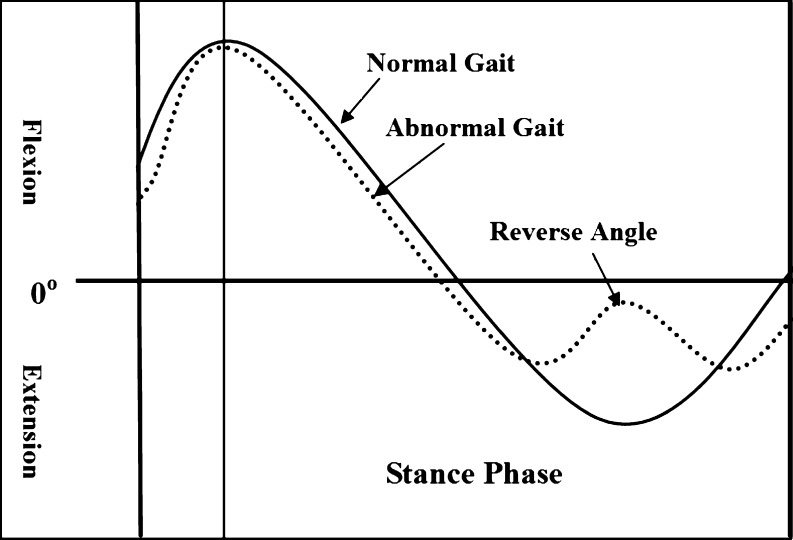
The reverse flexion angle (or discontinuity in motion) occurs when the smooth pattern of flexion and extension (sagittal plane movement) is disturbed by an abnormal hesitation or reversal during the flexion-extension cycle [37] (Fig. 1). This discontinuity of motion tends to occur at a point as the hip passes from flexion into extension during the stance phase of the gait cycle [20, 37, 38]. This is rarely seen in normal individuals, and even when present it tends to have a significantly smaller magnitude [38]. However, this phenomenon has been strongly linked to OA [38], and its prevalence and magnitude have been independently correlated with the radiological severity and the progression of OA regardless of pain or hip functional scores [37, 38].
Fig. 1.
An approximate presentation of part of the gait cycle pattern comparing normal and abnormal gait with reverse angle (time duration and range of flexion and extension is only an approximation and not accurately scaled)
Therefore, this raises the possibility that the abnormal kinematics seen in FAI might be because of an underlying presence of early OA associated with FAI rather than by the actual act of physical impingement. This possibility was also raised by Rylander et al. [20] and it is further supported by the following observations:
According to Ganz et al. and other authors, early OA in FAI is pre-radiological [39–41]. All the studies on kinematics of FAI have so far relied on X-rays to identify the presence of OA and none have commented on the presence (or not) of any OA features on the magnetic resonance imaging (MRI) scans. Therefore, we suspect that many patients with early OA in association with FAI were included in the above studies.
The reverse angle tended to occur in the mid-stance or later part of the stance phase as the hip is extending [20]. Again this contradicts our expectations of FAI (especially cam FAI) because any FAI-related reverse angle should theoretically occur during the early part of the stance phase (during flexion) because in this position the distance between the impinging ossicles is less and the femur is closer to the anterior aspect of the acetabulum where impingement occurs [32].
In early OA, Foucher et al. [38] reported that the position of the reverse angle began at around mid-stance (44 ± 13 % of the stance phase) and lasted for 27 ± 13 % (of the stance phase) into the extension phase. Similarly, Hurwitz et al. [37] reported that the position of the reverse angle in OA occurred at 69 ± 26 % of the range of motion during the stance phase, i.e. as the subject was reaching the limit of the extension motion. Therefore, the position of the reverse angle in early OA [38] is consistent with what has been reported in FAI [20].
-
3.
Rylander et al. demonstrated an increase in the range of motion post surgical treatment of FAI [20]. This was also associated with the complete resolution or reduction of these reverse angles. However, this improved movement did not correlate with reduction in pain or with improvement in hip functional scores. The cohort of patients in the study by Brisson et al. [23] did not have reverse angles pre-operatively [28] and neither did they show any improvement in the sagittal plane range of motion post-operatively (or in any of the kinematics) despite removing the impinging lesion and the improvement in pain score [23]. A simplistic suggestion here may be that whatever process was responsible (more likely to be early OA) for these reverse angles (in the cohort of Rylander et al.) was also responsible for the reduction in sagittal movements before surgery regardless of pain or function. Treating the underlying cause for this reverse angle translated into an improvement in the movements following surgery. It is also worth noting that Rylander et al. carried out multiple procedures, including repair or resection of the labrum and microfracture of the damaged chondral surface of the acetabulum.
We can only speculate from these findings that the cohort of patients in the Brisson et al. study [23] had early OA to cause abnormal gait patterns, but this early OA was not significant enough to cause obvious reverse angles during gait analysis. It is also not clear from their study whether they detected or treated any significant acetabular chondral damage.
-
4.
As demonstrated by Kennedy et al. [28] and Hunt et al. [29], the reduction in the sagittal plane of movement was mainly attributed to the reduction in the peak extension angle and not to the peak flexion angle (contrary to our expectation as impingement mainly occurs during flexion [27, 31, 32]). These findings are consistent with the kinematic findings in early OA [42]. Eitzen et al. demonstrated that patients with early OA walked at a reduced velocity and revealed a significantly reduced hip joint excursion, specifically manifesting in a significantly reduced peak extension angle [42]. On the other hand, peak flexion angles of early OA patients were similar to those of the controls [42].
-
5.
In the Brisson et al. study [23], operative treatment of FAI did not result in improvement in the ROM despite the improvement in pain. Even when improvement in ROM occurred, as in the Rylander et al. study [20], this did not correlate with improvement in pain. This suggests that the ROM during normal gait in FAI might not be significantly related to pain. Similar findings were found in OA where some authors did not attribute the decrease in the kinematics range (during normal gait) to pain but to the overall decrease in the range of motion of the affected joint [37, 43].
Future research
The above points draw similarities between the characteristics of patterns in gait in OA and FAI suggesting that the presence of early OA in association with FAI may explain at least some of variations seen in the results published. However, the studies done so far have included inconsistent cohorts of patients, and therefore from the available limited data, it is difficult to draw any comfortable and robust conclusions. The logical recommendation, therefore, would be to do further clinical gait analysis in FAI with strict inclusion criteria. This, however, is more likely to reproduce the same inconsistent results, unless we made sure that we have accounted for all the different explanatory variables in our analysis model.
There are several consistent radiological features associated with FAI [8–10, 14], yet there are many people with these radiological features who are asymptomatic [44–47]. In fact there are patients with bilateral radiological evidence of FAI but with only one symptomatic hip [29]. Furthermore, there have been contradictory reports in the form of longitudinal studies linking some of these radiological features with the development of OA in these asymptomatic people [44, 47]. This highlights the fact that FAI represents not a single entity but a wide spectrum [24] caused by many variable parameters with some having more influence than others either independently or in constellation with other demographic and clinical variables. Recognising the heterogeneity of this condition is fundamental to research in this arena. Categorising patients into cam, pincer and mixed FAI may be adequate in the clinical setting, but this classification is still very broad in research terms especially when considering the number of radiological variables associated with each type of FAI [8–10]. We need to have a system of not only recording the presence or absence of certain radiological and clinical signs but we also need to quantify these signs on categorical or continuous scales so that they can be specifically and directly correlated with the outcomes in kinematics and kinetics. For example, categorising patients into groups according to an alpha angle of greater or less than 50° may not be sufficient, instead the actual angle will need to be recorded and correlated as a continuous variable with the measured outcome in a univariate or multivariate analysis with other factors.
Another important factor that has been ignored by the studies but highlighted by several authors is the significant impact of early and pre-radiological OA in FAI [39–41]. None of the studies conducted so far assessed for the absence or presence of OA on MRI scans or during arthroscopy or attempted to quantify its severity on the symptomatic hip. They have relied on simple radiographs during the recruitment of patients, therefore inevitably missing many patients with pre-radiological early OA. We therefore recommend the quantification of the amount of OA based on MRI scans and/or chondral damage found during surgery [48]. This can be then correlated alongside other radiological features with different kinematic and kinetic variables.
In conclusion, there is very little published in the field of gait analysis and FAI and the studies conducted so far suffer from common weaknesses such as the inclusion of a small and inconsistent cohort of participants. Considering the multiple variables (radiological, demographic and clinical) associated with this condition, studies with a large cohort of patients are needed in order to be able to draw meaningful conclusions. This will require the collaboration of the different centres interested in this field for the recruitment of enough participants that will allow for adequate subgroup analysis according to these variables.
References
- 1.Audenaert EA, Peeters I, Vigneron L, Baelde N, Pattyn C. Hip morphological characteristics and range of internal rotation in femoroacetabular impingement. Am J Sports Med. 2012;40:1329–1336. doi: 10.1177/0363546512441328. [DOI] [PubMed] [Google Scholar]
- 2.Leunig M, Beaulé PE, Ganz R. The concept of femoroacetabular impingement: current status and future perspectives. Clin Orthop Relat Res. 2009;467:616–622. doi: 10.1007/s11999-008-0646-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anderson SE, Siebenrock KA, Tannast M. Femoroacetabular impingement: evidence of an established hip abnormality. Radiology. 2010;257:8–13. doi: 10.1148/radiol.10091480. [DOI] [PubMed] [Google Scholar]
- 4.Ito K, Minka MA, 2nd, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. doi: 10.1302/0301-620X.83B2.11092. [DOI] [PubMed] [Google Scholar]
- 5.Leunig M, Beck M, Kalhor M, Kim YJ, Werlen S, Ganz R. Fibrocystic changes at anterosuperior femoral neck: prevalence in hips with femoroacetabular impingement. Radiology. 2005;236:237–246. doi: 10.1148/radiol.2361040140. [DOI] [PubMed] [Google Scholar]
- 6.Imam S, Khanduja V. Current concepts in the diagnosis and management of femoroacetabular impingement. Int Orthop. 2011;35:1427–1435. doi: 10.1007/s00264-011-1278-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lamontagne M, Kennedy MJ, Beaulé PE. The effect of cam FAI on hip and pelvic motion during maximum squat. Clin Orthop Relat Res. 2009;467:645–650. doi: 10.1007/s11999-008-0620-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pfirrmann CW, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240:778–785. doi: 10.1148/radiol.2403050767. [DOI] [PubMed] [Google Scholar]
- 9.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis–what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 10.Beall DP, Sweet CF, Martin HD, Lastine CL, Grayson DE, Ly JQ, Fish JR. Imaging findings of femoroacetabular impingement syndrome. Skeletal Radiol. 2005;34:691–701. doi: 10.1007/s00256-005-0932-9. [DOI] [PubMed] [Google Scholar]
- 11.Agricola R, Heijboer MP, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK) Ann Rheum Dis. 2013;72:918–923. doi: 10.1136/annrheumdis-2012-201643. [DOI] [PubMed] [Google Scholar]
- 12.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 13.Takeyama A, Naito M, Shiramizu K, Kiyama T. Prevalence of femoroacetabular impingement in Asian patients with osteoarthritis of the hip. Int Orthop. 2009;33:1229–1232. doi: 10.1007/s00264-009-0742-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cavaignac E, Chiron P, Espié A, Reina N, Lepage B, Laffosse JM. Experimental study of an original radiographic view for diagnosis of cam-type anterior femoroacetabular impingement. Int Orthop. 2012;36:1783–1788. doi: 10.1007/s00264-012-1550-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Papalia R, Del Buono A, Franceschi F, Marinozzi A, Maffulli N, Denaro V. Femoroacetabular impingement syndrome management: arthroscopy or open surgery? Int Orthop. 2012;36:903–914. doi: 10.1007/s00264-011-1443-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khanduja V, Villar RN. The arthroscopic management of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15:1035–1040. doi: 10.1007/s00167-007-0319-7. [DOI] [PubMed] [Google Scholar]
- 17.Bedi A, Kelly BT, Khanduja V. Arthroscopic hip preservation surgery: current concepts and perspective. Bone Joint J. 2013;95-B:10–19. doi: 10.1302/0301-620X.95B1.29608. [DOI] [PubMed] [Google Scholar]
- 18.Kadaba MP, Ramakrishnan HK, Wootten ME. Measurement of lower extremity kinematics during level walking. J Orthop Res. 1990;8:383–392. doi: 10.1002/jor.1100080310. [DOI] [PubMed] [Google Scholar]
- 19.Ornetti P, Maillefert JF, Laroche D, Morisset C, Dougados M, Gossec L. Gait analysis as a quantifiable outcome measure in hip or knee osteoarthritis: a systematic review. Joint Bone Spine. 2010;77:421–425. doi: 10.1016/j.jbspin.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 20.Rylander JH, Shu B, Andriacchi TP, Safran MR. Preoperative and postoperative sagittal plane hip kinematics in patients with femoroacetabular impingement during level walking. Am J Sports Med. 2011;39(Suppl):36S–42S. doi: 10.1177/0363546511413993. [DOI] [PubMed] [Google Scholar]
- 21.Paoloni M, Di Sante L, Dimaggio M, Bernetti A, Mangone M, Di Renzo S, Santilli V. Kinematic and kinetic modifications in walking pattern of hip osteoarthritis patients induced by intra-articular injections of hyaluronic acid. Clin Biomech (Bristol, Avon) 2012;27:661–665. doi: 10.1016/j.clinbiomech.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 22.Ewen AM, Stewart S, St Clair Gibson A, Kashyap SN, Caplan N. Post-operative gait analysis in total hip replacement patients-a review of current literature and meta-analysis. Gait Posture. 2012;36:1–6. doi: 10.1016/j.gaitpost.2011.12.024. [DOI] [PubMed] [Google Scholar]
- 23.Brisson N, Lamontagne M, Kennedy MJ, Beaulé PE. The effects of cam femoroacetabular impingement corrective surgery on lower-extremity gait biomechanics. Gait Posture. 2013;37:258–263. doi: 10.1016/j.gaitpost.2012.07.016. [DOI] [PubMed] [Google Scholar]
- 24.Zebala LP, Schoenecker PL, Clohisy JC. Anterior femoroacetabular impingement: a diverse disease with evolving treatment options. Iowa Orthop J. 2007;27:71–81. [PMC free article] [PubMed] [Google Scholar]
- 25.Gore TA, Higginson GR, Stevens J. The kinematics of hip joints: normal functioning. Clin Phys Physiol Meas. 1984;5:233–252. doi: 10.1088/0143-0815/5/4/001. [DOI] [PubMed] [Google Scholar]
- 26.McGinley JL, Baker R, Wolfe R, Morris ME. The reliability of three-dimensional kinematic gait measurements: a systematic review. Gait Posture. 2009;29:360–369. doi: 10.1016/j.gaitpost.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 27.Rab GT. The geometry of slipped capital femoral epiphysis: implications for movement, impingement, and corrective osteotomy. J Pediatr Orthop. 1999;19:419–424. doi: 10.1097/00004694-199907000-00001. [DOI] [PubMed] [Google Scholar]
- 28.Kennedy MJ, Lamontagne M, Beaulé PE. Femoroacetabular impingement alters hip and pelvic biomechanics during gait: walking biomechanics of FAI. Gait Posture. 2009;30:41–44. doi: 10.1016/j.gaitpost.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 29.Hunt MA, Gunether JR, Gilbart MK. Kinematic and kinetic differences during walking in patients with and without symptomatic femoroacetabular impingement. Clin Biomech (Bristol, Avon) 2013;28:519–523. doi: 10.1016/j.clinbiomech.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 30.Roaas A, Andersson GB. Normal range of motion of the hip, knee and ankle joints in male subjects, 30–40 years of age. Acta Orthop Scand. 1982;53:205–208. doi: 10.3109/17453678208992202. [DOI] [PubMed] [Google Scholar]
- 31.Bedi A, Dolan M, Hetsroni I, Magennis E, Lipman J, Buly R, Kelly BT. Surgical treatment of femoroacetabular impingement improves hip kinematics: a computer-assisted model. Am J Sports Med. 2011;39(Suppl):43S–49S. doi: 10.1177/0363546511414635. [DOI] [PubMed] [Google Scholar]
- 32.Kubiak-Langer M, Tannast M, Murphy SB, Siebenrock KA, Langlotz F. Range of motion in anterior femoroacetabular impingement. Clin Orthop Relat Res. 2007;458:117–124. doi: 10.1097/BLO.0b013e318031c595. [DOI] [PubMed] [Google Scholar]
- 33.Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467:638–644. doi: 10.1007/s11999-008-0680-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Philippon MJ, Maxwell RB, Johnston TL, Schenker M, Briggs KK. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15:1041–1047. doi: 10.1007/s00167-007-0348-2. [DOI] [PubMed] [Google Scholar]
- 35.Casartelli NC, Leunig M, Item-Glatthorn JF, Lepers R, Maffiuletti NA. Hip flexor muscle fatigue in patients with symptomatic femoroacetabular impingement. Int Orthop. 2012;36:967–973. doi: 10.1007/s00264-011-1385-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Casartelli NC, Maffiuletti NA, Item-Glatthorn JF, Staehli S, Bizzini M, Impellizzeri FM, Leunig M. Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthritis Cartilage. 2011;19:816–821. doi: 10.1016/j.joca.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 37.Hurwitz DE, Hulet CH, Andriacchi TP, Rosenberg AG, Galante JO. Gait compensations in patients with osteoarthritis of the hip and their relationship to pain and passive hip motion. J Orthop Res. 1997;15:629–635. doi: 10.1002/jor.1100150421. [DOI] [PubMed] [Google Scholar]
- 38.Foucher KC, Schlink BR, Shakoor N, Wimmer MA. Sagittal plane hip motion reversals during walking are associated with disease severity and poorer function in subjects with hip osteoarthritis. J Biomech. 2012;45:1360–1365. doi: 10.1016/j.jbiomech.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 39.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA (2003) Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 417:112–120. doi:10.1097/01.blo.0000096804.78689.c2 [DOI] [PubMed]
- 41.Wagner S, Hofstetter W, Chiquet M, Mainil-Varlet P, Stauffer E, Ganz R, Siebenrock KA. Early osteoarthritic changes of human femoral head cartilage subsequent to femoro-acetabular impingement. Osteoarthritis Cartilage. 2003;11:508–518. doi: 10.1016/S1063-4584(03)00075-X. [DOI] [PubMed] [Google Scholar]
- 42.Eitzen I, Fernandes L, Nordsletten L, Risberg MA. Sagittal plane gait characteristics in hip osteoarthritis patients with mild to moderate symptoms compared to healthy controls: a cross-sectional study. BMC Musculoskelet Disord. 2012;13:258. doi: 10.1186/1471-2474-13-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Olsson E. Gait analysis in hip and knee surgery. Scand J Rehabil Med Suppl. 1986;15:1–55. [PubMed] [Google Scholar]
- 44.Hartofilakidis G, Bardakos NV, Babis GC, Georgiades G. An examination of the association between different morphotypes of femoroacetabular impingement in asymptomatic subjects and the development of osteoarthritis of the hip. J Bone Joint Surg Br. 2011;93:580–586. doi: 10.1302/0301-620X.93B5.25236. [DOI] [PubMed] [Google Scholar]
- 45.Hack K, Di Primio G, Rakhra K, Beaulé PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92:2436–2444. doi: 10.2106/JBJS.J.01280. [DOI] [PubMed] [Google Scholar]
- 46.Laborie LB, Lehmann TG, Engesæter IØ, Eastwood DM, Engesæter LB, Rosendahl K. Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology. 2011;260:494–502. doi: 10.1148/radiol.11102354. [DOI] [PubMed] [Google Scholar]
- 47.Şahin N, Atici T, Öztürk A, Özkaya G, Özkan Y, Avcu B. Prevalence of femoroacetabular impingement in asymptomatic contralateral hips in patients with unilateral idiopathic osteoarthritis. J Int Med Res. 2011;39:790–797. doi: 10.1177/147323001103900311. [DOI] [PubMed] [Google Scholar]
- 48.Sankar WN, Arden N, Kim YJ, Grodzinsky AJ, Sandell L, Scanzello C, Siebenrock KA. Staging of hip osteoarthritis for clinical trials on femoroacetabular impingement. J Am Acad Orthop Surg. 2013;21(Suppl 1):S33–S38. doi: 10.5435/JAAOS-21-07-S33. [DOI] [PubMed] [Google Scholar]