Abstract
The aims of this study were to 1) determine the relationships between BMI and the frequency of food cravings for different categories of foods, 2) examine the associations between cravings for different types of foods and self-reported, habitual intake of these foods, and 3) assess how these relationships differ by BMI. Six hundred and forty-six participants (55.7% female; 66.4% White; mean age 29.5±9.1 years; mean BMI 27.3±5.5 kg/m2) completed a comprehensive assessment battery including the Food Craving Inventory (FCI) and a semi-quantitative food frequency questionnaire (FFQ). There was a significant positive relationship between BMI and food cravings. There were significant positive associations of cravings for sweets, high fats, carbohydrates/starches, and fast-food fats on respective intake of these types of foods; however, there were no significant interactions between food cravings and BMI on the respective type of food intake. This study indicates significant positive relationships between specific categories of food cravings and habitual intake of those foods.
Keywords: Food cravings, food intake, nutrition, obesity
1. Introduction
Amidst the growing obesity epidemic, research on eating patterns, behaviors, and factors that influence food intake has proliferated. While there is consensus that being overweight (25 kg/m2 ≤ body mass index (BMI) < 30 kg/m2) or obese (BMI ≥ 30 kg/m2) is associated with high consumption of energy-dense foods, determinants of consumption behaviors are not well understood (Centers for Disease Control, 2013; Duffey, Gordon-Larsen, Jacobs, Williams, & Popkin, 2007; Pereira et al., 2005). In an effort to understand the determinants of over-consumption, researchers have increasingly focused on more specific eating constructs such as food cravings.
Food cravings, an intense desire to consume a certain food or food type that is difficult to resist, are unique because of their specificity (Weingarten & Elston, 1990, 1991). Yet, studies on food cravings have primarily focused on the relationships with intake of macronutrients and total energy (Gilhooly et al., 2007; Hill, Weaver, & Blundell, 1991; Lafay et al., 2001), and intake of a single food such as chocolate (e.g., Forman et al., 2007) or single food type such as sweets (e.g., Forman et al., 2013). While cravings are typically for high caloric foods, particular individuals may crave different types of food (e.g., sweets or fast-food) and the type of food craved may play an important role in consumption behaviors. These relationships may be especially important when considered within the context of weight status.
Though most people have experienced a food craving at some point (Hill & Heaton-Brown, 1994; Lafay et al., 2001), there is evidence that individuals who are obese have higher frequencies of food cravings than normal weight (BMI <25 kg/m2) individuals (Abilés et al., 2010; Franken & Muris, 2005; White, Whisenhunt, Williamson, Greenway, & Netemeyer, 2002). However, it is uncertain if higher food cravings relate to higher overall, habitual consumption of the types of foods craved. In a laboratory-based study, Martin et al. (2008) found that cravings for specific types of foods were significantly related to intake of similar food types among overweight and obese individuals (BMI > 29). They found that cravings for sweets correlated with intake of sweets (M & M’s® and jelly beans) but not with intake of fats (chips) and cravings for fats correlated only with intake of fats (regular potato chips). More research is indicated to clarify the relationships between food cravings and food intake, and to ascertain if there are variations by weight. Such knowledge can provide important insights for interventions to decrease the consumption of high calorie, energy-dense foods.
Thus, we examined the relationships between the frequency of food cravings for different categories of foods (high fats, sweets, carbohydrates/starches, and fast-food fats), habitual, self-reported intake of these foods and BMI. Our aims were to: 1) determine the relationships between BMI and the frequency of food cravings for different categories of foods, 2) examine the associations between cravings for different types of foods and self-reported, habitual intake of these foods, and 3) assess how these relationships differ by BMI. First, we hypothesized that the frequency for all types of food cravings would be positively associated with BMI. Second, we hypothesized that the relationship between cravings for different types of food and self-reported, habitual intake of these foods would be positively associated. Third, we hypothesized that these relationships would be stronger among individuals with a higher BMI. We expected to observe these differences after adjusting for age, gender, and race/ethnicity.
2. Materials and Methods
2.1 Participants
Participants were 646 adults enrolled in a larger set of studies assessing the role of stress, self-control and addictive behaviors, including overeating of high calorie foods. Participants were recruited from advertisements in local newspapers and flyers at community centers and churches in New Haven, Connecticut between December 2007 and May 2012. Inclusion criteria were that participants were between the ages of 18-50 years and able to read English at the sixth grade level. Exclusion criteria were dependence on any drug other than nicotine, use of prescribed medications for any psychiatric disorders, pregnancy, and medical conditions that would preclude participation in the study. Due to a low number of underweight individuals in this sample (n=4), participants with a BMI<18.5 kg/m2 were excluded from analysis.
The mean age of the sample was 29.5±9.1 years and 55.7% of the sample was female. The majority of the sample (66.4%) identified themselves as White, 21.1% as Black, 12.6% Other. The mean BMI was 27.3±5.5 kg/m2, and 39.6% of participants were normal weight, 33.3% were overweight, and 27.1% were obese.
2.2 Procedures
The Yale University Institutional Review Board reviewed and approved the parent studies. Study procedures were conducted at the Yale Stress Center. Potential participants completed an initial screening over the telephone or in person to determine eligibility as discussed in section 2.1. Substance dependence was assessed using the Structured Clinical Interview for DSM-IV (SCID) by researchers experienced in caring for individuals with substance abuse (American Psychiatric Association, 2000). These researchers also had training on how to administer and measure using the SCID. Following screening, eligible participants met with a research assistant for a 2-hour intake session to obtain informed consent and begin assessments. After the intake session, participants completed a comprehensive assessment battery of self-report questionnaires, which took a total of 8 to 12 hours to complete. Assessments were spread over three to four sessions to decrease questionnaire fatigue. Trained research assistants measured each participant’s height and weight using a standard procedure where the research assistant used a physician’s scale to determine weight and height rod to determine height. All participants were required to take off their shoes and remove anything heavy from their pockets prior to stepping on the scale. Participants received $20 for each assessment session.
2.3 Measures
2.3.1 Demographics/BMI
Demographic data for age, gender, and race/ethnicity were collected via a questionnaire designed for this study. A research nurse or trained research staff member calculated BMI from the measured heights and weights during the physical health assessment.
2.3.2 Food cravings
Food cravings were measured using the Food Craving Inventory (FCI), a 28-item self-report measure that assesses general and specific food cravings (White et al., 2002). This measure defines craving as “an intense desire to consume a particular food (or food type) that is difficult to resist.” Participants rated how often each food was craved over the past month on a 5-point Likert scale ranging from 1 (never) to 5 (always/almost every day). The FCI has four subscales: high fat foods (fried chicken, sausage, gravy, fried fish, bacon, cornbread, hot dogs, steak), sweets (brownies, cookies, candy, chocolate, donuts, cake, cinnamon rolls, ice cream), complex carbohydrates/starches (rolls, pancakes/waffles, biscuits, sandwich bread, rice, baked potato, pasta, cereal), and fast-food fats (hamburger, French fries, chips, pizza). The FCI has established content validity from experts in the field of eating behaviors, concurrent validity with the Conceptual Craving Scale (Hill et al., 1991) and disinhibition and hunger scales of the Three Factor Eating Questionnaire (TFEQ; Stunkard & Messick, 1985), and discriminant validity with the restraint scale of the TFEQ. The FCI has demonstrated acceptable internal consistency reliability and test-retest reliability in adults (White et al., 2002). Further psychometric support for the FCI has been established in diverse community and clinical samples (Barnes & Tantleff-Dunn, 2010; Barnes & White, 2010; White & Grilo, 2005). In the current study, Cronbach’s alpha was .93 for the total score and ranged from .70 to .85 for the subscales, indicating adequate internal consistency.
2.3.3 Semi-quantitative food frequency questionnaire
The nutrition questionnaire used in this study was modified from the self-report, semi-quantitative Food Frequency Questionnaire (FFQ) used in the Nurses’ Health Study (Willett et al., 1985). The questionnaire includes 104 items assessing current eating habits of basic foods (e.g., consumption of French fries, pizza, candy bars, cookies, brownies, cake, pie, hamburgers). It defines standard serving sizes and uses a 9-point Likert scale for frequency ranging from 1 (never, or less than once/month) to 9 (6+/day). Previous studies have established the validity of the FFQ with food diaries (Rimm et al., 1992; Salvini et al., 1989; Willett, 1998). In the current study, the Cronbach’s alpha was adequate for the sweets, high fats, and fast food scales (Cronbach’s alpha=.79, .70, .66 respectively); but was poor for the complex carbohydrates/starches scale (Cronbach’s alpha=.55).
2.4 Data Analysis
We performed data analyses using SPSS v.22 (SPSS Inc., Chicago, IL). Items from the FCI were compared and matched to items from the FFQ (e.g., the FCI item indicating cravings for chocolate was matched to intake of chocolate and candy bars containing chocolate). These items were used to form subscales that matched the FCI subscales as closely as possible. To test aim 1, we conducted a series of linear mixed models with correlated outcomes (Heck, Thomas, & Tabata, 2013; Hoffman & Rovine, 2007; Hox, 2010). This analysis was chosen as it accounts for non-independence among repeated observations for each participant. The dependent variables were the four types of food cravings and we used the main and interactional effects of BMI and each category of food craving. To test aim 2, we used a series of linear mixed models for correlated outcomes with the main effects of each type of food craving and dependent variables of each type of food intake. To test aim 3, we created interaction terms between each type of food craving and BMI. To explore whether each type of food craving was unique to the corresponding food intake (e.g., if cravings for sweets were significantly associated with cravings for sweets, high fats, fast-food fats, and/or complex carbohydrates/starches), we used a cross-level interaction model with interaction contrasts between each category of food craving and category of food intake in the mixed models (Heck et al., 2013). Coefficients in all models were estimated after adjusting for age, gender, and race/ethnicity (White, Black, Other). Each continuous independent variable was mean-centered before being entered into the models (Enders & Tofighi, 2007) and an unstructured correlation metric was used (Heck et al., 2013). Statistical significance for analyses was defined as a 2-sided p-value of <.05.
3. Results
3.1 Preliminary Analysis
The most craved categories of food were fast-food fats (M=2.29, SD=.79) and sweets (M=2.14, SD=.78), then carbohydrates/starches (M=1.86, SD=.70) and high fats (M=1.69, SD=.68). The highest craved foods were pizza (M = 2.65, SD = 1.04), chocolate (M = 2.62, SD = 1.30), and ice cream (M = 2.61, SD = 1.21). Most individuals (83.9%) indicated having cravings for pizza one or more times over the past month, 75.5% for ice cream, and 73.2% for chocolate. Bivariate correlations were calculated among the study variables. As shown in Table 1, there were moderate positive correlations among the four different types of food cravings (r(644)=.47-.66, p<.001) and four different types of unhealthy food groups (r(644)=.33-.66, p<.001). There was a weak, positive relationship between BMI and cravings for high fats (r(644)=.21, p<.001) and low, positive correlations with cravings for sweets, carbohydrates/starches, fast-food fats (r(644)=.13-.15, p<.05), and intake of high fats (r(644)=.16, p<.001). There were moderate, positive correlations between food cravings and intake for the respective type of food including high fats (r(644)=.51, p<.001), sweets (r(644)=.49, p<.001), carbohydrates/starches (r(644)=.25, p<.001), and fast-food fats (r(644)=.39, p<.001).
Table 1. Food Cravings, Food Intake, BMI, and Demographics: Correlations.
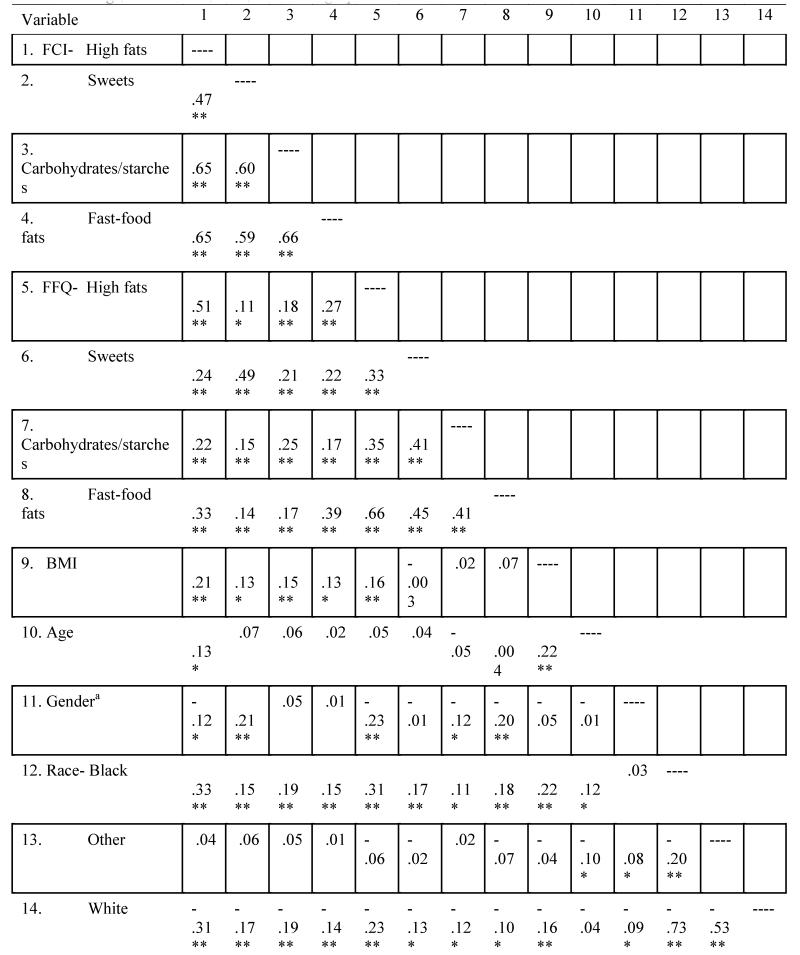
|
Note. Correlations for a community sample of adults (N=646). For all scales, higher scores indicate more extreme responding in the direction of the construct assessed. FCI=Food Craving Inventory; FFQ=Food Frequency Questionnaire; BMI=body mass index.
Gender: 0=Male, 1=Female
p < .05.
p < .001.
3.2 Relationship between Frequencies of Food Cravings and BMI
After adjusting for age, gender, and race/ethnicity, there was a significant main effect of BMI on food cravings (F(1, 2574)=10.70, p=.001) such that individuals with a higher BMI had higher frequencies of cravings (B=.01, SE=.004, p=.001, 95% CI=.01, .02). Furthermore, there was a significant relationship between food cravings, and age (F(1, 2571)=4.67, p=.03, B=.006, SE=.003, 95% CI=.001, .01) and race/ethnicity ((Black (F(1, 2571)=57.98, p<.001, B=.44, SE=.06, 95% CI=.33, .55), Other (F(1, 2571=8.88, p=.003, B=.21, SE=.07, 95% CI=.07, .35)). The effect of gender was non-significant. An interaction term was added to explore whether there were differences in these relationships depending on the category of food craving. This interaction term was non-significant (p>.05).
3.3 Associations between Food Cravings and Food Intake
There were statistically significant positive associations of cravings for high fats and fast-food fats on intake of unhealthy foods (p<.001, p=.001 respectively) and a negative association of cravings for carbohydrates/starches and intake of unhealthy foods (p<.001; Table 2). Being male and black were also statistically significantly positively associated with intake on unhealthy foods (p<.001).
Table 2. Linear Mixed-Effects Model for Food Intake.
| Main Effects Model | Cross-level Interaction Model | ||||
|---|---|---|---|---|---|
|
|
|||||
| Coefficient(SE) |
P-
value |
Coefficient(SE) |
P-
value |
||
| FCI- | High fats | 1.84(.22) | <.001 | .71(.25) | .005 |
| Sweets | 15(17) | .37 | −.07(.19) | .73 | |
| Carbohydrates/starches | −.78(.21) | <.001 | −.87(.24) | <.001 | |
| Fast-food fats | .62(.19) | .001 | 1.69(.21) | <.001 | |
| Age | −.01(.01) | .31 | −.01(.01) | .31 | |
| Gender | Male | 1.12(.21) | <.001 | 1.11(21) | <.001 |
| Race-Black | 1.18(.26) | <.001 | 1.17(.26) | <.001 | |
| Other | −.22(.30) | .46 | −.22(.30) | .46 | |
| Index 1 (High fats) | −.01(.09) | .89 | |||
| Index 2 (Sweets) | .02(.16) | .91 | |||
| Index 3 (Carbohydrates/starches) | −.03(.18) | .88 | |||
| Index 4 (Fast-food fats) | Ref | Ref | |||
| FCI High fats | *High fats | 2.37(.21) | <.001 | ||
| *Sweets | −.21(.35) | .55 | |||
| *Carbohydrates/starches | −.39(.39) | .33 | |||
| *Fast-food fats | Ref | Ref | |||
| FCI Sweets | *High fats | .05(.15) | .74 | ||
| *Sweets | 4.52(.28) | <.001 | |||
| *Carbohydrates/starches | .43(.31) | .17 | |||
| *Fast-food fats | Ref | Ref | |||
| FCI | *High fats | −.20(.21) | .34 | ||
| Carbohydrates/starches | *Sweets | −.29(.36) | .42 | ||
| *Carbohydrates/starches | 2.61(.40) | <.001 | |||
| *Fast-food fats | Ref | Ref | |||
| FCI Fast-food fats | *High fats | −1.69(.18) | <.001 | ||
| *Sweets | −2.35(.31) | <.001 | |||
| *Carbohydrates/starches | −2.11(.35) | <.001 | |||
| *Fast-food fats | Ref | Ref | |||
Indicates interaction term with food intake type
In the model that included cross-level interaction terms, there were differential effects on each type of food intake based on the type of food cravings. As expected, cravings for high fats were significantly associated with intake of high fat foods (p<.001) but were not significantly associated with intake of sweets, carbohydrates/starches, or fast-food fats. Cravings for sweets was significantly associated with intake of sweets but not with intake of high fats, carbohydrates/starches, or fast-food fats (p<.001) and cravings for carbohydrates/starches was significantly associated with intake of carbohydrates/starches (p<.001). Cravings for fast-food fats (reference category) were significantly negatively associated with all other types of food intake (p<.001).
3.4 Associations between Food Cravings, Food Intake, and BMI
Next, BMI was added into the main effects and cross-level interaction models. BMI was non-significantly associated with intake of unhealthy foods in the model (p>.05). Interaction terms were created to examine whether there were differences in the relationship between food cravings and food intake based on BMI. These interaction terms were all non-significant (p>05).
4. Discussion
This study expands the literature by examining associations between cravings for particular categories of foods and self-reported, habitual intake of those types of foods and the relationship with BMI in a diverse and large sample of adults from the community. We found that individuals with higher BMIs reported higher frequencies of food cravings. There were significant, positive associations of cravings for high fats, sweets, fast-food fats, and carbohydrates/starches on respective intake of those foods; however, there were no significant interaction effects observed between food cravings and BMI on the respective type of food intake.
Given prior literature suggesting positive associations between food cravings and weight status and our results supporting these findings (Delahanty, Meigs, Hayden, Williamson, & Nathan, 2002; White et al., 2002), the findings that the magnitude of associations between cravings and intake did not differ by BMI were unexpected. It is possible that normal weight and overweight individuals compensate for consumption of craved foods by reducing their caloric intake at other meals or increasing their physical activity to maintain their weight status. It is also possible that individuals with a higher BMI underreported their food intake.
It was also unexpected that there was a negative association of cravings for carbohydrates/starches and intake of unhealthy foods. It is possible that individuals who craved carbohydrates/starches may substitute these types of foods with healthier carbohydrates or may be able to better resist eating in response to these cravings; however, further research is necessary to examine these relationships.
Our results support and extend prior findings that food cravings and consumption are significantly related constructs (Martin, O’Neil, Tollefson, Greenway, & White, 2008; Weingarten & Elston, 1991; White, Whisenhunt, Williamson, Greenway, & Netemeyer, 2002). Previous studies also reported strong associations between cravings and intake of high fats, sweets, and fast-food fats (Forman, Hoffman, Juarascio, Butryn, & Herbert, 2013; Martin et al., 2008). Our findings extend these results to demonstrate that higher food cravings are related to higher habitual consumption of the types of foods craved and support the specificity of each type of food craving to the corresponding type of food intake. The use of a self-report measure allowed us to examine habitual intake. These results expand and corroborate the results that have been conducted in laboratory settings and give us indication of patterns over longer times and with a greater diversity and comprehensiveness of foods. These findings suggest that creating interventions to help individuals curb their cravings and resist food intake in response to those cravings, may be important in helping prevent the consumption of high calorie, energy dense foods.
Despite a large and diverse sample, these results should be interpreted in the context of several limitations. First, food intake was self-reported which may be subject to recall and response biases. Second, we compared cravings for specific types of foods with intake of these categories of food. It is possible that some food cravings may be quite specific to the individual food item rather than an entire food class. Third, this was a cross-sectional study and we cannot make any inferences about temporality. Craving frequencies were not related to intake frequencies on a specific occasion. Cravings could have occurred that were not followed by intake and intake could have occurred without cravings. It is also possible that cravings are conditioned phenomena: people may crave the foods that they frequently eat. Fourth, dietary preferences (i.e., vegetarian, gluten-free) were not assessed or accounted for in the analysis but may impact the foods that an individual craves and/or consumes. Fifth, the Cronbach’s alpha was low for the complex carbohydrate’s scale. Sixth, self-reported measures were used to examine the study constructs. Future work investigating these constructs using clinical interviews is warranted. Lastly, craving intensity was not measured but is likely an important factor influencing the relationship between food craving and food intake.
In conclusion, the results of this study suggest that there is a significant positive relationship between BMI and food cravings, and positive associations between cravings for sweets, high fats, carbohydrates/starches, and fast-food fats and respective intake of these types of foods. Future research examining biobehavioral mechanisms underlying food cravings, temporal relationships between food cravings and intake, and individual responses to cravings is warranted.
Highlights.
We examined food cravings and habitual food intake in a community sample of adults.
Individuals with a higher BMI had higher frequencies of food cravings.
Cravings were associated with respective intake of the craved food type.
Food cravings and BMI did not interact to estimate food intake.
Acknowledgments
Role of funding sources: The National Institute on Drug Abuse/National Institute of Health (NIH) grants PL1-DA024859 and UL1-DE019859 funded this study. AC was funded by pre-doctoral fellowships from the Jonas Center for Nursing Excellence and the National Institute of Nursing Research/NIH (T32-NR-008346-10; F31-NR014375). CMG was funded, in part, by K24DK070052. The above funding sources did not have a role in study design, collection, analysis and interpretation of the data, writing of the report, or in the decision to submit the article for publication.
Funding: The National Institute on Drug Abuse/National Institute of Health (NIH) grants PL1-DA024859 and UL1-DE019859 funded this study. AC was funded by pre-doctoral fellowships from the Jonas Center for Nursing Excellence and the National Institute of Nursing Research/NIH (F31-NR014375; T32-NR008346). CMG was funded, in part, by K24-DK070052.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors: Study concept and design: AC, CMG, MAW, RS. Acquisition and collection of data: RS. Analysis of data: AC. Obtained funding for study: RS. Administrative, technical, and material support: RS. All authors were involved in writing and revising the paper, and provided final approval of the manuscript.
Author Disclosures
Conflicts of Interest: The authors have declared no conflicts of interest
References
- Abilés V, Rodríguez-Ruiz S, Abilés J, Mellado C, García A, Pérez de la Cruz A, Fernández-Santaella MC. Psychological characteristics of morbidly obese candidates for bariatric surgery. Obesity Surgery. 2010;20(2):161–167. doi: 10.1007/s11695-008-9726-1. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM-IV-TR. American Psychiatric Pub; Washington, DC: 2000. [Google Scholar]
- Barnes RD, Tantleff-Dunn S. Food for thought: Examining the relationship between food thought suppression and weight-related outcomes. Eating Behaviors. 2010;11(3):175–179. doi: 10.1016/j.eatbeh.2010.03.001. [DOI] [PubMed] [Google Scholar]
- Barnes RD, White MA. Psychometric properties of the food thought suppression inventory in men. Journal of Health Psychology. 2010;15(7):1113–1120. doi: 10.1177/1359105310365179. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention About BMI for adults. 2011 Retrieved from http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/
- Delahanty LM, Meigs JB, Hayden D, Williamson DA, Nathan DM. Psychological and behavioral correlates of baseline BMI in the Diabetes Prevention Program (DPP) Diabetes Care. 2002;25(11):1992–1998. doi: 10.2337/diacare.25.11.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffey KJ, Gordon-Larsen P, Jacobs DR, Williams OD, Popkin BM. Differential associations of fast food and restaurant food consumption with 3-y change in body mass index: The Coronary Artery Risk Development in Young Adults Study. The American Journal of Clinical Nutrition. 2007;85(1):201–208. doi: 10.1093/ajcn/85.1.201. [DOI] [PubMed] [Google Scholar]
- Enders CK, Tofighi D. Centering predictor variables in cross-sectional multilevel models: a new look at an old issue. Psychological Methods. 2007;12(2):121–138. doi: 10.1037/1082-989X.12.2.121. [DOI] [PubMed] [Google Scholar]
- Forman EM, Hoffman KL, Juarascio AS, Butryn ML, Herbert JD. Comparison of acceptance-based and standard cognitive-based coping strategies for craving sweets in overweight and obese women. Eating Behaviors. 2013;14(1):64–68. doi: 10.1016/j.eatbeh.2012.10.016. [DOI] [PubMed] [Google Scholar]
- Forman EM, Hoffman KL, McGrath KB, Herbert JD, Brandsma LL, Lowe MR. A comparison of acceptance- and control-based strategies for coping with food cravings: An analog study. Behaviour Research and Therapy. 2007;45(10):2372–2386. doi: 10.1016/j.brat.2007.04.004. [DOI] [PubMed] [Google Scholar]
- Franken IH, Muris P. Individual differences in reward sensitivity are related to food craving and relative body weight in healthy women. Appetite. 2005;45(2):198–201. doi: 10.1016/j.appet.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Gilhooly CH, Das SK, Golden JK, McCrory MA, Dallal GE, Saltzman E, Kramer M, Roberts SB. Food cravings and energy regulation: The characteristics of craved foods and their relationship with eating behaviors and weight change during 6 months of dietary energy restriction. International Journal of Obesity. 2007;31(12):1849–1858. doi: 10.1038/sj.ijo.0803672. [DOI] [PubMed] [Google Scholar]
- Heck RH, Thomas SL, Tabata LN. Multilevel and longitudinal modeling with IBM SPSS. Routledge; New York, NY: 2013. [Google Scholar]
- Hill AJ, Heaton-Brown L. The experience of food craving: A prospective investigation in healthy women. Journal of Psychosomatic Research. 1994;38(8):801–814. doi: 10.1016/0022-3999(94)90068-x. [DOI] [PubMed] [Google Scholar]
- Hill AJ, Weaver CF, Blundell JE. Food craving, dietary restraint and mood. Appetite. 1991;17(3):187–197. doi: 10.1016/0195-6663(91)90021-j. [DOI] [PubMed] [Google Scholar]
- Hoffman L, Rovine MJ. Multilevel models for the experimental psychologist: Foundations and illustrative examples. Behavior Research Methods. 2007;39(1):101–117. doi: 10.3758/bf03192848. [DOI] [PubMed] [Google Scholar]
- Hox J. Multilevel analysis: Techniques and applications. Routledge; New York, NY: 2010. [Google Scholar]
- Lafay L, Thomas F, Mennen L, Charles MA, Eschwege E, Borys JM. Gender differences in the relation between food cravings and mood in an adult community: Results from the Fleurbaix Laventie Ville Sante study. International Journal of Eating Disorders. 2001;29(2):195–204. doi: 10.1002/1098-108x(200103)29:2<195::aid-eat1009>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Martin CK, O’Neil PM, Tollefson G, Greenway FL, White MA. The association between food cravings and consumption of specific foods in a laboratory taste test. Appetite. 2008;51(2):324–326. doi: 10.1016/j.appet.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira MA, Kartashov AI, Ebbeling CB, Van Horn L, Slattery ML, Jacobs DR, Ludwig DS. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. The Lancet. 2005;365(9453):36–42. doi: 10.1016/S0140-6736(04)17663-0. [DOI] [PubMed] [Google Scholar]
- Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. American Journal of Epidemiology. 1992;135(10):1114–1126. doi: 10.1093/oxfordjournals.aje.a116211. [DOI] [PubMed] [Google Scholar]
- Salvini S, Hunter DJ, Sampson L, Stampfer MJ, Colditz GA, Rosner B, Willett WC. Food-based validation of a dietary questionnaire: The effects of week- to-week variation in food consumption. International Journal of Epidemiology. 1989;18(4):858–867. doi: 10.1093/ije/18.4.858. [DOI] [PubMed] [Google Scholar]
- Stunkard AJ, Messick S. The Three-Factor Eating Questionnaire to measure dietary restraint, disinhibition and hunger. Journal of Psychosomatic Research. 1985;29(1):71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- Weingarten HP, Elston D. The phenomenology of food cravings. Appetite. 1990;15(3):231–246. doi: 10.1016/0195-6663(90)90023-2. [DOI] [PubMed] [Google Scholar]
- Weingarten HP, Elston D. Food cravings in a college population. Appetite. 1991;17(3):167–175. doi: 10.1016/0195-6663(91)90019-o. doi: 10.1016/0195-6663(91)90019-O. [DOI] [PubMed] [Google Scholar]
- White MA, Grilo CM. Psychometric properties of the Food Craving Inventory among obese patients with binge eating disorder. Eating Behaviors. 2005;6(3):239–246. doi: 10.1016/j.eatbeh.2005.01.001. [DOI] [PubMed] [Google Scholar]
- White MA, Whisenhunt BL, Williamson DA, Greenway FL, Netemeyer RG. Development and validation of the food-craving inventory. Obesity. 2002;10(2):107–114. doi: 10.1038/oby.2002.17. [DOI] [PubMed] [Google Scholar]
- Willett W. Nutritional epidemiology. Vol. 30. Oxford University Press; New York, NY: 1998. [Google Scholar]
- Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, Hennekens CH, Speizer FE. Reproducibility and validity of a semiquantitative food frequency questionnaire. American Journal of Epidemiology. 1985;122(1):51–65. doi: 10.1093/oxfordjournals.aje.a114086. [DOI] [PubMed] [Google Scholar]


