Abstract
Background:
Currently there is a paucity of information about biomarkers that can predict hospitalization for acute exacerbations of chronic obstructive pulmonary disease (AECOPD) patients presenting to the emergency department (ED). There is limited data on the consistency of ED management of AECOPD with local COPD guidelines. The aim of this study was to identify biomarkers associated with hospitalization in AECOPD patients and to determine if the ED management was concordant with local COPD guidelines.
Materials and Methods:
We performed a retrospective audit of consecutive AECOPD patients presenting to the Gold Coast Hospital ED over a 6-month period.
Results:
During the study period, 122 AECOPD patients (51% male, mean age (SE) 71 (±11) years) presented to the ED. Ninety-eight (80%) patients were hospitalized. Univariate analysis identified certain factors associated with hospitalization: Older age, former smokers, home oxygen therapy, weekday presentation, SpO2 < 92%, and raised inflammatory markers (white cell count (WCC) and C-reactive protein (CRP)). After adjustment for multiple variable, increased age was significantly associated with hospitalization (odds ratio (OR) 1.09; 95% confidence interval (CI): 1.00-1.18; P = 0.05). Radiology assessment and pharmacological management was in accordance with COPD guidelines. However, spirometry was performed in 17% of patients and 28% of patients with hypercapneic respiratory failure received noninvasive ventilation (NIV).
Conclusion:
We identified several factors on univariate analysis that were associated with hospitalization. Further research is required to determine the utility of these biomarkers in clinical practice. Also, while overall adherence to local COPD guidelines was good, there is scope for improvement in performing spirometry and provision of NIV to eligible patients.
Keywords: Emergencies, lung disease, obstructive
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality both in Australia[1] and worldwide.[2] It is estimated that about 2.1 million Australians suffer from COPD.[1] The clinical course of COPD is aggravated by exacerbations, characterized by increased cough, dyspnea, and production of purulent sputum.[3] Patients with an acute exacerbation of COPD (AECOPD) often present to the emergency department (ED) and many subsequently require hospitalization for ongoing management. In 2008-2009, COPD-related hospitalization accounted for 56,201 hospital admissions for Australians aged 55 years and over.[4] In this context, it is estimated that COPD is the second leading cause of avoidable hospital admissions in Australia.[5]
Clinical guidelines have been developed and widely promoted to assist ED and hospital and community clinicians in providing evidence-based management for AECOPD patients. Most prominent among them are the Global Initiative for COPD (GOLD), National Institute for Clinical Excellence (NICE) clinical guideline on management of COPD,[6,7] and the COPD-X Plan (specifically for Australia and New Zealand).[8] The COPD-X plan provides recommendations to assist clinicians in confirming the exacerbation and categorizing severity (spirometry, blood gas measurements, chest X-ray, and electrocardiography) and optimizing treatment (bronchodilators, glucocorticoids, antibiotics, controlled oxygen therapy, and ventilatory assistance).[9] Adherence to guideline-based management of AECOPD is not only expected to achieve good outcomes for the immediate treatment of the exacerbation, but also long-term outcomes such as lung function, morbidity, and mortality.[3] To date there have only been a few ED validation studies of the COPD management guidelines.[10,11,12] To the best of our knowledge there has been only one Australian study, which was a retrospective audit performed across five Melbourne EDs.[10] However, the study only measured compliance with evidence-based recommendations regarding use of bronchodilators, methylxanthines, steroids, and noninvasive ventilation (NIV).[10] More recent studies on the actual standards of clinical care provided to AECOPD patients in the ED are lacking.
The current study examined the characteristics, assessment, management, and outcome of AECOPD presentations to a large regional Australian hospital ED. The objective of the study was to determine the factors associated with hospitalization and to examine compliance with the COPD-X Plan 2011[9] recommendations (most current version at the time of the study) for assessment and management of AECOPD patients.
MATERIALS AND METHODS
A retrospective cohort study was conducted at the Gold Coast Hospital, Southport Campus. This is a 570-bed major regional teaching hospital with all major specialties, except for cardiac surgery and burns. The ED of the Gold Coast Hospital provides care for a mixed adult and pediatric (approximately 70 and 30%, respectively) population. In 2012, there were more than 67,000 presentations to the Gold Coast Hospital ED. Included in the study were adult patients (age ≥ 18 years) diagnosed with COPD by a medical practitioner, who had presented to the ED over a 6-month period (December 15, 2011-June 15, 2012). COPD patients whose primary reason for admission was not due to an acute exacerbation were excluded from the study. When patients presented with AECOPD more than once in the study period, only the first presentation was used for the primary analysis. The Gold Coast Health Services District Human Research Ethics Committee approved the study (Ethics Reference Number: HREC/12/QGC/99).
Potential study subjects were identified on the basis of International Classification of Diseases (ICD)-10 codes of E65A and E65B (complex and noncomplex COPD). Eligible patients’ electronic medical record (EMR) entries, ED information system (EDIS) records, and electronic discharge summaries were reviewed. Biochemistry results were obtained through the AUSLAB laboratory information system. The following information was collected:
Patient demographics (age, gender, smoking status, living situation, and comorbidities)
Characteristics of underlying disease (oxygen therapy at home and COPD-related hospital admissions in the preceding 12 months)
Features of current exacerbation (day of week of presentation, clinical symptoms on presentation, and vital signs)
Investigations performed in ED (spirometry, chest X-ray, full blood counts, biochemistry, and blood gas analysis)
Treatments provided in ED (oxygen, systemic steroids, antibiotics, and bronchodilators)
Outcomes (admission or discharge from ED)
Follow-up: COPD-related ED presentations over the subsequent 3 months.
According to the COPD-X Plan, NIV is indicated for severe dyspnea that responds inadequately to initial emergency therapy, confusion, lethargy or evidence of hypoventilation, persistent or worsening hypoxemia despite supplemental oxygen, worsening hypercapnia (PaCO2 > 70 mmHg), or severe or worsening respiratory acidosis (blood pH < 7.3). However, the strongest indication for NIV in AECOPD patients is for acute hypercapnic respiratory failure (arterial blood pH of less than 7.35 and PaCO2 >45 mmHg). Adherence to the COPD-X Plan regarding the evaluation and treatment of AECOPD was assessed.[9]
Statistical analysis
All statistical analyses were performed using Statistical Package for Social Sciences (SPSS) version 20.0 (SPSS, Chicago, IL, USA). Kolmogorov-Smirnov and Shapiro-Wilk tests were used to assess for normality of the data. Normally distributed data was analyzed for differences between individual groups using the Student's t-test and presented as mean and standard error. Nonparametric data was analyzed for differences between groups using the Mann-Whitney U test and results expressed as median and interquartile range. Logistic regression analysis was used to identify factors associated with hospitalization. Variables from the univariate analysis that which had P-values < 0.05 were evaluated for the multivariate logistic regression analysis. Statistical significance was indicated by P-value of less than 0.05.
RESULTS
During the 6-month study period, 188 patients were identified using the ICD-10 codes. After review of the medical case records, 12 presentations were excluded from analysis as they were found to be either incorrectly coded or AECOPD was not the primary reason for presentation to the ED. Final analysis was performed on 122 patients who had 176 AECOPD presentations. Baseline characteristics and information about the ED presentation and management are summarized in Table 1. Mean age (± standard error (SE)) of the patients was 71 (±11) years and 51% were male. Twenty-eight percent of patients were living alone and 23% were current smokers. One-third of patients used home oxygen therapy and almost 40% of patients had been hospitalized for AECOPD in the preceding 12 months.
Table 1.
Demographic and baseline clinical characteristics of patients presenting to the emergency department according to hospitalization status
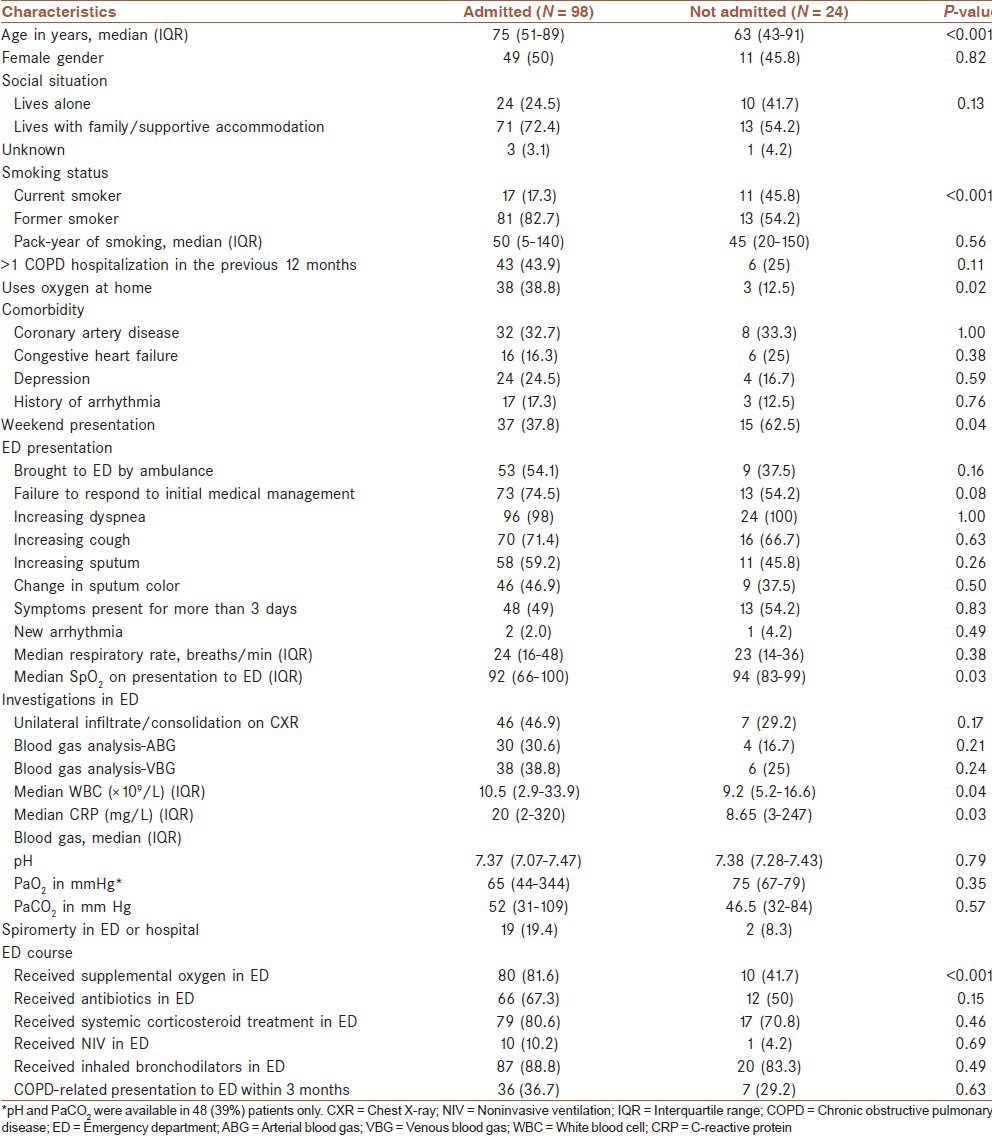
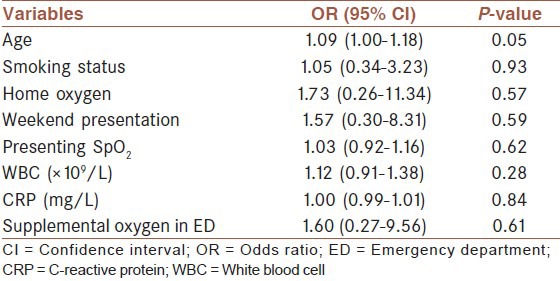
Eighty percent of AECOPD patients who presented to the ED were hospitalized. Admitted patients in comparison to discharged patients, were older (75 vs 65 years, P = 0.005), received home oxygen (39 vs 13%, P = 0.016), presented on a weekday (62 vs 37%, P = 0.038), had lower oxygen saturations (median SpO2, 92 vs 94%, P = 0.034), and had a higher median white cell count (WCC; ×109/L) (10.5 vs 9.2, P = 0.046) and C-reactive protein (CRP; 20 vs 8.65 mg/L, P = 0.032). AECOPD patients who were eventually hospitalized received supplemental oxygen (82 vs 42%, P < 0.001) and systemic corticosteroids (81 vs 71%, P = 0.046), more often compared to AECOPD patients who were discharged from the ED. Overall, 34% (n = 43) of patients represented within the study period with another episode of AECOPD, but this proportion of representations was the same between the hospitalized patients compared to patients who were discharged from the ED (representation rate: 37 vs 29%, P = 0.635). Multivariate analysis was performed on the predictors of admission [Table 2]. Among the variables, only increased age was independently associated with hospitalization (odds ratio (OR) 1.09; 95% confidence interval (CI): 1.00-1.18; P = 0.05).
Table 2.
Odds ratio by binary logistic regression for hospitalization
Overall, adherence to the COPD-X Plan guideline was good [Table 3]. Adherence to guideline recommendations regarding chest radiographs was excellent (100%). Most patients received bronchodilators (88%) and systemic corticosteroids (79%), but only 67% of patients with appropriate indications, received antibiotics. There was also good adherence to the guideline recommendations for hospitalization. The majority of patients with marked increase in intensity of symptoms or those who had failed to improve with ambulatory treatment (75%) and had worsening hypoxia (88%) were hospitalized. However, adherence to certain guideline recommendations was suboptimal: Objective measurement of pulmonary function, while in the ED was obtained in only 17% of patients and evaluation of arterial blood gases was performed in only 28% overall. However, when only patients with a severe exacerbation (SpO2 < 92%) are considered, an arterial (ABG) or venous blood gas (VBG) analysis was performed in 77% of patients.
Table 3.
Observed frequencies for diagnostic procedures and clinical management of AECOPD patients in the ED
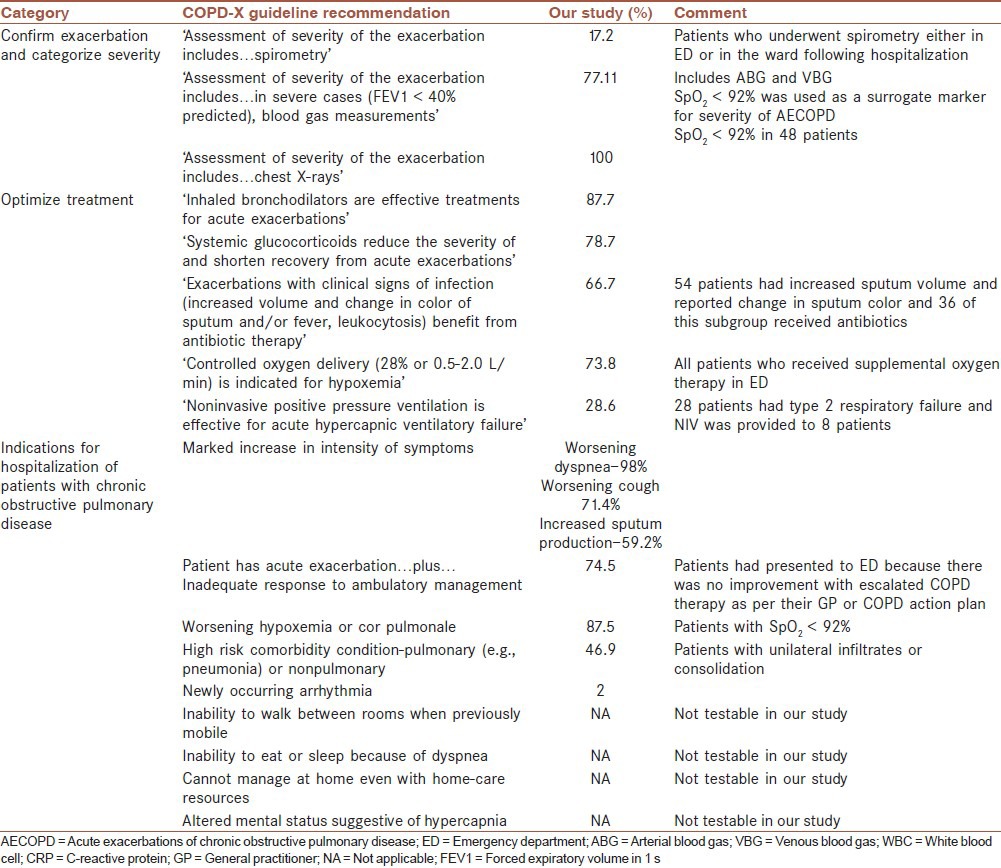
Using an arterial blood pH of less than 7.35 as the cutoff value, there were 39 admissions where treatment via NIV was indicated. The median (interquartile range (IQR)) PaCO2 for these 39 admissions was 59 (48-102) mmHg. Despite suitable NIV equipment being available, this treatment was provided for only 11 (29%) patients. Interestingly there was no documentation as to reasons why NIV was not provided to the 71% (n = 28) of patients with type 2 respiratory failure.
DISCUSSION
Our study evaluated the ED management in patients with an AECOPD over a 6-month period in a regional tertiary hospital. Eighty percent of these patients were hospitalized. Overall there was good adherence to many of the recommendations of the COPD-X Plan. However, there are certain clinical management areas with potential for improvement. We identified several factors in AECOPD patients that were associated with hospitalization. This may facilitate future ED management of AECOPD patients.
In our study, 80% of COPD patients presenting to ED were hospitalized, which is similar to previous reports.[10,13] A better understanding of the factors associated with hospitalization may translate to more rapid decision making for ‘at risk’ patients, resulting in less time spent in the ED and better clinical outcomes. This is of particular interest with the introduction of the National Emergency Access Target (NEAT) to address growing ED demand (http://www.health.gov.au and http://www.ecinsw.com.au/neat). However, currently there are no reliable methods of risk stratification for patients with COPD exacerbations presenting to the ED. Recently, Garcia-Sanz et al.,[14] evaluated 409 exacerbations in 239 COPD patients over a 12-month period and found that impaired oxygenation, presence of neutrophilia, and administration of antibiotics in ED were associated with hospitalization. Interestingly, impaired oxygenation and neutrophilia were associated with hospitalization in our study as well. We also found that an elevated CRP was also associated with hospital admission. CRP is an inflammatory biomarker that has been previously been associated with severe COPD.[15,16] Furthermore, in COPD exacerbations, raised CRP has been associated with bacterial infections[17] and adverse clinical outcomes.[18] Hence it is not surprising that a raised CRP is a biomarker for severe AECOPD exacerbations that require hospital admissions. We found that hospital admission occurred more frequently during weekdays compared with weekends, potentially due to patients postponing presentation till after the weekend or review by own general practitioner (GP). Our results are consistent with those of a recent large multicenter study of nine EDs, which reported that a weekday presentation was associated with longer length of stay in ED and increased likelihood of hospitalization.[19]
Interestingly, we found that while the alterations in the individual variables were associated with admission, only increased age was significantly associated with hospitalization. Other variables did not achieve statistical significance. This is most likely due to the relatively small sample size in our study. The clinical utility of ED physicians being aware of these admission associated factors in improving outcomes for AECOPD patients will need to be evaluated in multicenter prospective studies. If validated, then the factors may need to be incorporated into future versions of AECOPD guidelines.
In this study, we found generally good concordance of ED management with guideline recommendations, such as the testable indicators for hospitalization in the COPD-X Plan. Not unexpectedly we found that older age and home oxygen therapy were associated with hospitalization. These two factors, while not present in the COPD-X Plan, are recommended in international COPD guidelines.[6,7] With regards to treatment given in the ED, bronchodilators, systemic corticosteroids, and antibiotics were provided in the great majority of patients. These results are consistent with a previous study of Australian EDs, with our study having a higher prescription rate of systemic corticosteroids (79 vs 57%).[10] The higher adherence to guideline recommendations in our study maybe explained in part by the different time periods of the two studies (2011-2012 vs 2006-2007[10]). The trend for increased prescription of systemic steroids more recently is consistent with the findings of Tsai et al., who noted that between 2000 and 2005-2006, there was an increased prescriptions of systemic corticosteroids and antibiotics in a Boston ED.[13] This finding may be due to increased awareness of guideline recommendations among ED physicians.
As per the COPD-X guidelines, the appropriate management of hypercapneic respiratory failure begins with the performance of an arterial blood gas (ABG) when the forced expiratory volume in 1 s (FEV1) is less than 1.0 L or less than 40% of predicted or if there are any signs of respiratory failure or cor pulmonale.[9] Overall we found that an ABG was performed in 28% of patients, but that a blood gas analysis (ABG and/or VBG) was performed in hypoxic patients in 77% of patients. In our experience, the decision to perform a blood gas analysis is based on baseline oxygen saturations and clinical acumen rather than spirometric values. In our study, a sizeable proportion of patients had a VBG instead of an ABG. The practice of measuring VBG in AECOPD patients is supported by recent studies, which have shown that a VBG in conjunction with oxygen saturation has similar clinical utility to an ABG in identifying hypercapneic respiratory failure.[20,21,22] So, we found that even though spirometry in ED was not performed commonly, the decision to perform (arterial or venous) blood gas analysis was based on appropriate clinical judgment.
The benefits of NIV in the treatment of hypercapneic respiratory failure in AECOPD include improved survival, reduced length of stay, and need for intubation.[23] However in our study NIV was provided to only 29% of eligible patients. Interestingly, very similar results have been reported in other national and international COPD audits.[24,25,26,27] Previous studies have also noted that often no reason is provided in the medical notes as to why NIV is not provided to eligible patients. Possible explanations for such low provision of NIV in eligible patients include a poor understanding of the clinical indications for NIV, limited experience and/or lack of staff education.[26] Educational initiatives including checklists have been shown to improve adherence to guidelines in the provision of NIV for eligible patients.[28] Further study is required to understand why NIV provision is low in ED (both in Australia and worldwide) and measures that need to be undertaken to improve this practice.
We found that spirometry had been performed in the ED in only 17% of patients. This is particularly divergent from the COPD-X Plan which recommends that spirometry can be performed even in the sickest of patients, unless they are confused or comatose.[9] It has been suggested that increased rates of spirometry either at presentation or at some stage during the admission could be expected to allow better characterization of disease severity, and hence improved management.[26] However, the feasibility and accuracy of spirometry in the ED has been questioned in the GOLD guidelines[29] and it has been noted that it is rarely performed in the ED.[11] An alternative to consider for future studies will be to obtain an accurate assessment of smoking history, and to use this information as a proxy measure of spirometry since pack-years of smoking is a surrogate measure of the severity of COPD.[11,30]
We acknowledge that our study design and results have several limitations. First, because our study is a retrospective review of medical records it suffers from the principal assumption that documentation is an accurate reflection of clinical practice. Second, it is possible that by using ICD codes as a strategy of identifying COPD patients for our study, we may have missed patients due to the problems of underreporting, incorrect EDIS diagnosis, and/or ICD coding. We identified 176 ED presentations in 6 months which equates to approximately 7.6 per 1,000 presentations, which is similar to reports in the US where COPD accounts for 10 per 1,000 ED presentations.[31] Third, since we did not interview ED physicians, we cannot determine if there were individual physician factors that may have been associated with hospitalization. Fourth, potentially important measurements were not obtained in all patients, particularly spirometry and blood gas analysis. However, since our study was designed to study actual ‘real-world’ ED practice, we do not consider this to be a study-related problem.
CONCLUSION
We also identified several factors that are associated with hospital admission. Awareness of these factors in the design of future AECOPD management guidelines may allow ED physicians to triage patients who are likely to be admitted rapidly and efficiently. We also found that in general, ED clinicians adhered well to the COPD-X Plan for management of AECOPD patients. However there is scope for improvement in the performance of spirometry and provision of NIV to be more in concordance with national COPD guidelines.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Access Economics Pty Limited; 2008. Oct, Economic Impact of COPD and cost effective solutions. [Google Scholar]
- 2.Halbert RJ, Natoli JL, Gano A, Badamgarav E, Buist AS, Mannino DM. Global burden of COPD: Systematic review and meta-analysis. Eur Respir J. 2006;28:523–32. doi: 10.1183/09031936.06.00124605. [DOI] [PubMed] [Google Scholar]
- 3.Decramer M, Janssens W, Miravitlles M. Chronic obstructive pulmonary disease. Lancet. 2012;379:1341–51. doi: 10.1016/S0140-6736(11)60968-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.AIHW. Canberra: AIHW; 2011. Australian hospital statistics 2009-10. [Google Scholar]
- 5.Glover J, Ambrose S, Page A, Tennant S. PHIDU. Adelaide: The University of Adelaide; 2008. Atlas of potentially avoidable hospitalisations in South Australia. [Google Scholar]
- 6.Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176:532–55. doi: 10.1164/rccm.200703-456SO. [DOI] [PubMed] [Google Scholar]
- 7.National Institute for Clinical Excellence; 2004. N.I.C.E. Management of Chronic Obstructive Pulmonary Disease in Adults in Primary and Secondary Care. [Google Scholar]
- 8.McKenzie DK, Frith PA, Burdon JG, Town GI. Australian Lung Foundation, Thoracic Society of Australia and New Zealand. The COPDX Plan: Australian and New Zealand guidelines for the management of Chronic Obstructive Pulmonary Disease. Med J Aust. 2003;178:S7–39. doi: 10.5694/j.1326-5377.2003.tb05213.x. [DOI] [PubMed] [Google Scholar]
- 9.McKenzie DK, Abramson M, Crockett AJ, et al. The COPD-X Plan: Australian and New Zealand Guidelines for the management of Chronic Obstructive Pulmonary Disease. The Australian Lung Foundation. 2011 [Google Scholar]
- 10.Considine J, Botti M, Thomas S. Emergency department management of exacerbation of chronic obstructive pulmonary disease: Audit of compliance with evidence-based guidelines. Intern Med J. 2011;41:48–54. doi: 10.1111/j.1445-5994.2009.02065.x. [DOI] [PubMed] [Google Scholar]
- 11.Tsai CL, Clark S, Cydulka RK, Rowe BH, Camargo CA. Factors associated with hospital admission among emergency department patients with chronic obstructive pulmonary disease exacerbation. Acad Emerg Med. 2007;14:6–14. doi: 10.1197/j.aem.2006.07.034. [DOI] [PubMed] [Google Scholar]
- 12.Cydulka RK, Rowe BH, Clark S, Emerman CL, Camargo CA. On behalf of the mi. emergency department management of acute exacerbations of chronic obstructive pulmonary disease in the elderly: The Multicenter Airway Research Collaboration. J Am Geriatr Soc. 2003;51:908–16. doi: 10.1046/j.1365-2389.2003.51302.x. [DOI] [PubMed] [Google Scholar]
- 13.Tsai CL, Ginde AA, Blanc PG, Camargo CA. Improved care of acute exacerbation of chronic obstructive pulmonary disease in two academic emergency departments. Int J Emerg Med. 2009;2:111–6. doi: 10.1007/s12245-009-0089-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garcia-Sanz M, Pol-Balado C, Abellas C, Canive-Gomez J, Anton-Sanmartin D, Gonzalez-Barcala F. Factors associated with hospital admission in patients reaching the emergency department with COPD exacerbation. Multidisciplinary Respir Med. 2012;7:6. doi: 10.1186/2049-6958-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dev D, Wallace E, Sankaran R, Cunniffe J, Govan JR, Wathen CG, et al. Value of C-reactive protein measurements in exacerbations of chronic obstructive pulmonary disease. Respir Med. 1998;92:664–7. doi: 10.1016/s0954-6111(98)90515-7. [DOI] [PubMed] [Google Scholar]
- 16.Zhang Y, Bunjhoo H, Xiong W, Xu Y, Yang D. Association between C-reactive Protein Concentration and Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-analysis. J Int Med Res. 2012;40:1629–35. doi: 10.1177/030006051204000501. [DOI] [PubMed] [Google Scholar]
- 17.Peng C, Tian C, Zhang Y, Yang X, Fan H, Feng Y. C-Reactive protein levels predict bacterial exacerbation in patients with chronic obstructive pulmonary disease. Am J Med Sci. 2013;345:190–4. doi: 10.1097/MAJ.0b013e318253c921. [DOI] [PubMed] [Google Scholar]
- 18.Ruiz-Gonzalez A, Lacasta D, Ibarz M, Martinez-Alonso M, Falguera M, Porcel JM. C-reactive protein and other predictors of poor outcome in patients hospitalized with exacerbations of chronic obstructive pulmonary disease. Respirology. 2008;13:1028–33. doi: 10.1111/j.1440-1843.2008.01403.x. [DOI] [PubMed] [Google Scholar]
- 19.Wiler JL, Handel DA, Ginde AA, Aronsky D, Genes NG, Hackman JL, et al. Predictors of patient length of stay in 9 emergency departments. Am J Emerg Med. 2012;30:1860–4. doi: 10.1016/j.ajem.2012.03.028. [DOI] [PubMed] [Google Scholar]
- 20.Kelly AM, McAlpine R, Kyle E. Venous pH can safely replace arterial pH in the initial evaluation of patients in the emergency department. Emerg Med J. 2001;18:340–2. doi: 10.1136/emj.18.5.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kelly AM, Kyle E, McAlpine R. Venous pCO2 and pH can be used to screen for significant hypercarbia in emergency patients with acute respiratory disease. J Emerg Med. 2002;22:15–9. doi: 10.1016/s0736-4679(01)00431-0. [DOI] [PubMed] [Google Scholar]
- 22.Lim BL, Kelly AM. A meta-analysis on the utility of peripheral venous blood gas analyses in exacerbations of chronic obstructive pulmonary disease in the emergency department. Eur J Emerg Med. 2010;17:246–8. doi: 10.1097/MEJ.0b013e328335622a. [DOI] [PubMed] [Google Scholar]
- 23.Ram Felix SF, Picot J, Lightowler J, Wedzicha Jadwiga A. Cochrane Database Syst Rev. John Wiley & Sons, Ltd; 2004. Non-invasive positive pressure ventilation for treatment of respiratory failure due to exacerbations of chronic obstructive pulmonary disease. [DOI] [PubMed] [Google Scholar]
- 24.Hosker H, Anstey K, Lowe D, Pearson M, Roberts CM. Variability in the organisation and management of hospital care for COPD exacerbations in the UK. Respir Med. 2007;101:754–61. doi: 10.1016/j.rmed.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 25.Lodewijckx C, Sermeus W, Vanhaecht K, Panella M, Deneckere S, Leigheb F, et al. Inhospital management of COPD exacerbations: A systematic review of the literature with regard to adherence to international guidelines. J Eval Clin Pract. 2009;15:1101–10. doi: 10.1111/j.1365-2753.2009.01305.x. [DOI] [PubMed] [Google Scholar]
- 26.Pretto JJ, McDonald VM, Wark PA, Hensley MJ. Multicentre audit of inpatient management of acute exacerbations of chronic obstructive pulmonary disease: Comparison with clinical guidelines. Intern Med J. 2012;42:380–7. doi: 10.1111/j.1445-5994.2011.02475.x. [DOI] [PubMed] [Google Scholar]
- 27.Roberts CM, Ryland I, Lowe D, Kelly Y, Bucknall CE, Pearson MG. Audit Sub-committee of the Standards of Care Committee, British Thoracic Society, Clinical Effectiveness and Evaluation Unit, Royal College of Physicians. Audit of acute admissions of COPD: Standards of care and management in the hospital setting. Eur Respir J. 2001;17:343–9. doi: 10.1183/09031936.01.17303430. [DOI] [PubMed] [Google Scholar]
- 28.Sen B, Woollard M, Desira NL. Does the Introduction of a COPD Pro-Forma Improve the Standards of Care Delivered by Junior Doctors in the Emergency Department. COPD. 2010;7:199–203. doi: 10.3109/15412555.2010.481699. [DOI] [PubMed] [Google Scholar]
- 29.Vestbo J, Hurd SS, Agusti AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease, GOLD Executive Summary. Am J Respir Crit Care Med. 2013;187:347–65. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 30.Burrows B, Knudson RJ, Cline MG, Lebowitz MD. Quantitative relationships between cigarette smoking and ventilatory function. Am Rev Respir Dis. 1977;115:195–205. doi: 10.1164/arrd.1977.115.2.195. [DOI] [PubMed] [Google Scholar]
- 31.Mannino DM, Homa DM, Akinbami LJ, Ford ES, Redd SC. Chronic obstructive pulmonary disease surveillance—United States, 1971-2000. MMWR Surveill Summ. 2002;51:1–16. [PubMed] [Google Scholar]


