Abstract
Objectives
The influence of body size on dialysis-related mortality among Asians and Pacific Islanders - heterogeneous ethnic groups with dissimilar body compositions - is poorly understood. Our study objective was to compare the relations of body size and mortality among patients with end-stage renal disease of different ethnicities.
Design, setting, and participants
We examined data from a cohort of 21,492 adult Asians, Pacific Islanders and non-Hispanic Whites who initiated dialysis during 1995–2003 within California, Hawaii and the US Pacific Islands.
Main outcome measure
Time to death through September 22, 2008.
Results
Among both men and women, Pacific Islanders were the heaviest and Whites the tallest of the ethnic groups examined. Annual mortality rates were highest among Whites (29.6%), intermediate among Pacific Islanders (18.8%) and lowest among Asians (17.3%). Larger body size was associated with lower mortality among Pacific Islanders, Whites and most Asians on dialysis after adjustment for patient-level sociodemographic and clinical factors, area-based socioeconomic status and geographic clustering. Filipinos were the exception to this rule and showed a trend towards higher mortality with increasing body size. These findings were consistent irrespective of how body size was measured.
Conclusions
Larger body size is associated with lower mortality among Pacific Islanders, Whites and most Asians on dialysis. Use of disaggregated ethnicity data may enhance our understanding of how ethnicity- or community-specific factors influence body size, body composition and dialysis-related outcomes in these diverse populations.
Keywords: ESRD, Body Size, Obesity, Mortality, Ethnicity, Asian, Pacific Islander
Introduction
In contrast to observations from the general US population, larger body size as measured by Quetélet’s body mass index (BMI) is associated with enhanced survival in end-stage renal disease (ESRD).1–5 Where higher BMI reflects lean as well as adipose tissue, larger body size may reflect better physical health and nutritional status, rather than obesity per se.6 Indeed, ample energy stores in the form of adipose tissue may be protective in the face of chronic inflammatory conditions such as ESRD, that may be accompanied by anorexia and wasting.7
Body composition may confound weight-per-height indices such as BMI.8,9 While the BMI is the most widely used obesity index, Benn demonstrated that a more flexible, population-specific index, W/Hρ (where exponent ρ is derived from a specific set of weight-height measurements) is independent of height and thus may better reflect adiposity.9 In many populations, BMI is directly correlated with height and thus may not accurately represent obesity.9 Prior US-based studies in ESRD have suggested that BMI-survival relations may differ among jointly classified Asians and Pacific Islanders compared with other ethnicities.3,10 Studies from Asia in the general population have also described higher degrees of body fat at every level of BMI among some Asian subgroups compared with European Whites.11 Thus, the potential effects of excess body fat – both positive and negative – may differ among Asians and Pacific Islanders, populations with dissimilar body compositions who are frequently classified into a single ethnic category in epidemiological studies.
We hypothesized that the influence of adiposity on patient survival (positive from increased energy stores and negative from adverse hormonal and metabolic effects) differs in ESRD according to ethnicity. We further hypothesized that in some ethnic groups, Benn’s rather than Quetélet’s index may more accurately reflect these effects. To address these issues, we examined the associations of body size, ethnicity and mortality among 22,152 incident Asian, Pacific Islander and non-Hispanic White dialysis patients from the Western Pacific Renal Network (ESRD Network 17).
Methods
Data Sources
We obtained patient-level data by linking identifiers from ESRD Network 17 with the United States Renal Data System (USRDS) registry. Network 17 collects and maintains regional data for patients with ESRD receiving care in the 45 counties of central and northern California, Hawaii, American Samoa, Guam and the Mariana Islands. We extracted patient-level data from the USRDS Core CDs. We obtained area-based socioeconomic data from the 2000 US Census at the level of the zip code. Institutional review boards at the collaborating institutions approved the study.
Study Sample
We identified all patients aged ≥18 years who initiated dialysis in Network 17 between April 1, 1995 and September 30, 2003 (n=33,063). Approximately 35% of all US Asians and Pacific Islanders receive dialysis care within this network. We excluded patients who self-identified themselves as Hispanic (n=6033), Black (n=4702), American Indian or other ethnicity (n=123), and patients who were missing an ethnicity determination (n=8). We further excluded 522 patients whose height or weight measurements fell into the upper and lower one percent of values (extreme outliers) and those whose zip code of residence could not be linked to a Census tabulation area (n=149). The analytic sample consisted of the remaining 21,492 patients.
Outcome Variable
The primary outcome was time from dialysis initiation to death. Because the risk of death is modified by receipt of a kidney transplant, we censored patients at the time of living (n=820) or deceased (n=1973) donor kidney transplantation or at the end of the study observation period on September 22, 2008.
Primary Explanatory Variables
The primary explanatory variables for all analyses were body size and patient self-reported ethnicity. We examined two weight per height indices: Quetélet’s body mass index, calculated as weight (kg) divided by height (m2), and Benn’s index, calculated as weight (kg) divided by height in meters to the exponent ρ, calculated within each ethnicity classification.8 We divided patients into World Health Organization (WHO)-designated categories of BMI (<18.5, 18.5–24.9, 25–29.9 and ≥30 kg/m2), while considering an additional category for the sizable fraction of patients with BMI ≥35, and into ethnicity-specific quintiles of Benn’s index. Patients were classified as Asian (Asian Indian, Chinese, Filipino, Japanese, Korean, and Vietnamese), Pacific Islander (Chamorro, Native Hawaiian, Samoan and other Pacific Islanders), or non-Hispanic White. We used ethnicity data from Network 17 in preference to data supplied by USRDS because Network 17 independently collected self-reported ethnicity from incident dialysis patients during this time frame.12
Patient-level Covariates
Additional patient-level sociodemographic covariates included age, sex, and health insurance coverage (Medicare, Medicaid, employer group insurance, other insurance or no insurance). We estimated comorbidity burden using the Charlson index13 based on the following conditions from the USRDS Medical Evidence form: cardiovascular disease (CVD), chronic lung disease, diabetes (insulin- or non-insulin-requiring), HIV/AIDS, hypertension, peripheral arterial disease, poor functional status, and drug or tobacco use at the time of dialysis initiation. We further identified patients who were prescribed erythropoietin prior to dialysis initiation and extracted laboratory data for blood urea nitrogen, serum albumin, creatinine and hemoglobin concentrations.
Zip Code-level Covariates
We included a variable for poverty based on US Census estimates of the percentage of residents living in poverty within the zip code where each patient resided when they initiated maintenance dialysis (<5%, 5–9%, 10–14%, 15–19%, or ≥20% of the population).14 The US Census defines a poverty area as an area where at least 20 percent of residents are poor.15
Treatment of Missing Data
Missing data patterns were examined for all variables. To minimize potential bias caused by excluding patients with missing data we used a multiple imputation procedure with five replications. Imputed values were obtained by sampling with replacement from available data.16
Statistical Analysis
We calculated annual crude rates of death from dialysis initiation, stratified by ethnicity. We analyzed the associations of body size, ethnicity and time to death using proportional hazards (Cox) regression. We incorporated potential explanatory variables in the final adjusted model that were significant at the P<.05 level from bivariate analyses including patient-level sociodemographic factors, comorbities, and laboratory variables described above, as well as proxies for residential poverty. We used scaled Schoenfeld residual plots against time and estimated log (-log [survivor function]) versus time survival curves to assess the proportionality assumption and found no violations. We used the likelihood ratio test to examine for effect modification of the body size-mortality relations by patient ethnicity. To account for potential correlations within zip codes, we obtained robust sandwich estimates for the Cox model using the 5-digit zip code as a cluster variable.17,18 We checked for model fit using Cox-Snell residuals. We considered two-tailed P<.05 as statistically significant and performed all analyses using Stata Statistical Software (Stata MP 11.0, Stata Corp, College Station, TX).
Results
Sociodemographic Characteristics
Overall, 13,007 (61%) White, 7227 (33%) Asian, and 1258 (6%) Pacific Islanders initiated dialysis during the study period. Among self-identified Asians, 1116 (15%) were Chinese or Japanese and 889 (12%) were Filipino; the remaining 5222 Asians did not specify a specific subgroup. Most Pacific Islanders self-identified as Native Hawaiian (40%), Chamorro (30%) or Samoan (16%).
Pacific Islanders were the youngest and Chinese/Japanese were the oldest ethnic group. Pacific Islanders were more likely to be female, have Medicaid and reside in impoverished areas compared with Whites and Asians. The prevalence of major comorbid conditions was highest among Pacific Islanders and lowest among Asians. Ethnic differences in prevalent diabetes were generally larger than differences in prevalent CVD (Table 1).
Table 1.
Baseline characteristics of 21,492 patients initiating dialysis during 1995–2003 in the Western Pacific Renal Network
| Characteristic | Ethnicity
|
||||
|---|---|---|---|---|---|
| White | Asian, unspecified | Chinese or Japanese | Filipino | Pacific Islander | |
| n of participants | 13,007 | 5,222 | 1,116 | 889 | 1,258 |
| Age, mean (SE) | 64.9 (.13) | 62.7 (.22) | 67.5 (.41) | 60.9 (.51) | 56.9 (.38) |
| Female, n (%) | 5,571 (43) | 2,541 (49) | 507 (45) | 424 (48) | 664 (53) |
| Health insurance coverage*, n (%) | |||||
| Employer group | 3,278 (25) | 1,394 (27) | 551 (49) | 370 (42) | 440 (35) |
| Medicare | 4,088 (31) | 1,413 (27) | 388 (35) | 240 (27) | 229 (18) |
| Medicaid | 2,644 (20) | 1,985 (38) | 103 (9) | 194 (22) | 319 (25) |
| Other insurance | 5,697 (44) | 1,365 (26) | 394 (35) | 232 (26) | 362 (29) |
| No insurance | 282 (2) | 245 (5) | 11 (1) | 27 (3) | 64 (5) |
| Comorbid conditions, n (%) | |||||
| Diabetes | 5,395 (41) | 2,463 (47) | 669 (60) | 509 (57) | 891 (71) |
| Cardiovascular disease | 6,370 (49) | 2,125 (41) | 630 (56) | 432 (49) | 642 (51) |
| Charlson index, mean (95%CI) | 3.7 (3.7,3.8) | 3.6 (3.5,3.6) | 4.1 (4.0,4.2) | 3.9 (3.8,4.0) | 4.2 (4.1,4.3) |
| Physical measures, mean (SE) | |||||
| Height, cm | 169.3 (.09) | 161.0 (.13) | 161.5 (.28) | 160.3 (.31) | 165.1 (.28) |
| Weight, kg | 72.2 (.19) | 60.1 (.25) | 62.0 (.51) | 61.1 (.59) | 75.5 (.63) |
| Quetélet’s index (BMI), kg/m2 | 25.2 (.07) | 23.1 (.09) | 23.6 (.17) | 23.6 (.20) | 27.6 (.21) |
| Benn’s index, kg/mρ | 32.7 (.08) | 20.8 (.08) | 20.9 (.15) | 20.7 (.18) | 27.7 (.27) |
| Laboratory measures, mean (SE) | |||||
| Serum albumin, g/dL | 3.3 (.01) | 3.2 (.01) | 3.0 (.02) | 3.0 (.02) | 2.9 (.02) |
| Serum creatinine, mg/dL | 7.0 (.03) | 8.2 (.05) | 9.0 (.11) | 9.5 (.15) | 9.9 (.12) |
| Blood urea nitrogen, mg/dL | 88.0 (.30) | 92.4 (.51) | 105.4 (1.04) | 101.5 (1.20) | 100.7 (1.00) |
| Percentage of residents living in poverty within zip code where patient resides, n (%) | |||||
| <5% | 1,968 (15) | 602 (11) | 96 (9) | 39 (4) | 29 (2) |
| 5–9% | 4,777 (37) | 2,051 (39) | 505 (45) | 345 (39) | 278 (22) |
| 10–14% | 2,765 (21) | 1,106 (21) | 216 (19) | 216 (24) | 157 (13) |
| 15–19% | 1,423 (11) | 491 (9) | 258 (23) | 104 (12) | 155 (12) |
| ≥20% | 2,074 (16) | 972 (19) | 41 (4) | 185 (21) | 639 (51) |
Due to multiple sources, health insurance coverage may exceed 100%.
Ethnic Differences in Nutritional Parameters and Body Size
Substantial ethnic differences were observed in nutritional parameters and body size. Pacific Islanders had the highest serum creatinine and the lowest serum albumin concentrations. In contrast, Whites had the lowest serum creatinine and blood urea nitrogen concentrations and the highest concentrations of serum albumin. In general, Asians had laboratory values that were intermediate between those Pacific Islanders and Whites with the exception of high blood urea nitrogen levels observed in persons of Chinese/Japanese descent (Table 1).
Among both men and women, Pacific Islanders were the heaviest, Whites were the tallest, and Asians were the shortest and lightest ethnic group. Mean BMI was highest among Pacific Islanders, intermediate among Whites and lowest among Asians. Asians had the highest fraction of patients who were classified as having normal (18.5–24.9 kg/m2) body mass. Over one-third of Pacific Islanders and one-fifth of Whites qualified as obese using conventional WHO criteria compared with 11 percent of Asians. The exponent ρ of Benn’s index that extinguished the correlation with height differed widely by ethnicity. Among men, values of exponent ρ were 1.48, 2.23, 2.39, 2.21 and 1.62 for Whites, Asians (unspecified), Chinese/Japanese, Filipinos and Pacific Islanders, respectively. Corresponding values among women were 1.53, 2.20, 2.08, 2.38 and 2.46, respectively.
Mortality
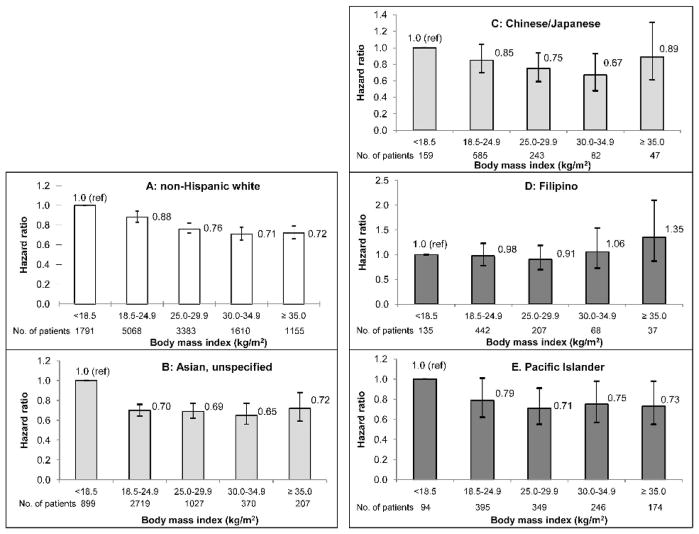
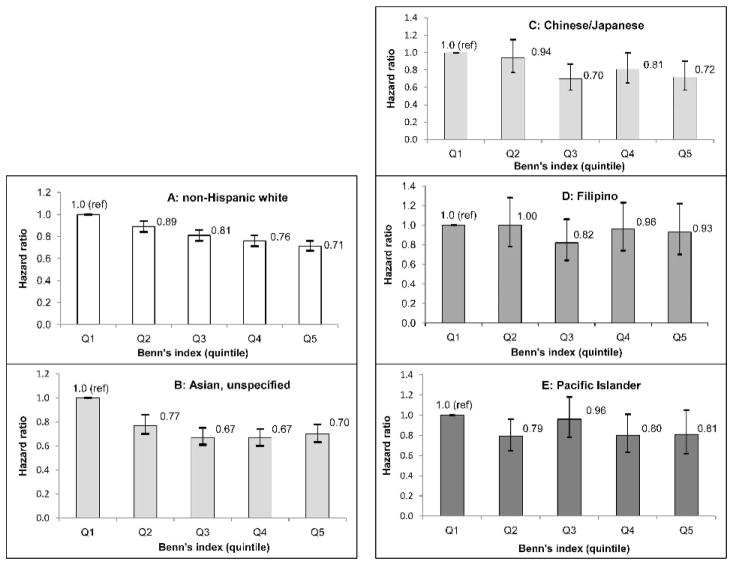
Overall, 16,644 deaths occurred during the study period. Annual mortality rates were highest among Whites (29.6%), intermediate among Pacific Islanders (18.8%) and lowest among Asians (17.3%). Most ethnic groups showed lower dialysis mortality with larger body size. Filipinos were the exception and did not experience any survival benefit with larger body size. The relation between body size and mortality remained consistent in analyses that adjusted for patient-level socio-demographic and clinical factors, area-based estimates of socioeconomic status and geographic clustering (Figures 1a–e and 2a–e).
Fig. 1.
Figs 1a–1e. Adjusted mortality risk for different ethnic groups according to body mass index
Data bars represent 95% confidence intervals.
Fig. 2.
Figs 2a–2e. Adjusted mortality risk for different ethnic groups according to Benn’s index
Other factors associated with higher mortality included older age, male sex, lower concentrations of hemoglobin, serum albumin and serum creatinine, higher concentrations of blood urea nitrogen, more extensive comorbidity, and residence in the two most impoverished categories (P<.001 for all except moderate [15–19%] poverty, P=.010).
Companion analyses in which Quetélet’s and Benn’s index were treated as continuous variables showed generally lower mortality with larger body size. The quadratic term had a positive coefficient suggesting a curvilinear U-or reverse J-shaped relation between body size and mortality. Among Filipinos, we saw nominally higher mortality with higher Quetélet’s index. However, we found no evidence of effect modification of the body size-mortality relations by ethnicity (P=.65 and P=.14 for the likelihood ratio test of models with and without the interaction terms of BMI- and Benn’s index-ethnicity, respectively).
Discussion
We observed substantial ethnic differences in body size but relatively similar patterns of associated survival in a large cohort of Asian, Pacific Islander and White patients initiating maintenance dialysis in California, Hawaii and the US Pacific Islands. In general, dialysis patients of all ethnic groups demonstrated better survival with larger body size irrespective of how body size was estimated. Filipinos were the exception and did not experience lower mortality with larger body size. These observations were independent of differences in socioeconomic status, clinical and laboratory measures and geographic clustering. These results highlight a need for more in-depth investigations on the mechanism(s) linking body size with survival and ultimately, guidance for patients with ESRD from diverse populations regarding body composition and weight management.
Despite considerable growth of Asian and Pacific Islander populations in the United States, our understanding of the influence of body size on ESRD outcomes in these dissimilar ethnic groups remains limited. Wong et al observed a U-shaped association between BMI and mortality among 4471 Asian Americans on dialysis during the 1990s.10 Unlike the current study, Wong et al described the relations of body size and mortality among jointly categorized Asians and Pacific Islanders, controlled for relatively few confounders (age, sex and diabetes) and were limited to short-term follow up for death (8 to 31 months). Johansen et al reported that Asian dialysis patients did not enjoy a survival advantage at higher body mass but were likewise limited in characterizing the relations of body size and mortality in Pacific Islanders or in Asian subgroups.3 In comparison, our study had access to disaggregated, self-reported ethnicity data and long-term follow up for death enabling examination of mortality risk across body size categories and within ethnic subgroups. We also included estimates of socioeconomic status and accounted for geographic clustering, factors increasingly recognized as important determinants of mortality, morbidity, dietary intake and body composition in diverse communities.19,20 In contrast to the aforementioned studies, our results suggest that most Asians and Pacific Islanders on dialysis experience better survival with larger body size, findings consistent with those previously described in Whites, Blacks and Hispanics.1–4
The absence of survival benefit with increasing body size among Filipinos may reflect disproportionately larger stores of visceral fat predisposing members of this ethnic group to diabetes and CVD, even without correspondingly larger overall body mass.21,22 Prior US-based studies in non-ESRD populations have shown high rates of diabetes and CVD risk factors among some Asian subgroups at normal body weights.23,24 Likewise, the findings of increased visceral adiposity, diabetes and CVD in the presence of normal or slightly elevated body mass among Japanese and Filipinos without ESRD suggest that ethnic differences in body composition and the distribution of body fat might also account for these observations.25,26 These differences further highlight the limitations of extrapolating body size cut-points derived from non-ESRD populations to diverse groups on dialysis.
Our study also underscores the phenotypic heterogeneity of Asians and Pacific Islanders on dialysis. Asian men and women were on average 15 kilograms lighter and 5 centimeters shorter than their Pacific Islander counterparts. Despite their smaller body size, Asians experienced slightly better overall survival on dialysis than Pacific Islanders. While genetic factors may have played a role in these findings, ethnic differences in modifiable factors including diet, exercise, smoking and access to higher quality medical care might have contributed as well.27,28 Contrary to our original hypothesis, we found relatively similar relations between body size and mortality irrespective of how we estimated adiposity. The protective effect of larger body size could result from the presence of energy reserves that protect patients from the consequences of malnutrition induced by uremia.3
Limitations
Our study’s strengths included analysis of a large, diverse cohort of ESRD patients with comprehensive, long-term follow up for death and inclusion of comparative data for Asians and Pacific Islanders – phenotypically diverse groups that are rarely disaggregated in US-based studies on kidney disease. Our study also had several limitations. First, our results are potentially limited by residual confounding from under-ascertainment of comorbid conditions such as CVD, based on the Medical Evidence form.29 Given the magnitude of the differences in mortality risk across body size categories and the consistency of results across ethnic groups, it seems unlikely that our results were due to residual confounding alone. Second, although we observed similar body size-mortality relations using two different estimates of adiposity based on height and weight, we were limited in examining other measures of body composition such as visceral adiposity, phase angle, or lean body mass, as these data were not available.30 Third, although we found no evidence of effect modification by ethnicity, it remains possible that dialysis patients from some ethnic groups experience higher, rather than lower mortality with increased adiposity. Fourth, selection bias might partly account for the body size-mortality relations observed in our study because larger body size may contribute to better survival during earlier stages of chronic kidney disease. Fifth, while Network 17 included over one-third of Asians and Pacific Islanders who initiated dialysis in the United States during the study period, our results may not be completely generalizable to Asians and Pacific Islanders residing in other locales. Finally, since these data examine only baseline body size, no conclusions or clinical recommendations should be reached regarding any potential harm or benefit of prescribed weight loss or gain. It is possible that with updated information on body weight, we could better estimate the effects of adiposity and wasting in this population.
Conclusions
Our findings support the need for additional studies to examine the impact of body size and body composition on ESRD outcomes in diverse communities. In particular, our results highlight the heterogeneity of body size among Asians and Pacific Islanders and underscore current challenges in counseling patients on maintaining optimal body weight in ESRD. Use of disaggregated ethnicity data may lead to more specific ethnicity- or community-based interventions to improve dietary, exercise and weight management for these diverse populations on dialysis.
Acknowledgments
Dr. Hall received support from K23 DK 087900 and the Norman S. Coplon Extramural Grant Program of Satellite Healthcare. Dr. Chertow received support from N01 DK 012450, U01 DK 066481 and K24 085446.
Footnotes
Author Contributions
Design concept of study: Hall, Chertow
Acquisition of data: Hall, Xu, Chertow
Data analysis and interpretation: Hall, Xu, Chertow
Manuscript draft: Hall, Xu, Chertow
Statistical expertise: Hall, Xu, Chertow
Acquisition of funding: Hall, Chertow
Administrative: Hall, Chertow
Supervision: Hall, Chertow
References
- 1.Port FK, Ashby VB, Dhingra RK, Roys EC, Wolfe RA. Dialysis dose and body mass index are strongly associated with survival in hemodialysis patients. J Am Soc Nephrol. 2002;13(4):1061–1066. doi: 10.1681/ASN.V1341061. [DOI] [PubMed] [Google Scholar]
- 2.Leavey SF, Strawderman RL, Jones CA, Port FK, Held PJ. Simple nutritional indicators as independent predictors of mortality in hemodialysis patients. Am J Kidney Dis. 1998;31(6):997–1006. doi: 10.1053/ajkd.1998.v31.pm9631845. [DOI] [PubMed] [Google Scholar]
- 3.Johansen KL, Young B, Kaysen GA, Chertow GM. Association of body size with outcomes among patients beginning dialysis. Am J Clin Nutr. 2004;80(2):324–332. doi: 10.1093/ajcn/80.2.324. [DOI] [PubMed] [Google Scholar]
- 4.Kopple JD, Zhu X, Lew NL, Lowrie EG. Body weight-for-height relationships predict mortality in maintenance hemodialysis patients. Kidney Int. 1999;56(3):1136–1148. doi: 10.1046/j.1523-1755.1999.00615.x. [DOI] [PubMed] [Google Scholar]
- 5.Beddhu S, Pappas LM, Ramkumar N, Samore M. Effects of body size and body composition on survival in hemodialysis patients. J Am Soc Nephrol. 2003 Sep;14(9):2366–2372. doi: 10.1097/01.asn.0000083905.72794.e6. [DOI] [PubMed] [Google Scholar]
- 6.Johansen KL, Kaysen GA, Young BS, Hung AM, da Silva M, Chertow GM. Longitudinal study of nutritional status, body composition, and physical function in hemodialysis patients. Am J Clin Nutr. 2003;77(4):842–846. doi: 10.1093/ajcn/77.4.842. [DOI] [PubMed] [Google Scholar]
- 7.Johansen KL, Kutner NG, Young B, Chertow GM. Association of body size with health status in patients beginning dialysis. Am J Clin Nutr. 2006;83(3):543–549. doi: 10.1093/ajcn.83.3.543. [DOI] [PubMed] [Google Scholar]
- 8.Benn RT. Some mathematical properties of weight-for-height indices used as measures of adiposity. Br J Prev Soc Med. 1971;25(1):42–50. doi: 10.1136/jech.25.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee J, Kolonel LN, Hinds MW. Relative merits of the weight-corrected-for-height indices. Am J Clin Nutr. 1981;34(11):2521–2529. doi: 10.1093/ajcn/34.11.2521. [DOI] [PubMed] [Google Scholar]
- 10.Wong JS, Port FK, Hulbert-Shearon TE, et al. Survival advantage in Asian American end-stage renal disease patients. Kidney Int. 1999;55(6):2515–2523. doi: 10.1046/j.1523-1755.1999.00464.x. [DOI] [PubMed] [Google Scholar]
- 11.Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363 (9403):157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 12.Hall YN, Sugihara JG, Go AS, Chertow GM. Differential mortality and transplantation rates among Asians and Pacific Islanders with ESRD. J Am Soc Nephrol. 2005;16(12):3711–3720. doi: 10.1681/ASN.2005060580. [DOI] [PubMed] [Google Scholar]
- 13.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 14.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82(5):703–710. doi: 10.2105/ajph.82.5.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.US Bureau of the Census. [Last accessed on 27 February 2010];Poverty Areas. Available at: http://www.census.gov/population/socdemo/statbriefs/povarea.html.
- 16.Little RJA, Rubin DB. Statistical Analysis with Missing Data. New York: J. Wiley & Sons; 1987. [Google Scholar]
- 17.Lin DY, Wei LJ. The robust inference for the Cox proportional hazards model. J Am Statist Assoc. 1989;84:1074–1079. [Google Scholar]
- 18.Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56(2):645–646. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- 19.Diez Roux AV, Detrano R, Jackson S, et al. Acculturation and socioeconomic position as predictors of coronary calcification in a multiethnic sample. Circulation. 2005;112(11):1557–1565. doi: 10.1161/CIRCULATIONAHA.104.530147. [DOI] [PubMed] [Google Scholar]
- 20.Komatsu F, Kagawa Y, Kawabata T, Kaneko Y, Ishiguro K. Relationship of dietary habits and obesity to oxidative stress in Palauan people: compared with Japanese and Mongolian people. Curr Aging Sci. 2009;2(3):214–222. doi: 10.2174/1874609810902030214. [DOI] [PubMed] [Google Scholar]
- 21.Maskarinec G, Grandinetti A, Matsuura G, et al. Diabetes prevalence and body mass index differ by ethnicity: the Multiethnic Cohort. Ethn Dis. 2009;19(1):49–55. [PMC free article] [PubMed] [Google Scholar]
- 22.Narayan KM, Aviles-Santa L, Oza-Frank R, et al. Report of a National Heart, Lung, And Blood Institute Workshop: heterogeneity in cardiometabolic risk in Asian Americans In the U.S. Opportunities for research. J Am Coll Cardiol. 2010;55(10):966–973. doi: 10.1016/j.jacc.2009.07.075. [DOI] [PubMed] [Google Scholar]
- 23.Araneta MR, Barrett-Connor E. Subclinical coronary atherosclerosis in asymptomatic Filipino and white women. Circulation. 2004;110(18):2817–2823. doi: 10.1161/01.CIR.0000146377.15057.CC. [DOI] [PubMed] [Google Scholar]
- 24.Oza-Frank R, Ali MK, Vaccarino V, Narayan KM. Asian Americans: diabetes prevalence across U.S. and World Health Organization weight classifications. Diabetes Care. 2009;32(9):1644–1646. doi: 10.2337/dc09-0573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Araneta MR, Barrett-Connor E. Ethnic differences in visceral adipose tissue and type 2 diabetes: Filipino, African-American, and white women. Obes Res. 2005;13(8):1458–1465. doi: 10.1038/oby.2005.176. [DOI] [PubMed] [Google Scholar]
- 26.Hayashi T, Boyko EJ, Leonetti DL, et al. Visceral adiposity is an independent predictor of incident hypertension in Japanese Americans. Ann Intern Med. 2004;140(12):992–1000. doi: 10.7326/0003-4819-140-12-200406150-00008. [DOI] [PubMed] [Google Scholar]
- 27.Moy KL, Sallis JF, David KJ. Health indicators of Native Hawaiian and Pacific Islanders in the United States. J Community Health. 2010;35(1):81–92. doi: 10.1007/s10900-009-9194-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mishra SI, Osann K, Luce PH. Prevalence and predictors of smoking behavior among Samoans in three geographical regions. Ethn Dis. 2005;15(2):305–315. [PubMed] [Google Scholar]
- 29.Longenecker JC, Coresh J, Klag MJ, et al. Validation of comorbid conditions on the end-stage renal disease medical evidence report: the CHOICE study. Choices for Healthy Outcomes in Caring for ESRD. J Am Soc Nephrol. 2000;11(3):520–529. doi: 10.1681/ASN.V113520. [DOI] [PubMed] [Google Scholar]
- 30.Chertow GM, Jacobs DO, Lazarus JM, Lew NL, Lowrie EG. Phase Angle Predicts Survival in Hemodialysis Patients. J Renal Nutrition. 1997;7(4):204–207. [Google Scholar]