Abstract
Low-income youth are at increased risk for excess weight gain. Although evidence-based prevention programs exist, successful adaptation to provide wide dissemination presents a challenge. Hip-Hop to Health (HH) is a school-based obesity prevention intervention that targets primarily preschool children of low-income families. In a large randomized controlled trial, HH was found to be efficacious for prevention of excessive weight gain. The Expanded Food and Nutrition Education Program (EFNEP) and the Supplemental Nutrition Assistance Program--Education (SNAP-Ed) are USDA-funded nutrition education programs offered to low-income families, and may provide an ideal platform for the wide dissemination of evidence-based obesity prevention programs. A research-practice partnership was established in order to conduct formative research to guide the adaptation and implementation of HH through EFNEP and SNAP-Ed. We present the design and method of a comparative effectiveness trial that will determine the efficacy of HH when delivered by peer educators through these programs compared to the standard EFNEP and SNAP-Ed nutrition education (NE) curriculum. Results from this trial will inform larger scale dissemination. The dissemination of HH through government programs has the potential to increase the reach of efficacious obesity prevention programs that target low-income children and families.
Keywords: Obesity prevention, preschool children, USDA, dissemination, EFNEP, SNAP-Ed
1. Introduction
Obesity is an epidemic in the U.S.[1], with important implications for obesity-associated comorbid conditions.[2] Notably, the prevalence of obesity (defined as body mass index (BMI) at or above the 95th percentile for a given age) has tripled among young children since 1980. [3, 4] Although the rates of obesity among preschool children decreased from 2002-2012 (13.9% to 8.4%), they are still alarmingly high overall.[5] Without intervention, obese children are more likely to remain obese into adulthood, increasing the risk of poor health outcomes.[6-8]
Socioeconomic status (SES) and race/ethnicity are associated with disparities in many health behaviors and health outcomes, [9] and these associations are evident with obesity and related conditions in children and adults from low-income populations and some racial/ethnic minority groups. Results from the 2011-2012 National Health and Nutrition Examination Survey (NHANES) show that among 2- to 5-year olds, 3.5% of Non-Hispanic Whites, 11.3% of Non-Hispanic Blacks, and 16.7% of Hispanics are obese, and the prevalence of obesity is even higher among 6-11 years olds (13.1% of Non-Hispanic Whites, 23.8% of Non-Hispanic Blacks, and 26.1% of Hispanics).[5] As compared to the results from 2007-2008, the rates of obesity among Non-Hispanic Whites have decreased, while rates among Hispanic and African American children have either increased or remained constant.[4] Thus, the preschool years represent a critical period for addressing weight- related health behaviors and excessive weight gain trajectories among at-risk children. [10-12]
Although a limited number of nutrition and physical activity interventions have been found to be efficacious in changing behaviors associated with weight gain among low-income populations, few have been broadly disseminated. [13-15] The National Institutes of Health (NIH) and other agencies emphasize the need for the widespread implementation and dissemination of evidence-based interventions to bridge the gap between research and practice.[15] The focus of this study was to assess the potential of adapting and disseminating “Hip Hop to Health” (HH), a NIH-funded school-based nutrition and physical activity obesity prevention program for low-income preschool children, through federally-funded community based nutrition education programs that target low-income families.
The HH program includes nutrition and physical activity programming, directed to both children and parents. The child component includes a 20 minute, 3 times weekly intervention for 14 weeks. The parent component includes weekly newsletters that complemented topics delivered during the child sessions. Parents are asked to assist their child in completing a weekly homework assignment related to healthy eating and activity. We evaluated the intervention by comparing changes in body mass index (BMI [kg/m2]) in 3-5 year old predominantly African American and Latino children randomized to either HH or a general health intervention (GH). Results at the 1 and 2 year follow-ups showed that children in HH had significantly smaller increases in BMI compared to children in the GH control group. HH was the first intervention to exhibit positive effects on BMI in low-income, preschool children. [11]
Delivered through the USDA-National Institute of Food and Agriculture cooperative extension system, the Expanded Food and Nutrition Education Program (EFNEP) teaches nutrition, food safety and food resource management and is designed to improve diet and overall nutritional well being among low-income families. Currently operating in all 50 states and the United States Territories, the program provided education to approximately 130,000 adults and 479,000 youth in 2012. Similarly, the goal of the Supplemental Nutrition Assistance Program Education (SNAP-Ed) is to improve the likelihood that Supplemental Nutrition Assistance Program (SNAP) recipients will make healthier food choices consistent with the current Dietary Guidelines for Americans and MyPlate, even on a limited budget. Although SNAP-Ed is offered to all segments of the population, a primary focus is on women and children, who make up the majority of SNAP recipients. In 2011, 19 % of SNAP participants, or almost 8 million, were women living in households with children, and an additional 45% of recipients were children.
Evaluations of these programs show that they positively affect meal planning, comparison shopping, and diet, [16, 17] suggesting that they may provide attractive settings for obesity prevention interventions. [18] However, traditionally these programs have not focused specifically on obesity prevention. Given the established efficacy of HH and the broad reach of EFNEP and SNAP-Ed, we partnered with the University of Illinois Extension Expanded Food and Nutrition Education Program (EFNEP) and the Chicago Partnership for Heath Promotion Supplemental Nutrition Assistance Program Education Program (SNAP-Ed) to determine whether HH could be adapted, implemented, and disseminated within these established programs.
This paper describes the rationale and design of this comparative effectiveness trial that will adapt, implement, and test whether the adapted HH intervention is more effective than the nutrition education (NE) routinely provided by these programs in changing diet, physical activity, and screen time among both parents and children. As an exploratory aim, we will also analyze group differences in body mass index trajectories.
2. Material and methods
2.1 Hypotheses
It is hypothesized that delivering HH through EFNEP and SNAP-Ed will be feasible and acceptable to study participants. We also hypothesize that participants in HH will exhibit more positive outcomes relative to participants in Nutrition Education (NE). Specifically, we hypothesize that post-intervention, participants in HH will have 1) higher levels of fruit and vegetable consumption; 2) lower levels of fat consumption; 3) higher levels of physical activity; and 4) lower levels of screen time.
2.2 Study Design
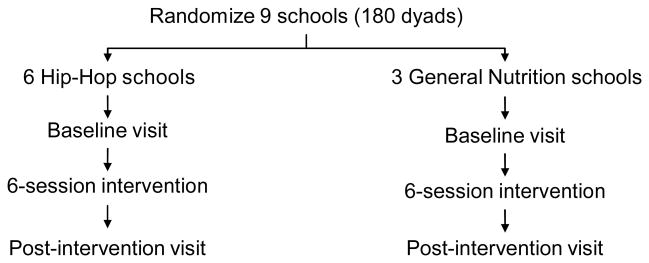
This study is a randomized comparative effectiveness trial comparing Hip-Hop to Health (HH) to the usual EFNEP and SNAP-Ed nutrition education (NE) curriculum for low-income parents and children. The study will be conducted in 3 successive cohorts of 3 schools each, with 2 HH and 1 NE school in each cohort and 1 participating classroom per school. Therefore, 9 schools from EFNEP or SNAP-Ed programs will be randomized to either HH or NE. EFNEP and SNAP-Ed paraprofessionals who are taught the HH curriculum will work in different sites than paraprofessionals who teach the standard EFNEP and SNAP-Ed curricula. Parent-child dyads in HH will receive a six-session obesity prevention intervention that is delivered over 6 weeks. NE parent-child dyads will receive the standard curriculum, also delivered in six sessions over 6 weeks. We will collect data on weight, height, dietary intake, physical activity, and screen time post-intervention to assess the effects of the intervention at each time point. We will also collect information on potential mediators of diet and physical activity behavior change: parental support and role modeling and parental feeding style.
2.3 Participants
Participants will be 3- to 5- year old preschool children who attend EFNEP or SNAP-Ed programs and their parent(s) or caregiver(s). The overall enrollment is predicted to be 180 parent-child dyads (Figure 1). Paraprofessional staff of EFNEP and SNAP-Ed will also be observed to assess fidelity of intervention delivery and satisfaction with the curriculum.
Figure 1. Study Design: Recruitment.
2.3.1 Eligibility
All children and parents who are recipients of EFNEP and SNAP-Ed services at the participating sites are eligible to participate. Although EFNEP and SNAP-Ed provide services in a variety of settings, we have chosen to recruit primarily from preschools. Parents will sign an informed consent for themselves and their children.
2.4 Intervention and Staff Training
2.4.1 Interventions
2.4.1.1 Hip-Hop Intervention (HH)
We adapted HH from our previously tested curriculum in close consultation with our community partners and other stakeholders. Key informant interviews were conducted with USDA staff, investigators who had extensive experience both working and conducting research with EFNEP and SNAP-Ed participants and personnel, and local and regional EFNEP and SNAP-Ed staff. These interviews provided information that aided in the adaptation. For example, we decreased the number of sessions from 3 times per week for 14 weeks to 1 time per week for 6-8 weeks to be consistent with the format of EFNEP and SNAP-Ed and also to promote intervention adherence. We also made accommodations for the change in intervention delivery. Our original HH intervention was led by trained early-childhood educators, whereas the adapted version will be led by peer educators, who are paraprofessional staff hired from the community where they work and are trained to specifically deliver the desired intervention
HH focuses on healthy eating and exercise for preschoolers and their families. The lessons for preschoolers include developmentally-appropriate activities that reinforce important concepts related to choosing foods and activities that are “go and grow” (i.e., fruits and vegetables, low-fat milk, whole grains, running, dancing, playing sports) as opposed to choosing those that can make you slow if you choose them too often (i.e., fried foods, chips, cookies, watching television, playing video games). Specific topics covered include “slow foods” versus “go and grow foods”, fruits, vegetables, grains, protein, milk, drinking water, and healthy snacking. The majority of the lessons incorporate colorful puppets representing major food groups (Miss Grain, Miss Fruit, Mr. Vegetable, Mr. Protein, Miss Dairy, Mr. Fat, and Miss Sugar). Following each lesson, the instructor leads a 20-minute exercise routine that includes warm-up, aerobic activities, and cool-down. The curriculum is manualized and is available in both English and Spanish. The curriculum also includes a CD (available in both English and Spanish) with curriculum songs and raps, as well two fully-scripted 20-minute exercise routines that use lively and engaging songs.
Instructors each receive the curriculum manual, the CD, and a toolbox containing the supplies needed for each lesson. The curriculum manual presents the program in structured, easy-to-follow lesson plans that address a variety of health and nutrition topics (e.g., portion size, grains, vegetables, fruit, healthy snacks, exercise). Each lesson plan includes the following information:
Preparation – steps to complete prior to beginning an activity
Description of daily activity - bullet points for ease of implementation
List of supplies needed
Objectives for each lesson
While the child program is designed to be developmentally appropriate for preschool children, the parent component is designed to engage parents in their child's learning and promote increased interaction between parent and child around making healthy choices related to eating and exercise patterns. The sessions were created based on the principles of adult learning, respecting the autonomy of adults to engage in self-directed and goal-oriented learning based on their current knowledge and life experience.[19] The parent component includes 6-8 sessions that complement what the children are learning by including newsletters, interactive take home activities, and cooking and physical activity demonstrations. Themes for the newsletters parallel those for the children, but also include important information related to healthy lifestyle parenting tips, problem solving around barriers to making healthy eating and activity choices, budget conscious shopping, and community resources.
2.4.1.2 Nutrition Education Curriculum (NE)
The standard NE curriculum delivered through the local EFNEP and SNAP-Ed programs provides separate programming for parents and children. EFNEP and SNAP-Ed provide lessons for preschool children that are consistent with the Dietary Guidelines for Americans 2010, but they do not have a standard preschool curriculum. The parent curriculum is a six-session program based on “Eating Smart, Being Active,” which was developed by Colorado State University. The curriculum utilizes a combination of dialogue and “hands-on” activities to encourage behavior change related to making healthy food choices, food safety, food budgeting, and physical activity. NE participants will receive the same number of classes as HH participants (one session per week for 6-8 weeks). However, the NE program was developed for older children (5 years and older), does not have a complementary parent and child curriculum, and does not have an explicit focus on weight gain prevention.
2.4.2 Staff Training
EFNEP and SNAP-Ed peer educators are critical in the delivery of the HH curriculum due to their ability to establish enhanced rapport with the low-income participants. [20] The peer educators participating in this study have experience delivering nutrition education interventions. Therefore, they have a background in basic nutrition and only need additional training on the new intervention for this study. The training includes an initial 4-hour group training session that provides an introduction to current information on childhood obesity, an overview of the curriculum, a curriculum demonstration, and a fitness session led by a certified fitness instructor. Staff receives 1) complete manuals with specific instructions on planning each curriculum session and 2) a toolkit that includes all materials needed for delivery of the curriculum. This session for HH staff includes a review of specific content for each of the six sessions, with emphasis on the different developmental needs of adults and children in making dietary and activity choices.
2.5 Data Collection and outcomes
2.5.1 Data Collection
Data will be collected before the intervention begins and immediately post-intervention. Except where otherwise noted, all measures will be administered at both visits.
2.5.2 Measures
Since sustainability and ease of dissemination are important goals of the study, we chose brief, relatively simple measures that could be used by SNAP-Ed and EFNEP for evaluation purposes in the future. This excludes the use of objective measures of physical activity, such as accelerometers or direct observation, as well as the use of 24-hour recalls to measure dietary intake. Parents completed all measures for the child.
Demographics
At baseline, parents will report date of birth (parent and child), gender (parent and child), race/ethnicity (parent and child), relationship to the child, education, employment, marital status, country of birth, public assistance in the last 6 months (WIC, SNAP, cash assistance), and whether they own a car or have regular access to one.
Acculturation
At baseline, parents who identified as Hispanic/Latino will complete the four-item Short Acculturation Scale, a four-item questionnaire that measures acculturation as a preference for English or Spanish in spoken language, written material, and social networks.
Anthropometrics
Children's height and weight and parents' weight will be measured at baseline and post-intervention. Parents' height will be measured at baseline only. Height will be measured by trained research assistants using a portable stadiometer. Weight will be measured using a Tanita BWB-800 digital scale (Tanita Corporation of America, Inc., Arlington Heights, IL). Shoes and any heavy outer clothing will be removed for the anthropometric measurements. Both height and weight will be measured twice, to the nearest 0.1 cm and 0.1 kg respectively. If the two height measurements are >0.5 cm apart or if the two weight measurements are >0.2 kg apart, a third measurement will be taken. The mean of the two closest measurements will be used for analysis. BMI will be computed from height and weight. BMI Z scores and BMI percentiles for age and sex will be calculated for each child based on the 2000 Centers for Disease Control and Prevention Growth Charts, using a SAS program provided by the Centers for Disease Control and Prevention.
Dietary Intake
Starting the Conversation (STC) is an 8-item dietary assessment instrument that was designed for use by non-dietitians in primary care and health-promotion settings. Parents will report their own and their child's consumption of fast food, fruit, vegetables, soda or sweet tea, chips or crackers, desserts or sweets, butter or other added fats, and beans, chicken or fish in the past week. A summary score will be calculated from the 8 responses.[21]
Physical Activity
The Godin Leisure-Time Exercise Questionnaire asks parents to report how many times they or their child engage in strenuous exercise, moderate exercise, or mild exercise during their free time for more than 15 minutes at a time during a typical 7-day period. For children, we modified the instructions slightly to specify that free time does not include time in school. We also revised the examples of activity types to make them more appropriate for children (e.g., strenuous: running, playing tag, basketball, roller skating, soccer, vigorous swimming, jumping rope, trampoline; moderate: bicycling, gymnastics, dancing, playing actively on the playground/house/yard; mild: hop-scotch, easy walking, swinging). A weekly leisure activity score will be calculated from the responses: 9*Strenuous + 5*Moderate + 3*Light.[22]
Screen Time
Parents will be asked to estimate the number of hours their child spends on a typical school day (or a typical weekday if the child is not in school) and on a typical weekend day; 1) watching television (broadcast, cable, or satellite); 2) watching DVDs or video; 3) playing video games while sitting down (not including active video games); or 4) using a computer. Parents will also report their own screen time on a typical weekday and weekend day. Screen time (hours/day) is calculated as a weighted average: [5*(all screen time on an average weekday) + 2*(all screen time on an average weekend day)]/7.[23]
Parental Support and Role Modeling
The Parental Support and Role Modeling measure is a self-report measure that consists of 10 questions on the frequency of supportive and/or modeling behaviors. Participants answer questions such as “How often do you check food labels?”[24]
Feeding styles
The Caregiver's Feeding Styles Questionnaire is a 19-item questionnaire that asks the parent to report how often they interact with their child in various ways during the dinner meal (e.g., “Tell the child to eat at least a little bit of food on his or her plate”). A scoring algorithm is used to categorize parental feeding style as authoritative, authoritarian, indulgent, or uninvolved.[25]
2.6 Sample Size and Randomization
This study will be conducted in three cohorts, with 3 schools in each cohort (9 schools total). Within each cohort, schools will be randomized using a “coin” with prob(Heads) = .67, so that 2 will be randomized to receive the HH intervention and 1 will receive the NE. Approximately 20 parent-child dyads per school are expected to participate, so at baseline there will be 9 X 20 = 180 dyads (120 in HH and 60 in NE). This cluster randomization reduces the effective sample size due to the design effect, which will be 1.57 assuming an intraclass correlation of 0.03. Assuming 90% retention at follow up and correcting for the design effect, the effective sample size is 102 (68 HH and 34 NE). The power available to detect a “smallish” effect size of 0.35 [26]with two-sided alpha = 0.05 and cross-time correlation of 0.30 is 0.54. [27] To achieve power = .80 under these conditions would require a baseline sample size of about 330 dyads from at least 17 schools.
2.7 Data Management and Analytic Plan
All interview data will be collected on scannable paper forms and processed using the TeleForm program. After processing, TeleForm will export the data to a database for storage. The data will be imported into SAS for data cleaning and data analysis.
The study is a two-group (HH, NE) X 2 Times (Baseline, End of Program) repeated measures design with subject and school clustering. PROC MIXED will be employed in SAS version 9.4 or later to conduct the analysis within the linear mixed models framework [28] with random effects to represent within-subjects and within-schools similarity. Outliers will be transformed as warranted. Discrete outcomes will be analyzed using the companion PROC GLIMMIX for generalized linear mixed models. [29] Mixed models accommodate both time-invariant and time-varying covariates and make best use of incomplete data under plausible missing at random missing data assumptions.[30]
Discussion
The purpose of the current study is to adapt and disseminate an evidence-based obesity prevention program targeting low-income children and families through established government-sponsored nutrition education programs (EFNEP: http://www.csrees.usda.gov/nea/food/efnep/efnep.html and SNAP-Ed: http://www.nifa.usda.gov/nea/food/fsne/fsne.html). The study also seeks to provide complementary and developmentally-appropriate parent and child versions of our HH curriculum with the inclusion of specific weight gain prevention strategies.
In crafting the adapted curriculum for dissemination, we recognize the substantial barriers that need to be addressed if we are to be successful in both reaching and potentially influencing behavior change in both parents and their children.[31-33] Glasgow & Emmons [34]identified a number of barriers to effective dissemination, including certain characteristics of the interventions (e.g., high cost, intensive time demands, lack of manualization of the intervention, lack of sustainability), characteristics of intended target settings (e.g., competing demands on time and resources, failure to obtain provider buy-in, resource and time limitations), and poor research design (e.g., non-representative sample, failure to evaluate cost, failure to assess implementation). We worked with EFNEP and SNAP-Ed stakeholders to examine potential barriers to dissemination of HH. Table 1 outlines our responses to these barriers. The HH intervention is flexible, manualized, tailored, and can be delivered by paraprofessionals. This makes already existing government programs funded to improve nutrition an ideal venue for dissemination. The proposed intervention is a complement to the teaching methods and materials delivered through the EFNEP and SNAP-Ed programs, and we anticipate that a successful demonstration of the intervention in this setting will prompt widespread adoption of the intervention throughout the EFNEP and SNAP-Ed programs nationally.
Table 1. Responses to Potential Barriers to Dissemination.
| Potential Barrier* | Response |
|---|---|
| Lack of a manualized curriculum targeting obesity prevention in preschool age children | Hip-Hop is manualized and packaged with l an accompanying tool box |
| Delivery staff may have other competing responsibilities | Delivery of diet-related curriculum is the primary responsibility of EFNEP and SNAP-Ed staff |
| High level of staff expertise often required | Hip-Hop curriculum has been taught to and implemented by other paraprofessional staff who did not have particular expertise related to the intervention |
| Interventions are often not flexible | Hip-Hop can be adapted for delivery in a variety of settings and formats |
| Intervention may not be appropriate for the target population | Hip-Hop was developed specifically for use with the target population (i.e., low-income preschool children and their parents) |
| Organization and intervention philosophies are often not aligned | The philosophies of the investigative team and the EFNEP and SNAP-Ed programs are aligned, and leadership and staff of the organizations have been involved in the development of the proposed approach |
| Organizations often cannot implement the intervention adequately | The EFNEP and SNAP-Ed delivery staff have significant experience in receiving training for and delivering similar interventions to low-income families |
Adapted with permission from Glasgow & Emmons (2006) Annual Review of Public Health 38, 413-433.
If results from our comparative effectiveness trial are positive, the HH intervention will be disseminated on a larger scale. The adapted, manualized HH curriculum and study findings will be disseminated to the target audience, namely local, state, and national EFNEP coordinators and SNAP-Ed administrators, educators, and program delivery staff. This approach will be facilitated by the involvement of EFNEP and SNAP-Ed administrators throughout the proposed project. Importantly, as part of dissemination efforts, all staff at the EFNEP Cook County sites will be trained at the end of the intervention. Training sessions will also be conducted as part of the joint regional training session held for EFENP and SNAP-Ed staff. To facilitate dissemination and implementation locally and more broadly, we will make our findings and all measurement tools and material (including CD's and the manualized curriculum) available on the University of Illinois Extension website, the National EFNEP website, and the SNAP-Ed Connection Resource Library website. We will conduct 2-3 day Hip-Hop Institutes for extension educators and other nutrition educators at the university as well as mini-training at national meetings. We will also deliver presentations at conferences attended by EFNEP and SNAP-Ed program staff, including the Association of State Nutrition Network Administrators, National EFNEP Coordinators Meeting, and the Society for Nutrition Education. Finally, we will disseminate our findings through peer-reviewed, high impact journals. RE-AIM will be used to evaluate Reach, Efficacy, Adoption, Implementation, and Maintenance at the dissemination phase of the HH program, including how many EFNEP and SNAP-Ed staff are trained on the adapted HH program, the number of EFNEP and SNAP-Ed staff who decided to deliver it, and the number and representativeness of clients reached.
The primary goal of our study is to adapt an evidence-based obesity prevention intervention that prepares and empowers recipients to make informed choices about obesity-related behaviors. Through this research-practice partnership, there is the potential to produce long-term changes in obesity-related behaviors and weight gain trajectories for as many as 600,000 low-income individuals each year, including 450,000 children.
Acknowledgments
This project was supported by Grant Number 2011-67001-30109 from the National Institute of Food and Agriculture of the U.S. Department of Agriculture. Additional support for this project was provided by National Cancer Institute of the National Institutes of Health under Award Number R25CA057699. The content is solely the responsibility of the authors and does not necessarily represent the official views of the U.S. Department of Agriculture or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.World Health Organization. Obesity: preventing and managing the global epidemic, in World Health Organization Technical Report Series. 2000:i, xii. [PubMed] [Google Scholar]
- 2.Must A, et al. The disease burden associated with overweight and obesity. Jama-Journal of the American Medical Association. 1999;282(16):1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, et al. Prevalence of High Body Mass Index in US Children and Adolescents, 2007-2008. Jama-Journal of the American Medical Association. 2010;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, et al. Prevalence of overweight and obesity in the United States, 1999-2004. Jama-Journal of the American Medical Association. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 5.Ogden CL, C MD, Kit BK, Flegal KM. Prevalence of Childhood and Adult Obesity in the United States, 2011-2012. Jama-Journal of the American Medical Association. 2014;311(311):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fahlman MM, et al. Racial and Socioeconomic Disparities in Nutrition Behaviors: Targeted Interventions Needed. Journal of Nutrition Education and Behavior. 2010;42(1):10–16. doi: 10.1016/j.jneb.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 7.Olshansky S, Passaro DJ, Hershaw RC, et al. A Potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352(11):1138–1145. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- 8.Cunningham SA, Kramer MR, Narayan KM. Incidence of childhood obesity in the United States. N Engl J Med. 2014;370(5):403–11. doi: 10.1056/NEJMoa1309753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Isaacs R. Ethical implications of ethnic disparities in chronic kidney disease and kidney transplantation. Advances in Renal Replacement Therapy. 2004;11(1):55–58. doi: 10.1053/j.arrt.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 10.Hesketh KD, KJ Interventions to Prevent Obesity in 0-5 Year Olds: An Updated Systematic Review of the Literature. Obesity. 2010;18:S27–S35. doi: 10.1038/oby.2009.429. [DOI] [PubMed] [Google Scholar]
- 11.Fitzgibbon ML, et al. Two-year follow-up results for hip-hop to health Jr.: A randomized controlled trial for overweight prevention in preschool minority children. Journal of Pediatrics. 2005;146(5):618–625. doi: 10.1016/j.jpeds.2004.12.019. [DOI] [PubMed] [Google Scholar]
- 12.Estabrooks P, et al. Reporting of validity from school health promotion studies published in 12 leading journals, 1996-2000. Journal of School Health. 2003;73(1):21–28. doi: 10.1111/j.1746-1561.2003.tb06554.x. [DOI] [PubMed] [Google Scholar]
- 13.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322–7. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Westfall JM, Mold J, Fagnan L. Practice-based research--“Blue Highways” on the NIH roadmap. JAMA. 2007;297(4):403–6. doi: 10.1001/jama.297.4.403. [DOI] [PubMed] [Google Scholar]
- 15.Woolf SH. The meaning of translational research and why it matters. JAMA. 2008;299(2):211–3. doi: 10.1001/jama.2007.26. [DOI] [PubMed] [Google Scholar]
- 16.Burney J, Haughton B. EFNEP: A nutrition education program that demonstrates cost-benefit. Journal of the American Dietetic Association. 2002;102(1):39–45. doi: 10.1016/s0002-8223(02)90014-3. [DOI] [PubMed] [Google Scholar]
- 17.Deltredici AM, et al. Evaluation Study of the California-Expanded-Food-and-Nutrition-Education-Program - 24-Hour Food Recall Data. Journal of the American Dietetic Association. 1988;88(2):185–190. [PubMed] [Google Scholar]
- 18.Cullen KW, et al. Creating Healthful Home Food Environments: Results of a Study with Participants in the Expanded Food and Nutrition Education Program. Journal of Nutrition Education and Behavior. 2009;41(6):380–388. doi: 10.1016/j.jneb.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 19.Knowles MS. The Jossey-Bass management series. 1st. San Francisco: Jossey-Bass; 1984. Andragogy in action; p. xxiv.p. 444. [Google Scholar]
- 20.Perri MG, et al. Extended-care programs for weight management in rural communities: the treatment of obesity in underserved rural settings (TOURS) randomized trial. Arch Intern Med. 2008;168(21):2347–54. doi: 10.1001/archinte.168.21.2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paxton AE, et al. Starting the conversation performance of a brief dietary assessment and intervention tool for health professionals. Am J Prev Med. 2011;40(1):67–71. doi: 10.1016/j.amepre.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 22.Godin GS, RJ A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1995;10:141–146. [PubMed] [Google Scholar]
- 23.Borzekowski DL, Robinson TN. The remote, the mouse, and the no. 2 pencil: the household media environment and academic achievement among third grade students. Arch Pediatr Adolesc Med. 2005;159(7):607–13. doi: 10.1001/archpedi.159.7.607. [DOI] [PubMed] [Google Scholar]
- 24.Sallis JF, et al. The Development of Scales to Measure Social Support for Diet and Exercise Behaviors. Preventive Medicine. 1987;16(6):825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 25.Hughes SO, et al. Revisiting a neglected construct: parenting styles in a child-feeding context. Appetite. 2005;44(1):83–92. doi: 10.1016/j.appet.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 26.Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, N.J: L. Erlbaum Associates; 1988. p. xxi.p. 567. [Google Scholar]
- 27.Hintze J. In: Power Analysis and Sample Size (PASS) 2008. L, editor. Kaysville: NCSS; 2008. [Google Scholar]
- 28.Fitzmaurice GM, Laird NM, Ware JH. Wiley series in probability and statistics. 2nd. Hoboken, N.J.: Wiley; 2011. Applied longitudinal analysis; p. xxv.p. 701. [Google Scholar]
- 29.Molenberghs G, Verbeke G. Springer series in statistics. New York ; London: Springer; 2005. Models for discrete longitudinal data; p. xxii.p. 683. [Google Scholar]
- 30.Little RJA, Rubin DB. 2nd ed Wiley series in probability and statistics. Hoboken, N.J: Wiley; 2002. Statistical analysis with missing data; p. xv.p. 381. [Google Scholar]
- 31.Koh HK, et al. Translating Research Evidence Into Practice to Reduce Health Disparities: A Social Determinants Approach. American Journal of Public Health. 2010;100:S72–S80. doi: 10.2105/AJPH.2009.167353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ellis P, et al. A systematic review of studies evaluating diffusion and dissemination of selected cancer control interventions. Health Psychology. 2005;24(5):488–500. doi: 10.1037/0278-6133.24.5.488. [DOI] [PubMed] [Google Scholar]
- 33.Mercer SL, et al. Study designs for effectiveness and translation research -Identifying trade-offs. American Journal of Preventive Medicine. 2007;33(2):139–154. doi: 10.1016/j.amepre.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 34.Glasgow RE, Emmons KM. How can we increase translation of research into practice? Types of evidence needed. Annual Review of Public Health. 2007;28:413–433. doi: 10.1146/annurev.publhealth.28.021406.144145. [DOI] [PubMed] [Google Scholar]