Abstract
WHO categorizes causes of death and disability into (1) communicable diseases, maternal and perinatal conditions, and nutritional deficiencies; (2) non-communicable diseases (NCD); and (3) injuries. NCD are the leading cause of death and disability globally and are rising as a result of demographic and epidemiologic changes occurring in both developed and developing countries.1,2 Increasing life expectancies, unhealthy diet, physical inactivity, tobacco use, and harmful use of alcohol contribute to the growing incidence and prevalence of NCD, such as heart disease, stroke, diabetes, cancers, and chronic respiratory diseases. Deaths from communicable diseases, such as HIV/AIDS, tuberculosis, and malaria, are declining as a result of billions of dollars of annual international and domestic funding that target the prevention and treatment of these diseases. In recent years, less than 3% of official development assistance for health has been directed toward NCD.3 However, when measured in disability-adjusted life-years (DALY), NCD accounted for 54% of the global burden of disease in 2010, compared to 43% in 1990.1 DALY are the sum of 2 components: years of life lost due to premature mortality and years lived with disability. One DALY is the equivalent of one healthy life-year lost (for a complete definition of DALY, see reference 1). DALY are a particularly useful metric to quantify the burden of NCD (e.g., stroke) that often result in long-term disability for survivors.
WHO categorizes causes of death and disability into (1) communicable diseases, maternal and perinatal conditions, and nutritional deficiencies; (2) non-communicable diseases (NCD); and (3) injuries. NCD are the leading cause of death and disability globally and are rising as a result of demographic and epidemiologic changes occurring in both developed and developing countries.1,2 Increasing life expectancies, unhealthy diet, physical inactivity, tobacco use, and harmful use of alcohol contribute to the growing incidence and prevalence of NCD, such as heart disease, stroke, diabetes, cancers, and chronic respiratory diseases. Deaths from communicable diseases, such as HIV/AIDS, tuberculosis, and malaria, are declining as a result of billions of dollars of annual international and domestic funding that target the prevention and treatment of these diseases. In recent years, less than 3% of official development assistance for health has been directed toward NCD.3 However, when measured in disability-adjusted life-years (DALY), NCD accounted for 54% of the global burden of disease in 2010, compared to 43% in 1990.1 DALY are the sum of 2 components: years of life lost due to premature mortality and years lived with disability. One DALY is the equivalent of one healthy life-year lost (for a complete definition of DALY, see reference 1). DALY are a particularly useful metric to quantify the burden of NCD (e.g., stroke) that often result in long-term disability for survivors.
In addition to affecting health outcomes, NCD contribute to poverty and are a major barrier to economic development. According to a study conducted by the World Economic Forum, the Harvard School of Public Health, and WHO, the lost economic output from cardiovascular disease (including stroke), diabetes, cancer, and chronic respiratory disease in low- and middle-income countries (LMIC) is estimated to exceed USD $7 trillion over the period 2011–2025.4 WHO has identified a number of cost-effective interventions (“best buys”) at the population-wide and individual health care levels to address NCD in LMIC. For example, interventions to reduce mortality from stroke and ischemic heart disease by 10% are projected to reduce economic losses by an average of USD $25 billion annually with a threefold return on investment.4
The massive health and economic impacts of NCD have raised the issue to an international health policy level. The year 2012 will be remembered as a watershed year when the global health conversation shifted its emphasis from communicable diseases to NCD. The United Nations High-Level Summit on the Prevention and Control of NCD set the agenda for the 2012 World Health Assembly where member states agreed to adopt a global target of a 25% reduction in premature deaths from NCD by 2025. Significantly, in November 2012, WHO member states agreed to the first-ever global monitoring framework to combat NCD, including 25 indicators and 9 voluntary global targets. The targets call for reducing premature mortality from NCD, harmful use of alcohol, physical inactivity, diabetes and obesity, raised blood pressure, salt/sodium intake, and tobacco use and increasing access to drug therapy to prevent heart attacks and stroke, essential NCD medicines, and basic technologies to treat major NCD.
Where does neurology stand in the global burden of disease? According to the recently published Global Burden of Disease 2010 Study (GBD 2010),1 stroke is the second leading cause of death globally and the third leading cause of premature death and disability as measured in DALY. Ischemic heart disease, sharing many risk factors of stroke, is the leading cause of both death and premature death and disability. The GBD 2010 quantifies DALY for cerebrovascular disease (ischemic, hemorrhagic, and other nonischemic stroke) in the category “Cardiovascular and circulatory diseases.” This is separate from the category “Neurological disorders,” which includes subcategories of Alzheimer disease (AD) and other dementias, Parkinson disease (PD), epilepsy, multiple sclerosis (MS), migraine, tension-type headache, and other neurologic disorders. Neurologic disorders and cerebrovascular disease combined represent 7.1% of the total global burden of disease measured in DALY for all causes and ages. Cerebrovascular disease is the largest neurologic contributor and accounts for 4.1% of total global DALY, followed by headaches (0.97%; migraine 0.90%, tension-type headache 0.07%), other neurologic disorders (0.72%), epilepsy (0.70%), AD and other dementias (0.46%), PD (0.08%), and MS (0.04%). Neurologic conditions not included in the category of neurologic disorders include meningitis (1.2%), encephalitis (0.29%), and traumatic brain injury (TBI). All TBIs are recorded within the subcategories of “Injuries” that, as a group, represent 11.2% of total global DALY.1 Within the combined burden of neurologic disorders and cerebrovascular disease as measured in the GBD 2010, hemorrhagic stroke (35.7%) and ischemic stroke (22.4%) contribute the largest proportions of DALY, followed by migraine (12.7%), other neurologic disorders (10.2%), epilepsy (9.9%), AD and other dementias (6.4%), PD (1.1%), tension-type headache (1.0%), and MS (0.6%) (figure). The greater global burden of hemorrhagic stroke compared to ischemic stroke is attributable to (1) the large contribution of stroke in Asia (Central, East, South, and Southeast) to the global burden of stroke (59% of global stroke DALY) and (2) the substantially higher share of DALY for hemorrhagic stroke in Asia (70% of all stroke DALY in Asia).
Figure. Contribution of specific causes to the combined burden of neurologic disorders and cerebrovascular disease (percent of total disability-adjusted life-years).
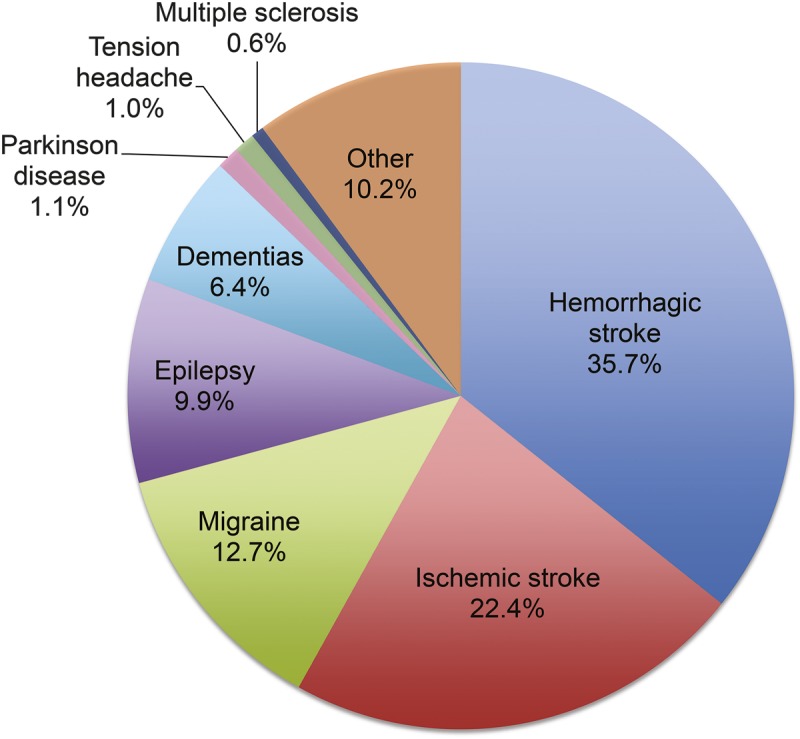
Source: GBD 2010 Results by Cause 1990–2010. Available at: http://ghdx.healthmetricsandevaluation.org/global-burden-disease-study-2010-gbd-2010-data-downloads.
Regional differences in the contribution of neurologic disorders and stroke to the total burden of disease measured in DALY are shown in the table. LMIC have a smaller relative contribution of neurologic disorders and cerebrovascular disease compared to high-income regions because of the large burden of communicable diseases. However, the absolute burden is 6 times higher among LMIC compared to high-income regions, largely due to epilepsy (14-fold higher), cerebrovascular disease (8-fold higher), and migraine (6-fold higher). Age-adjusted mortality rates for stroke in LMIC are 3–4 times higher than in high-income countries.5 In the least developed countries, resources for acute stroke treatment and care are extremely limited, making primary and secondary prevention strategies critical to reducing the burden of disease.6 Building capacity for community-based screening programs and affordable treatments to address leading risk factors, particularly hypertension, is essential.6,7 The majority of people living with epilepsy in LMIC do not have access to appropriate care and treatment. Barriers to closing this massive treatment gap include shortages of trained health workers, inadequate supplies of antiepileptic medications, transportation, stigma, and discrimination.8,9
Table.
DALY for all causes and for neurologic disorders and cerebrovascular disease, stratified by region and income

Findings of the GBD 2010 shed light on the heavy impact of neurologic disorders and cerebrovascular disease in LMIC. However, rigorous population-based epidemiologic studies are needed in many resource-constrained countries to better target solutions. This challenge can only be addressed with the financial support and collaboration of research centers in developed countries. Coordinated advocacy efforts and stronger financial commitments will be necessary to raise the priority of neurologic diseases in health policy development and program planning at global, regional, and national levels.
STUDY FUNDING
No targeted funding reported.
DISCLOSURE
The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Murray CJL, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2197–2223 [DOI] [PubMed] [Google Scholar]
- 2.The Growing Danger of Non-Communicable Diseases: Acting Now to Reverse Course, Conference edition Washington, DC: The World Bank; 2011. Available at: http://documents.worldbank.org/curated/en/2011/09/15512807/growing-danger-non-communicable-diseases-acting-now-reverse-course. Accessed July 21, 2013 [Google Scholar]
- 3.Nugent RA, Feigl AB. Where Have All the Donors Gone? Scarce Donor Funding for Non-Communicable Diseases. CGD Working Paper 228. Washington, DC: Center for Global Development; 2010. Available at: http://www.cgdev.org/content/publications/detail/1424546. Accessed July 21, 2013 [Google Scholar]
- 4.World Economic Forum and World Health Organization. From Burden to “Best Buys”: Reducing the Economic Impact of Non-Communicable Diseases in Low- and Middle-Income Countries. Geneva: World Economic Forum; 2011. Available at: http://www.who.int/nmh/publications/best_buys_summary/en/. Accessed July 21, 2013 [Google Scholar]
- 5.Johnston SC, Mendis S, Mathers CD. Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. Lancet Neurol 2009;8:345–354 [DOI] [PubMed] [Google Scholar]
- 6.Chin JH. Stroke in sub-Saharan Africa: an urgent call for prevention. Neurology 2012;78:1007–1008 [DOI] [PubMed] [Google Scholar]
- 7.O'Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorraghic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 2010;376:112–123 [DOI] [PubMed] [Google Scholar]
- 8.Meyer AC, Dua T, Ma J, et al. Global disparities in the epilepsy treatment gap: a systematic review. Bull World Health Organ 2010;88:260–266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chin JH. The global fund for epilepsy: a proposal. Neurology 2013;80:754–755 [DOI] [PubMed] [Google Scholar]


