Abstract
Objective
To assess potential selection bias in participant recruitment for randomized clinical trials (RCTs) of adolescent eating disorders (ED), we compared participants recruited for RCTs evaluating psychosocial treatments with individuals seeking fee-for-service outpatient ED treatment (CTS).
Method
Participants were 214 adolescents presenting to an outpatient ED research-clinical program (92.1% female; M age=15.4±1.8). ANOVA and chi-square tests assessed differences between CTS participants and those presenting for no-cost treatment through RCTs. A secondary analysis compared RCT participants to participants eligible for the RCTs that opted for fee-for-service treatment.
Results
RCT participants had greater baseline ED and general psychopathology (ps<.001); however, CTS participants were more likely to present with a comorbid psychiatric disorder (p<.05) and higher family income (p<.05).
Discussion
Results suggest that RCT participants did not have less pathology than CTS participants. While preliminary, results do not indicate a systematic population bias in selecting healthier patients for RCTs involving adolescent ED.
Keywords: recruitment, adolescent eating disorders, representative samples
Eating disorders (ED) are a public health concern associated with significant morbidity and mortality (Jacobi et al., 2004, Keel et al., 2003). Early identification and treatment is therefore critical (Le Grange and Loeb, 2007). Despite the negative physical and psychosocial health outcomes associated with EDs, treatment is underutilized (Vitiello and Lederhendler, 2000, Fairburn et al., 1993) and clinical trials often have difficulties with recruitment and retention (Halmi et al., 2005).
Some investigators argue that research findings are not always generalizable to community populations (Kazdin, 2008) because study participants must meet pre-defined inclusion criteria. This may be particularly important in ED research, as many patients are diagnosed with eating disorder not otherwise specified (EDNOS) (Eddy et al., 2008) and hence might not qualify for studies with rigid entry criteria based on diagnostic categories. Research studies often have utilized manualized treatments with specified numbers of sessions and time course of treatment (Westen et al., 2004) which might dissuade potential participants with greater psychopathology or comorbidities from enrolling. If this were the case, randomized controlled trial (RCT) samples would be skewed toward those with less severe psychopathology and the results obtained might not be generalizable to patients with more complex presentations (Godart et al., 2007, Humphreys and Weisner, 2000). However, at least one study suggests that most clinic outpatients would meet inclusion criteria for a prior published RCT (Stirman et al., 2003). This finding has been supported by ED research reporting more similarities than differences among adult clinic and research samples in terms of symptom severity, but not in demographic features (e.g., age, level of education) (Wilfley et al., 2001).
It is important to better understand how fee-for-service clinic and research samples compare for purposes of recruitment, as well as to gain more insight into the generalizability of research findings to clinic samples. To our knowledge, no research has compared children and adolescents with EDs seeking outpatient treatment through a fee-for-service clinic or RCT. The purpose of the current study was to fill this gap in the literature by comparing demographic, eating-related, and psychosocial characteristics of an adolescent sample with EDs that are clinic treatment-seeking (CTS) or research treatment-seeking through an RCT. We hypothesized that, consistent with previous research in the adult ED field (Wilfley et al., 2001), differences in demographics would be found between the two groups. Specifically, we expected that CTS participants would have a higher family income than RCT participants, given that the RCTs offering treatment for this sample are at no-cost to participants. We also hypothesized that, consistent with previous findings (Stirman et al., 2003, Wilfley et al., 2001), the two groups would not significantly differ in terms of eating-related or general psychopathology, but that the CTS sample would be more likely to have a comorbid diagnosis, as this might not be addressed in an RCT or such patients might be excluded from RCTs. As there could be differences in samples during a recruitment period for an RCT compared to usual practice, we conducted a secondary analysis comparing adolescents randomized to an RCT to those who presented for treatment during the recruitment window for an RCT and met inclusion criteria for an RCT, but opted to receive fee-for-service treatment.
Methods
Participants
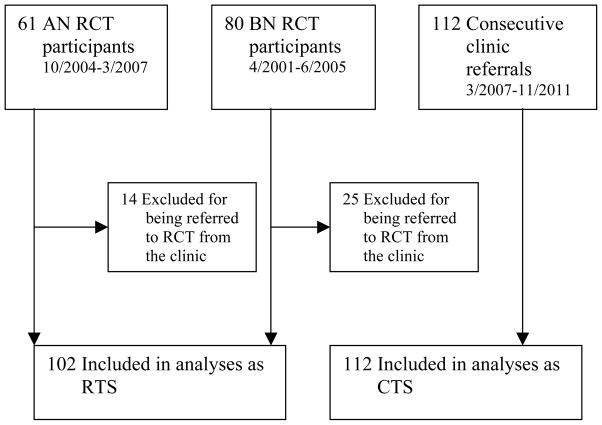
Participants for the primary analysis were adolescents (n=214), aged 12 to 19 years (M age=15.4±1.8 years) presenting for treatment at The University of Chicago Medicine’s Eating Disorders Program. Participants were either consecutive referrals for two RCTs for adolescents with anorexia nervosa (AN) (Lock et al., 2010) and bulimia nervosa (BN) (Le Grange et al., 2007), or consecutive referrals to our outpatient clinic (see Figure 1). Participants had a mean body mass index (BMI; kg/m2) of 19.3±5.0, and were comprised of mostly females (92.1%; n=197) and Caucasians (76.2%; n=163). Participants met Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM IV-TR) criteria for AN (39.3%; n=84; Mean BMI=16.1±1.2), BN (14.0%; n=30; Mean BMI=20.6±1.8), or EDNOS (46.7%; n=100; Mean BMI=21.0±7.1).
Figure 1.
Study flowchart. AN, anorexia nervosa; RCT, randomized controlled trial; BN, bulimia nervosa; RTS, research treatment-seeking; CTS, clinic treatment-seeking.
Procedure
RCT participants were direct referrals from health care professionals (50.9%), word of mouth (17.6%), Internet searches (16.7%), or participants that were familiar with past publications by the senior author (14.8%). Of the 141 participants recruited for an RCT, 39 were excluded from this sub-sample as they had been referred to the study through the outpatient clinic and therefore were not specifically seeking treatment through an RCT, despite ultimately qualifying and participating in RCTs.
Recruitment for the RCT of adolescents with BN occurred from April 2001 to June 2005. This RCT (n=80) evaluated the relative efficacy of family-based treatment (FBT) and supportive psychotherapy (SPT) for adolescents with BN; treatment was at no-cost. Participants were eligible for randomization if they were ages 12–19, lived with at least one adult caregiver, and met criteria for BN or the BN subtype of EDNOS. Exclusion criteria were the presence of a physical or psychiatric disorder necessitating hospitalization, insufficient knowledge of English, current substance dependence, a BMI below 17.5, and current use of medication and/or physical conditions known to affect eating or weight (Le Grange et al., 2007).
Recruitment for a multi-site RCT of adolescents with AN (n=121) occurred from October 2004 to March 2007. This RCT evaluated the relative efficacy of FBT and adolescent-focused individual therapy (AFT) for adolescents with AN; treatment was at no-cost and 61 patients were enrolled at The University of Chicago site. Participants were eligible for randomization if they were ages 12–18, were living with at least one legal guardian, and met the DSM-IV criteria for AN excluding the amenorrhea criterion. Exclusion criteria were the presence of a current psychotic disorder or physical condition known to influence eating or weight, current substance dependence, or previous ED treatment with FBT or AFT (Lock et al., 2010).
Participants presenting for fee-for-service treatment at The University of Chicago Medicine’s Eating Disorders Program’s outpatient clinic were recruited from March 2007 to November 2011. During this time period, there were no ongoing recruiting efforts for research participants for either AN or BN. Participants were direct referrals from health care professionals, word of mouth, Internet searches, and participants familiar with past publications by the principle investigator.
To examine the potential bias of recruitment associated with an ongoing RCT, participants that received fee-for-service treatment at The University of Chicago Medicine’s Eating Disorders Program’s outpatient clinic that also qualified for the RCTs of adolescents with BN and AN but declined RCT treatment were included in secondary analyses if they presented for treatment from April 2001 to June 2005 or October 2004 to March 2007, respectively.
All participants, regardless of treatment type sought, completed semi-structured interviews and questionnaires during a baseline assessment to establish diagnosis and severity. Assessments were conducted by bachelors-level research assistants who completed at least 20 hours of training and received weekly assessment supervision to ensure standardized delivery. Written consent for patients over 18 years of age or guardian consent and adolescent assent for patients under 18 years of age were obtained. All studies were approved by The University of Chicago and Stanford University’s Institutional Review Board.
Physical Assessment
Participants’ weight and height were measured by a trained research assistant using a calibrated digital or balance-beam scale and stadiometer, respectively. All patients were weighed in light indoor clothing.
Measures
The Eating Disorder Examination (EDE) (Cooper and Fairburn, 1987) is a semi-structured investigator-based interview measuring cognitive and behavioral symptoms related to ED. Global scores reflect the overall severity of ED symptoms. Frequency of self-induced vomiting, laxative and diuretic misuse, and loss of control eating (eating episodes characterized by the sense that one cannot control what or how much one is eating) is assessed for 3 months prior to assessment. The EDE has demonstrated good reliability and validity (Grilo et al., 2004, Rizvi et al., 2000). The EDE was used to generate DSM-IV-TR diagnoses for an ED.
Schedule for Affective Disorders and Schizophrenia for School-Aged Children (K-SADS) is a semi-structured diagnostic interview designed to assess current and past presence of psychiatric disorders in children and adolescents according to DSM-IV criteria. The K-SADS has demonstrated good reliability (Chambers et al., 1985).
The Beck Depression Inventory (BDI) (Beck, 1987) is a 21-item self-report questionnaire designed to assess depressive symptoms. The BDI has good psychometric properties (Barrera and Garrison-Jones, 1988, Kashani et al., 1990).
Data Analysis
ANOVA and chi-square analyses were used to compare RCT and CST participants on demographic variables. ANCOVA’s, controlling for DSM-IV diagnosis, were used to compare RCT and CST participants on continuous measures of eating-related and general psychopathology.
As a secondary analysis, ANOVA, chi-square, and ANCOVA’s, controlling for DSM-IV diagnosis, were used to compare RCT participants to participants treated through the outpatient clinic that met study inclusion criteria during the open recruitment of the RCTs for AN and BN on demographic variables and continuous measures of eating-related and general psychopathology.
Results
A total of 112 (52.3%) adolescents were CTS and 102 (47.7%) were seeking treatment through an RCT for AN or BN. CTS participants had significantly higher family incomes [F(1,128)=7.48; p=.007, η2=.056; see Table 1]; they were also more likely to be diagnosed with EDNOS and less likely to be diagnosed with BN, compared to RCT participants [χ2(2, N=214)=34.6; p<.001, ϕc=.402]. There were no group differences in terms of age, BMI, gender, race, or family status (i.e., intact or non-intact).
Table 1.
Distribution of eating-related and psychosocial variables by treatment type sought (M±SD, unless otherwise indicated)
| Variables | Outpatient Clinic (n=112) | No-Cost Outpatient Research (n=102) | Total Sample (n=214) | Test Statistic |
|---|---|---|---|---|
| Age (years) | 15.4±1.8 | 15.4±1.7 | 15.4±1.8 | F(1,214)=.000; p=.99, η2=.00 |
| Gender | ||||
| Male | 10 (8.9%) | 7 (6.9%) | 17 (7.9%) | χ2(1, N=214)=.312; p=.58, ϕc=.038 |
| Female | 102 (91.1%) | 95 (93.1%) | 197 (92.1%) | |
| Ethnicity | ||||
| Caucasian | 86 (76.8%) | 77 (75.5%) | 163 (76.2%) | χ2(1, N=213)=.117; p=.73, ϕc=.102 |
| Minority | 25 (22.3%) | 25 (24.2%) | 50 (23.4%) | |
| BMI | 19.4±6.1 | 19.3±3.5 | 19.3±5.0 | F(1,213)=0.21; p=.89, η2=.00 |
| Family Income (in US dollars) | 158,218±169,402 | 98,472±68,364 | 124,144±125,432 | F(1,128)=7.48; p=.007, η2=.056 |
| Family Status | ||||
| Intact | 85 (75.9%) | 72 (70.6%) | 157 (73.4%) | χ2(1, N=214)=.769; p=.38, ϕc=.060 |
| Not Intact | 21 (24.1%) | 30 (29.4%) | 57 (26.6%) | |
|
| ||||
| DSM-IV TR | ||||
| Diagnosis | ||||
| AN | 37 (33.0%) | 47 (46.1%) | 84 (39.3%) | χ2(2, N=214)=34.6; p<.001, ϕc=.402 |
| BN | 4 (3.6%) | 26 (25.5%) | 30 (14.0%) | |
| EDNOS | 71 (63.4%) | 29 (28.4%) | 100 (46.7%) | |
| Sub-AN | 32 (45.1%) | |||
| Sub-BN | 10 (14.1%) | |||
| EDE Global Score | 2.28±1.5 | 2.85±1.6 | 2.55±1.5 | F(2, 214)=8.73; p<.001, η2=.076 |
| LOC Episode | ||||
| Yes | 47 (42.0%) | 71 (69.6%) | 118 (55.1%) | χ2(1, N=214)=16.5; p<.001, ϕc=.278 |
| No | 65 (58.0%) | 31 (30.4%) | 96 (44.9%) | |
| Purging | ||||
| Yes | 32 (28.6%) | 61 (59.8%) | 93 (43.5%) | χ2(1, N=214)=21.2; p<.001, ϕc=.315 |
| No | 80 (71.4%) | 41 (40.2%) | 121 (56.5%) | |
| BDI Total Score | 14.25±10.54 | 20.65±12.83 | 17.40±12.13 | F(2, 203)=12.16; p<.001, η2=.108 |
| Comorbid | ||||
| Diagnosis | ||||
| Yes | 59 (56.7%) | 39 (38.2%) | 98 (47.6%) | χ2(1, N=206)=7.06; p=.008, ϕc=.185 |
| No | 45 (43.3%) | 63 (61.8%) | 108 (52.4%) | |
Note: BMI=Body Mass Index; US=United States; DSM-IV TR=Diagnostic and Statistical Manual of Mental Disorder Fourth Edition, Text Revision; AN=Anorexia Nervosa; BN=Bulimia Nervosa; EDNOS=Eating Disorder Not Otherwise Specified; EDE=Eating Disorder Examination; LOC=Loss of Control eating in three months prior to baseline; BDI=Beck Depression Inventory.
Eating-related and general psychopathology in relation to treatment type sought
RCT participants had significantly higher EDE global scores than CTS participants [F(2, 214)=8.73; p<.001, η2=.076]. The RCT group was also more likely to report loss of control eating and purging in the 3 months prior to the baseline assessment (ps<.001). RCT participants also had significantly higher BDI total scores than CTS participants [F(2, 202)=12.16; p<.001, η2=.108]. CTS participants were significantly more likely to have a comorbid diagnosis at baseline [χ2(1, N=206)=7.06; p=.008, ϕc=.185]; most comorbid diagnoses were related to depression (52.9%) and anxiety (22.5%).
Comparison of RCT participants and fee-for-service participants treated during RCT recruitment
A total of 61 adolescents (M age=15.4±2.0) that met study inclusion criteria during the open recruitment of the RCTs for AN and BN received fee-for-service treatment through the outpatient clinic. The sample consisted of 34 participants that met inclusion criteria for the RCT for adolescent AN (55.7%; Mean BMI=17.4±1.3) and 27 participants that met inclusion criteria for the RCT for adolescent BN (44.3%; Mean BMI=24.1±4.7).
The RCT and concurrent clinic sample did not differ significantly on any demographic variables (ps>.07), including family income (p=.3) and family status (p>.07). RCT participants had significantly higher EDE global scores [F(2, 162)=23.3; p=.004, η2=.137] and BDI total scores [F(2, 154)=3.7; p=.03, η2=.182], and were more likely to endorse episodes of purging in the prior three months [χ2(1, N=162)=7.0; p=.008, ϕc=.208] than their fee-for-service counterparts. Fee-for-service participants meeting RCT inclusion criteria had significantly higher BMIs than the RCT sample [F(2, 162)=18.9; p<.001, η2=.324]. There were no significant differences in frequency of endorsing episodes of loss of control (p=.75) or having a comorbid diagnosis (p=.26).
Discussion
To understand if there was systematic selection bias toward including less severely ill patients in RCTs of adolescents with EDs, we compared demographic characteristics and eating-related and general psychopathology among adolescents with EDs seeking either outpatient fee-for-service treatment or treatment offered at no cost via an RCT. Secondary analyses examined the same variables among adolescents that met study inclusion criteria who sought either treatment offered at no cost via an RCT, or outpatient fee-for-service treatment during open recruitment for the RCTs. Consistent with our hypotheses, participants seeking outpatient treatment through an RCT demonstrated greater baseline ED and depressive symptomatology. Conversely, CTS participants came from families with a significantly higher yearly income and were more likely to be diagnosed with a comorbid psychiatric disorder at baseline; these differences were not significant in the comparison involving the fee-for-service sample that met study inclusion criteria.
The higher yearly incomes of families seeking treatment through our clinic may indicate a level of financial security that enabled such families to be less concerned about whether their children receive no-cost research treatment. The clinical meaning of this difference is unknown, but providing no-cost treatment therefore might not be an effective recruitment strategy for patients with higher socio-economic status in the United States. Interestingly, patients who were offered but declined RCT treatment did not differ from those who elected RCT treatment on family income. These findings are of note for the treatment of adolescents with EDs in the United States; however it is unclear if similar trends would be present in countries with a national healthcare system. There is a need to better understand factors that motivate families with and without the option of a national healthcare system to opt for fee-for-service treatment when RCT treatment is available in order to engage families’ interest in RCT treatments.
Some prior research has shown that the majority of Axis I disorders are comorbid with other Axis I or II disorders (Zaider et al., 2000, Fischer and Le Grange, 2007, Westen et al., 2004), but research studies generally focus on treating one primary disorder (Westen et al., 2004). Our findings suggest those with more comorbid conditions sought treatment through our clinic rather than the RCTs. Such patients may prefer clinic treatment because they anticipate that this route of treatment will be more flexible and allow treatment for all present diagnoses. We found this difference between clinic and RCT participants even though the RCTs included in this study allowed participants with co-morbid disorders and succeeded in recruiting a high percentage of participants with co-morbid disorders (AN=43%; BN=63%). Future studies might consider designs which allow for adapting treatments for participants with co-morbid conditions to minimize differences between clinic patients and those enrolling in an RCT.
It is of note that the higher rates of co-morbid disorders in the clinic participants did not align with more severe ED symptomology compared with those enrolling in an RCT. More severe ED symptoms, such as loss of control eating, among RCT participants may be related to the findings that participants in this sample were more likely to be diagnosed with BN than EDNOS. While ED diagnosis was controlled for in the analyses, it is of note that the CTS sample had few participants diagnosed with BN (n=4); yet many of the participants diagnosed with EDNOS had sub-threshold BN. The discrepancy in representation of participants with BN may suggest that participants with different diagnostic thresholds may seek different methods of treatment. However, the differences in ED symptoms remained in the comparison of RCT participants to their counterparts that received fee-for-service treatment during the same time period despite the fact that the fee-for-service sample contained a larger number of participants with BN (n=27) than the CTS sample.
To our knowledge, this is the first study to investigate an adolescent sample with EDs in terms of type of treatment sought. Understanding the differences and similarities of CTS and RCT groups provides insights into the generalizability of research findings. Our findings indicate that research inclusion criteria for treatment-seeking adolescents with EDs in the studies examined were not strongly biased towards those with less severe psychopathology.
Strengths of this analysis include a reasonably large and diverse sample assessed with well-validated measures. Yet important limitations also warrant acknowledgment. Our assessment of pathology was limited to eating-related and depressive symptomology and the presence or absence of a comorbid diagnosis. Additionally, in the primary analyses, the CTS sample was recruited at a time when an RCT was unavailable; this brings into question whether any participants from the CTS sample may have also investigated participating in an RCT had one been available during the time of treatment-seeking. To address this limitation, we included a secondary analysis of participants meeting inclusion criteria for the RCTs that received fee-for-service treatment during the recruitment for the RCTs and the pattern of results was largely similar. The CTS sample also sought treatment from a specialist, outpatient ED service that requires medical stability for treatment and it remains unclear how representative these patients are of those who seek treatment from community settings or of patients with medical instability or low BMIs who seek treatment from inpatient settings. Additionally, as we were unable to analyze duration of illness prior to assessment for all samples, it is unclear how such information may impact the interpretation of differences in severity between the RTC and CTS samples. This research was conducted in the United States and it is unclear how these results generalize to countries with national health care (e.g., Canada, Australia and most of Europe). Future studies should explore differences in larger samples in clinical, community, and research settings in terms other psychological factors, such as anxiety, as well as differences in treatment outcome.
In summary, the findings of the present study suggest that the assumption that research samples of adolescents with EDs are less severe than clinic samples is not supported. Future research with improved sampling techniques should examine other psychological factors, such as anxiety, and treatment outcome in relation to research and clinic samples.
References
- Barrera M, Garrison-Jones CV. Properties of the beck depression inventory as a screening instrument for adolescent depression. Journal of Abnormal Child Psychology. 1988;16:263–273. doi: 10.1007/BF00913799. [DOI] [PubMed] [Google Scholar]
- Beck AT. Beck Depression Inventory. San Antonia, TX: Psychological Corporation; 1987. [Google Scholar]
- Chambers W, Puig-Antich J, Hirsch M, Paez P, Ambrosini P, Tabrizi MA, Davies M. The assessment of affective disorders in children and adolescents by semistructured interview: Test-retest reliability of the Schedule for Affective Disorders and Schizophrenia for School-Age Children, present episode version. Archives of General Psychiatry. 1985;42:696–702. doi: 10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- Cooper Z, Fairburn CG. The Eating Disorder Examination: A semistructured interview for the assessment of the specific psychopathology of eating disorders. International Journal of Eating Disorders. 1987;6:1–8. [Google Scholar]
- Eddy KT, Celio Doyle A, Rienecke Hoste R, Herzog DB, Le Grange D. Eating Disorder Not Otherwise Specified in Adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:156–164. doi: 10.1097/chi.0b013e31815cd9cf. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Hay PJ, Welch SL. Binge eating: Nature, assessment, and treatment. New York, NY, US: Guilford Press; 1993. Binge eating and bulimia nervosa: Distribution and determinants. [Google Scholar]
- Fischer S, Le Grange D. Comorbidity and high-risk behaviors in treatment-seeking adolescents with bulimia nervosa. International Journal of Eating Disorders. 2007;40:751–753. doi: 10.1002/eat.20442. [DOI] [PubMed] [Google Scholar]
- Godart NT, Perdereau F, Rein Z, Berthoz S, Wallier J, Jeammet P, Flament MF. Comorbidity studies of eating disorders and mood disorders. Critical review of the literature. Journal of Affective Disorders. 2007;97:37–49. doi: 10.1016/j.jad.2006.06.023. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Lozano-Blanco C, Barry DT. Reliability of the Eating Disorder Examination in patients with binge eating disorder. International Journal of Eating Disorders. 2004;35:80–85. doi: 10.1002/eat.10238. [DOI] [PubMed] [Google Scholar]
- Halmi KA, Agras WS, Crow S, Mitchell J, Wilson GT, Bryson SW, Kraemer HC. Predictors of Treatment Acceptance and Completion in Anorexia Nervosa: Implications for Future Study Designs. Archives of General Psychiatry. 2005;62:776–781. doi: 10.1001/archpsyc.62.7.776. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Weisner C. Use of exclusion criteria in selecting research subjects and its effect on the generalizability of alcohol treatment outcome studies. American Journal of Psychiatry. 2000;157:588–594. doi: 10.1176/appi.ajp.157.4.588. [DOI] [PubMed] [Google Scholar]
- Jacobi C, Hayward C, De Zwaan M, Kraemer HC, Agras WS. Coming to Terms With Risk Factors for Eating Disorders: Application of Risk Terminology and Suggestions for a General Taxonomy. Psychological Bulletin. 2004;130:19–65. doi: 10.1037/0033-2909.130.1.19. [DOI] [PubMed] [Google Scholar]
- Kashani JH, Sherman DD, Parker DR, Reid JC. Utility of the Beck Depression Inventory with Clinic-Referred Adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1990;29:278–282. doi: 10.1097/00004583-199003000-00018. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Evidence-based treatment and practice: new opportunities to bridge clinical research and practice, enhance the knowledge base, and improve patient care. Am Psychol. 2008;63:146–59. doi: 10.1037/0003-066X.63.3.146. [DOI] [PubMed] [Google Scholar]
- Keel PK, Dorer DJ, Eddy KT, Franko D, Charatan DL, Herzog DB. Predictors of Mortality in Eating Disorders. Archives of General Psychiatry. 2003;60:179–183. doi: 10.1001/archpsyc.60.2.179. [DOI] [PubMed] [Google Scholar]
- Le Grange D, Crosby RD, Rathouz PJ, Leventhal BL. A Randomized Controlled Comparison of Family-Based Treatment and Supportive Psychotherapy for Adolescent Bulimia Nervosa. Archives of General Psychiatry. 2007;64:1049–1056. doi: 10.1001/archpsyc.64.9.1049. [DOI] [PubMed] [Google Scholar]
- Le Grange D, Loeb KL. Early identification and treatment of eating disorders: prodrome to syndrome. Early Intervention in Psychiatry. 2007;1:27–39. doi: 10.1111/j.1751-7893.2007.00007.x. [DOI] [PubMed] [Google Scholar]
- Lock J, Le Grange D, Agras WS, Moye A, Bryson SW, Jo B. Randomized Clinical Trial Comparing Family-Based Treatment With Adolescent-Focused Individual Therapy for Adolescents With Anorexia Nervosa. Archives of General Psychiatry. 2010;67:1025–1032. doi: 10.1001/archgenpsychiatry.2010.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi SL, Peterson CB, Crow SJ, Agras WS. Test-retest reliability of the eating disorder examination. International Journal of Eating Disorders. 2000;28:311–316. doi: 10.1002/1098-108x(200011)28:3<311::aid-eat8>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- Stirman SW, Derubeis RJ, Crits-Christoph P, Brody PE. Are Samples in Randomized Controlled Trials of Psychotherapy Representative of Community Outpatients? A New Methodology and Initial Findings. Journal of Consulting and Clinical Psychology. 2003;71:963–972. doi: 10.1037/0022-006X.71.6.963. [DOI] [PubMed] [Google Scholar]
- Vitiello B, Lederhendler I. Research on eating disorders: current status and future prospects. Biological Psychiatry. 2000;47:777–786. doi: 10.1016/s0006-3223(99)00319-4. [DOI] [PubMed] [Google Scholar]
- Westen D, Novotny C, Thompson-Brenner H. The empirical status of empirically supported psychotherapies: Assumptions, findings, and reporting in controlled clinical trials. Psychological Bulletin. 2004;130:631–663. doi: 10.1037/0033-2909.130.4.631. [DOI] [PubMed] [Google Scholar]
- Wilfley D, Pike KM, Dohm F, Striegel-Moore R, Fairburn CG. Bias in binge eating disorder: How representative are recruited clinic samples? Journal of Consulting and Clin Psychol. 2001;69:383–388. doi: 10.1037//0022-006x.69.3.383. [DOI] [PubMed] [Google Scholar]
- Zaider TI, Johnson JG, Cockell SJ. Psychiatric comorbidity associated with eating disorder symptomatology among adolescents in the community. International Journal of Eating Disorders. 2000;28:58–67. doi: 10.1002/(sici)1098-108x(200007)28:1<58::aid-eat7>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]