Abstract
Lipophilic persistent environmental chemicals (LPECs) have the potential to accumulate within a woman’s body lipids over the course of many years prior to pregnancy, to partition into human milk, and to transfer to infants upon breastfeeding. As a result of this accumulation and partitioning, a breastfeeding infant’s intake of these LPECs may be much greater than his/her mother’s average daily exposure. Because the developmental period sets the stage for lifelong health, it is important to be able to accurately assess chemical exposures in early life. In many cases, current human health risk assessment methods do not account for differences between maternal and infant exposures to LPECs or for lifestage-specific effects of exposure to these chemicals. Because of their persistence and accumulation in body lipids and partitioning into breast milk, LPECs present unique challenges for each component of the human health risk assessment process, including hazard identification, dose-response assessment, and exposure assessment. Specific biological modeling approaches are available to support both dose-response and exposure assessment for lactational exposures to LPECs. Yet, lack of data limits the application of these approaches. The goal of this review is to outline the available approaches and to identify key issues that, if addressed, could improve efforts to apply these approaches to risk assessment of lactational exposure to these chemicals.
Keywords: children, exposure, PBT chemicals, persistent organic pollutants, POPs, research needs, risk assessment, uncertainty
Introduction
This review derives from a workshop held in Research Triangle Park, North Carolina, in October 2012 to discuss innovative approaches to the assessment of early life exposure to and potential health effects from persistent environmental chemicals (PECs) in breast milk. Workshop participants were selected based on their broad expertise in key scientific disciplines (e.g., toxicology, risk assessment, epidemiology, physiologically-based pharmacokinetic (PBPK) modeling, public health), as well as their specific expertise with this class of chemicals. The topics discussed at the workshop are reviewed here, with emphasis on potential methods for improving the risk assessment of PECs in breast milk, along with the data gaps, uncertainties and other issues identified, and the suggested solutions. Methods were proposed for use in human exposure assessment and to extrapolate data from animal studies for use in human dose-response assessment. The goal was to identify approaches that can be adapted for application to any persistent and bioaccumulative chemical, whether it be a legacy PEC (e.g. hexachlorobenzene (HCB)), another known chemical, or a chemical that may emerge in the future. A complete summary of the workshop proceedings is available (ICF International, 2013).
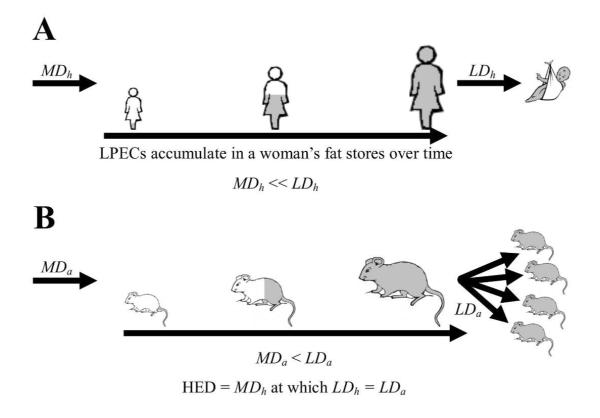
Many PECs are highly lipophilic, including those commonly known as persistent organic pollutants (POPs) and many of those identified by the U.S. Environmental Protection Agency as persistent, bioaccumulative and toxic (PBT) chemicals (U.S. EPA, 2013). In humans and other animals, lipophilic PECs (LPECs) are stored in body lipids where they have long elimination half-lives. Due to their slow rate of elimination, these chemicals have the potential to accumulate within a woman’s lipids over the course of many years prior to pregnancy and child birth. LPECs partition from body lipids into breast milk because of its high lipid content; consequently, breast milk produced by exposed women may have a significant burden of LPECs, and breastfed infants may be exposed to these chemicals. Moreover, these exposures may occur at higher levels and over a shorter time period compared to maternal exposure, which occurs over the long-term prior to and during pregnancy and lactation (Figure 1A). In addition, because of the relatively small size of a nursing infant, this high exposure may lead to LPEC levels in blood and tissues that far exceed those in the mother.
Figure 1.
LPEC accumulation in maternal body lipids and partitioning into milk (A) in humans, and (B) in laboratory animals. Because LPECs (represented by gray shading) accumulate within maternal body lipids over time, offspring lactational doses of these chemicals (LDh and LDa) may be much greater than average daily maternal doses (MDh and MDa). This is particularly true in humans, and offspring lactational dose in an animal study (LDa) may be very different compared to infant lactational dose in humans (LDh), even when the average daily maternal dose in animals (MDa) is equal to that in humans (MDh). The human equivalent dose (HED) can be used to apply dose-response data from toxicological studies in animals to human dose-response assessment.
Breastfeeding occurs during an important developmental period when organ and hormonal systems are being generated or acquiring function in the newborn. Human development occurs during the prenatal period, infancy, adolescence and even later (e.g. the nervous system continues to develop throughout childhood and into early adulthood) (Adams et al., 2000; Makris et al., 2008). Throughout development, critical windows of exposure (i.e. developmental periods of vulnerability during which adverse effects may be triggered by exposures to environmental agents or other stressors) vary for different endpoints, depending on the duration or timing of the programmed developmental process, and may also differ in their relative sensitivity. Further, for many endpoints, these critical windows of exposure have not been delineated.
For endpoints with very wide or undefined critical windows of exposure, it is important to consider the potential impacts of exposure at all lifestages when the relevant developmental process might occur (Cohen Hubal, Moya, and Selevan, 2008). Thus, postnatal exposures to LPECs, especially during potentially sensitive lifestages such as infancy, are important to evaluate. The tendency for these chemicals to persist and accumulate in body lipids and to partition into breast milk presents unique challenges for risk assessment. These challenges are briefly outlined below for each component of the risk assessment process, including hazard identification, dose-response assessment and exposure assessment.
Comprehensive hazard identification requires the investigation of a wide variety of potential health effects that might occur as a result of chemical exposure. There is a rich literature demonstrating that children are exposed to LPECs during infancy via breastfeeding (LaKind, Amina Wilkins, and Berlin, 2004; Landrigan et al., 2002; Lloyd-Smith and Sheffield-Brotherton, 2008; Needham, Barr, and Calafat, 2005); however, many human studies have also reported beneficial effects of breastfeeding relative to formula-feeding despite this exposure (Mead, 2008). In order to identify hazards posed by exposure to these chemicals in breastfed infants, toxicological endpoints relevant to that time period of exposure should be compared across populations of breastfed infants with varying levels of exposure (Makris et al., 2008). However, relatively few studies have addressed whether infancy encompasses a window during which LPEC exposure triggers developmental effects. Furthermore, for many toxicological endpoints, critical windows of exposure have not been delineated; the potential impacts of early life exposure to environmental chemicals on these endpoints are not clear. Thus, identification of hazards to health or development associated with early life exposure to most LPECs is limited by a paucity of data.
Challenges to dose-response and human exposure assessment for infants arise from the accumulation of LPECs in body lipids of women prior to pregnancy and their subsequent partitioning into breast milk and ingestion by infants (Figure 1A). As noted above, a human infant’s exposure to LPECs through ingestion of breast milk (hereafter, “infant (or offspring) lactational dose”) may be substantially greater than the average daily exposure of his/her mother from contact with these chemicals in environmental media (hereafter “average daily maternal exposure”). Although many studies have reported LPEC concentrations in human milk (LaKind, Amina Wilkins, and Berlin, 2004), dose-response and human exposure assessments presently conducted for these chemicals often do not account for the nature or magnitude of the differences between infant lactational dose and average daily maternal exposure. This particularly holds when (1) the dose-response assessment for toxicological endpoints relies on data derived from animal studies, or (2) the human exposure assessment relies on measures of LPEC concentrations in environmental media. These situations are further outlined and delineated as follows:
- Several specific differences between humans and laboratory animals are important to consider when using experimental animal data for a dose-response assessment of developmental endpoints that could result from early life exposure to LPECs:
- Differences in elimination half-life. A LPEC’s elimination half-life in humans may be dramatically longer than it is in laboratory animals (Matthews and Dedrick, 1984; Poiger and Schlatter, 1986). For example, the half-life of HCB was estimated to be 6 years in humans (To-Figueras et al., 2000) and 80 days in rats (Yesair et al., 1986).
- Differences in exposure duration. LPECs may accumulate in a female’s lipids throughout the period of time prior to pregnancy. Many reproductive and developmental toxicity studies in animals expose females to these chemicals for only a relatively short time (e.g. days or weeks) before and/or during gestation and/or lactation. In humans, this period spans decades and may include important changes in diet (especially across life stages) and historical exposure levels.
- Differences in distribution to offspring. Humans most often give birth to singletons while most laboratory animal species bear young in litters. As a result, in humans, the lactational dose is delivered to one infant while, in animals, it is divided among offspring. Differences in milk yield and suckling rates for a single human infant, versus all young in a litter, may affect both the relative rates at which human mothers and animal dams eliminate LPECs via lactation and the relative rates at which human infants and animal offspring are exposed via this route (Arcus-Arth, Krowech, and Zeise, 2005; Fiorotto et al., 1991).
As a result of these and other interspecies differences (e.g. differences in absorption and metabolism), lactational exposure to a LPEC in an animal study may be very different compared to lactational exposure for a human infant, even when the animal dam and the human mother are exposed to the same chemical at the same average daily dose, and even if maternal body burdens are comparable between the two species (Figure 1). In assessing the developmental effects of these chemicals that occur in offspring, it is the dose of the chemical to the offspring that is the most important for dose-response assessment. Yet, most studies report doses administered to animal dams and not the lactational doses ingested by their offspring. Thus, when animal data are used in the dose-response assessment of developmental endpoints resulting from lactational exposure to LPECs, methods are needed to determine (1) the offspring lactational dose achieved in an animal study, and (2) the average daily maternal exposure in humans that would deliver an infant lactational dose in humans of the same magnitude as the offspring lactational dose achieved in the animal study. The method employed to estimate these respective doses may vary depending on how much information is known about a given LPEC with regard to its toxicokinetic profile in humans and laboratory animals.
- (2) Several considerations are important when conducting an exposure assessment for LPECs in breastfed human infants:
- Lack of data. Data for LPEC content of breast milk are often unavailable. As a result, it may not be possible to estimate exposure based on the concentration of the chemical of interest in breast milk.
- Unique exposure conditions. Available data to support exposure assessment often consist of chemical concentrations in environmental media (e.g. food, water, soil, air), which are combined with data on the intake or contact rate of a population with one or more of these media to estimate the chemical exposure level of particular groups within the population (e.g. adult men, adult women, children of various ages). However, compared to other groups, breastfed infants are relatively sheltered from some environmental media (e.g. food, ingested water) while being uniquely exposed to breast milk (Cohen Hubal, Moya, and Selevan, 2008).
- Differences between maternal and breastfed infant exposures. As discussed above, LPEC concentrations in breast milk may produce infant lactational doses that are higher than the average daily maternal exposures encountered from contact with environmental media (Figure 1A).
Given these considerations, in order to use environmental sampling data to estimate LPEC exposure in breastfed human infants, methods are needed to determine the relationship between the infant and maternal doses of exposure.
In light of the challenges outlined above, the main objectives of this review are (1) to describe the types of data needed to best support the identification of hazards related to early life exposure to LPECs, and (2) to illustrate innovative approaches that may be used to support dose-response and exposure assessment of LPECs in breast milk, including methods to quantify differences between offspring lactational dose and average daily maternal exposure.
Strategies to support hazard identification
To better understand the relative importance of LPEC exposures at different lifestages, there is a need to delineate the periods during which infants are more vulnerable to chemical insults, commonly referred to as “critical windows of exposure”. This can be achieved in both experimental and epidemiologic settings where dose-response relationships are characterized for different periods of exposure. In studies of human exposure to LPECs, it can be difficult to determine whether a developmental effect resulted from prenatal exposure, postnatal exposure or both. Toxicokinetic models can be used to estimate internal dosimetry of the breastfed infant using information on (1) lipid-adjusted concentration of a chemical in maternal blood, cord blood or breast milk samples and (2) maternal and infant physiology (i.e. infant sex, maternal age at pregnancy, duration of breastfeeding, weight and height of both infant and mother). Resulting internal concentration vs. time profiles can be used in epidemiological studies to identify critical windows of exposure in humans by assessing the associations that may exist between effects and exposures at different time periods. For example, to identify critical windows of exposure during which polychlorinated biphenyls (PCBs) may impair human infant attention and activity level (assessed at 11 months of age by video coding of infants’ behavior during the administration of the Bayley Scales of Infant Development), Verner et al. (2010) used a PBPK model for PCB 153 in humans. The model was used to simulate infant blood PCB 153 levels at delivery and on a month-by-month basis during the first year of life. The association between inattention and estimated infant blood PCB 153 level was greatest (larger standardized beta in multivariable regression models) and only statistically significant at delivery, suggesting that prenatal exposure has the strongest effect on this neurobehavioral domain. On the other hand, non-elicited activity duration, another neurobehavioral domain, was only significantly associated with postnatal exposure estimates: the strongest association was with the estimated level of PCB 153 in infant blood at approximately 4 months of age. Whether these associations are attributable exclusively to either prenatal or postnatal exposures remains unclear as regression models were not adjusted for exposures during other time windows (i.e. regression models of prenatal exposure were not controlled for postnatal exposure and vice versa).
Information on critical windows of exposure may also come from studies in laboratory animals. A cross-fostering study design can be used to isolate prenatal and postnatal exposures, or chemicals may be administered directly to neonatal animals to identify effects of postnatal exposure (Holladay and Smialowicz, 2000; Makris et al., 2008). Critical windows of exposure may be different between humans and laboratory animals (Makris et al., 2008). Rodents are more immature at and soon after birth than humans (National Research Council, 1993); effects triggered by postnatal exposure in some animal species may be induced by prenatal exposure in humans (Selevan, Kimmel, and Mendola, 2000). Also, in an animal such as a rat, a critical window of exposure may be a few days long while the same window in humans may last for weeks or months. Although some information relating critical windows in different species exists, more information is needed to fully understand the similarities and differences in windows of exposure that affect developmental processes in humans and laboratory animal species.
The toxicological endpoints that are sensitive to LPEC exposure during infancy need to be identified. As described above, neurodevelopment occurs over a very prolonged period in humans, and there are different components of neurological function that develop prenatally and postnatally (Adams et al., 2000). Other biological systems, including the immune, respiratory, reproductive and endocrine systems, also continue to develop postnatally in humans and are susceptible to disruption by postnatal exposure to environmental chemicals (Makris et al., 2008; National Research Council, 1993).
Strategies to support dose-response and exposure assessment
A full spectrum of modeling approaches is available to support dose-response and exposure assessment for lactational exposures to LPECs. Methods have been developed (1) to quantify differences between offspring lactational dose and average daily maternal exposure in humans and laboratory animals, and (2) to facilitate the use of data from animal studies in human dose response assessment (Figure 1). Specific examples of some of the methods are provided using data for HCB. HCB was chosen as the exemplar because (1) its toxicokinetic behavior is relatively well-understood, (2) its metabolism in both humans and laboratory animals is limited, and (3) it exists in the environment as a single chemical. As discussed later, additional considerations are necessary if these modeling approaches are to be applied in risk assessment of LPECs that are well metabolized or that exist as mixtures (e.g. chlordane, PCBs).
Mathematical modeling approaches
PBPK approaches may offer significant advantages over simpler modeling approaches for estimating offspring exposure to LPECs in humans or laboratory animals. Primary reasons for using PBPK models to develop offspring exposure estimates for these chemicals include the ability to account for ongoing exposure, fat (and chemical) deposition in the mother before and during gestation, postpartum fat (and chemical) mobilization in the mother (e.g. Redding et al., 2008), and dose-dependent variations in chemical metabolism or half life.
However, as noted by Verner et al. (2013), an existing PBPK model may be complex yet not adequately flexible to consider key information to address the question at hand. To assess infant exposure through consumption of breast milk, a model should accurately simulate germane data such as maternal and infant blood levels and breast milk levels. PBPK models that explicitly estimate infant lactational doses in humans are currently available for only a few of the many chemicals found in human milk [e.g. PCB 153 (Redding et al., 2008), perchlorate (Clewell and Gearhart, 2002), dioxin (Lorber and Phillips, 2002), perfluorooctanoic acid (PFOA) and perfluorooctane sulfonate (PFOS) (Loccisano et al., 2013), manganese (Yoon et al., 2011), methylmercury (Byczkowski and Lipscomb, 2001), organic solvents (Fisher et al., 1997), and moxidectin (Korth-Bradley et al., 2011)]. When an appropriate chemical-specific PBPK model is not available, more general models developed by Verner et al. (2009; 2013) for LPECs that distribute according to lipid solubility and have elimination half-lives in humans on the order of years may be considered. An important advantage of the models developed by Verner et al. is that the chemical-specific parameters can be estimated using only the elimination half-life (Verner et al., 2013) or both the elimination half-life and the octanol-water partition coefficient (Kow) of the compound (Verner et al., 2009).
The maternal and infant PBPK model presented in Verner et al. (2009) is intended to simulate the entire life-cycle of a woman up to age 55 years and includes nine maternal tissue compartments and five infant tissue compartments. The oral maternal dose of a LPEC is modeled as being directly absorbed into the liver and is assumed to be fully bioavailable. First-order hepatic metabolism is included and assumed to represent all excretion in the absence of breastfeeding or childbirth. The elimination rate constant is derived for the chemical from the adult whole-body half-life. Chemical concentrations in each compartment are determined using partition coefficients, where estimates of the chemical-specific partition coefficients are based on Kow. Physiological parameters (e.g. body weight and adiposity) are assumed to vary across time to capture changes over the life of a woman. The average daily maternal exposure to a particular chemical can be estimated by modeling its concentration in mother’s blood, assuming constant daily dosing from birth. In turn, the chemical concentration in milk can be estimated based on a milk:blood partition coefficient. The infant lactational dose can be derived using estimates of infant daily milk intake.
In a less complex approach, the multi-compartment PBPK model is reduced to the consideration of only two-compartments representing the mass of maternal and fetal/child body lipids as a function of age (Verner et al., 2013). A conceptual representation of the two-compartment model is provided in Figure 2. The infant lactational dose estimation is based on the lipid-adjusted chemical concentration in milk, infant daily milk intake and milk lipid content (Arcus-Arth, Krowech, and Zeise, 2005). Both the multi- and two-compartment models have been validated for multiple LPECs (HCB, p,p’-dichlorodiphenyldichloroethylene (p,p’-DDE), p,p’-dichlorodiphenyltrichloroethane (DDT), β-hexachlorocyclohexane (β-HCH), PCB 118, PCB 138, PCB 153, PCB 170 and PCB 180) (Verner et al., 2009; Verner et al., 2013). When each model was evaluated using the same data, they yielded similar results. These models may be very useful for estimating human infant lactational doses for a wide variety of LPECs.
Figure 2.
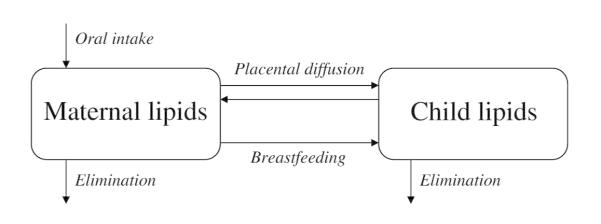
Conceptual representation of the Verner et al. (2013) two-compartment model reproduced with permission from Environmental Health Perspectives.
To illustrate the use of a model such as the one described by Verner et al. (2013) to estimate a human infant lactational dose from an average daily maternal exposure, data for HCB were employed to execute the model. The model parameter values for humans used for this example chemical are given in Table 1. Details on the model equations employed are presented as supplemental material to Verner et al. (2013). Using this model and assuming an average daily maternal exposure of 1 ng HCB/kg body weight (bw)-day in humans, an average infant lactational dose of 28 ng HCB/kg bw-day is estimated over a 12-month nursing duration. The analyses in this review assume a breastfeeding duration of 12 months in humans because both the American Academy of Pediatrics (AAP) and the World Health Organization (WHO) recommend exclusive breastfeeding until 6 months of age and continued breastfeeding for 12 months or longer (AAP, 2012; WHO, 2003). The resulting estimate of average infant lactational dose can be used to support an exposure assessment for lactational exposure to HCB when available data allow for an estimation of average daily maternal exposure but do not include values for the chemical concentration in breast milk.
Table 1.
Model parameters used in model simulations for HCB in humans (Verner et al., 2013)
| Model parameter (units) | Parameter value |
Reference |
|---|---|---|
| Maternal age at delivery (years) | 25 | Martin et al. (2012) |
| Pre-pregnancy weight (kg) | 74.7 | McDowell et al. (2008) |
| Gestational weight gain (kg) | 14.3 | Oken et al. (2008) |
| Postpartum weight (6 mo after delivery) (kg) |
79.7 | Baker et al. (2008) |
| Postpartum weight (18 mo after delivery) (kg) |
77.3 | Baker et al. (2008) |
| Gestational age (weeks) | 39 | Assumption |
| Child weight at birth (kg) | 3.4 | Kuczmarski et al. (2002) |
| Child weight at 6 months of age (kg) | 7.2 | Kuczmarski et al. (2002) |
| Child weight at 12 months of age (kg) | 9.6 | Kuczmarski et al. (2002) |
| Child gender | Female | Assumption |
| HCB half-life (years) | 6 | To-Figueras et al. (2000) |
Importantly, both models developed by Verner et al. (2009; 2013) assume that a chemical essentially distributes in neutral lipids only. Although the assumption of homogeneous distribution of LPECs into neutral lipids is a simplification of a more complex partitioning into the different components of blood and tissues (Parham et al., 1997), the models were shown to generate accurate predictions of children’s blood levels in validation studies. However, if there are data to suggest that a particular chemical may partition into other lipid or aqueous compartments, then another complex multi compartment model that can accommodate this information may be useful. In addition, if distribution mechanisms such as protein or phospholipid binding are implicated and may significantly affect the overall kinetics of a chemical, then other models will need to be developed to accommodate these processes.
Simple no-elimination modeling approach
The implementation of the models discussed above requires that the elimination half-life be known for the chemical of interest. For chemicals for which there are no reliable half-life data, a very simple approach based on a method presented by Rogan and Ragan (1994) may provide a first approximation or worst-case scenario that could be considered until these data are available. This approach, referred to in this document as the “simple no-elimination model”, is based on the conservative, default assumption that lactation is the only LPEC elimination route for mothers. Examples of factors that are considered in this model include the average daily maternal LPEC exposure, age at parturition, and infant daily milk intake.
Assuming an average daily maternal exposure of 1 ng HCB/kg bw-day and a 12-month nursing duration, an average infant lactational dose of 77 ng/kg bw-day is estimated using this approach. This estimate is reached through the following steps. First, maternal body burden at the time of parturition (assumed to be at 25 years of age (Martin et al., 2012)) is calculated:
| (1) |
Where:
| BBMAT | = the maternal body burden (mg/kg bw); |
| ADDMAT | = the average daily maternal dose in mg/kg bw-day (1 ng/kg bw-day = 0.000001 mg/kg bw-day); and |
| AgeMAT | = the mother’s age at parturition in days (25 years = 9125 days). |
Then, the lipid-adjusted chemical concentration in milk is calculated:
| (2) |
Where:
| Cmilk fat | = the chemical concentration in milk fat (mg/kg milk fat); |
| BBMAT | = the maternal body burden (mg/kg bw); and |
| ffm | = the fraction of the mother’s weight that is fat (assumed to be 0.4 kg fat/kg bw (Borrud et al., 2010)). |
And finally, the average infant lactational dose is calculated:
| (3) |
Where:
| ADDINF | = the average infant lactational dose of a LPEC (mg/kg bw-day); |
| Cmilk fat | = the chemical concentration in milk fat (mg/kg milk fat); |
| CRmilk | = the average infant ingestion rate of milk (assumed to be 0.66 kg/day (U.S. EPA, 2011)); |
| ffbm | = the fraction of fat in milk (assumed to be 0.04 (U.S. EPA, 2011)); and |
| BWINF | = the average infant’s body weight (assumed to be 7.8 kg (U.S. EPA, 2011)). |
Monte Carlo methods to account for natural variability
The parameters used in the modeling approaches outlined above consist of point estimates for the various measures. Typically, the exposure level and the values for certain physiological characteristics vary across a population group and with time. The parameter values associated with the models described above may vary significantly across human population groups. Some that may impact the determination of the infant lactational dose include average daily maternal exposure, body weight (maternal and infant), age at pregnancy, maternal adiposity, milk lipid content, infant milk intake, duration of lactation, parity of the mother, duration of previous breastfeeding episode(s), and years since previous breastfeeding.
For parameters for which there are a range of values or estimates, average values are often used in modeling approaches as shown in the example approaches described above. However, when a parameter varies across a wide range, the model output using an average value may differ significantly from that using a 5th or 95th percentile value. It is necessary and important to account for the variability of a parameter and to assess the impact that this variability may have on model output and results in order to identify population groups most susceptible to lactational LPEC exposure. To this end, stochastic modeling methods may be used to address concerns regarding variability in model parameters.
Population-based projections of an exposure distribution can be generated using Monte Carlo methods (Bogen et al., 2009). To perform this type of analysis, the distribution of a parameter must be developed to replace the simple point estimate values for all parameters that are expected to vary widely across the population, or to significantly affect the estimation of exposure, or both. This information allows the model to be run for numerous iterations, where the model generates a different estimate at each iteration. In this case of factors associated with the average daily maternal exposure, the iterations will be for offspring lactational dose. In general, to execute an iteration, each model input is assigned a value sampled from its observed distribution in the population. Then, the combination of inputs is used by the model to estimate the offspring lactational dose. The overall outcome of the model analysis is a set of model predictions comprised of the results of the different iterations. When taken together for the specific case described here, they give an indication of the likely distribution of lactational exposure in offspring across the population.
Using data associated with HCB, the model put forth by Verner et al. (2013) was used to perform a simple Monte Carlo analysis as an example of a calculation of a human infant lactational dose for HCB using parameter distributions. The following parameters were all varied in the model using distributions for each one (Table 2): maternal age at delivery; pre-pregnancy body weight; gestational weight gain; postpartum weight retention 6 months after delivery; postpartum weight retention 18 months after delivery; HCB elimination half-life; maternal lipids; infant milk intake; lipids in breast milk; infant sex; gestational age; infant body weight; and infant lipids. Because LPECs may be eliminated during lactation, doses to the first breastfed child are expected to be higher than those to subsequent children, although data indicate that this cannot be assumed for every member of this chemical class (LaKind et al., 2009). Nonetheless, if maternal exposure is limited to a level posing minimal risk to the first child, later children may also be protected. For this reason, this analysis assumes a parity of 1.
Table 2.
Parameter distributions used in Monte Carlo simulation for HCB in humans
| Model parameter (units) | Distribution | Mean parameter value |
Standard deviation |
Range | Reference |
|---|---|---|---|---|---|
| Maternal age at delivery (years)* | Normal | 25 | 6 | 15 - 54 | Martin et al. (2012) |
| Pre-pregnancy weight (kg) | Normal | 74.7 | 17.8† | 50 – 114 | McDowell et al. (2008) |
| Gestational weight gain (kg) | Normal | 14.3 | 5.1 | 0 - 45.4 | Oken et al. (2008) |
| Postpartum weight retention 6 mo after delivery (kg per kg of gestational weight gain) |
Uniform | 0.30 - 0.40 | Baker et al. (2008) | ||
| Postpartum weight retention 18 mo after delivery (kg per kg of gestational weight gain) |
Uniform | 0.16 - 0.21 | Baker et al. (2008) | ||
| HCB half-life (years)‡ | Normal | 6 | 0.9 | 4.2 - 7.8 | To-Figueras et al. (2000) |
| Maternal lipids¶ | Normal | 1.0 | 0.21† | 0.58 - 1.42 | Borrud et al. (2010) |
| Volume of breast milk¶ | Normal | 1.0 | 0.17 | 0.66 - 1.34 | Arcus-Arth et al. (2005) |
| Lipids in breast milk¶ | Normal | 1.0 | 0.28 | 0.48 - 1.52 | Arcus-Arth et al. (2005) |
| Child sex | Bernouilli (p=0.5) | Assumed | |||
| Gestational age (weeks) | Normal | 39 | 2 | 35-43 | Assumed |
| Child weight¶ | Normal | 1.0 | 0.12 | 0.76 - 1.24 | Kuczmarski et al. (2002) |
| Child lipids¶ | Normal | 1.0 | 0.15 | 0.70 - 1.30 | Enzi et al. (1981), Butte et al. (2000) |
Martin et al. (2012) reported the percentage of pregnant women across different age ranges as of 2002: 3.0%, 6.6%, 51.5%, 36.2%, and 2.6% were ages 15-17, 18-19, 20-29, 30-39, and 40-54 years, respectively. These proportions were used to estimate the best-fitting normal distribution; a distribution with a mean age of 25 years and a standard deviation of 6 years was selected.
Standard deviation calculated from the interquartile range (SD = 0.74*IQR).
The SD was calculated assuming a coefficient of variation of 0.15 and the range was set to ± 2 SD.
Parameters that fluctuate within individual simulations were varied using a multiplier with a distribution centered around 1.0, a standard deviation equal to the coefficient of variation and a range of ± 2 SD.
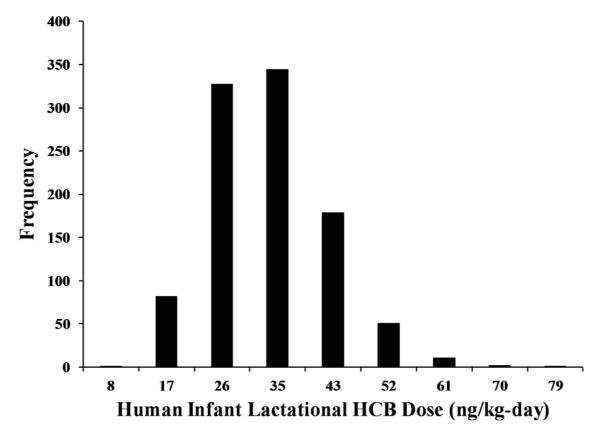
A hypothetical average daily maternal exposure of 1 ng/kg bw-day was assumed. The estimated probability density function for the human infant lactational dose based on this maternal exposure level is shown in Figure 3. This distribution is estimated by taking the prediction of the human infant lactational dose for 1000 iterations and finding the proportions that fall within different dose ranges. For the input distributions assumed in this example, the resulting distribution is slightly skewed, with a mean of 29 ng/kg bw-day and a 95th percentile of 45 ng/kg bw-day.
Figure 3.
Results from Monte Carlo simulation to calculate human infant lactational dose assuming an average daily maternal exposure of 1 ng/kg bw-day HCB.
Similar analyses could be conducted for other LPECs using the model by Verner et al. (2013), which was developed for chemicals with a log Kow greater than 4. The only chemical-specific parameter that is included in the model is the half-life of elimination, so this model could be used to run Monte Carlo simulations for any LPEC for which the half life is known. In a validation study, the model accurately predicted children’s levels of multiple LPECs (PCB 118, 138, 153, 180, DDE, DDT, HCB) although accuracy was slightly lower for compounds with shorter half-lives. The model should accommodate any LPEC with a half life within the range of half-lives for which it was evaluated (5 to 15 years).
It is possible that the effects and/or dose response of a LPEC are different across subgroups of the population (i.e. the potential impact of exposure at a given level may differ across population groups). For example, certain individuals may be more sensitive to p,p’-DDT exposure because glutathione S-transferase polymorphisms may modulate how p,p’-DDT affects neurodevelopment (Morales et al., 2008). The most effective way to address interindividual variability in sensitivity or susceptibility is to gather toxicological dose-response data in the sensitive or susceptible population of interest or in an animal model of that population.
Toxicokinetic modeling approach for offspring lactational dose estimation in laboratory animals
The models discussed above may be used to support human exposure assessment for lactational exposure to LPECs or dose-response assessment when human dose-response data are available. Another approach can be used to determine an offspring lactational dose of a LPEC in laboratory animals. When health effects are observed in laboratory animal offspring following lactational exposure to a LPEC, estimates of offspring lactational dose can be used to support dose response assessment for those effects. This includes estimation of a human equivalent dose (HED), which represents the average daily maternal exposure to a LPEC in humans expected to deliver a human infant lactational dose of the same magnitude as the offspring lactational dose achieved in an animal study (Figure 1). A toxicokinetic model based on equations presented in U.S. EPA’s Methodology for assessing health risks associated with multiple pathways of exposure to combustor emissions (U.S. EPA, 1998) can be used to estimate offspring lactational dose in laboratory animals when a chemical-specific PBPK model is not available. As with the human modeling approaches described above, this animal toxicokinetic model is based on “body burden” or the total average concentration of chemical in the body. It allows the maternal dose, the offspring body weight, and the milk ingestion rate to vary over time by using different point estimates for each measure over the course of the simulation. It also allows for an observation period after dosing ends. This is particularly important for application to laboratory animals since the exact dosing protocol (e.g. dosing only on particular gestation days) can be reproduced in the model. Varying offspring body weight and milk ingestion rate allows the model to better approximate the chemical exposures of offspring during the neonatal period when these parameters are changing rapidly. LPEC elimination from the body is represented as a rate constant multiplied by the total body burden. This rate constant is estimated from the whole-body elimination half-life of the LPEC in the relevant laboratory animal species. The body burden is based on the chemical dose normalized by the total body weight. Thus, the toxicokinetic animal model can be represented by the following differential equation:
| (4) |
Where:
| BB(t) | = | the time-dependent total body burden of the maternal animal (mg/kg); |
| fam | = | the fraction of ingested chemical absorbed by the maternal animal (dimensionless); |
| DImat(t) | = | the time-dependent dose administered to the maternal animal (mg/kg bw-day); and |
| kelim | = | the first order elimination rate (days−1) = ln(2)/half-life (days). |
The differential equation can be converted to a difference equation and iterated in time as follows:
| (5) |
Where:
| BBt+Δt | = | the total body burden of the maternal animal at the current time step (mg/kg); |
| BBt | = | the total body burden of the maternal animal at the previous time step (mg/kg); |
| Δt | = | the time step (days); and |
| DImat,t | = | the dose administered to the maternal animal at the current time step (mg/kg bw-day). |
This equation allows maternal body burden in laboratory animals to be estimated; additional equations can be used to estimate animal offspring lactational dose and body burden. First, the chemical concentration in milk fat is assumed to be equal to the concentration in maternal lipid and can be estimated as:
| (6) |
Where:
| Cmilk fat, t | = | the concentration of chemical in milk fat at the current time step (mg/kg milk fat); |
| ff | = | the fraction of chemical stored in the fat of the maternal animal (dimensionless); and |
| ffm | = | the fraction of the maternal animal’s weight that is fat (kg fat/kg bw). |
To account for maternal elimination of the chemical via lactation, the elimination rate during lactation is increased:
| (7) |
Where:
| kelac | = the elimination rate in the maternal animal during lactation (days−1); |
| CRmilk ,t | = the time-dependent rate at which offspring ingest milk (kg/day); |
| fmbm | = the fraction of fat in milk (dimensionless); |
| LS | = litter size; and |
| BWmat | = body weight of the maternal animal (kg). |
Then, offspring lactational dose can be estimated as:
| (8) |
Where:
| DIINF,t | = | the time-dependent offspring lactational dose (mg/kg bw-day); and |
| BWINF,t | = | the time-dependent offspring body weight (kg). |
Finally, offspring body burden resulting from ingestion of milk can be estimated as:
| (9) |
Where:
| BBINF,t+Δt | = | the total offspring body burden at the current time step (mg/kg); |
| BBINF,t | = | the total offspring body burden at the previous time step (mg/kg); and |
| fai | = | the fraction of ingested chemical absorbed by offspring (dimensionless). |
To illustrate how this toxicokinetic animal model might support the estimation of a HED for use in dose-response assessment for humans, the model was implemented in a hypothetical case in which 1 mg/kg bw-day HCB was administered to rat dams from the time of mating until weaning of the pups. Parameter values used for this example are given in Table 3. A gestation time of 3 weeks and lactation duration of 3 weeks were assumed as representative of typical values in rats (U.S. EPA, 2002). To incorporate offspring gestational exposure (in addition to lactational exposure), offspring body burden at parturition can be incorporated by using an initial condition for BBINF,t. For the purposes of this example, at birth, the offspring body burden was assumed to equal the maternal body burden. Using the model, the offspring HCB body burden averaged over the lactation period was estimated to be 54 mg/kg. Next, to determine the HED for HCB, this animal body burden value was then used with the two-compartment model developed by Verner et al. (2013) to calculate an average daily maternal exposure in humans that might be expected to result in the same average HCB body burden in a human infant who nursed for 12 months. Model equations and parameter values used in this calculation are located in Table 1 and in the supplemental material associated with Verner et al. (2013). The resulting average daily maternal HED was 0.0118 mg/kg bw-day. This type of HED could be used to support a dose-response assessment for lactational exposure to LPECs as it allows for dose-response data from animal studies to be expressed in terms of human maternal exposure.
Table 3.
Model parameters used in model simulations 1 for HCB in rats
| Model parameter (units) |
Variable | Parameter value |
Comments |
|---|---|---|---|
| HCB dose administered to dam (mg/kg bw- day) |
DImat(t); DImat,t |
1 | Assumption |
| Time step (days) | Δt | 0.5 | Assumption To minimize uncertainty introduced by using an algebraic equation to solve a differential equation, Δt should be much smaller than t1/2. |
| Fraction of ingested HCB absorbed by the rat dam (dimensionless) |
fam | 0.8 | Koss and Koransky (1975) |
| HCB half-life in rats (days) |
t1/2 | 80 | Yesair et al. (1986) |
| First order elimination rate constant for HCB (day−1) |
kelim | 0.0087 |
If an offspring-specific t1/2 value is available, separate kelim values may be calculated for the dam and the pup (i.e. kelim and kelim,INF). For this example, t1/2 of HCB in the offspring is unknown, and only one kelim value was calculated using a t1/2 reported for HCB in adult female rats. Also for this example, kelim was used to describe maternal HCB elimination during 3 weeks of gestation but was replaced with kelac (defined below) for elimination during 3 weeks of lactation. |
| Dam HCB body burden (mg/kg) |
BB(t); BBt+Δt; BBt |
calculated |
BBt+Δt = BBt + Δt(famDImat,t − kelim × BBt) Iterated over time for 3 weeks of gestation and 3 weeks of lactation. BBt+Δt is body burden at the current time step, and BBt is body burden at the previous time step. BBt is assumed to be 0 at the first time step. |
| Fraction of HCB stored in maternal adipose tissue (dimensionless) |
ff | 0.9 | Assumption |
| Fraction of dam’s weight that is fat (kg fat/kg bw) |
ffm | 0.09 | Fisher et al. (1990) |
| HCB concentration in milk fat (mg/kg milk fat) |
Cmilk fat,t | calculated |
Iterated over time for 3 weeks of lactation |
| Litter size (number of pups) |
LS | 10 | Assumption |
| Pup ingestion rate, week 1 (kg milk/day) |
CRmilk,t | 0.0030 | Calculated from experimentally determined milk production values of 29.7, 54.3, and 59.1 g/rat/day measured on lactation days 2, 7, and 14, respectively, divided by 10 to get per pup ingestion rates (Knight, Docherty, and Peaker, 1984) |
| Pup ingestion rate, week 2 (kg milk/day) |
0.0054 | ||
| Pup ingestion rate, week 3 (kg milk/day) |
0.0059 | ||
| Fraction of fat in milk (dimensionless) |
fmbm | 0.15 | Welch and Findlay (1981) |
| Dam weight during lactation (kg) |
BWmat | 0.273 | Knight et al. (1984) |
| Elimination rate of HCB in dam during lactation (days−1) |
kelac | calculated |
Iterated over time for 3 weeks of lactation |
| Pup body weight, week 1 (kg) |
BWINF,t | 0.0066 | Knight et al. (1984) presented litter weights at different time points in a figure. This figure was digitized using the GetData Graph Digitizer (2008), and the values were divided by 10 pups per litter to get average pup body weights on lactation days 2, 7, and 14. |
| Pup body weight, week 2 (kg) |
0.014 | ||
| Pup body weight, week 3 (kg) |
0.028 | ||
| Offspring lactational HCB dose (mg/kg bw- day) |
DIINF,t | calculated |
Iterated over time for 3 weeks of lactation |
| Fraction of ingested HCB absorbed by the rat pup (dimensionless) |
fai | 0.8 | Assumption |
| Offspring HCB body burden (mg/kg) |
BBINF,t+δt; BBINF,t |
calculated |
BBINF,t+Δt = BBINF,t + Δt(faiDIINF,t − kelim,INF × BBINF,t) Iterated over time for 3 weeks of lactation. Iterations may be extended to include time after lactation, with appropriate adjustments to DIINF,t. DIINF,t = 0 after lactation unless exposure to offspring continues via an alternate (i.e. non-lactational) source. |
As shown in this example, using these modeling approaches to estimate a HED for a LPEC may reveal a substantial difference between humans and animals in the average daily maternal exposure required to produce a certain offspring lactational exposure. Even if the design of an animal study allows maximal accumulation of a chemical in maternal body lipids prior to lactation, the ratio between offspring lactational exposure and maternal exposure in that study may be far smaller than the ratio between infant lactational exposure and average daily maternal exposure in humans exposed to the same chemical. This difference arises from differences in elimination of LPECs between humans and animals and differences in the number of concurrent offspring. For example, the elimination half-life, a major factor influencing the accumulation of a LPEC in body lipids, may be much longer in humans than it is in animals (Matthews and Dedrick, 1984; Poiger and Schlatter, 1986), contributing to a greater LPEC accumulation in maternal body lipids and a greater lactational dose in humans. Additionally, rodents typically nurse litters of offspring, each of whom gets only a share of the total milk supply and any chemicals present in milk. Thus, the ratio between individual offspring lactational dose and maternal dose may be smaller than it is in humans, who commonly nurse only one infant. These knowledge gaps deserve further investigation for many LPECs.
Important factors to consider when implementing strategies to support risk assessment of LPECs in breast milk
Before and during the workshop, participants were asked to identify the presence and nature of gaps in data and parameter measures, potential issues, problems, complications and uncertainties related to conducting hazard identification, dose-response assessments, and exposure assessments of LPECs in breast milk. The factors identified can be grouped into seven general categories: model selection; choice of exposure metric; uncertainty in modeling data and parameters; reproductive and developmental study design; LPEC metabolism; exposure to chemical mixtures; and risk communication.
Model selection
Selection of modeling approaches for estimating the offspring lactational dose and the average daily maternal exposure depends on the LPEC under evaluation and the availability of data to inform parameter values for that chemical or similar chemicals. The most robust estimates will often result from using a model that includes as much physiological and chemical-specific information as possible. Of the approaches discussed here, PBPK modeling is the most robust approach. In some circumstances, PBPK modeling may be preferred over simpler models because it accounts for physiological differences and has the capability to extrapolate across doses, species, lifestages, and exposure scenarios. Thus, a PBPK model is most useful when extrapolations are required to describe different physiological or exposure groups. PBPK models may also be preferred for LPECs that are metabolized by humans and/or laboratory animals.
However, when applicable chemical-specific PBPK models are not available for a particular chemical for a species of interest, more general models may be appropriate for estimating human infant lactational doses for a variety of highly lipophilic chemicals that do not appreciably bind with proteins and are not soluble in aqueous compartments. An important advantage of this approach is that the chemical-specific parameters needed for the models can be estimated using only elimination half-life. For emerging chemicals and others for which limited data are available, a simple modeling approach may be applied that does not require that the elimination half-life be known (Rogan and Ragan, 1994). This very conservative approach incorporates for the chemical of focus a default assumption of no elimination from the body. In turn, it serves to establish a tentative relationship between average daily maternal exposure and the subsequent infant lactational dose that could be considered until chemical-specific information (i.e. elimination half-life) is available. Stochastic modeling techniques, including Monte Carlo methods, may be used with any of these approaches to better characterize interindividual variability within certain populations. When laboratory animal data are available, PBPK models specific to that species and chemical are useful for estimating offspring lactational doses. When a chemical-specific PBPK model is not available, the toxicokinetic model based on equations presented in U.S. EPA’s Methodology for assessing health risks associated with multiple pathways of exposure to combustor emissions (U.S. EPA, 1998) may be used. This model accommodates a wide variety of dosing protocols that might be utilized in animal studies. Each of the modeling approaches presented in this review have advantages and disadvantages for their use, and the selection of the most appropriate model for a given LPEC depends on factors like availability of data to inform modeling parameter values, tolerance for model uncertainty, available time and funding for conducting the analysis, and the application of the model(s) for the specific situation.
To illustrate the impact that model selection may have on infant lactational dose estimates, the results of various modeling approaches for the same chemical can be compared. For the example presented in this review, the two-compartment model published by Verner et al. (2013) was selected to simulate lactational exposure to HCB because this model’s validity has been thoroughly evaluated using blood levels measured in children from two longitudinal birth cohorts at ages 6 months, 16 months and 45 months. Simpler approaches presented herein (e.g. Rogan and Ragan, 1994) have not been evaluated against chemical levels measured in children. However, models by Verner et al. (2009; 2013) were compared with a variety of simpler approaches in ICF International (2013); the results of this comparison are summarized in Table 4. Assuming an average daily maternal exposure of 1 ng HCB/kg bw-day in humans, the average infant lactational dose estimations over a 12-month nursing duration ranged from 17 to 77 ng HCB/kg bw-day, with the highest estimate derived using the simple no-elimination modeling approach (Rogan and Ragan, 1994). Furthermore, the Oregon Department of Environmental Quality (2010) compared estimates of lactational exposure to PCB 153 using the PBPK models by Redding et al. (2008) and Verner et al. (2009) and equations presented in U.S. EPA (1998). Estimates from these three approaches were similar within a factor of 2. In general, the lowest estimates were derived using the model by Verner et al. (2009), and the highest were derived using equations from U.S. EPA (1998).
Table 4.
Comparison of mathematical modeling approaches to estimate infant 1 lactational dose in 2 humans (Adapted from ICF International (2013))
| Modeling approach | Infant nursing duration (months) |
Infant lactational dose (ng HCB/kg bw-day) corresponding to an average daily maternal exposure of 1 ng HCB/kg bw-day* |
|---|---|---|
| Multi-compartment model (Verner et al., 2009) |
1 | 26 |
| 12 | 21 | |
| Two-compartment model (Verner et al., 2013) |
1 | 34 |
| 12 | 32 | |
| Toxicokinetic model (ICF International, 2013) |
1 | 23 |
| 12 | 17 | |
| U.S. EPA model (U.S. EPA, 1998) |
1 | 29 |
| 12 | 23 | |
| No-elimination model (Rogan and Ragan, 1994) |
1 | 97 |
| 12 | 77 |
Infant lactational dose is averaged over the nursing duration.
Choice of exposure metric
Several exposure metrics might be useful for extrapolating doses from a laboratory animal study to human doses for a dose response assessment of infant lactational exposure. These include measures of average daily maternal exposure, maternal body burden, offspring lactational dose and offspring body burden. In the case of early life exposure that results in developmental effects, the dose-response relationship of interest is that between the health effect and the dose to the human or animal offspring. When using data from animal studies of LPEC exposure, dose extrapolation from animals to humans for the level of maternal exposure might be inadequate to account for differences in chemical exposures between animal offspring and human infants. Extrapolation from animals to humans in this context is complicated because animal dams and human mothers exposed to the same average daily dose of a LPEC may deliver different lactational doses to their respective offspring, even if resulting maternal body burdens are comparable between the two species. For this reason, it may be important to conduct an interspecies extrapolation for LPECs at the level of offspring lactational exposure as opposed to the level of maternal exposure.
Offspring exposure metrics that could be used for interspecies extrapolation include tissue dose, body burden and lactational dose. In the example HED calculation provided earlier in this review, the interspecies extrapolation was conducted using offspring body burden. The average offspring HCB body burden estimated for the animal study was assumed for a human infant, and this served as the starting point for the estimation of a corresponding average daily maternal exposure in humans. Offspring body burden may be estimated using modeling approaches, as in the example provided above. Or, for many LPECs, lipid-adjusted blood concentrations might be used as a surrogate measure of target tissue dose or offspring body burden. For highly lipophilic compounds, lipid-adjusted blood concentrations might be assumed to be similar to lipid-adjusted chemical concentrations in target tissues when the target tissue or dose to that tissue is not known (Haddad, Poulin, and Krishnan, 2000; Poulin and Haddad, 2012). However, there are some indications in the literature that some LPECs may distribute differently to different lipid compartments (LaKind et al., 2009) and that transport of such compounds in blood also involves lipoprotein low-affinity binding (Skalsky and Guthrie, 1978; Spindler-Vomachka, Vodicnik, and Lech, 1984) and binding to hemoglobin, proteins and phospholipids (Peyret, Poulin, and Krishnan, 2010). Also, modeling offspring body burden for use as the exposure metric for interspecies extrapolation may be complicated because body burden increases rapidly in neonates due to increased exposure with the onset of nursing, but also may decrease due to factors including growth-related chemical dilution and changes in metabolic enzyme expression (Hines, 2008; Hines and McCarver, 2002). Accurate estimation of offspring body burden over time requires knowledge of a chemical’s half-life in the juvenile. Chemical half-lives in juveniles may be quite different from half-lives in adults (Kerger et al., 2006; Kreuzer et al., 1997; Lorber and Phillips, 2002; Milbrath et al., 2009), and juvenile-specific half-lives are rarely available in the literature.
Another exposure metric that may be used for interspecies extrapolation is offspring lactational dose as calculated from LPEC concentrations in milk and estimates of offspring milk consumption. One advantage of using this metric is that juvenile-specific chemical half-lives are not required. Interspecies extrapolations based on lactational dose may result in higher HED estimations than those based on offspring body burden (ICF International, 2013). However, an extrapolation based on lactational dose does not account for gestational exposure, and interspecies scaling may be needed to account for pharmacokinetic differences between humans and animals (Thompson et al., 2008). Such scaling is not necessary if data are available to use target tissue dose or body burden as the exposure metric.
Please note that for all of these potential exposure metrics, there is an assumption that an average metric (e.g., offspring body burden or lactational dose averaged over the lactation period) is appropriate. While this may be a reasonable assumption, there is a need to evaluate the accuracy of this approach by identifying critical windows of exposure, as discussed above. If the critical window of exposure for a particular developmental effect is known, then the most appropriate metric would be the average exposure during the critical window rather than the average over the entire exposure duration.
Uncertainty in modeling data and parameters
As discussed above, mathematical modeling approaches are available to support dose-response and exposure assessment for lactational exposures to LPECs. Using accurate or representative parameters in these models is critically important for accurate results; but, limited data availability often produces uncertainty in parameter values such as for chemical absorption fractions, log Kow, elimination half-life, and tissue-specific partition coefficients. Importantly, when the results of a dose-response assessment are reported, the uncertainty in the overall assessment and in each of its parameters must be transparently acknowledged. For example, the model used above to estimate infant lactational dose (Verner et al., 2013) describes LPEC elimination based on published half-life values. Because there may be uncertainty in published estimates of half-life, sensitivity analyses can be performed to evaluate the influence of variations in this parameter. In the example above, assuming a half-life of 6 years for HCB (To-Figueras et al., 2000), an average daily maternal exposure of 1 ng HCB/kg bw-day was estimated to produce an infant lactational dose of 28 ng HCB/kg bw-day (95th percentile: 44). Using 0.5x and 2.0x the published 6-year half-life value, for the same average daily maternal exposure, the model predicts infant lactational doses of 17 ng/kg bw-day (95th percentile: 26) and 43 ng/kg bw-day (95th percentile: 68), respectively. These values provide a quantitative insight into the variability in exposure estimates given a certain degree of uncertainty. Verner et al. (2013) presents a global sensitivity analysis for additional model parameters, including prepregnancy body weight, maternal weight gain during pregnancy, postpartum maternal weight changes, infant gestational age, birth weight, infant weight at 6 months, and infant weight at 1 year.
Building upon previous efforts to optimize the collection and use of biomonitoring data in a similar context (Fenton et al., 2005; LaKind, Amina Wilkins, and Berlin, 2004), workshop participants identified several types of human biomonitoring data that may be particularly useful to reduce uncertainty in assessments of the toxicological risk from early life exposure to LPECs:
Maternal exposure data (e.g. dietary exposure) collected in the same populations in which chemical concentrations in breast milk are measured. These data serve to inform the relationship between average daily maternal exposure and infant lactational dose of the LPEC.
Lipid-adjusted PEC concentrations in breast milk, serum and adipose tissue samples from the same individuals. These data would be useful for understanding chemical distribution across various lipid compartments in the body. Ideally, these studies would also measure lipid-adjusted chemical concentrations in serum from breastfeeding infants born to those same women. This information could be used in a model to determine the infant lactational dose of a LPEC. Other biological samples that could be analyzed for LPEC content to inform and/or evaluate predictions of chemical kinetics in the infant include placenta, amniotic fluid, cord blood, meconium, infant blood and infant feces.
Lipid-adjusted PEC concentrations in serum taken from the same women over time that (1) include estimates of average daily exposure to the chemical from environmental media, and (2) control for changes in body weight. These data could be used to derive estimates of the elimination half-life in humans.
Reproductive and developmental study design
The design of reproductive and developmental studies in animals may be improved to better delineate the relative impacts of prenatal and postnatal exposure to LPECs on health effects observed in offspring. Current protocols for standard reproductive and developmental toxicity studies that typically expose dams to a chemical agent during the gestation period could be expanded to include additional endpoints and time periods. As discussed below, these expansions could reduce uncertainty when animal studies are used to support hazard identification and dose-response assessment for lactational exposures. For instance, in this context, it is important to investigate developmental endpoints that may be susceptible to disruption during the postnatal period in humans (Makris et al., 2008). These toxicological endpoints are not included in some current protocols for standard reproductive and developmental toxicity studies (e.g. the National Toxicology Program (NTP) reproductive assessment by continuous breeding (NTP, 2011)). Albeit, some developmental effects that occur in humans are difficult to evaluate in laboratory animal models, especially non-primate animals (e.g. effects on language development or IQ, some types of behavior and learning) (Adams et al., 2000). In these cases, human data from well-designed epidemiological studies are useful to support hazard identification and dose-response assessment. Furthermore, as discussed above, the identification of developmental hazards requires an understanding of the timing of critical windows of exposure, which remains unknown for many developmental endpoints. Critical windows of exposure in humans may be delineated by using modeling approaches together with data from epidemiological studies (Verner et al., 2010) while such windows can be identified in animals through the use of specific exposure protocols (Holladay and Smialowicz, 2000; Makris et al., 2008).
Protocols for some standard reproductive and developmental toxicity studies in animals could also be expanded to investigate the full impact of LPEC bioaccumulation on lactational dose by extending the duration of maternal exposure prior to pregnancy to allow for chemical accumulation in maternal lipids prior to lactation and to better reflect the typical exposure pattern occurring in humans. For example, test material is not administered until gestation day 6 in a NTP modified one generation study (NTP, 2011). Furthermore, the precision and applicability of modeling approaches to support dose-response assessment would be greatly enhanced if reproductive and developmental toxicity studies collected data on offspring exposure. Uncertainty related to the estimation of offspring exposure that is based on administered dose to the dam would be eliminated if lactational dose or internal dose to the offspring were measured in the same study in which a developmental effect of postnatal exposure to a LPEC was observed. The availability of offspring exposure data would greatly simplify the extrapolation of dose-response data from that study to a human exposure scenario. Similarly, if studies provided data on fetal exposure at a given maternal dose, this would facilitate the extrapolation of dose-response information for developmental endpoints that occur as a result of prenatal exposure.
It would also be useful to have time-course data on the tissue distribution of chemicals in toxicologically relevant animal species to inform modeling efforts (e.g. tissue-specific and whole-body elimination rates, partition coefficients). These studies might employ single or repeated dosing of dams followed by analysis of the chemical in a variety of tissues harvested from dams and offspring at various time points (e.g. milk, urine, feces, blood, fat, liver, target tissue). In particular, the comparison of human infant and nursing pup elimination rates over time is a critical factor in establishing relative body burdens. Much higher human infant than adult elimination rates for PCBs, dioxins and furans have been reported or modeled (Kerger et al., 2006; Kreuzer et al., 1997; Lorber and Phillips, 2002; Milbrath et al., 2009); however, there is a lack of data on rodent pup elimination rates for LPECs.
At present, the extended one-generation reproductive toxicity study developed by the Organisation for Economic Co-operation and Development may be the most comprehensive protocol available with regard to the considerations described above (OECD, 2011). This protocol includes (1) the assessment of potential impacts of chemical exposure on the developing nervous and immune systems, and (2) the administration of test material for a defined pre-mating period selected based on existing toxicokinetic information. The protocol also addresses other uses for toxicokinetic data in planning and interpreting the results of reproductive and developmental toxicity studies, including the estimation of internal dosimetry and development of concentration vs. time profiles.
LPEC metabolism
Metabolism has a profound effect on chemical kinetics. Because of this, there are additional considerations important when assessing LPECs that are metabolized. If a LPEC is readily converted to easily eliminated metabolites, then that chemical will be unlikely to accumulate in maternal fat stores, and infant lactational dose may not be higher than average daily maternal exposure. However, some LPECs are metabolized slowly or incompletely in humans, and some LPEC metabolites persist, accumulate in body lipids, and partition into breast milk (e.g. DDE).
Metabolism rates and pathways often differ substantially among animal species (Thompson et al., 2008). In order to use data from animal studies in human health risk assessment of metabolized chemicals, it is important to delineate the metabolic pathways of the chemical in all relevant species. Also, patterns of metabolic enzyme expression change over the course of development such that the metabolic pathway for a given chemical may differ in infants, children and adults (Hines, 2008). Thus, when assessing risk of developmental effects in young children, it may also be important to delineate metabolic pathways of the chemical at different lifestages. In addition to a qualitative understanding of the metabolic processes occurring in different species at different lifestages, it may also be useful to know metabolism rates and elimination half-lives for a parent compound and its metabolites in both humans and relevant laboratory animals. When the appropriate data on metabolic pathways and rates are available, PBPK models can be used to address metabolism and metabolic differences between species and lifestages (Thompson et al., 2008).
Metabolism may impact not only kinetics but also toxicity: the types of health effects caused by a metabolite may differ from those caused by its parent compound (Dekant, 2009). Because of the potential for these types of differences, when effects observed in an animal study are used to inform hazard identification for lactational exposures to metabolized LPECs, it is important to consider which chemical species (i.e. metabolite(s) and/or parent compound) may be responsible for the observed effects and to analyze whether and to what extent human infants might be exposed to those specific chemicals in breast milk.
Exposure to chemical mixtures
Metabolism of some LPECs creates a mixture of parent compound and metabolite(s) to which offspring may be exposed, and other LPECs exist as mixtures even in the absence of metabolism (e.g. chlordane, PCBs). Human mothers may be exposed simultaneously to multiple components of these mixtures as well as many other chemicals (persistent and non-persistent) in the environment (LaKind, Berlin, and Mattison, 2008). Human health risk assessment based on exposure to individual chemicals may underestimate risk when populations of interest are exposed to multiple chemicals with overlapping, additive or synergistic toxicities, but these other chemicals are not included in the risk assessment.
U.S. EPA’s Supplementary guidance for conducting health risk assessment of chemical mixtures (U.S. EPA, 2000) recommends several approaches to quantitative health risk assessment of a chemical mixture, depending upon the type of available data. In the ideal approach, toxicity data on the mixture of concern are available, and the quantitative risk assessment is done directly from these data. However, at this time, very limited toxicity data are currently available for the specific mixture(s) of LPECs found in human milk (e.g., Desaulniers et al., 2005). Thus, additional toxicological research along these lines is needed to apply the assessment approach preferred by U.S. EPA (2000) to postnatal developmental risk.
In the future, researchers might consider certain steps to facilitate a more comprehensive assessment of risk from early life exposures that would consider the entire mixture of LPECs found in human milk in place of the assessment of only one chemical at a time. The collection of biomonitoring data might allow for the determination of the composition of a “typical” breast milk LPEC mixture to which infants may be exposed. Other possible factors that may be necessary or useful to consider include differences in the content of the LPEC mixture found in breast milk that is representative of a national population in contrast to that of a specific geographical region (e.g. near pollution sources) or a particular lifestyle choice (e.g. sportfish consumption) (LaKind, Amina Wilkins, and Berlin, 2004). Next, toxicological research in animals to identify hazards and to gather mixture-specific dose-response information on postnatal developmental toxicity might be conducted using LPEC mixtures based on the findings of human biomonitoring data. Toxicological testing of the wide array of chemical mixtures found in the environment may yield information important for assessing the risk of health effects in various populations.
Risk communication
The focus of the workshop was on understanding transfer of chemicals from the environment to women and then to their breastfeeding infants. As has been noted previously (Berlin et al., 2002; Geraghty et al., 2008), research on chemicals in breast milk can inadvertently produce a barrier to breastfeeding as women develop concerns that breastfeeding may be unsafe despite the fact that breast milk is considered the best form of nutrition for the infant (Eidelman, 2012; Mead, 2008). Human exposure models focused on chemicals in breast milk may therefore produce the undesired effect of reducing breastfeeding rates, which runs counter to public health goals stated by the Department of Health and Human Services (HHS, 2011), the AAP (AAP, 2012), and the WHO (WHO, 2003).
While it is important to assess early life exposures as part of an overall risk assessment, it is also critical that messaging strategies be developed early in the process that are mindful of the potential for women to be discouraged inadvertently from breastfeeding. To help prevent unwarranted anxiety in breastfeeding women and in those deciding whether or not to breastfeed, researchers have encouraged a heightened attention to use of risk communication language that does not unduly frighten (LaKind, Fenton, and Dorea, 2009). For example, Berlin et al. (2002) stated, “…in human milk studies the communication of information to participants is at least as important as obtaining study data from the participants themselves.” Further, Dórea et al. (2012) noted, “Scientists conducting biomonitoring research using human milk have an obligation to understand the sensitivity of this issue and the impact their information and/or message may have on health professionals and breastfeeding mothers.” As an example of a messaging strategy sensitive to the concerns of breastfeeding women, the neutral phrase “lipophilic persistent environmental chemicals (LPECs)” was chosen over “persistent organic pollutants (POPs)” or “persistent, bioaccumulative and toxic (PBT) chemicals” to describe the chemical class of interest in this review.
Conclusions and future directions
In conclusion, specific improvements could be made for the three major components of the human health risk assessment process for LPECs: hazard identification, dose-response assessment, and exposure assessment. Identification of hazards to development requires an understanding of the timing of critical windows of exposure. However, for many developmental endpoints, the precise timing of these critical windows remains unknown. Modeling approaches can be used with data from epidemiological studies to identify critical windows of exposure in humans (Verner et al., 2010). Critical windows of exposure can also be identified in animals through the use of experimental designs that examine the effects of exposure during specific periods of time (Holladay and Smialowicz, 2000; Makris et al., 2008). Because the timing of developmental processes in humans and animals is often very different, it is important to understand this timing in all relevant species if animal data are to be used to support human health risk assessment. Future research should address this knowledge gap.
Dose response assessment may be impacted by species differences. For instance, because of differences in rates of elimination of LPECs, and thus, their bioaccumulation, between humans and laboratory animals, lactational exposure to a LPEC in offspring in an animal study may greatly differ from lactational exposure in a human infant whose mother was exposed to the same chemical at the same average daily dose as that administered to the animal dam. Modeling approaches can be used to estimate a human equivalent dose (HED) to improve the use of dose-response data from animal studies of early life exposure to LPECs. To improve the use of animal data in the modeling approaches, future toxicological studies could collect measures of internal dose in the same animals monitored for toxicological outcomes.
The accuracy of the exposure estimates produced by these modeling approaches depends on the availability of accurate data and parameter values for use in the models. Modeling approaches based on information from a mother’s exposure can also be used in an exposure assessment to estimate infant lactational exposures to LPECs. This is particularly useful for conducting an exposure assessment in situations where data on chemical concentrations in environmental media are available, but breast milk chemical concentrations are not. In addition, human biomonitoring data may be useful for reducing uncertainty in critical modeling parameters. It is important to measure LPEC concentrations in human milk to support neonatal exposure assessment and to gain a better understanding of chemical partitioning between milk and serum, including how this parameter may vary among women (LaKind et al., 2009).
A collaborative effort by the scientific community (e.g., public and private funding entities, academic researchers, regulators) would be useful to prioritize data gaps and protocol deficiencies identified in this review. The particular data gaps or protocol revisions that may be most beneficial to pursue will likely vary by LPEC depending on the existing database and associated hazards. Although it is difficult to rank the importance of the factors considered when implementing strategies in support of risk assessment of LPECs in milk, acquisition of reliable data or estimates to use in the selected models or to compare in a mixture assessment would seem paramount. Thus, for LPECs as a class of chemicals, resources might have the most impact if applied to the following areas in parallel: 1) expanding current reproductive and developmental test protocols (e.g., using OECD’s extended one-generation reproductive toxicity study as a model), 2) delineating metabolic pathways and rates, and 3) collecting biomonitoring data to reduce uncertainty and to establish “typical” breast milk LPEC mixtures for low, moderate, and high exposure groups.
The modeling approaches described in this review may prove to be useful in conducting risk assessments for exposure during development for many well-known LPECs [e.g. HCB, mirex, DDT, chlordane, PCBs, polybrominated diphenyl ethers (PBDEs), polychlorinated dibenzodioxins (PCDDs), polychlorinated dibenzofurans (PCDFs)]. In addition, there are LPECs that are not currently monitored. And, as new chemicals are synthesized or changes are made to the use and/or disposal of existing chemicals, there is the potential for more chemicals like these to enter the environment. Importantly, this review provides strategies that may be useful for the assessment of risk to children from possible health impacts of these emerging chemicals, for which very little data are likely to exist to support hazard identification or a dose-response assessment.
Although LPECs were the specific focus of this review, infants may be exposed to many other types of environmental chemicals. These include perfluorinated chemicals (PFCs), perchlorates, heavy metals, phthalates, bisphenols, and many more. For some of these, breastfed infant exposure may be of interest (Mead, 2008). However, it should be noted that formula-fed infants may also be exposed to certain chemicals for which neonatal developmental endpoints are of significance and also need to be adequately investigated (LaKind et al., 2005). And, both breastfed and formula-fed infants may also be exposed to environmental chemicals via non-dietary sources (e.g. air, soil, dust). A better understanding of critical windows of exposure in both humans and animals would support the identification of neonatal health impacts of chemicals with wide-ranging biochemical properties and sources of exposure.
Finally, when developing risk assessments that include evaluations of lactational exposures to environmental chemicals, many experts agree that it is important to develop parallel risk communication strategies that consider the benefits of breastfeeding to infant and maternal health (Berlin et al., 2005; Frank and Newman, 1993; LaKind, Amina Wilkins, and Berlin, 2004). Currently, when available evidence is considered, compared to formula feeding, breastfeeding is thought to be the healthiest option for infants despite the presence of environmental chemicals in breast milk (Eidelman, 2012; Mead, 2008). The goal of risk assessment efforts is not to discourage breastfeeding, but to accurately account for and evaluate all possible risk associated with chemical exposures and, if indicated, to help determine how to reduce chemical levels in breast milk by reducing maternal exposure.
Acknowledgements
Appreciation is expressed to Rebecca Dzubow, Susan Makris, Lyle Burgoon, and John Vandenberg (U.S. EPA) for providing a thorough review of the draft manuscript, to Audrey Turley (ICF International) for workshop planning, facilitation, and support, to Penny Kellar and Whitney Kihlstrom (ICF International) for technical editing and workshop support, to Kristen Fedak (ICF International) for research, technical writing, and workshop support, to Susan Knadle (California Environmental Protection Agency), Wilfried Karmaus (University of South Carolina), Walter Rogan and Paul Foster (National Institute of Environmental Health Sciences) for workshop participation, and to Anu Mudipalli and Sheppard Martin (U.S. EPA) for review of workshop briefing materials.
Footnotes
Declaration of interest The employment affiliation of the authors is shown on the cover page. The following authors were participants in a multidisciplinary workshop that served as the basis for this review paper: MAV, SAA, JSL, MHD, SH, MPL, MTP, DGF, YMT, SKS, CW, JCS, JLC, WGF, BMF, RSHY, JBB, HAE, SEF, JES, and RT. Some workshop participants chose not to participate as authors in the development of this review. Those individuals are acknowledged in the preceding section. The workshop was co-chaired by GML and EDM. ICF International organized the workshop under contract from the U.S. EPA (Contract No. EP-C-09-009, Work Assignments 2-62, 3-62, and 4-62). Workshop organization functions performed by ICF International included the independent identification and selection of workshop participants. ICF International is a for-profit firm providing professional services and technology solutions to clients in the following markets: energy, environment, and infrastructure; health, social programs, and consumer/financial; and public safety and defense. ICF International provides these services to both government and private sector clients. This research was also supported [in part] by the Intramural Research Program of the National Institutes of Health (NIH), National Institute of Environmental Health Sciences (NIEHS). The following workshop participants received support for travel and/or lodging: MAV, SAA, JSL, MHD, SH, MTP, DGF, SKS, WGF, BMF, RSHY, and JBB. MAV, SH, SKS, JLC, WGF, BMF, RSHY, JBB, and JSL received an honorarium for their participation in the workshop. LaKind Associates is a private consulting firm specializing in strategic risk management, assessment of human exposures and health risks, biomonitoring, state-of-the-science reviews, and environmental regulatory review; LaKind Associates consults to governmental and private sectors. The Hamner Institutes for Health Sciences is a nonprofit research institute with a primary focus on drug and chemical safety, including the development of methods to improve human health risk assessment. This paper has been reviewed in accordance with the peer and administrative review policies of the U.S. EPA, Food and Drug Administration (FDA), NIEHS, and Agency for Toxic Substances and Disease Registry (ATSDR) and approved for publication. The views expressed in this report are those of the authors and do not necessarily reflect the opinions and/or policies of the U.S. EPA, FDA, NIEHS or ATSDR. The remaining authors are all employees of either state governments or various academic institutions. Many of the academic scientists participating in the workshop and authoring this paper have received financial support for their research programs from the U.S. EPA and/or the NIH. All authors have sole responsibility as individual scientists for the writing and content of this review. The views, conclusions and recommendations are not necessarily those of their employers.
References
- AAP Breastfeeding and the use of human milk. Pediatrics. 2012;129:e827–e841. doi: 10.1542/peds.2011-3552. [DOI] [PubMed] [Google Scholar]
- Adams J, Barone S, Jr., Lamantia A, Philen R, Rice DC, Spear L, Susser E. Workshop to identify critical windows of exposure for children’s health: Neurobehavioral Work Group summary. Environ Health Perspect. 2000;108:535–544. doi: 10.1289/ehp.00108s3535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arcus-Arth A, Krowech G, Zeise L. Breast milk and lipid intake distributions for assessing cumulative exposure and risk. J Expo Anal Environ Epidemiol. 2005;15:357–365. doi: 10.1038/sj.jea.7500412. [DOI] [PubMed] [Google Scholar]
- Baker JL, Gamborg M, Heitmann BL, Lissner L, Sørensen TI, Rasmussen KM. Breastfeeding reduces postpartum weight retention. Am J Clin Nutr. 2008;88:1543–1551. doi: 10.3945/ajcn.2008.26379. [DOI] [PubMed] [Google Scholar]
- Berlin CM, Lakind JS, Fenton SE, Wang RY, Bates MN, Brent RL, Condon M, Crase BL, Dourson ML, Ettinger AS, Foos B, Fürst P, Giacoia GP, Goldstein DA, Haynes SG, Hench KD, Kacew S, Koren G, Lawrence RA, Mason A, McDiarmid MA, Moy G, Needham LL, Paul IM, Pugh LC, Qian Z, Salamone L, Selevan SG, Sonawane B, Tarzian AJ, Rose Tully M, Uhl K. Conclusions and recommendations of the expert panel: technical workshop on human milk surveillance and biomonitoring for environmental chemicals in the United States. J Toxicol Environ Health A. 2005;68:1825–1831. doi: 10.1080/15287390500226896. [DOI] [PubMed] [Google Scholar]
- Berlin CM, Lakind JS, Sonawane BR, Kacew S, Borgert CJ, Bates MN, Birnbach N, Campbell R, Dermer A, Dewey KG, Ellerbee SM, Fürst P, Giacoia GP, Gartner L, Groer M, Haynes SG, Humerick SS, Lawrence RA, Lorber M, Lovelady C, Mason A, Needham LL, Picciano MF, Plautz J, Ryan JJ, Selevan SG, Sumaya CV, Tully MR, Uhl K, Vesell E, Wilson JT. Conclusions, research needs, and recommendations of the expert panel: technical workshop on human milk surveillance and research for environmental chemicals in the United States. J Toxicol Environ Health A. 2002;65:1929–1935. doi: 10.1080/00984100290071801. [DOI] [PubMed] [Google Scholar]
- Bogen KT, Cullen AC, Frey HC, Price PS. Probabilistic exposure analysis for chemical risk characterization. Toxicol Sci. 2009;109:4–17. doi: 10.1093/toxsci/kfp036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrud LG, Flegal KM, Looker AC, Everhart JE, Harris TB, Shepherd JA. Body composition data for individuals 8 years of age and older: U.S. population, 1999–2004. National Center for Health Statistics. Vital Health Stat. 2010;11(250) [PMC free article] [PubMed] [Google Scholar]
- Butte NF, Hopkinson JM, Wong WW, Smith EO, Ellis KJ. Body composition during the first 2 years of life: an updated reference. Pediatr Res. 2000;47:578–585. doi: 10.1203/00006450-200005000-00004. [DOI] [PubMed] [Google Scholar]
- Byczkowski JZ, Lipscomb JC. Physiologically based pharmacokinetic modeling of the lactational transfer of methylmercury. Risk Anal. 2001;21:869–882. doi: 10.1111/0272-4332.215158. [DOI] [PubMed] [Google Scholar]
- Clewell RA, Gearhart JM. Pharmacokinetics of toxic chemicals in breast milk: use of PBPK models to predict infant exposure. Environ Health Perspect. 2002;110:A333–A337. doi: 10.1289/ehp.021100333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen Hubal EA, Moya J, Selevan SG. A lifestage approach to assessing children’s exposure. Birth Defects Res B Dev Reprod Toxicol. 2008;83:522–529. doi: 10.1002/bdrb.20173. [DOI] [PubMed] [Google Scholar]
- Dekant W. The role of biotransformation and bioactivation in toxicity. EXS. 2009;99:57–86. doi: 10.1007/978-3-7643-8336-7_3. [DOI] [PubMed] [Google Scholar]
- Desaulniers D, Cooke GM, Leingartner K, Soumano K, Cole J, Yang J, Wade M, Yagminas A. Effects of postnatal exposure to a mixture of polychlorinated biphenyls, p,p’-dichlorodiphenyltrichloroethane, and p-p’-dichlorodiphenyldichloroethene in prepubertal and adult female Sprague-Dawley rats. Int J Toxicol. 2005;24:111–127. doi: 10.1080/10915810590936382. [DOI] [PubMed] [Google Scholar]
- Dorea JG, Fenton SE, LaKind JS, Berlin CM., Jr. Researching chemicals in human milk can be conducted without discouraging breastfeeding. Bosn J Basic Med Sci. 2012;12:137–138. doi: 10.17305/bjbms.2012.2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eidelman AI. Breastfeeding and the use of human milk: an analysis of the American Academy of Pediatrics 2012 Breastfeeding Policy Statement. Breastfeed Med. 2012;7:323–324. doi: 10.1089/bfm.2012.0067. [DOI] [PubMed] [Google Scholar]
- Enzi G, Zanardo V, Caretta F, Inelmen EM, Rubaltelli F. Intrauterine growth and adipose tissue development. Am J Clin Nutr. 1981;34:1785–1790. doi: 10.1093/ajcn/34.9.1785. [DOI] [PubMed] [Google Scholar]
- Fenton SE, Condon M, Ettinger AS, Lakind JS, Mason A, McDiarmid M, Qian Z, Selevan SG. Collection and use of exposure data from human milk biomonitoring in the United States. J Toxicol Environ Health A. 2005;68:1691–1712. doi: 10.1080/15287390500225708. [DOI] [PubMed] [Google Scholar]
- Fiorotto ML, Burrin DG, Perez M, Reeds PJ. Intake and use of milk nutrients by rat pups suckled in small, medium, or large litters. Am J Physiol. 1991;260:R1104–R1113. doi: 10.1152/ajpregu.1991.260.6.R1104. [DOI] [PubMed] [Google Scholar]
- Fisher J, Mahle D, Bankston L, Greene R, Gearhart J. Lactational transfer of volatile chemicals in breast milk. Am Ind Hyg Assoc J. 1997;58:425–431. doi: 10.1080/15428119791012667. [DOI] [PubMed] [Google Scholar]
- Fisher JW, Whittaker TA, Taylor DH, Clewell HJ, III, Andersen ME. Physiologically based pharmacokinetic modeling of the lactating rat and nursing pup: A multiroute exposure model for trichloroethylene and its metabolite, trichloroacetic acid. Toxicol Appl Pharmacol. 1990;102:497–513. doi: 10.1016/0041-008x(90)90045-v. [DOI] [PubMed] [Google Scholar]
- Frank JW, Newman J. Breast-feeding in a polluted world - uncertain risks, clear benefits. Can Med Assoc J. 1993;149:33–37. [PMC free article] [PubMed] [Google Scholar]
- Geraghty SR, Khoury JC, Morrow AL, Lanphear BP. Reporting individual test results of environmental chemicals in breastmilk: potential for premature weaning. Breastfeed Med. 2008;3:207–213. doi: 10.1089/bfm.2008.0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GetData Graph Digitizer 2008 Available at: http://www.getdata-graph-digitizer.com/index.php.
- Haddad S, Poulin P, Krishnan K. Relative lipid content as the sole mechanistic determinant of the adipose tissue: Blood partition coefficients of highly lipophilic organic chemicals. Chemosphere. 2000;40:839–843. doi: 10.1016/s0045-6535(99)00279-9. [DOI] [PubMed] [Google Scholar]
- HHS . Executive Summary: The Surgeon General’s Call to Action to Support Breastfeeding. U.S. Department of Health and Human Services, Office of the Surgeon General; Washington, DC: 2011. Available at http://www.surgeongeneral.gov/library/calls/breastfeeding/executivesummary.pdf. [Google Scholar]
- Hines RN. The ontogeny of drug metabolism enzymes and implications for adverse drug events. Pharmacol Ther. 2008;118:250–267. doi: 10.1016/j.pharmthera.2008.02.005. [DOI] [PubMed] [Google Scholar]
- Hines RN, McCarver DG. The ontogeny of human drug metabolizing enzymes: phase I oxidative enzymes. J Pharmacol Exp Ther. 2002;300:355–360. doi: 10.1124/jpet.300.2.355. [DOI] [PubMed] [Google Scholar]
- Holladay SD, Smialowicz RJ. Development of the murine and human immune system: Differential effects of immunotoxicants depend on time of exposure. Environ Health Perspect. 2000;108:463–473. doi: 10.1289/ehp.00108s3463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ICF International . Improving the risk assessment of persistent, bioaccumulative, and toxic (PBT) chemicals in breast milk: Workshop summary report. U.S. Environmental Protection Agency; Washington, DC: 2013. Available at http://cfpub.epa.gov/ncea/risk/recordisplay.cfm?deid=262210. [Google Scholar]
- Kerger BD, Leung HW, Scott P, Paustenbach DJ, Needham LL, Patterson DG, Jr., Gerthoux PM, Mocarelli P. Age- and concentration-dependent elimination half-life of 2,3,7,8-tetrachlorodibenzo-p-dioxin in Seveso children. Environ Health Perspect. 2006;114:1596–1602. doi: 10.1289/ehp.8884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight CH, Docherty AH, Peaker M. Milk yield in rats in relation to activity and size of the mammary secretory cell population. J Dairy Res. 1984;51:29–35. doi: 10.1017/s0022029900023293. [DOI] [PubMed] [Google Scholar]
- Korth-Bradley JM, Parks V, Chalon S, Gourley I, Matschke K, Gossart S, Bryson P, Fleckenstein L. Excretion of moxidectin into breast milk and pharmacokinetics in healthy lactating women. Antimicrob Agents Chemother. 2011;55:5200–5204. doi: 10.1128/AAC.00311-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koss G, Koransky W. Studies on the toxicology of hexachlorobenzene: I pharmacokinetics. Arch Toxicol. 1975;34:203–212. doi: 10.1007/BF00353283. [DOI] [PubMed] [Google Scholar]
- Kreuzer PE, Csanady GA, Baur C, Kessler W, Papke O, Greim H, Filser JG. 2,3,7,8-Tetrachlorodibenzo-p-dioxin (TCDD) and congeners in infants. A toxicokinetic model of human lifetime body burden by TCDD with special emphasis on its uptake by nutrition. Arch Toxicol. 1997;71:383–400. doi: 10.1007/s002040050402. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL. 2000 CDC growth charts for the United States: Methods and development. National Center for Health Statistics. Vital Health Stat. 2002;11(246):36. [PubMed] [Google Scholar]
- LaKind JS, Amina Wilkins A, Berlin CM. Environmental chemicals in human milk: a review of levels, infant exposures and health, and guidance for future research. Toxicol Appl Pharmacol. 2004;198:184–208. doi: 10.1016/j.taap.2003.08.021. [DOI] [PubMed] [Google Scholar]
- LaKind JS, Berlin CM, Mattison DR. The heart of the matter on breastmilk and environmental chemicals: Essential points for healthcare providers and new parents. Breastfeed Med. 2008;3:251–259. doi: 10.1089/bfm.2008.0121. [DOI] [PubMed] [Google Scholar]
- LaKind JS, Berlin CM, Sjödin A, Turner W, Wang RY, Needham LL, Paul IM, Stokes JL, Naiman DQ, Patterson DG. Do human milk concentrations of persistent organic chemicals really decline during lactation? Chemical concentrations during lactation and milk/serum partitioning. Environ Health Perspect. 2009;117:1625–1631. doi: 10.1289/ehp.0900876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaKind JS, Brent RL, Dourson ML, Kacew S, Koren G, Sonawane B, Tarzian AJ, Uhl K. Human milk biomonitoring data: Interpretation and risk assessment issues. J Toxicol Environ Health A. 2005;68:1713–1769. doi: 10.1080/15287390500225724. [DOI] [PubMed] [Google Scholar]
- LaKind JS, Fenton SE, Dorea JG. Human milk biomonitoring of phthalates: expanding our understanding of infant exposure is compatible with supporting breastfeeding. Environ Int. 2009;35:994–995. doi: 10.1016/j.envint.2009.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landrigan PJ, Sonawane B, Mattison D, McCally M, Garg A. Chemical contaminants in breast milk and their impacts on children’s health: an overview. Environ Health Perspect. 2002;110:A313–315. doi: 10.1289/ehp.021100313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd-Smith M, Sheffield-Brotherton B. Children’s environmental health: intergenerational equity in action--a civil society perspective. Ann N Y Acad Sci. 2008;1140:190–200. doi: 10.1196/annals.1454.051. [DOI] [PubMed] [Google Scholar]
- Loccisano AE, Longnecker MP, Campbell JL, Jr., Andersen ME, Clewell HJ., 3rd Development of PBPK models for PFOA and PFOS for human pregnancy and lactation life stages. J Toxicol Environ Health A. 2013;76:25–57. doi: 10.1080/15287394.2012.722523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorber M, Phillips L. Infant exposure to dioxin-like compounds in breast milk. Environ Health Perspect. 2002;110:A325–A332. doi: 10.1289/ehp.021100325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makris SL, Thompson CM, Euling SY, Selevan SG, Sonawane B. A lifestage-specific approach to hazard and dose-response characterization for children’s health risk assessment. Birth Defects Res B Dev Reprod Toxicol. 2008;83:530–546. doi: 10.1002/bdrb.20176. [DOI] [PubMed] [Google Scholar]
- Martin J, Hamilton B, Ventura S, Osterman M, Wilson E, Mathews T. Births: Final data for 2010. no 1. Vol. 61. National Vital Statistics Reports; National Center for Health Statistics; Hyattsville, MD: 2012. Available at http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_01.pdf. [PubMed] [Google Scholar]
- Matthews HB, Dedrick RL. Pharmacokinetics of PCBs. Annu Rev Pharmacol Toxicol. 1984;24:85–103. doi: 10.1146/annurev.pa.24.040184.000505. [DOI] [PubMed] [Google Scholar]
- McDowell MA, Fryar CD, Ogden CL, Flegal KM. Anthropometric reference data for children and adults: United States, 2003–2006. National Center for Health Statistics; Hyattsville, MD: 2008. National Health Statistics Reports: No 10. Available at http://www.cdc.gov/nchs/data/nhsr/nhsr010.pdf. [PubMed] [Google Scholar]
- Mead MN. Contaminants in human milk: weighing the risks against the benefits of breastfeeding. Environ Health Perspect. 2008;116:A427–A434. [PMC free article] [PubMed] [Google Scholar]
- Milbrath MO, Wenger Y, Chang CW, Emond C, Garabrant D, Gillespie BW, Jolliet O. Apparent half-lives of dioxins, furans, and polychlorinated biphenyls as a function of age, body fat, smoking status, and breast-feeding. Environ Health Perspect. 2009;117:417–425. doi: 10.1289/ehp.11781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales E, Sunyer J, Castro-Giner F, Estivill X, Julvez J, Ribas-Fitó N, Torrent M, Grimalt JO, de Cid R. Influence of glutathione s-transferase polymorphisms on cognitive functioning effects induced by p,p’-DDT among preschoolers. Environ Health Perspect. 2008;116:1581–1585. doi: 10.1289/ehp.11303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council . Pesticides in the Diets of Infants and Children. National Academies Press; Washington, DC: 1993. Available at http://www.nap.edu/catalog.php?record_id=2126. [PubMed] [Google Scholar]
- Needham LL, Barr DB, Calafat AM. Characterizing children’s exposures: beyond NHANES. Neurotoxicology. 2005;26:547–553. doi: 10.1016/j.neuro.2004.09.006. [DOI] [PubMed] [Google Scholar]
- NTP . Specifications for the conduct of studies to evaluate the reproductive and developmental toxicity of chemical, biological and physical agents in laboratory animals. National Toxicology Program; Research Triangle Park, NC: 2011. Available at http://ntp.niehs.nih.gov/ntp/test_info/finalntp_reprospecsmay2011_508.pdf. [Google Scholar]
- OECD . Test No. 443: Extended one-generation reproductive toxicity study, OECD guidelines for the testing of chemicals, Section 4. OECD Publishing; Paris, France: 2011. Available at http://dx.doi.org/10.1787/9789264122550-en. [Google Scholar]
- Oken E, Rifas-Shiman SL, Field AE, Frazier AL, Gillman MW. Maternal gestational weight gain and offspring weight in adolescence. Obstet Gynecol. 2008;112:999–1006. doi: 10.1097/AOG.0b013e31818a5d50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oregon DEQ . Human health risk assessment guidance. Oregon Department of Environmental Quality; Portland, OR: 2010. Available at http://www.deq.state.or.us/lq/pubs/docs/cu/HumanHealthRiskAssessmentGuidance.pdf. [Google Scholar]
- Parham FM, Kohn MC, Matthews HB, DeRosa C, Portier CJ. Using structural information to create physiologically based pharmacokinetic models for all polychlorinated biphenyls. Toxicol Appl Pharmacol. 1997;144:340–347. doi: 10.1006/taap.1997.8139. [DOI] [PubMed] [Google Scholar]
- Peyret T, Poulin P, Krishnan K. A unified algorithm for predicting partition coefficients for PBPK modeling of drugs and environmental chemicals. Toxicol Appl Pharmacol. 2010;249:197–207. doi: 10.1016/j.taap.2010.09.010. [DOI] [PubMed] [Google Scholar]
- Poiger H, Schlatter C. Pharmacokinetics of 2,3,7,8-TCDD in man. Chemosphere. 1986;15:1489–1494. [Google Scholar]
- Poulin P, Haddad S. Advancing prediction of tissue distribution and volume of distribution of highly lipophilic compounds from a simplified tissue-composition-based model as a mechanistic animal alternative method. J Pharm Sci. 2012;101:2250–2261. doi: 10.1002/jps.23090. [DOI] [PubMed] [Google Scholar]
- Redding LE, Sohn MD, McKone TE, Chen JW, Wang SL, Hsieh DP, Yang RS. Population physiologically based pharmacokinetic modeling for the human lactational transfer of PCB-153 with consideration of worldwide human biomonitoring results. Environ Health Perspect. 2008;116:1629–1635. doi: 10.1289/ehp.11519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogan WJ, Ragan NB. Chemical contaminants, pharmacokinetics, and the lactating mother. Environ Health Perspect. 1994;102:89–95. doi: 10.1289/ehp.94102s1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selevan SG, Kimmel CA, Mendola P. Identifying critical windows of exposure for children’s health. Environ Health Perspect. 2000;1083:451–455. doi: 10.1289/ehp.00108s3451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skalsky HL, Guthrie FE. Binding of insecticides to human serum proteins. Toxicol Appl Pharmacol. 1978;43:229–235. doi: 10.1016/0041-008x(78)90002-9. [DOI] [PubMed] [Google Scholar]
- Spindler-Vomachka M, Vodicnik MJ, Lech JJ. Transport of 2,4,5,2′,4′,5′-hexachlorobiphenyl by lipoproteins in vivo. Toxicol Appl Pharmacol. 1984;74:70–77. doi: 10.1016/0041-008x(84)90271-0. [DOI] [PubMed] [Google Scholar]
- Thompson CM, Sonawane B, Barton HA, DeWoskin RS, Lipscomb JC, Schlosser P, Chiu WA, Krishnan K. Approaches for applications of physiologically based pharmacokinetic models in risk assessment. J Toxicol Environ Health B Crit Rev. 2008;11:519–547. doi: 10.1080/10937400701724337. [DOI] [PubMed] [Google Scholar]
- To-Figueras J, Barrot C, Sala M, Otero R, Silva M, Ozalla MD, Herrero C, Corbella J, Grimalt J, Sunyer J. Excretion of hexachlorobenzene and metabolites in feces in a highly exposed human population. Environ Health Perspect. 2000;108:595–598. doi: 10.1289/ehp.00108595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. EPA. Exposure factors handbook 2011 edition (final) U.S. Environmental Protection Agency; Washington, DC: 2011. Available at http://cfpub.epa.gov/ncea/cfm/recordisplay.cfm?deid=236252. [Google Scholar]
- U.S. EPA. Methodology for assessing health risks associated with multiple pathways of exposure to combustor emissions. U.S. Environmental Protection Agency; Washington, DC: 1998. Available at http://cfpub.epa.gov/ncea/CFM/recordisplay.cfm?deid=55525. [Google Scholar]
- U.S. EPA. [Accessed on January 10, 2014];Persistent Bioaccumulative and Toxic (PBT) Chemical Program. EPA Website [Online] 2013 Available at: http://www.epa.gov/pbt/index.htm. Updated on March 27, 2013. [Google Scholar]
- U.S. EPA . A review of the reference dose and reference concentration processes. U.S. Environmental Protection Agency; Washington, DC: 2002. Available at http://cfpub.epa.gov/ncea/cfm/recordisplay.cfm?deid=51717. [Google Scholar]
- U.S. EPA. Supplementary guidance for conducting health risk assessment of chemical mixtures. U.S. Environmental Protection Agency; Washington, DC: 2000. Available at http://cfpub.epa.gov/ncea/cfm/recordisplay.cfm?deid=20533. [Google Scholar]
- Verner MA, Ayotte P, Muckle G, Charbonneau M, Haddad S. A physiologically based pharmacokinetic model for the assessment of infant exposure to persistent organic pollutants in epidemiologic studies. Environ Health Perspect. 2009;117:481–487. doi: 10.1289/ehp.0800047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verner MA, Plusquellec P, Muckle G, Ayotte P, Dewailly E, Jacobson SW, Jacobson JL, Charbonneau M, Haddad S. Alteration of infant attention and activity by polychlorinated biphenyls: unravelling critical windows of susceptibility using physiologically based pharmacokinetic modeling. Neurotoxicology. 2010;31:424–431. doi: 10.1016/j.neuro.2010.05.011. [DOI] [PubMed] [Google Scholar]
- Verner MA, Sonneborn D, Lancz K, Muckle G, Ayotte P, Dewailly É , Kocan A, Palkovicová L, Trnovec T, Haddad S, Hertz-Picciotto I, Eggesbø M. Toxicokinetic modeling of persistent organic pollutant levels in blood from birth to 45 months of age in longitudinal birth cohort studies. Environ Health Perspect. 2013;121:131–137. doi: 10.1289/ehp.1205552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch RM, Findlay JW. Excretion of drugs in human breast milk. Drug Metab Rev. 1981;12:261–277. doi: 10.3109/03602538108994032. [DOI] [PubMed] [Google Scholar]
- WHO . Global strategy for infant and young child feeding. World Health Organization; Geneva, Switzerland: 2003. Available at http://www.who.int/nutrition/publications/infantfeeding/9241562218/en/index.html. [Google Scholar]
- Yesair DW, Feder PI, Chin AE, Naber SJ, Kuiper-Goodman T, Siegel Scott C, Robinson PE. Development, evaluation and use of a pharmacokinetic model for hexachlorobenzene. In: Morris CR, Cabral JRP, editors. Hexachlorobenzene: Proceedings of an international symposium. International Agency for Research on Cancer; Lyon, France: 1986. pp. 297–318. [PubMed] [Google Scholar]
- Yoon M, Schroeter JD, Nong A, Taylor MD, Dorman DC, Andersen ME, Clewell HJ., 3rd Physiologically based pharmacokinetic modeling of fetal and neonatal manganese exposure in humans: describing manganese homeostasis during development. Toxicol Sci. 2011;122:297–316. doi: 10.1093/toxsci/kfr141. [DOI] [PubMed] [Google Scholar]