Abstract
The Kilimanjaro Christian Medical University (KCMU) College and the Medical Education Partnership Initiative (MEPI) are addressing the crisis in Tanzanian health care manpower by modernizing the college’s medical education with new tools and techniques. With a $10 million MEPI grant and the participation of its partner, Duke University, KCMU is harnessing the power of information technology (IT) to upgrade tools for students and faculty. Initiatives in eLearning have included bringing fiber-optic connectivity to the campus, offering campus-wide wireless access, opening student and faculty computer laboratories, and providing computer tablets to all incoming medical students. Beyond IT, the college is also offering wet laboratory instruction for hands-on diagnostic skills, team-based learning, and clinical skills workshops. In addition, modern teaching tools and techniques address the challenges posed by increasing numbers of students. To provide incentives for instructors, a performance-based compensation plan and teaching awards have been established. Also for faculty, IT tools and training have been made available, and a medical education course management system is now being widely employed. Student and faculty responses have been favorable, and the rapid uptake of these interventions by students, faculty, and the college’s administration suggests that the KCMU College MEPI approach has addressed unmet needs. This enabling environment has transformed the culture of learning and teaching at KCMU College, where a path to sustainability is now being pursued.
The Kilimanjaro Christian Medical University (KCMU) College was established in 1997 by the Good Samaritan Foundation to expand the training activities of the Kilimanjaro Christian Medical Center (KCMC) and address the critical shortage of health care providers in Tanzania. KCMU College has grown substantially over the past 17 years and now ranks among the largest medical schools in Tanzania, offering 16 separate health-related degrees.
While many Sub-Saharan Africa medical schools have doubled enrollment over the past five years1, KCMU College has increased its enrollment ten-fold over the past 13 years– from 15 medical students in 1997 to 155 students matriculated in 2011. However, this dramatic increase in enrollment has not been accompanied by a commensurate increase in faculty size or physical infrastructure. For example, faculty grew from 49 in 1997 to 87 in 2011, a 78% increase, while medical student enrollment grew by nearly 1000% during the same period. Because of this, the college, with limited faculty and facilities, was faced with the challenge of effectively delivering medical education to vastly increased numbers of medical students.
To modernize medical education, leaders at KCMU College, in partnership with the Duke University School of Medicine (DUSOM), applied for and in 2010 received a 5-year, $10 million award from the Medical Education Partnership Initiative (MEPI). MEPI works with medical schools in Sub-Sahara Africa to, among other things, increase the number of high-quality physicians and health care workers, retain physicians in the countries where they are needed most, and expand research capacity by encouraging a focus on locally relevant challenges.
Among the 13 Sub-Saharan Africa medical schools that have received MEPI support, the KCMU College award was unusual because of its focus on advanced technology to assist in the delivery of medical education, and on modern teaching tools and techniques to address the challenges posed by the increased numbers of students. The selection of specific technologies and modern teaching techniques was determined during the grant application development process, in consultation with the KCMU College leadership, as well as with information technology (IT) and instructional design specialists at DUSOM.
A recent systematic review of the literature on eLearning in medical education in resource-constrained low- and middle-income countries has confirmed the advantages of harnessing these approaches.2 The identified benefits included supplementary tools to assist teaching by faculty and enhance efficiency; expansion of the pool of faculty by connecting to remote sites; and provision of digital resources for student use. Blended approaches to learning were most common and included computer-assisted learning, multimedia software, web-based learning, and electronic tutoring and mentoring programs.
Our overall objective was to transform the culture of teaching and learning at KCMU College. Our specific goals were to enhance medical education at KCMU College through the use of IT and modern teaching methodologies; transform the culture of learning at KCMU College and KCMC; enhance research skills and engage the interest of students in research; and sustain the transformed educational environment beyond the period of the MEPI award.
Our Approach to Change
Theoretical framework
We decided to introduce changes incrementally to avoid overwhelming the college’s existing education system. We selected the “Plan, Do, Study, and Act” (PDSA) approach because it encourages the evaluation of small changes before implementing interventions on a larger scale. The PDSA model involves a four-stage cycle for improvement, which consists of planning the change to be tested; carrying out the change on a limited scale; studying the change and summarizing what was learned; and determining which changes should be made for employment on a larger scale.3 This model has successfully been used elsewhere to initiate improvements in medical education.4
To transform the culture of learning and teaching, the KCMU College-MEPI team utilized the strategies shown in Table 1. The following describes the interventions, in the order in which we introduced them. These interventions were incrementally introduced over three years, and they were carefully evaluated following initial implementation. Although their description gives the impression of rapid change, the PDSA framework guided the entire process.
Table 1.
Strategies Adopted to Transform the Culture of Learning and Teaching at KCMU College
| The culture of learning | The culture of teaching |
|---|---|
| Use IT in learning | Harness IT to deliver instruction |
| Reduce student dependency on faculty to deliver study materials only | Provide study materials and references before classes |
| Enhance student learning prior to attending classes utilizing team-based learning | Prepare materials ahead of class and post them in the LCMS+ and practice team-based learning in the classroom |
| Expose students to basic laboratory practical sessions | Create a wet laboratory for acquisition of skills and encourage faculty to utilize the laboratory |
The interventions
We identified four mechanisms for change: to enhance Internet connectivity and access; to organize the curriculum, supporting materials, and student communications; to increase faculty efficiency; and to encourage locally relevant research. Enhancing connectivity and access was achieved by bringing a fiber-optic cable to campus, creating computer laboratories, providing incoming students with personal tablet computers, offering training in IT, and upgrading classrooms. Organization of the curriculum, supporting materials, and student communications was undertaken by introducing a learning management system, expanding wet laboratory experiences of students, and offering annual funding for Education Innovation Projects. Faculty efficiency was increased through the learning management system, which included online exams, automated grading, and improved communications with students. Locally relevant research was encouraged by offering competitive funding opportunities for mentored research projects by medical students.
Bringing fiber-optic cable to campus
Fiber-optic cable had been available in downtown Moshi approximately six kilometers distance from the college, and in January 2011 it was extended to the campus. The cable was disseminated underground to all campus buildings and facilities. In consultation with IT engineers from Duke University, wireless access points were installed throughout the campus to provide universal access. Equipment to manage bandwidth was installed to ensure that each entity in the campus network received the appropriate bandwidth (KCMU College, KCMC, Kilimanjaro Clinical Research Institute, School of Nursing, School of Rehabilitation Medicine, and Regional Dermatology Training Centre), which was based upon their ability to cover the cost of this bandwidth. MEPI covered the bandwidth expense for KCMU College, but other entities are responsible for their own ongoing bandwidth costs.
Computer access
In consultation with IT engineers from Duke University, two computer laboratories were created in March 2011. A student computer laboratory was designed and equipped with 30 iMac computers, and a separate faculty computer laboratory was renovated and equipped with 12 computers. We chose iMacs because of the high prevalence of PC-based computer viruses. Beginning with the first-year medical student class entering in October 2011, each student has also been given a personal tablet and external hard drive loaded with curricular materials.
Classroom upgrades
In consultation with audiovisual engineers and instructional designers from Duke University, four classrooms were upgraded with modern equipment in July 2011. The upgrades were designed to enhance the accommodation of large class sizes and to promote improved interactions between teachers and students. The equipment included enhanced computer projection and high-quality microphone systems.
IT training
A series of IT training workshops for students and faculty were offered in October 2011. Student participation was mandatory. Faculty participation increased over time and was supplemented with individual tutorials. It became evident that the IT training process requires ongoing effort and dedicated IT staff to achieve desired outcomes.
Learning management system
Given the challenges inherent in large class sizes and a KCMU College faculty that was overloaded with responsibilities, the college and MEPI leadership sought a learning management system that would assist with curriculum organization and delivery. After considering several options, in March 2011 we chose the Duke system, known as the Learning Content Management System Plus (LCMS+), and Duke graciously donated the system to KCMU College. LCMS+ was specifically designed for medical student curricula. It provides curriculum mapping, content management, support for evaluations and exams, patient encounter tracking, clinical skills assessment, scheduling functions, and support for team-based learning. A full-time LCMS+ supervisor for KCMU College was trained at Duke in July 2011 and, over time, two additional LCMS+ engineers have been added as demand for access expanded.
Wet laboratory
We created a wet laboratory to allow medical students hands-on diagnostic laboratory experience. The goals for the laboratory were to prepare students for assignments in remote locations that lack clinical laboratory resources and to prepare students for mastering the quickly expanding portfolio of rapid diagnostic tests. The wet lab space was renovated in January 2012 and equipped with instrumentation and a sophisticated audiovisual system to improve teacher-student interactions. A curriculum was developed with modular exercises and posted to the LCMS+.
Education innovation and mentored research training projects
Beginning in 2012, annual competitive opportunities have been made available to support research projects that bring education innovations to the KCMU College campus. In addition, competitive opportunities are also offered to support mentored research projects, with the quality of the mentorship plan an important criterion considered during the review process.
Outcomes
Wireless Internet utilization
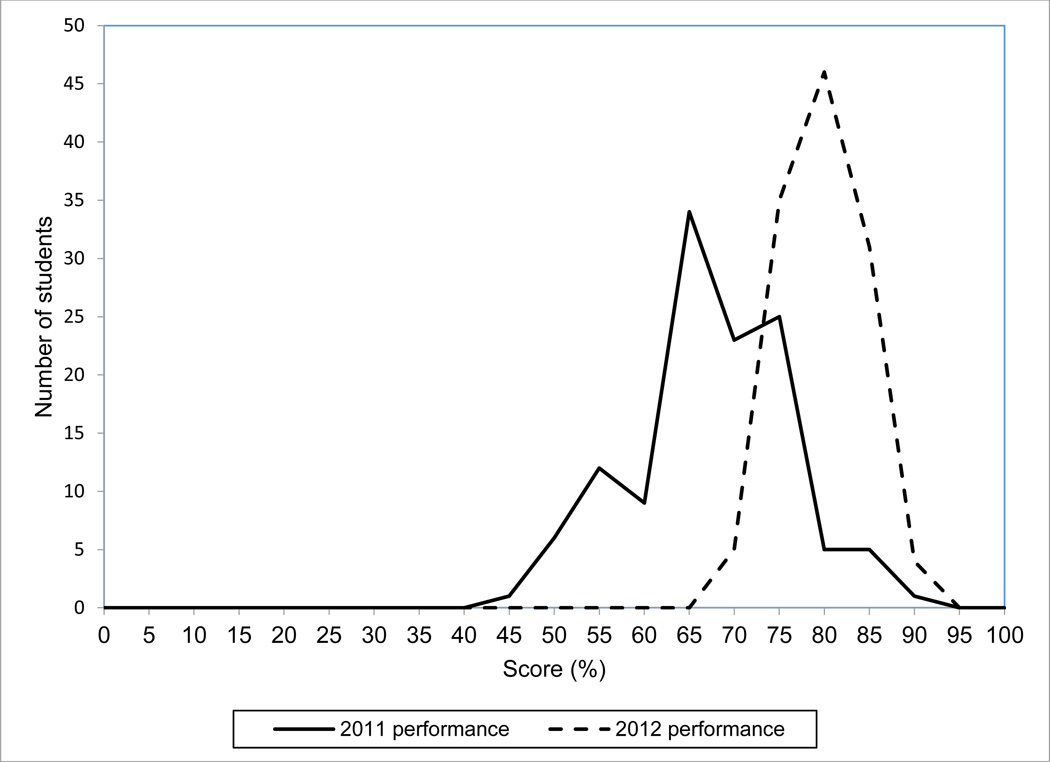
The uptake of wireless Internet usage among KCMU College students has been rapid, with 1,826 students (98%) across all academic programs now registered for access. One year after upgrading the wireless Internet, a survey of 128 first-year medical students found that 93 (73%) own computing devices (independent of the tablets issued through MEPI), and 96% of students had used the Internet to search for educational materials. These findings demonstrate that students recognize the importance of computing devices and use the Internet to enhance their education. In addition to the use of personal computing devices and tablets, the KCMU College Student Computer Laboratory hosts more than 100 students daily (Figure 1).
Figure 1.
The KCMU College student computer laboratory is equipped with 30 iMac computers and hosts more than 100 students daily.
LCMS+
By the end of the third year of the MEPI partnership (June 2013), all basic science study materials and curricula were included in the LCMS+ for students to access. LCMS+ usage was initially intended for only medical students but, as the benefits became more apparent, LCMS+ usage rapidly expanded to include curricula from programs in nursing, physiotherapy, health laboratory sciences, biostatistics and epidemiology, and the Master’s in Medicine program. A total of 494 students (158 MD1, 148 MD2, 15 physiotherapy, 38 BSc nursing, 53 BScHLS, and 82 postgraduates) were actively using LCMS+ at the end of the 2012/13 academic year. A survey from the first cohort of 154 MD1 students, given after using LCMS+ for one year, found that 138 (90%) of students reported frequent use of LCMS+ (daily to more than four days per week). Most students were pleased with the quality of the system, the content on LCMS+, and its enhancement of the learning process.5
On-line exams
The first computer-based examinations for medical students were given in March 2012. Today all basic sciences course examinations are given electronically. The KCMU College provost purchased an additional 90 iMac computers to expand this approach. An informal survey of faculty members who prepared computer-based examinations found great support for the system because of the time saved through an automated grading system.
Team-based learning
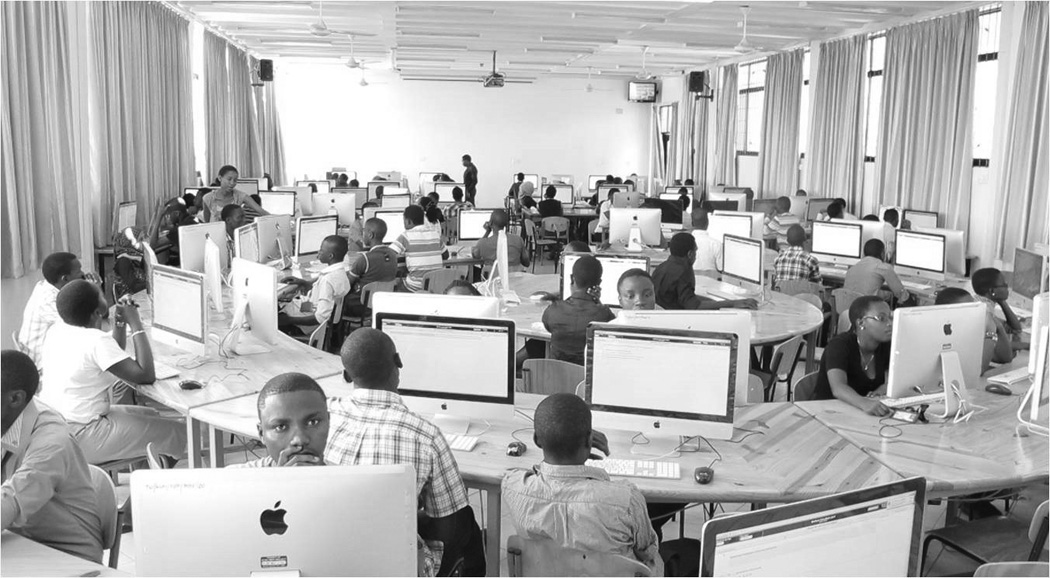
Team-based learning was adopted because of its potential to conserve faculty teaching time and a desire to use active teaching methods. Faculty from Duke Medical School and Duke-National University of Singapore introduced team-based learning to KCMU College faculty in 2012. Parasitology (Ectoparasites module) and community health were the first two courses taught using this approach. In a survey, students who completed the Ectoparasites module were highly supportive of the team approach.6 More importantly, their median final examination scores in 2012 were dramatically improved following the use of team-based learning compared to students during the previous year, when the same content was taught using didactic techniques (Figure 2).6 Team-based learning has now become an approved teaching method at KCMU College. Currently, eight faculty members utilize the team-based approach to teach three courses in the School of Medicine, and the School of Nursing faculty has also begun to use this method.
Figure 2.
Medical student Ectoparasite module final examination scores in 2011 when taught with didactic methods, and in 2012 when taught with team-based learning.
Wet laboratory
Faculty from the schools of medicine, nursing, health laboratory sciences, and physiotherapy have been increasingly using the wet lab in their programs. At the end of the 2012/13 academic year, 748 students at KCMU College had received instruction in the wet laboratory. The curriculum includes modules on laboratory safety, instrumentation, sample collection, handling and processing, hematology, blood transfusion, parasitology, clinical chemistry, point-of-care tests, and microbiology. The KCMU College provost is providing salary support for three technologists to staff the wet laboratory. The laboratory has also been used by the London School of Hygiene and Tropical Medicine as a component for its diploma in tropical medicine and hygiene course.
Education innovation projects
To date, two rounds of applications for the education innovation projects discussed above have been completed. Nine applications were received in each round, and five projects have been selected for funding. These projects include creation of a media center to create instructional videos; purchase of a vehicle to facilitate the transport of medical students to their community health rotations; and enhanced audiovisual support to aid in the teaching of anatomy and physiology.
Mentored research projects
Interest in the mentored research project program has been tremendous; through two rounds of applications, 42 proposals have been received and 22 have been funded. A total of 75 medical students have participated in these proposals and received mentoring from their faculty supervisors.
Teaching awards
The best faculty teachers, as voted by KCMU College students, have been recognized in a public ceremony at commencement for the past two years. The students have embraced the opportunity to nominate the best faculty teachers, with more than 80% of them voting.
Performance-based compensation plan
The KCMU College MEPI partnership created a performance-based compensation plan that measures participation in MEPI activities such as submitting curricular materials to LCMS+, workshops, and authorship of education innovation or mentored research projects, and allocates resources to support active participation. Each year, more than 80% of faculty and staff have received performance-based compensation.
Discussion
Through a deliberate and carefully planned process, the KCMU College, with support from MEPI and Duke, has introduced modern IT and teaching methods into the academic community, with the resources provided by MEPI and the partnership of DUSOM. The rapid uptake of these changes by the KCMC/KCMU College community, including students and faculty from multiple schools and programs, suggests that the college MEPI leadership has targeted interventions that address significant needs of the academic community. KCMU College plans to continue expansion of LCMS+ to include the entire medical school curriculum in the coming two years and will soon embark on a project to extend distance e-learning to medical students rotating at peripheral hospitals. These changes have been supported by dedicated IT staff, instructional design expertise, and monitoring and evaluation functions that allow documentation of impact. Other institutions that seek to replicate the KCMU College model should consider strategic investments in these areas.
To our knowledge, such a comprehensive set on interventions has not been undertaken previously in medical education within a low- or middle-income context.2 The incremental nature of the PDSA approach assisted us in their implementation, and several examples demonstrate the process. With regard to LCMS+, a modest goal of implementation for the first-year curriculum in October 2011 allowed observations and problem solving to occur, and in subsequent years LCMS+ was incrementally expanded to host one more year of the curriculum. Online exams were not introduced until March 2012, and they were gradually expanded to include all of the basic sciences. In the implementation of team-based learning, the instructors in two courses embraced this pedagogy. Over time, students’ perceptions were very positive and exam performance improved, and other faculty witnessed these potential benefits and began to use team-based learning.
Clearly, KCMU College was very fortunate to have the financial resources of MEPI. The cost for the interventions and programs described above is approximately $1 million USD a year. Sustainability beyond the MEPI award could prove challenging, but there are reasons for optimism. The initial investments in the fiber-optic cable, computer labs and wet laboratory, classroom upgrades, LCMS+, and online examinations should be sustainable at low cost. Internet bandwidth cost is decreasing, and the Tanzanian Ministry of Education recently invested in extending Internet accessibility to all Tanzanian universities. The contributions of the college to purchase computers and support salaries for the wet laboratory are encouraging. The creation of a KCMC Alumni and Career Counseling Office might offer opportunities to solicit alumni donations in the future. As class size has grown, tuition income to KCMU College has increased, offering new revenue to invest in expanding innovations.
In summary, the KCMU College MEPI project is transforming the culture of learning and teaching and has created an environment for continuing improvements. The genie is clearly out of the bottle.
Acknowledgments
Funding/Support: The Kilimanjaro Christian Medical Centre Medical Education Partnership Initiative is supported by the Health Resources and Services Administration (HRSA) Award T84HA21123. Dr. Bartlett also receives funding support from the United States National Institutes of Health Awards 3D43CA153722-03S1, 1D43TW009595, 5U01AI69484-08, and 5P30AI064518-05, and the Doris Duke Charitable Foundation 2012085.
Footnotes
Other disclosures: Dr. Bartlett and Mr. Muiruri are employees of Duke University Medical Center, which has a proprietary interest in the Learning Content Management System Plus. Dr. Bartlett and Mr. Muiruri have no direct financial interest in the company.
Ethical approval: Ethical approval was waived by the Kilimanjaro Christian Medical Centre Research Ethics Committee.
Previous presentations: This work was presented at the Consortium for Universities in Global Health Meeting, Washington, DC, May 2013.
Contributor Information
Esther Lisasi, monitoring and evaluation Officer, Kilimanjaro Christian Medical Centre Medical Education Partnership Initiative..
Ahaz Kulanga, project leader, Kilimanjaro Christian Medical Centre Medical Education Partnership Initiative, and deputy provost for administration, Kilimanjaro Christian Medical University College..
Charles Muiruri, Duke project leader, Kilimanjaro Christian Medical Centre Medical Education Partnership Initiative..
Lucy Killewo, learning content management system leader, Kilimanjaro Christian Medical Centre Medical Education Partnership Initiative..
Ndimangwa Fadhili, information technology leader, Kilimanjaro Christian Medical Centre Medical Education Partnership Initiative..
Lucy Mimano, wet laboratory director, Kilimanjaro Christian Medical Centre Medical Education Partnership Initiative..
Gibson Kapanda, biostatistician, Kilimanjaro Christian Medical Centre Medical Education Partnership Initiative..
Dativa Tibyampansha, learning content management system specialist, Kilimanjaro Christian Medical Centre Medical Education Partnership Initiative..
Glory Ibrahim, learning content management system specialist, Kilimanjaro Christian Medical Centre Medical Education Partnership Initiative..
Mramba Nyindo, associate professor, Kilimanjaro Christian Medical University College..
Kien Mteta, associate professor and dean of the Faculty of Medicine, Kilimanjaro Christian Medical University College..
Egbert Kessi, professor and provost, Kilimanjaro Christian Medical University College..
Moshi Ntabaye, adjunct professor of global health, Duke University, executive director, Kilimanjaro Christian Medical Centre, and principal investigator, Kilimanjaro Christian Medical Centre Medical Education Partnership Initiative..
John Bartlett, professor of medicine, global health, and nursing, Duke University, and co-principal investigator, Kilimanjaro Christian Medical Centre Medical Education Partnership Initiative..
References
- 1.Mullan F, Frehywot S, Omaswa F, et al. Medical schools in sub-Saharan Africa. The Lancet. 2010;377:1113–1121. doi: 10.1016/S0140-6736(10)61961-7. [DOI] [PubMed] [Google Scholar]
- 2.Frehywot S, Vovides Y, Talib Z, et al. E-learning in medical education in resource-constrained low- and middle-income countries. Human Resources for Health. 2013;11:4. doi: 10.1186/1478-4491-11-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Langley G, Nolan K, Nolan T, Norman C, Provost L. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance., 1996; Jossey-Bass, San Francisco, CA. cited in: Walley, P; Gowland, B. “Completing the circle: from PD to PDSA”. International Journal of Health Care Quality Assurance. 2004;17:6. doi: 10.1108/09526860410557606. ABI/INFORM Complete pg. 349. [DOI] [PubMed] [Google Scholar]
- 4.Murphy J. Using plan, do, study, act to transform a simulation center. Clinical simulation in Nursing. 2013;9:e257–e264. [Google Scholar]
- 5.Killewo L, Lisasi E, Kapanda G, et al. Introduction of a learning management system at the Kilimanjaro Christian Medical University College. African Journal of Health Professions Education. 2014 in press. [Google Scholar]
- 6.Nyindo M, Kitau J, Lisasi E, Kapanda G, Matowo J, Francis P, Bartlett J. Introduction of team-based learning (TBL) at Kilimanjaro Christian Medical University College: Experience with the Ectoparasites Module. Medical Teacher. 2014 doi: 10.3109/0142159X.2013.876490. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]