Abstract
Objective:
This study compared the safety and efficacy of the Supreme Laryngeal Mask Airway (S-LMA) with that of the ProSeal-LMA (P-LMA) in laparoscopic cholecystectomy.
Material and Methods:
Sixty adults were randomly allocated. Following anaesthesia induction, experienced LMA users inserted the airway devices.
Results:
Oropharyngeal leak pressure was similar in groups (S-LMA, 27.8±2.9 cmH2O; P-LMA, 27.0±4.7 cmH2O; p=0.42) and did not change during the induction of and throughout pneumoperitoneum. The first attempt success rates were 93% with both S-LMA and P-LMA. Mean airway device insertion time was significantly shorter with S-LMA than with P-LMA (12.5±4.1 seconds versus 15.6±6.0 seconds; p=0.02). The first attempt success rates for the drainage tube insertion were similar (P-LMA, 93%; S-LMA 100%); however, drainage tubes were inserted more quickly with S-LMA than with P-LMA (9.0±3.2 seconds versus 14.7±6.6 seconds; p=0.001). In the PACU, vomiting was observed in five patients (three females and two males) in the S-LMA group and in one female patient in the P-LMA group (p=0.10).
Conclusion:
Both airway devices can be used safely in laparoscopic cholecystectomies with suitable patients and experienced users. However, further studies are required not only for comparing both airway devices in terms of postoperative nausea and vomiting but also for yielding definitive results.
Keywords: Laparoscopic cholecystectomy, supraglottic airway devices, laryngeal mask airway, proseal, supreme
Introduction
Supraglottic airway devices are currently the most commonly used instruments in airway management. Some of the newer supraglottic airway devices have been modified to improve sealing and have separate respiratory and gastrointestinal tracts. One of the most popular types of airway devices is the Proseal-Laryngeal Mask Airway (P-LMA) device. Another is the Supreme Laryngeal Mask Airway (S-LMA) device which was introduced in 2007. The S-LMA, a disposable airway device, consists of the features of P-LMA, Fastrach LMA and Unique LMA, with its own gastric drainage channel, fixed curve tube, and maneuvering handle (1).
There are certain studies that compare the P-LMA and SLMA. In some of these studies, in which the oropharyngeal leak pressure (OLP) was used as a reference, the results of usage of these two airway devices were similar (2, 3). In other studies using the S-LMA device, the OLP was lower when compared with P-LMA (4, 5). We aimed to compare P-LMA and S-LMA in terms of safety and efficacy in surgery requiring high seal pressure such as laparoscopic cholecystectomy. OLP is commonly performed with the LMA to indicate the degree of airway protection, the feasibility of positive pressure ventilation and success of the placement of the supraglottic airway device (6). The primary objective of our study was to compare the OLP of the S-LMA and P-LMA. The secondary aim of this study was to compare the efficacy and safety of these two devices with respect to insertion success rates, insertion times, degree of gastric distension, intra- and post-operative adverse events, and hemodynamic and respiratory response to pneumoperitoneum.
Material and Methods
Patient Selection
After the institutional ethics committee approval regarding the study and written informed consents of all the patients were obtained, 60 adult patients (age range, 18–70 years) with ASA I or II, undergoing elective laparoscopic cholecystectomy were randomly and prospectively assigned to have either P-LMA (n=30, The Laryngeal Mask Co. Limited, Mahe, Seychelles) or S-LMA (n=30, The Laryngeal Mask Company, Singapore) for airway management. Randomisation was performed using a sealed envelope method. Patients who had an interdental gap <2.5 cm, and those with a BMI >35 kg.m−2, or those who were at risk of aspiration (non-fasted, gastroesophageal reflux disease) were excluded.
Study Procedures
Following premedication with intravenous midazolam (0.02–0.03 mg.kg−1), the patients were taken to the operating room and standard anaesthesia monitoring was applied. Anaesthesia was induced by fentanyl 2 μg.kg−1 and propofol 2 mg.kg−1. Neuromuscular blockade was achieved with intravenous rocuronium 0.6 mg.kg−1. The lungs were ventilated via a face mask until complete neuromuscular blockade was achieved. An experienced LMA user (use of P-LMA>100 times) performed all insertions and an independent observer collected the intra-operative data. A blinded, trained observer collected the data post-operatively.
A size 3 P-LMA or S-LMA was used for adults weighing 30–50 kg, a size 4 P-LMA or S-LMA was used for adults weighing 50–70 kg and a size 5 P-LMA or S-LMA was used for adults weighing 70–100 kg. A lidocaine spray was used as a lubricant for airway devices and drainage tubes. P-LMA was inserted using the digital insertion technique in the sniffing position, while S-LMA was inserted using the single-handed rotational technique in the semi-sniffing position in accordance with the manufacturer’s instructions. Following insertion, the patients’ heads were stabilized in the neutral position, the cuff of the airway device was air-inflated to a pressure of 60 cmH2O and the cuff pressure was maintained at 60 cmH2O throughout the procedure using a cuff monitor (Endotest; Rüsch, Kernen, Germany). The LMA was connected to a circle breathing system. The number of insertion attempts required for both devices was recorded. The consideration of device use as a failure required three attempts. In cases when it was not possible to achieve a satisfactory result with the randomised device, tracheal intubation was performed. OLP was identified by closing the expiration valve of the circle system at a constant gas flow of 3 L.min−1 (peak airway pressure was allowed as a maximum of 40 cmH2O).The pressure at which an audible leak occurred through the mouth was recorded. Insertion time was defined as the time between picking up the P-LMA or S-LMA and obtaining an effective airway. Once an effective airway was obtained, a well-lubricated 16-French size drainage tube was passed into the stomach in each patient and connected to the passive drainage system. Appropriate tube placement was verified by auscultation over the stomach while 20 mL of air was injected into the tube. The time elapsed for the proper placement of the tube was recorded. Anaesthesia was maintained with 4%–6% desflurane in 40% oxygen and nitrous oxide. The lungs were ventilated using a volume-controlled ventilator (Primus, Dräger Medical AG&Co., Lübeck, Germany) with a FiO2 of 0.40 and a tidal volume of 8 ml.kg−1 at a respiratory rate (RR) of 12 breaths.min−1, and with an inspiration/expiration ratio of 1/2 and 3 L.min−1 of a fresh gas flow. If the end-tidal carbon dioxide (ETCO2) increased above 40 mmHg, RR was first increased to 14 breaths.min−1 then 16 breaths.min−1, and then tidal volume was increased to 12 ml.kg−1. Ventilation was considered suboptimal if ETCO2 was >45 mmHg or failed if ETCO2 was >55 mmHg. If the SpO2 level fell below 95%, FiO2 was increased to 0.5, then 0.6. If SpO2 was observed within the value of 94–90% the oxygenation was considered suboptimal and if SpO2 was <90% oxygenation was considered as a failure.
Pneumoperitoneum was established by insufflations of carbon dioxide to a pressure of 14 mmHg. OLP, SpO2, expired tidal volume, ETCO2, RR, mean arterial pressure (MAP) and heart rate (HR) were recorded at four different measurement times: T0, control value, in the supine position, immediately before the induction of pneumoperitoneum; T1, five minutes after the induction of pneumoperitoneum, by positioning the patients’ heads with a head-up tilt of 30 degrees and with 15 degrees left lateral rotation; T2, five minutes before peritoneal deflation; and T3, after removal of the trocars and Veress cannulas in supine position. The surgeon, who was blinded to the airway device, scored the degree of gastric distension on an ordinal scale ranging from 0 (the best score) to 10 (worst score) at insertion of the laparoscope upon decompression of the pneumoperitoneum (7).
We administered a crystalloid solution at a rate of 2 mL.kg−1.h−1 during surgery. Before completion of the surgery, the patients received intravenous ondansetron (4 mg) to avoid postoperative nausea, vomiting, and intravenous paracetamol (1000 mg) in order to provide postoperative analgesia. All patients received atropine and neostigmine to reverse the neuromuscular blockade. The drainage tube was removed before discontinuation of anaesthesia. The P-LMA or S-LMA was removed at the end of surgery when the patient was able to open his/her mouth in response to a verbal command. Intraoperative complications including any circumstances such as aspiration, laryngospasm/bronchospasm, hypoxia (<92%), cough, hiccup, requirement for another airway device placement, blood staining on the airway device, and minor tongue/lip/dental trauma were recorded. SpO2, MAP, HR and postoperative nausea and vomiting were documented in the post anaesthesia care unit (PACU). A blinded anaesthesiologist questioned the patients in terms of postoperative pharyngolaryngeal adverse events (sore throat, dysphonia and dysphagia) before leaving the PACU. The patients graded the symptoms as 0 (none), 1 (mild), 2 (moderate) or 3 (severe).
Statistical analysis
Based on the results of a previous study, in which OLP for P-LMA was reported to be 29 cmH2O with a standard deviation of 6 cmH2O, a sample size calculation was performed (8). Sample size was based on an estimated difference of 5 cmH2O between the groups for OLP, a type 1 error of 0.05 and power of 90%; power analysis indicated that 28 patients per group would be required. In order to increase the study’s power and to secure the 28 required patients in case of any dropouts, we included 30 patients in each group. The SPSS 13.0 statistical software system (SPSS Inc, Chicago, IL, USA) was used for statistical analysis. The distribution of data was determined using the Kolmogorov-Smirnov analysis. Parametric data was analysed by paired t-tests in the groups and by an ANOVA test between the groups. Nonparametric data was analysed with the Mann-Whitney rank-sum test and the Chi-square test. A p value <0.05 was considered statistically significant.
Results
In the present study, 60 patients were randomised into either the S-LMA group (n=30) or the P-LMA group (n=30); however, one patient in the P-LMA group was excluded from the study since the laparoscopic procedure was transformed into an open procedure. Therefore, 59 patients were analyzed in this study (Figure 1). There were no significant differences between the patients’ status and preoperative airway characteristics of the groups (Table 1). The first insertion attempts were successful in 28 patients (93%) of the S-LMA group and 27 patients (93%) of the P-LMA group (p=0.68). The mean insertion time was significantly shorter in the S-LMA group than in the P-LMA group (12.5±4.1 sec versus 15.6±6.0 sec; p=0.027). Insertion success rates for the drainage tube were similar in both groups (S-LMA, 100%; P-LMA, 93%; p=0.23). Drainage tube was inserted more quickly in the S-LMA group than in the P-LMA group (9.0±3.2 sec versus 14.7±6.6 sec; p=0.001). The degree of gastric distension of the groups defined by the surgeon was similar (p=0.67) (Table 2). The data regarding OLP and respiratory changes during pneumoperitoneum are depicted in Table 3. No significant difference was found in terms of the mean values of OLP between the SLMA group and P-LMA groups at T0 (27.8±2.9 cmH2O versus 27.0±4.7 cmH2O; p=0.42). OLP values did not change during the induction of and throughout pneumoperitoneum. ETCO2 increased significantly during the pneumoperitoneum compared to control values with both S-LMA and P-LMA. The changes of ETCO2 values were not different between the groups. The adjusted settings of RR and FiO2 that were required for optimal ventilation and oxygenation were similar in the groups. SpO2 changes were in normal ranges and did not fall below 92% in any patient (Table 3).
Figure 1.
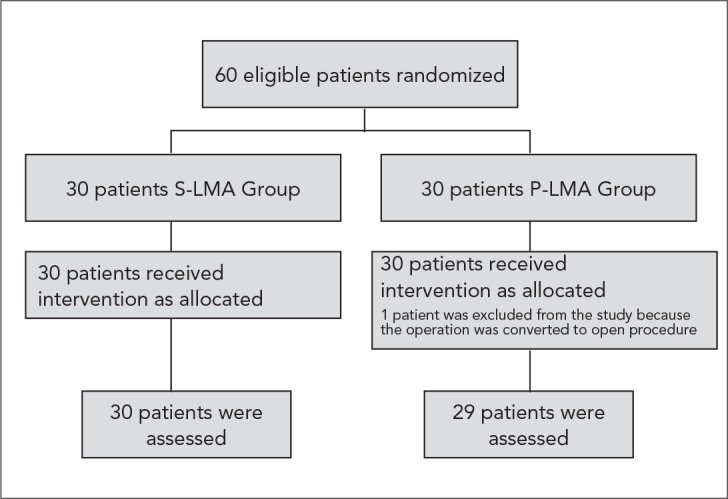
Patient flow chart
S-LMA: Supreme Laryngeal mask airway; P-LMA: Proseal Laryngeal mask airway
Table 1.
Patient status and pre-operative airway characteristics. Values are presented as mean±SD, or as numbers, or as numbers (%), as appropriate
| Proseal-LMA* (n=29) | Supreme-LMA* (n=30) | |
|---|---|---|
| Age, years | 44±14 | 50±9 |
| Height, cm | 169±8 | 169±10 |
| Weight, kg | 69±17 | 72±14 |
| Body mass index, kg.m−2 | 25±7.6 | 26±6.7 |
| ASA grade I / II | 14/15 | 14/16 |
| Preoperative drug usage, Yes/No | 14/15 | 14/16 |
| Smoking, Yes/No | 9/20 | 8/22 |
| Gender, Male/Female | 17/12 | 18/12 |
| Mallampati score, 1/2/3 | 20/6/3 | 19/6/5 |
| LMA size, 3/4/5* | 1/8/20 | 2/10/18 |
| Dentition, normal/lacking/edentulous | 8/20/1 | 4/24/2 |
LMA: Laryngeal mask airway
Table 2.
Assessment of airway device placement, surgical and anaesthtetic characteristics. Values are presented as mean±SD, or as numbers, or as numbers (%), as appropriate
| Proseal-LMA* (n=29) | Supreme-LMA* (n=30) | p value | ||
|---|---|---|---|---|
| Number of insertion attempts | 1 | 27 (93%) | 28 (93%) | 0.68 |
| 2 | 2 | 2 | ||
| 3 | 0 | 0 | ||
| Airway device insertion time, sec | 15.6±6.0 | 12.5±4.1 | 0.027 | |
| Drainage tube insertion attempts | 1 | 27 (93%) | 30 (100%) | 0.23 |
| 2 | 2 | 0 | ||
| 3 | 0 | 0 | ||
| Drainage tube insertion time, sec | 14.7±6.6 | 9.0±3.2 | 0.001 | |
| Duration of pneumoperitoneum, min | 62.7±32.3 | 62.2±31.0 | 0.94 | |
| Duration of anaesthesia, min | 68.3±9.4 | 69.2±10.5 | 0.73 | |
| Degree of gastric distension; 0/1/2/3/4/5 | 24/3/1/0/1 | 24/3/2/1/0 | 0.67 | |
| Total fentanyl dosage, μg | 150.0±26.8 | 140.3±26.3 | 0.16 |
LMA: Laryngeal mask airway
Table 3.
Respiratory, haemodynamic and oropharyngeal leak pressure changes during the induction of pneumoperitoneum. Values are presented as mean ± SD, or as numbers, as appropriate
| Time | Proseal-LMA* (n=29) | Supreme-LMA* (n=30) | p value | |
|---|---|---|---|---|
| Oropharyngeal leak pressure, cm H2O | T0 | 27.0±4.7 | 27.8±2.9 | 0.42 |
| T1 | 26.3±5.3 | 27. 6±4.9 | 0.30 | |
| T2 | 26.7±6.1 | 26.9±4.9 | 0.84 | |
| T3 | 26.1±5.4 | 27.2±5.1 | 0.40 | |
| End tidal CO2, mm Hg | T0 | 30.5±3.0 | 29.5±3.4 | 0.17 |
| T1 | 30.2±6.1 | 29.6±3.3 | 0.65 | |
| T2 | 34.0±3.7† | 33.5±2.9† | 0.53 | |
| T3 | 34.4±3.3† | 33.6±3.8† | 0.38 | |
| Expired tidal volume, mL | T0 | 616.3±98.8 | 591.8±110.0 | 0.37 |
| T1 | 620.3±99.4 | 588.8±110.9 | 0.25 | |
| T2 | 617.8±91.2 | 587.8±115.3 | 0.27 | |
| T3 | 613.0±94.5 | 589.7±114.4 | 0.39 | |
| Respiratory rate, breaths.min−1, 12/14/16 | T0 | 29/0/0 | 30/0/0 | 0.89 |
| T1 | 29/0/0 | 30/0/0 | 0.89 | |
| T2 | 25/4/0 | 25/3/2 | 0.34 | |
| T3 | 25/4/0 | 25/3/2 | 0.34 | |
| SpO2, % | T0 | 99.5±0.9 | 99.6±0.6 | 0.40 |
| T1 | 99.3±0.9 | 99.0±1.3† | 0.35 | |
| T2 | 98.5±1.4† | 98.4±1.1† | 0.65 | |
| T3 | 99.9±1.2† | 98.8±1.2† | 0.67 |
LMA: Laryngeal mask airway.
p<0.05 compared with the control values within the group.
T0; control value, T1; five minutes after the induction of pneumoperitoneum, T2; five minutes before peritoneal deflation; T3; after removal of the trocars and Veress cannulas.
In both groups, MAP decreased significantly during the induction of pneumoperitoneum compared with the control values; however, no significant change was observed in HR. There were no significant differences between the groups concerning haemodynamic responses during the induction of pneumoperitoneum, either. Aspiration, laryngospasm/bronchospasm, hypoxia and minor tongue/lip/dental trauma were not observed in any of the patients.
The rates of pharyngolaryngeal morbidity were also similar in the groups. Blood staining on the airway device was detected in one patient in the S-LMA group and in two patients in the P-LMA group. In the PACU, vomiting was observed in five patients (three females and two males) in the S-LMA group and in one female patient in the P-LMA group (p=0.10). There were no significant differences with respect to haemodynamic and respiratory responses between the groups in the PACU. The duration of the PACU stay was also similar between the groups (p=0.88) (Table 4).
Table 4.
Postoperative data in the post anaesthesia care unit. Values are presented as mean±SD, or as numbers (%), as appropriate
| Proseal-LMA* (n=29) | Supreme-LMA* (n=30) | p value | ||
|---|---|---|---|---|
| Sore throat, 0/1/2/3 | 25/4/0/0 | 28/2/0/0 | 0.31 | |
| Dysphonia, 0/1/2/3 | 29/0/0/0 | 30/0/0/0 | 0.89 | |
| Dysphagia, 0/1/2/3 | 28/1/0/0 | 27/2/1/0 | 0.51 | |
| Vomiting | 1 (3.4%) | 5 (16.6%) | 0.10 | |
| Mean arterial pressure, mmHg | 5th min | 110.8±18.9 | 102.5±17.8 | 0.08 |
| 15th min | 101.6±16.3‡ | 97.1±16.5‡ | 0.29 | |
| Heart rate, beats.min−1 | 5th min | 80.9±13.6 | 74.4±12.7 | 0.06 |
| 15th min | 74.6±9.8‡ | 69.6±12.4‡ | 0.09 | |
| SpO2, % | 5th min | 99.0±1.9 | 99.2±1.1 | 0.56 |
| 15th min | 99.6±0.7 | 99.6±0.9 | 0.92 | |
| Duration of staying in PACU; min† | 15.2±5.0 | 14.8±3.6 | 0.88 |
LMA: Laryngeal mask airway;
PACU: Post anaesthesia care unit,
P<0.05 between the 5th and 15th minute values within the group
Discussion
In this study, we compared the safety and efficacy of the SLMA and P-LMA in laparoscopic cholecystectomy procedures. The findings of our study showed that, even though the mean OLP values and airway device insertion success rates of two airway devices were similar to each other, the S-LMA was more quickly inserted than P-LMA.
While Carbon dioxide pneumoperitoneum results in ventilatory and respiratory change, thoracopulmonary compliance decreases and pulmonary resistance increases. Therefore, leak pressures gain a further significance with regards to the continuation of ventilation in laparoscopic cholecystectomy. While there are comparative studies on the safe usability of S-LMA in gynaecological laparoscopy, studies on laparoscopic cholecystectomy have not been reported in the literature yet (9). In our study, the mean OLP values with the S-LMA and PLMA were found as 27 cmH2O before the pneumoperitoneum, OLP did not change with the two airway devices throughout the pneumoperitoneum. The increase in ETCO2 values was not considered clinically significant as it was within physiological limits. Beleña et al. (10) found that the OLP was similar to our results (28 cmH2O) with S-LMA in their descriptive study and they suggested that S-LMA was used as a suitable airway device in laparoscopic cholecystectomy.
In a previous study which compared the S-LMA and P-LMA in gynaecological laparoscopy, the OLP and the maximum achievable tidal volume were lower with the S-LMA than with the P-LMA (9). In contrast, Abdi et al. (11) found that the OLP for the S-LMA was >30 cmH2O in 95% of the patients and SLMA and the tracheal tube were similarly effective airways. The technique of OLP measurement may influence the results. Abdi et al. (12) measured the OLP using the ventilator in a pressure-controlled manner and defined a sealing pressure. We measured OLP during manual ventilation and defined OLP as the pressure value at the moment when the audible sound of gas leakage from the mouth was heard. In our study, we measured OLP in regular intervals from the start until the completion of the surgery and found it similar at all time points. In their study, Lee et al. (9) examined a female population and inserted size 4 S-LMA or P-LMA. Abdi et al. (11) determined the size of S-LMA based on the height of the patient. We determined the size of the airway devices based on body weight and we used 3.4.and 5 sizes.
Van Zundert et al. (1) report that the increased OLP values with S-LMA are associated with the increase of intracuff pressures. Yet another study asserts that with the S-LMA, higher leak pressures are obtained at high intracuff pressures (12). On the contrary, despite the increased intracuff pressures during surgery, OLP did not increase in our previous study (3). While the silicone cuff of the P-LMA is permeable and intracuff pressure can increase when nitrous oxide is used, the cuff of the S-LMA is made of polyvinyl chloride is less elastic and less permeable to nitrous oxide (13). We maintained the cuff pressure at 60 cmH2O to eliminate the potential confounder effect of cuff pressure.
We found the first-attempt insertion success rate was 93% for both S-LMA and P-LMA. In the literature, first attempt success rates were reported to range between 90–100% for SLMA and 76–100% for P-LMA (1, 3, 14, 15).
In our previous study in which S-LMA and P-LMA were compared, we found that insertion times were similar with both airway devices (3). However, in this current study, we found that insertion time was shorter with S-LMA than with P-LMA. This difference, although statistically significant, is unlikely to be clinically important. Compared with the P-LMA, the design of S-LMA has several refinements: the airway tube has an anatomical shape, and more rigid than the P-LMA airway tube. This configuration allows for easy and reliable insertion. These advantages and increased experiences with S-LMA may be responsible for the shortened insertion time observed in the present study.
The drainage tube of the S-LMA is directly posterior to the ventilatory side and runs through the midline of the airway tube. We believe that an improved drainage tube design may explain the shortened insertion times of drainage tube for the S-LMA. This easy gastric access may be an additional safety benefit with the use of the S-LMA for this type of surgery.
Gastric distension may occur when high airway pressue is employed to overcome a partially obstructed airway or it may occur from inadvertent esophageal intubation with LMA. Consequently, this gastric distension may be a cause of nausea and vomiting and stomach perforation during laparoscopy (16, 17). In our study, the degree of gastric distension scores of the groups were similar. In more than 90% of cases, the surgeon estimated that scores were less than 2 with two airway devices.
When the patients had been evaluated before they were taken out the PACU, the postoperative adverse effects seemed to be similar. However, they were still under the influence of paracetamol at that time, the results could have been different if they had been evaluated at a later phase.
In the S-LMA group, the number of vomiting patients was higher than that in the P-LMA group. Although not statistically significant, this result may be clinically important. Since we had not predicted this outcome, we did not investigate the causes of nausea and vomiting. Measurement of gastric fluid volume, for example, could be useful to this end. This is one of the limitations of our study.
Conclusion
This study demonstrated that both the S-LMA and P-LMA groups had similar oropharyngeal leak pressures. Optimal ventilation and oxygenation were obtained with two airway devices, hence S-LMA can be used in laparoscopic cholecystectomies with suitable patients and experienced users as an alternative to the P-LMA. However, further studies are required, not only for comparing both airway devices in terms of postoperative nausea and vomiting, but also for yielding definitive results. The outcomes of such studies may affect the use of these two airway devices, particularly in laparoscopic cholecystectomies, in which these adverse effects are commonly observed.
Footnotes
It was presented in Turkish Anaesthesia and Reanimation Society, 44th Annual Congress. 27–31 Dec, Antalya, Turkey.
Conflict of Interest
No conflict of interest was declared by the authors.
References
- 1.Van Zundert A, Brimacombe J. The LMA Supreme--a pilot study. Anaesthesia. 2008;63:209–10. doi: 10.1111/j.1365-2044.2007.05421.x. [DOI] [PubMed] [Google Scholar]
- 2.Verghese C, Ramaswamy B. LMA-Supreme - a new single-use LMA with gastric access: a report on its clinical efficacy. Br J Anaesth. 2008;101:405–10. doi: 10.1093/bja/aen174. [DOI] [PubMed] [Google Scholar]
- 3.Hosten T, Gurkan Y, Ozdamar D, Tekin M, Toker K, Solak M. A new supraglottic airway device: LMA-Supreme, comparison with LMA-Proseal. Acta Anaesthesiol Scand. 2009;53:852–7. doi: 10.1111/j.1399-6576.2009.01986.x. [DOI] [PubMed] [Google Scholar]
- 4.Seet E, Rajeev S, Firoz T, Yousaf F, Wong J, Wong DT, et al. Safety and efficacy of laryngeal mask airway Supreme versus laryngeal mask airway ProSeal: a randomized controlled trial. Eur J Anaesthesiol. 2010;27:602–7. doi: 10.1097/eja.0b013e32833679e3. [DOI] [PubMed] [Google Scholar]
- 5.Eschertzhuber S, Brimacombe J, Hohlrieder M, Keller C. The laryngeal mask airway Supreme: a single use laryngeal mask airway with an oesophageal vent. A randomized, cross-over study with the laryngeal mask airway ProSeal in paralysed, anaesthetised patients. Anaesthesia. 2009;64:79–83. doi: 10.1111/j.1365-2044.2008.05682.x. [DOI] [PubMed] [Google Scholar]
- 6.Keller C, Brimacombe JR, Keller K, Morris R. Comparison of four methods for assessing airway sealing pressure with the laryngeal mask airway in adult patients. Br J Anaesth. 1999;82:286–7. doi: 10.1093/bja/82.2.286. [DOI] [PubMed] [Google Scholar]
- 7.Maltby JR, Beriault MT, Watson NC, Liepert D, Fick GH. The LMA-ProSeal is an effective alternative to tracheal intubation for laparoscopic cholecystectomy. Can J Anaesth. 2002;49:857–62. doi: 10.1007/BF03017420. [DOI] [PubMed] [Google Scholar]
- 8.Lu PP, Brimacombe J, Yang C, Shyr M. ProSeal versus the Classic laryngeal mask airway for positive pressure ventilation during laparoscopic cholecystectomy. Br J Anaesth. 2002;88:824–7. doi: 10.1093/bja/88.6.824. [DOI] [PubMed] [Google Scholar]
- 9.Lee AK, Tey JB, Lim Y, Sia AT. Comparison of the single-use LMA supreme with the reusable ProSeal LMA for anaesthesia in gynaecological laparoscopic surgery. Anaesth Intensive Care. 2009;37:815–9. doi: 10.1177/0310057X0903700537. [DOI] [PubMed] [Google Scholar]
- 10.Beleña JM, Gracia JL, Ayala JL, Núñez M, Lorenzo JA, de los Reyes A, et al. The Laryngeal Mask Airway Supreme for positive pressure ventilation during laparoscopic cholecystectomy. J Clin Anesth. 2011;23:456–60. doi: 10.1016/j.jclinane.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 11.Abdi W, Amathieu R, Adhoum A, Poncelet C, Slavov V, Kamoun W, et al. Sparing the larynx during gynecological laparoscopy: a randomized trial comparing the LMA Supreme and the ETT. Acta Anaesthesiol Scand. 2010;54:141–6. doi: 10.1111/j.1399-6576.2009.02095.x. [DOI] [PubMed] [Google Scholar]
- 12.Zhang L, Seet E, Mehta V, Subramanyam R, Ankichetty SP, Wong DT, et al. Oropharyngeal leak pressure with the laryngeal mask airway Supreme™ at different intracuff pressures: a randomized controlled trial. Can J Anaesth. 2011;58:624–9. doi: 10.1007/s12630-011-9514-6. [DOI] [PubMed] [Google Scholar]
- 13.Lumb AB, Wrigley MW. The effect of nitrous oxide on laryngeal mask cuff pressure: in vitro and in vivo studies. Anaesthesia. 1992;47:320–3. doi: 10.1111/j.1365-2044.1992.tb02173.x. [DOI] [PubMed] [Google Scholar]
- 14.Brain AI, Verghese C, Strube PJ. The LMA ‘ProSeal’-a laryngeal mask with an oesophageal vent. Br J Anaesth. 2000;84:650–4. doi: 10.1093/bja/84.5.650. [DOI] [PubMed] [Google Scholar]
- 15.Gaitini LA, Vaida SJ, Somri M, Yanovski B, Ben-David B, Hagberg CA. A randomized controlled trial comparing the ProSeal Laryngeal Mask Airway with the Laryngeal Tube Suction in mechanically ventilated patients. Anesthesiology. 2004;101:316–20. doi: 10.1097/00000542-200408000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Whitford JHW, Gunstone AJ. Gastric perforation: a hazard of laparoscopy under general anaesthesia. Br J Anaesth. 1972;40:97–9. doi: 10.1093/bja/44.1.97. [DOI] [PubMed] [Google Scholar]
- 17.Reynolds RC, Pauca AL. Gastric perforation, an anaesthesia-induced hazard in laparoscopy. Anesthesiology. 1973;38:84–5. doi: 10.1097/00000542-197301000-00021. [DOI] [PubMed] [Google Scholar]


