Abstract
Background:
The most commonly observed pathology in chest traumas is rib fracture, and the most important clinical symptom is severe pain.
Aims:
To investigate the effectiveness of intramuscular opioid (IMO), intravenous patient-controlled analgesia (IVPCA) and the Fentanyl transdermal therapeutic system (TTS) in the management of rib fracture pain.
Study Design:
Prospective randomized clinical trial.
Methods:
In our prospective and randomised study, we included 45 patients with a diagnosis of multiple rib fractures. There were three groups and intercostal nerve blockage (ICB) in the first day and oral paracetamol for five days was administered to each group as standard. In Group IMO (n=15), 4×40 mg pethidine HCl was administered to the patients, while in Group IVPCA (n=15) this was 5 μg/mL continuous intravenous fentanyl and was 50 μg fentanyl TTS in Group TTS (n=15). The demographics, injury data and vital signs of the patients were recorded. Pain was scored using Visual Analogue Scale (VAS). The pain during lying down (VASl) and mobilisation (VASm) was detected.
Results:
There were no differences between the three groups regarding age, sex, the trauma pattern, the number and distribution of costal fracture localisations, the presence of additional pathology, complications, thoracal catheter and the duration of thoracal catheter. No significant difference between the groups regarding systolic and diastolic arterial tension, number of breaths and beats in a minute was observed (p>0.05). We observed an improvement in the mean VAS score after treatment in all three groups. The mean VASl score significantly decreased after treatment in each group (p<0.05). The mean VASl and VASm scores measured on the 1st, 2nd, 3rd, 4th and 5th days were found to be higher in Group IMO than in Groups IVPCA and TTS; however, these differences were not statistically significant (p>0.05).
Conclusion:
In the analgesia of patients with multiple rib fractures, TTS administration with ICB showed similar effectiveness with IVPCA administration with ICB. In the management of pain due to multiple rib fractures, TTS administration is a safe, non-invasive and effective procedure.
Keywords: Multiple rib fracture, pain treatment, patient-controlled analgesia, transdermal therapeutic system
Introduction
In the management of patients with multiple rib fractures, effective pain treatment, pulmonary physiotherapy and respiratory care are essential components (1, 2). Pain due to multiple rib fractures may complicate the pulmonary damage caused after the trauma. The lack of enough and deep breathing, caused by pain, makes the patients’ mobilisation difficult and reduces the effectiveness of pulmonary physiotherapy (1, 3).
In the management of pain due to multiple rib fractures, intercostal blockage and parenteral administration of systemic opioids are among the most commonly applied procedures (4). The opioids used for this purpose can be administered in many different ways and dose intervals (3). The ways in which opioids are administered are mainly intramuscular, intravenously, patient controlled analgesia and thoracic epidural.
Our aim is to observe the effectiveness of the fentanyl transdermal therapeutic system (TTS) in the management of pain secondary to multiple rib fractures.
Material and Methods
Ethical approval was obtained from Afyon Kocatepe University Ethical Committee on the 18th February 2009, with the number 2–9, was obtained to perform the study. Our study was a prospective and randomised study. Randomisation was performed using a ‘Random Number Table’. We included patients with three or more rib fractures in our study. The patients’ demographics, the trauma patterns, analgesic administration methods, pain and sedation scores and complications were evaluated. The patients’ age, sex, trauma characteristics and pathologies accompanying rib fracture, the number of rib fractures, the presence of haemothorax and pneumothorax, and the necessity of chest tube was recorded. Visual Analogue Scale (VAS) was used for scoring pain. The effectiveness of the study was evaluated by scoring VAS during lying down (VASl) and VAS during mobilisation (VASm). VASl was scored before the treatment and on the 1st, 2nd, 3rd, 4th and 5th days after the treatment. VASm was scored on the 1st, 2nd, 3rd, 4th and 5th days after the treatment. The sedation due to opioids was monitored by Ramsey’s sedation scale (RSS) and arterial blood gas analysis. The patients’ number of breaths, pulse, arterial tension and O2Sat values were recorded. The study was ended on the 5th day of the treatment.
The patients were divided into three groups regarding the method used for the administration of narcotic treatment. In Group intramuscular opioid (IMO) (n=15), 4×40 mg/day of intramuscular pethidine HCl was administered to the patients. In Group intravenous patient-controlled analgesia (IVPCA) (n=15), 5μg/mL fentanyl was prepared in isotonic solution and administered using an IVPCA device (Model 6300 ambulatory infusion pump Smiths Medical, MD, USA). The IVPCA device was programmed to have a 5 mL bolus dose, a 20 minute locked period (basal infusion 4 mL/hr) and a 10 mL loading dose. In Group Fentanyl transdermal therapeutic system (TTS) (n=15), 50 μg transdermal fentanyl was administered plastering to the shoulder or upper arm. VAS was scored for all patients before the treatment and on the first day on which intercostal nerve blockage (ICB) was performed. In the course of ICB, 20 cc bupivacaine HCl was combined with 20 cc isotonic solution and 2 cc of this combination was applied to the intercostal level of each fractured costa. 4×500 mg/daily paracetamol was administered orally to all patients for five days.
Statistical Analysis
SPSS for Windows 13.0 (SPSS, Chicago, IL, USA) was used for statistical analysis. Sample size was determined prospectively using data from a previous study (Transcutaneous electric Nerve Stimulation for the treatment of post-thoracotomy pain: Randomised prospective study) in our institution. Power analysis indicated that 17 patients per group were required to detect the efficacy of TTS on VAS score (∝=0.05, β=0.2). One-Way ANOVA test was used to compare intergroup parametric values. We used the Tukey test to compare double group parametric values. Post hoc tests of repeated measures ANOVA design was used for the comparison of repeated measurements. We used the Chi-square test to compare the presence of complications and thoracal catheter, the need for intensive care and trauma patterns. Results were accepted statistically significant if p<0.05.
Results
The patients’ demographics and data regarding the injury secondary to the trauma are depicted in Table 1. There were no differences between the three groups with respect to age, sex, the number of rib fractures, the presence of pulmonary contusion, pneumothorax and haemothorax, the percentage of the presence of chest tube and accompanying additional pathologies (Table 1) (p>0.05).
Table 1.
Demographic and injury data
| Parameters | Group IMO (n=15) | Group PCA (n=15) | Group TTS (n=15) | p |
|---|---|---|---|---|
| Mean Age (yrs) | 51.5±11.3 | 43.8±10.9 | 49.7±13.5 | 0.09 |
| Sex Ratio (male/female) | 7/8 | 11/4 | 9/6 | 0.32 |
| Trauma pattern | 0.11 | |||
| Inside the vehicle | 5 | 7 | 5 | |
| Outside the vehicle | 6 | 4 | 4 | |
| Fall off | 4 | 4 | 6 | |
| Fractured ribs (n) | 5±1 | 5±2 | 5±2 | 0.22 |
| Patients with flychest (n) | 1 | 1 | 2 | 0.40 |
| Other fractured bones (n) | 2 | 3 | 4 | 0.07 |
| Patients with pulmonary contusion (n) | 9 | 5 | 4 | 0.06 |
| Patients with pneumothorax (n) | 3 | 4 | 4 | 0.27 |
| Patients with haemothorax (n) | 3 | 4 | 3 | 0.22 |
| Patients with chest tube (n) | 6 | 8 | 7 | 0.37 |
| Duration of chest tube (days) | 1.6±2.1 | 1.2±2.2 | 1.0±2.2 | 0.32 |
| Patients stayed in intensive care (n) | 1 | 2 | 2 | 0.13 |
IMO: Intramuscular opioid; IVPCA: Intravenous patient-controlled analgesia; TTS: Transdermal therapeutic system
We observed no significant difference between the groups regarding systolic and diastolic tension arterial, number of breaths and pulse in one minute, measured before the treatment and on the 1st, 2nd, 3rd, 4th and 5th days after the treatment (Figures 1 and 2) (p>0.05).
Figure 1.
The mean values of systolic and diastolic arterial tension. No significant differences between the groups regarding systolic and diastolic tension arterial measured before the treatment and on the 1st, 2nd, 3rd, 4th and 5th days after the treatment were observed (p>0.05). IMO: Intramuscular opioid; IVPCA: Intravenous patient-controlled analgesia; TTS: Transdermal therapeutic system
Figure 2.

The mean number of breaths per minute. No significant differences between the groups regarding the mean number of breaths per minute before the treatment and on the 1st, 2nd, 3rd, 4th and 5th days after the treatment were observed (p>0.05). IMO: Intramuscular opioid; IVPCA: Intravenous patient-controlled analgesia; TTS: Transdermal therapeutic system
No significant difference was observed with respect to the mean VASl scores before the treatment (Figure 3). The mean VASl scores decreased significantly after the treatment in each group (p<0.05). The mean VASl scores measured on the 1st, 2nd, 3rd, 4th and 5th days after the treatment were found to be higher in Group IMO compared to the Groups IVPCA and TTS. However, these differences were not statistically significant (p>0.05). The mean VASl score decreased by less than 3 on the 4th day in the Group IMO, on the 2nd day in the Group IVPCA and on the 1st day in the Group TTS. The mean VASl score decreased by less than 3 in the Group TTS at the earliest time point after treatment compared to the other groups.
Figure 3.

The mean VAS scores. The mean VASl score significantly decreased after the treatment in each group (p< 0.05). The mean VASl and VASm scores measured on the 1st, 2nd, 3rd, 4th and 5th days were found to be higher in Group IMO than in Groups IVCPA and TTS. However, these differences were not statistically significant (p>0.05). VAS: Visual Analogue Scale; VASl: The pain during lying down; VASm: The pain during mobilisation; IMO: Intramuscular opioid; IVPCA: Intravenous patient-controlled analgesia; TTS: Transdermal therapeutic system
The mean VASm scores measured on the 1st, 2nd, 3rd, 4th and 5th days after the treatment were found to be significantly higher in the Group IMO than the other groups (p<0.05). However, there were no significant differences between the Groups IVPCA and TTS in respect to the mean VASm scores (p>0.05). It was observed that the mean VASm scores decreased by fewer than 3 on the 4th day in the Group IVPCA and on the 3rd day in the Group TTS. The mean VASm score decreased by fewer than 3 at the earliest time point after the treatment compared to the other groups (Figure 3).
There were no significant differences between the groups in respect to the mean Ramsey’s sedation scores (p>0.05).
We observed no significant difference between the groups in respect to the mean PaO2 values measured in blood gas analysis before the treatment (p>0.05). The mean PaO2 values measured on the 1st, 2nd, 3rd, 4th and 5th days after the treatment were significantly higher in the Group IVPCA compared to the other groups (p<0.05) (Figure 4).
Figure 4.
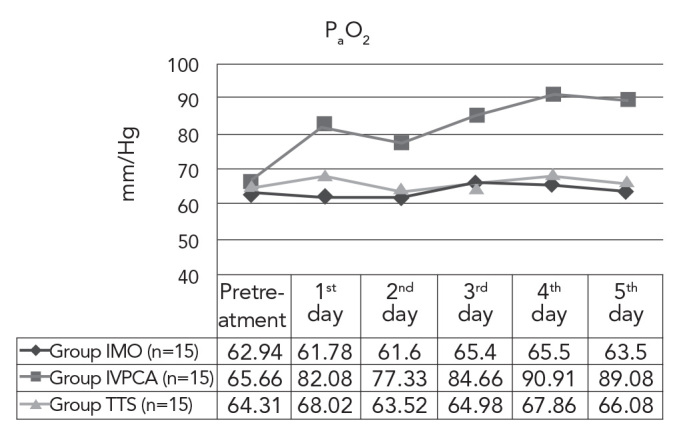
The mean PaO2 values. No significant differences between the groups in respect to the mean PaO2 values measured in blood gas analysis before the treatment were observed (p>0.05). The mean PaO2 values measured on the 1st, 2nd, 3rd, 4th and 5th days after the treatment were significantly higher in the Group IVPCA compared to the other groups (p<0.05) IMO: Intramuscular opioid; IVPCA: Intravenous patient-controlled analgesia; TTS: Transdermal therapeutic system
There were no significant differences between the groups regarding the mean O2sat, pH and PCO2 values on the 1st, 2nd, 3rd, 4th and 5th days after the treatment (p>0.05).
In the Group TTS, one patient had a headache, but it was not so severe and continuous that would require the cessation of treatment.
Discussion
The most confronted pathologies in thorax traumas are multiple rib fractures and pulmonary contusion; frequently, these are observed together. Pain due to rib fracture has a negative influence on respiratory physiology. Deep breathing, coughing and respiratory physiotherapy cannot be performed without effective analgesia. In this patient population, pulmonary contusion often accompanies rib fractures and dyspnoea develops more quickly (1–3). The effective treatment of pain will improve the patient’s respiratory mechanics. Therefore, the patient will be able to perform respiratory physiotherapy more comfortably and, as a result, the early mobilisation of the patient will prevent pulmonary complications (5–7). In this study, the effectiveness of the opioid administration using TTS, IVPCA and parenteral (IM) methods was compared in patients with multiple rib fractures. We observed that TTS administration provided equal pain management in this patient population.
In the management of pain due to multiple rib fractures, intercostal blockage and the administration of opioids are among the most frequently applied procedures (4, 8). The most common way in which the opioids are used is the parenteral method. It is essential to regulate opioid blood level for optimal pain management. The dose should be adjusted in order to not depress respiration and to not cause sedation, but to suppress pain by its systemic effect. The PCA device is one of the most frequently applied procedures that is able to provide these effects. By PCA device, it is possible to administer opioids safely in minimal doses and via continuous or intermittent intravenous mechanisms (1, 3, 4). PCA using opioids is one of the most common methods of providing postoperative analgesia for the treatment of acute pain (9, 10). The most significant risk when using PCA pumps is accidental overmedication leading to narcotic-induced respiratory depression. Furthermore, the PCA system requires a pump, line, tubing, power cables, and a pole. These are not only time consuming to set up and maintain, but may also reduce patient mobility and interfere with physical therapy (9, 11). In our study, we wanted to compare IVPCA method, of which the efficacy is obvious, with the TTS method, which is widespread in the management of different types of pain.
Systemic opioids are commonly used and are often the first-line management for relieving pain resulting from multiple rib fracture (3). However, many authors have reported that the efficacy of opioids in relieving pain is changeable because of respiratory depression risk and the difficulty of dose adjustment (1–4). Nevertheless, it is reported that the effective pain management can be performed when systemic opioids and locoregional nerve blockage methods are combined together (3, 4). In our study, we determined the fractured ribs’ levels and performed intercostal nerve blockage before opioid treatment. Intercostal nerve blockage provides highly effective analgesia lasting for 8–24 hours (3, 4); it can be administered to all fractured ribs except the first ribs. However, the requirement of multiple injections causes discomfort for the patients (3, 4). In our study, ICB was performed to the patients immediately after the diagnosis in the emergency service. Thus, the patient’s pain could be minimised. Also, effective pain treatment could be achieved during the window period until IVPCA was prepared and administered and until the effect of TTS fentanyl had started. Repetition of ICB was not required during IVPCA and TTS administration.
The most severe adverse effect of TTS is hypoventilation. The other adverse effects of TTS are nausea, vomiting, constipation, hypotension, bradycardia, dizziness, headache, confusion, hallucination, euphoria, itching, sweating and difficulty in urinating. Adverse effects related to the skin such as erythema and severe itching can be observed. Those effects generally disappear within 24 hours after the transdermal plaster is removed.
It is reported that TTS adverse effects are observed at doses of 60 μg and over for the management of acute pain. An effective and safe dose interval is reported to be between 40 and 60 μg (3,12). In our study, TTS was administered at the dose of 50 μg. One of our patients had nausea; however, this complaint was not as severe as to require quitting the treatment. We observed that TTS provided an advantage for the mobilisation of our patients.
TTS, as a non-invasive opioid administration technique, has advantages for both the patient and the nurse. The administration of ICB combined with TTS provided similar efficacy as the administration of ICB combined with IVPCA in the analgesia of our patients with multiple rib fractures. TTS is a safe, non-invasive and effective method in the treatment of pain secondary to multiple rib fractures.
Acknowledgments
The authors would like to thank to Ass. Prof. Dr. Reha Demirel from the Department of Public Health in Afyon Kocatepe University for his contributions on statistical analysis.
Footnotes
Ethics Committee Approval: Ethics committee approval from Afyon Kocatepe University Ethical Committe was obtained to perform the study (18.02.2009, No: 2–9).
Informed Consent: Written informed consent was received from the participants of this study.
Peer-review: Externally peer-reviewed.
Author contributions: Concept – O.S., Ö.S., Design – O.S., G.Ö., S.K.; Supervision - G.D., H.E., K.Ö., E.D.B.; Resource – O.S., G.Ö.; Materials – O.S., Ö.S., E.D.B.; Data Collection&/or Processing – G.D., K.Ö.; Analysis&/or Interpretation – O.S., R.D.; Literature Search – O.S.; Writing – O.S.; Critical Reviews – O.S.
Conflict of Interest: The authors declared no conflict of interest.
Financial Disclosure: The authors declared no financial disclosure.
References
- 1.Topcu I, Ekici Z, Sakarya M. Comparison of clinical effectiveness of thoracic epidural and intravenous patient-controlled analgesia for the treatment of rib fractures pain in intensive care unit. Ulus Travma Acil Cerrahi Derg. 2007;13:205–10. [PubMed] [Google Scholar]
- 2.Cicala RS, Voeller GR, Fox T, Fabian TC, Kudsk K, Mangiante EC. Epidural analgesia in thoracic trauma: effects of lumbar morphine and thoracic bupivacaine on pulmonary function. Crit Care Med. 1990;18:229–31. [PubMed] [Google Scholar]
- 3.Karmakar MK, Ho AM. Acute pain management of patients with multiple fractured ribs. J Trauma. 2003;54:615–625. doi: 10.1097/01.TA.0000053197.40145.62. [DOI] [PubMed] [Google Scholar]
- 4.Ho AM, Karmakar MK, Critchley LA. Acute pain management of patients with multiple fractured ribs: A focus on regional techniques. Curr Opin Crit Care. 2011;17:323–7. doi: 10.1097/MCC.0b013e328348bf6f. [DOI] [PubMed] [Google Scholar]
- 5.Liu S, Carpenter RL, Neal JM. Epidural anesthesia and analgesia. Their role in postoperative outcome. Anesthesiology. 1995;82:1474–506. doi: 10.1097/00000542-199506000-00019. [DOI] [PubMed] [Google Scholar]
- 6.Wisner DH. A stepwise logistic regression analysis of factors affecting morbidity and mortality after thoracic trauma: effect of epidural analgesia. J Trauma. 1990;30:799–805. doi: 10.1097/00005373-199007000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Brown SD, Walters MR. Patients with rib fractures: use of incentive spirometry volumes to guide care. J Trauma Nurs. 2012;19:89–91. doi: 10.1097/JTN.0b013e31825629ee. [DOI] [PubMed] [Google Scholar]
- 8.Truitt MS, Murry J, Amos J, Lorenzo M, Mangram A, Dunn E, Moore EE. Continuous intercostal nerve blockade for rib fractures: ready for primetime? J Trauma. 2011;71:1548–52. doi: 10.1097/TA.0b013e31823c96e0. [DOI] [PubMed] [Google Scholar]
- 9.Mattia C, Coluzzi F. Acute postoperative pain management: focus on iontophoretic transdermal fentanyl. Ther Clin Risk Manag. 2007;3:19–27. doi: 10.2147/tcrm.2007.3.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grass J. Patient-controlled analgesia. Anesth Analg. 2005;101:44–61. doi: 10.1213/01.ANE.0000177102.11682.20. [DOI] [PubMed] [Google Scholar]
- 11.Viscusi ER. Emerging techniques for postoperative analgesia in orthopedic surgery. Am J Orthop. 2004;33:13–6. [PubMed] [Google Scholar]
- 12.Chelly JE, Grass J, Houseman TW, Minkowitz H, Pue A. The safety and efficacy of a fentanyl patient-controlled transdermal system for acute postoperative analgesia: a multicenter, placebo-controlled trial. Anesth Analg. 2004;98:427–33. doi: 10.1213/01.ANE.0000093314.13848.7E. [DOI] [PubMed] [Google Scholar]



