Abstract
Having adequate numbers of qualified human resources for health (HRH) is essential for any effective health care system. However, there is a global shortage of skilled health care workers, especially in Sub-Saharan African countries. This shortage is exacerbated by a disproportionately high rate of infectious diseases, the burden of emerging chronic non-communicable diseases, and the emigration of medical doctors. Botswana has also experienced this critical shortage of doctors for many years. To address the shortage, the country in the 1990s embarked on an aggressive program to train its students at foreign medical schools. Despite intensified training, many graduates have not returned. As a result, the country decided to establish a medical school within Botswana. The newly established school was awarded a grant from the Medical Education Partnership Initiative (MEPI), which has helped to accelerate the school’s development. This paper describes the authors’ experiences, highlighting curriculum, staffing, infrastructure approaches, key successes, and challenges encountered. The paper concludes by proposing solutions. The authors’ experiences and the lessons learned can inform colleagues in other countries considering similar endeavors.
Adequate numbers of appropriately qualified human resources for health (HRH) are a critical component of any effective health system, being associated with positive health outcomes.1 Many regions suffer from a shortfall of health personnel. Africa represents 40% of the global shortfall, and the situation is critical in 36 of Sub-Saharan Africa’s 57 countries.1 The Sub-Saharan crisis is exacerbated by a disproportionately high rate of infectious diseases and the burden of emerging chronic non-communicable diseases.2–4 A major setback for the region has been the large numbers of highly trained doctors, educated in Sub-Saharan Africa countries, who have migrated outside the continent.3,5 For example, over the ten-year period 2002–2011, many Sub-Saharan countries experienced decreases in physician densities because of increasing migration.6 In addition, until 2010, eight Sub-Saharan countries had no medical schools of their own, which necessitated dependence on expatriates and external training.7
Although not as severely affected as most other Sub-Saharan counterparts, Botswana has for many years experienced its own physician shortages. Botswana, a country geographically smaller than Texas, has a population of two million but only 7,000 doctors (34 physicians for every 100,000 people).4 Only 21% of these physicians are citizens of Botswana.
To help address the shortage, Botswana in the 1990s embarked on an aggressive program to train its students at foreign medical schools. This effort was facilitated by a number of arrangements with countries such as Ireland, Australia, South Africa, and Ghana. Starting in 2000 and for the next 10 years, about 80 students annually were sent to other countries for training. By 2010, our doctors were being trained in at least 17 countries, and the Ministry of Education (MOE) estimates that by 2013 approximately 1,000 Batswanans will have graduated; despite intensified training, only 10% of the Botswana physicians have returned (personal communication – MOE). This was partly because of the lack of specialist training available in Botswana and also because some of the host countries view foreign medical graduates as an important component of their own HRH strategy.8 Thus, Botswana both heavily depends on expatriates and has difficulty in holding onto its own citizen-doctors. Clearly, external training has not been a cost-effective strategy because it is expensive to train doctors and difficult to retain them.6,9
In 1998, partly because of the external training strategy’s limited success, the president of Botswana issued a directive to establish a medical school at the University of Botswana (UB). The country’s first medical school opened in August 2009, enrolling the first 36 medical students in a five-year degree program after completing one year of pre-medical basic sciences. Six months later, the school established residency programs in internal medicine, pediatrics, public health, anesthesia, emergency medicine, family medicine, and pathology. As academics and officials at the University of Botswana School of Medicine (UBSOM), we believed such residency programs would be essential for building and retaining qualified HRH because the absence of specialist training was one of the reasons many of our externally trained doctors did not return.
In establishing the new medical school, a number of critical points had to be considered. Here we describe these experiences through discussing curriculum, staffing, and infrastructure approaches--and the successes and challenges we encountered. We conclude by proposing future directions.
Our Approach
Although UBSOM offers education and training at both the undergraduate and post-graduate levels, the primary reason for establishing the school was to train entry-level doctors. In establishing the school, we decided that three major aspects would be curriculum, staffing, and infrastructure, all of which we discuss below.
Curriculum
Based on advice from regional and international experts, such as the University of Witwatersrand Medical School in South Africa and the Hull York Medical School in the UK, we decided to use a community-oriented, learner-centered, problem-based curriculum delivered throughout the “teaching health system.” This approach meant that training would take place at health posts, clinics, hospitals, and elsewhere in the community. In crafting this approach, we considered a number of key factors, including Botswana’s experience in designing and implementing a medical curriculum, the country’s specific disease profile and needs, program structure and duration, and student entry requirements.
Designing and implementing a medical curriculum
Botswana had no previous experience in starting a new medical school, but our efforts received a boost in 2006, when, facilitated by an existing memorandum of understanding between the Botswana government and UB, Baylor College of Medicine contributed an experienced dean to live and work in-country for more than three years. This administrator oversaw the initial curriculum design and approval in 2007, helped determine staffing needs, and negotiated salary levels. This person also helped to guide the construction of a new building, identify satellite teaching sites, and identify optimum student enrolment numbers. A preliminary curriculum was approved in 2007, and revised versions were approved in 2009 and 2012.
Specific disease profile and needs
Although the curriculum has elements common to any medical school, a significant portion was informed by the disease profile and needs that are specific to Botswana. For example, our students spend a significant amount of time studying public health, family medicine, rural health, maternal and child health, surgery, HIV/AIDS, tuberculosis, and protozoal infections. Furthermore, in partnership with the Ministry of Health and community stakeholders, we decided that teaching would occur at four clinical sites located in different parts of the country (up to 1,000 km from the main campus), where the most people would benefit from specialist services. We hoped that early rural exposure during training would improve retention of health care workers in these areas.10–11 Thus, the curriculum was made socially accountable by addressing the country’s health care needs.12–15
Program structure and duration
We adopted a five-year, two-phase MBBS (bachelor of medicine and bachelor of surgery) program from the British model and customized it to our local needs. The program is integrated, spiralled (content of increasing complexity and breadth returns through the years), and system-, theme-, problem-, community-, and outcome-based. It is arranged in 2- to 8-week blocks, with each week devoted to a specific topic, such as HIV/AIDS or diabetes. Because students come without any problem-based learning (PBL) experience, they receive three 90-minute sessions of PBL training as part of orientation. We chose a guided PBL approach because it has been found to produce better results than either unguided PBL or traditional didactic teaching.16
Phase I of the training has three themes: biomedical sciences, doctor-patient relationships, and public health and medicine. During the two years of the first phase, students are grounded in the biomedical sciences, learn basic clinical and communication skills, and are introduced to patient contact and community-based learning. Phase II retains Phase I themes and covers the second three years. It is, however, predominantly clinical, with each year consisting of five 8-week rotations. Whereas Phase I students use paper-based cases, actual patient cases are used in Phase II as the basis for PBL. In both phases, most of the clinical teaching takes place at a national referral hospital in Gaborone (the capital), two district hospitals in the central and northern regions, a psychiatric hospital, and primary care clinics. Finally, for both phases we use standard assessment methods, such as multiple choice and modified essay questions, practical presentations, and objective structured clinical exams (OSCE), which is a multi-station, clinical skills examination, where students use simulated or actual patients, or models. Because students are exposed to early patient contact and training in clinical and communication skills, OSCEs are introduced in Year 1.
Staffing
Having adequate numbers of competent staff is a requirement for accreditation and is essential for establishing and sustaining any medical school. In addressing this, we considered the following criteria: minimum qualification requirements, numbers needed to teach, supply market, remuneration and benefits, faculty development, and capacity building.
Supply market, minimum qualifications, and numbers needed
Without experience in running a medical school, we expected that we could recruit significant numbers of senior and junior staff from the international and local communities, respectively. However, as we will discuss later, this proved to be overly optimistic. We deliberately set high qualification standards to attract the best staff and increase the likelihood of producing well-trained doctors. We required non-clinical and clinical scientists to have at minimum a master of science and master of medicine degree, respectively, or equivalent in their area of specialization. We estimated that we would need approximately 125 academics if we admitted about 100 undergraduate and 32 masters of medicine students annually.
Remuneration and benefits
Competitive salaries and benefits are a major requirement for attracting high-quality staff at medical schools.7 It is also generally accepted that academic salaries for clinicians are commonly higher than they are for other academic disciplines. Thus, in a bid to attract and help retain clinicians, we negotiated a separate and enhanced salary structure with university management and the Botswana government.
Faculty development, capacity building, and key partnerships
Recognizing the shortage of medical educators in Botswana, we knew that faculty development and capacity building should be priorities from inception. To date, UBSOM has hired nine staff development fellows, who are currently training under various specialities as potential clinical academics. Furthermore, since the vast majority of academics did not have PBL experience, all academics undergo training in basic PBL facilitation. Initially, we engaged the University of Witwatersrand in South Africa for this training, but we have since developed the expertise to train on our own.
The Botswana government has signed key agreements with Harvard University and the University of Pennsylvania, both of which helped UBSOM win a major grant from the Medical Education Partnership Initiative (MEPI). Our MEPI-funded program at the UB School of Medicine, called Botswana MEPI (BoMEPI), is funding projects in medical education, national maternal and child mortality, medical record reviews, and training in clinical audits. BoMEPI is also developing national primary care guidelines, supporting the training of research fellows, establishing a molecular diagnostics laboratory and Health Systems Research Unit, and helping facilitate the school’s stakeholder engagement on policy issues. The grant has been a significant catalyst in the development of the medical school.
Infrastructure
Following broad-based stakeholder consultations, we established the school within the University of Botswana. Placing the school within an established university provided important support through its extensive system of legal, regulatory, business, academic, and other processes and services. Similarly, UBSOM tapped into UB’s existing teaching and learning, research, and library resources. A government-financed state-of-the-art facility housing the new school was opened in 2012, and a new 450-bed teaching hospital is being built and is expected to open in 2014. These projects arguably represent the largest government investments ever in the country’s history and demonstrate political and public support for the School of Medicine. The BoMEPI funding has also immensely contributed to the infrastructure by providing office and research equipment, information and instructional technologies that enhance teaching, and connections between the main campus and remote teaching sites and other resources.
Successes
To begin with, it is noteworthy in itself that Botswana, having determined to open a medical school, was able to mobilize key resources and bring about this landmark accomplishment. It is a much-anticipated milestone that the first class of 36 doctors will graduate in 2014. Thereafter, approximately 50 doctors will graduate annually, greatly improving the health care system.7,17
One immediate benefit of having a medical school within Botswana is that the government has substantially reduced its training budget for medical students outside the country. The involvement of UBSOM at various government levels and clinical sites is helping shape national health care policy and delivery through participation of our students and specialist doctors in patient care, research, and formulation of health care protocols, guidelines, and policy.
The school has successfully established quality assurance procedures in line with the Botswana Health Professions Council (BHPC) accreditation standards, adopted from the World Federation for Medical Education, by appointing external examiners and setting up extensive committee structures. The BHPC subsequently granted the school provisional accreditation in 2013. Also notable are the collaborations we have established with regional and international partners, including the Consortium of New Southern African Medical Schools (CONSAMS). All of this has given us the ability to attract major grants, such as from MEPI, H3Africa, and the European Commission (FP7).
Challenges
Perhaps the biggest challenge the school faces is recruiting and retaining local and expatriate academics. During the five years since its inception, the school has fallen short of its staffing goal (revised to 87 academics) by 30-40%. Of particular concern is the persistently low 1:4 ratio of local to non-local staff, which makes building for the future and continuity problematic, since it is mostly non-locals who are leaving the school. Despite efforts to provide enhanced salaries for faculty clinicians, local entry-level medical specialists can still earn much more by working for the government, which funds both the public education and health sectors. Overall, university salaries are set with little regard for clinical experience and excellence but instead emphasize publications; and salaries have remained stagnant since 2007. Regionally, Namibia and South Africa pay doctors higher salaries, and, unlike Botswana, most other countries allow private practice for academics to supplement their salaries. This has the effect of exacerbating our recruitment and retention problems.
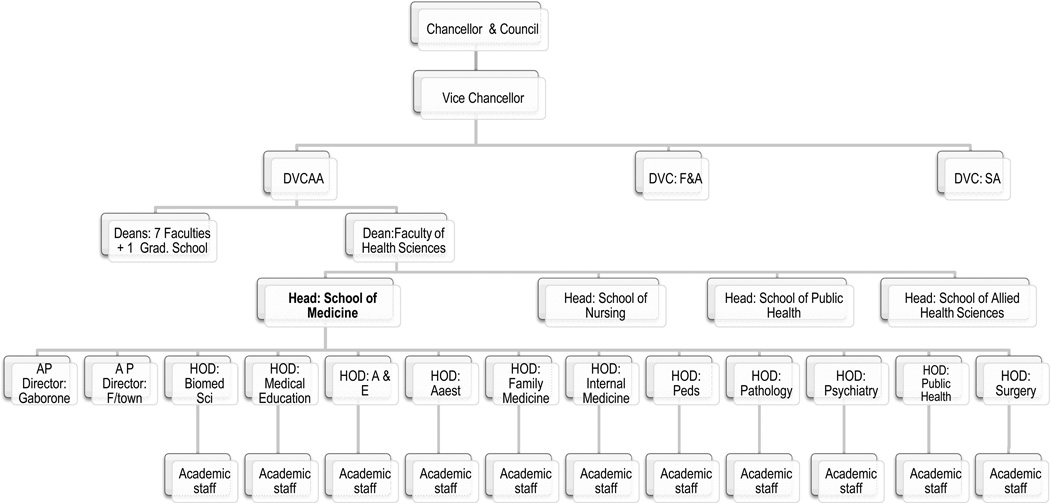
Despite the noted benefits, the placement of UBSOM within the existing university structure (Figure 1) has also had the unintended consequence of constraining the school. This is because the structure limits the school’s autonomy and requires us to follow often inflexible and time-consuming bureaucratic processes, all of which have negatively affected recruitment and retention efforts.18 As is often the case with new ventures, we were confronted with unexpected challenges. In our case, difficulties in recruiting and retaining faculty, combined with the unrealistic expectations of some students and the public, resulted in some negative media attention. All negative issues, as well as any underlying limitations, need to be addressed if we are to continue to provide high-quality education and training.
Figure 1.
The University of Botswana School of Medicine (UBSOM) as depicted within the larger university organizational structure. The structure shows that UBSOM is situated within the Faculty of Health Sciences (FHS), one of the seven faculties, with the head of UBSOM reporting to the dean of the faculty. The FHS dean in turn reports to the DVCAA, who then reports to the vice chancellor. DVCAA = Deputy Vice Chancelor of Academic Affairs; F&A = Finance and Administration; SA = Student Affairs; AP Director = Associate Programme Director; HOD = Head of Department; Biomed Sci = Biomedical Sciences; A&E = Accident and Emergency; Anest = Anesthesiology; Peds = Pediatrics; F/town = Francistown.
Future Directions
Despite the many challenges, we have accomplished much within a relatively short time. The school is a project of national strategic interest and will require vigorous government intervention.7 Critical problems cannot be addressed by UBSOM or the university management alone. For example, recruitment and retention challenges must be addressed. We propose four steps for doing this. First, there must be salary parity between entry-level specialists in the government and UBSOM. Second, for professionals with industry practice, experience and excellence are at least as important as the number of their published works. Third, although developing countries might not be able to match salaries paid in the private sector or in developed countries, Botswana should find creative ways to promote private practice for all academics and even government doctors in order to subsidize their salaries and thus reduce the already bloated government salary budget. Finally, there needs to be meaningful dialogue and research to determine the best ways to attract and retain academics.
At the university level, there needs to be a review of statutes and regulations to allow flexibility and autonomy so that the school and the university at large can more effectively and expeditiously respond to challenges. For example, by streamlining the recruitment process, at least for non-salaried adjunct faculty, the university could immediately help alleviate staff shortages. And although it is inevitable that any new program will create a certain amount of anxiety, the university should work with the school to engage students and the public with the current reality and planned improvements.
The accomplishments we have made during a relatively short period of time should hearten our colleagues both within Botswana as well as in other countries that might be considering improving their own medical education infrastructure, or creating one from the ground up. As we grow and improve, we see great potential to help transform Botswana’s health care system and, by extension, to improve the diagnosis, treatment, and prevention of disease and illness.
Acknowledgments
Funding/Support: The University of Botswana School of Medicine has received funding from the President’s Emergency Plan for AIDS Relief’s (PEPFAR’s) Medical Education Partnership Initiative (MEPI) through the Health Resources and Services Administration (HRSA) grant number T84HA21125.
Footnotes
Other Disclosures: None reported.
Ethical approval: Reported as not applicable.
Contributor Information
Gaonyadiwe G. Mokone, senior lecturer, Department of Biomedical Sciences, School of Medicine, University of Botswana, Gaborone, Botswana.
Maikutlo Kebaetse, senior lecturer, Department of Biomedical Sciences, School of Medicine, University of Botswana, Gaborone, Botswana.
John Wright, lecturer, Department of Biomedical Sciences, School of Medicine, University of Botswana, Gaborone, Botswana.
Masego B. Kebaetse, distance learning specialist, Botswana Medical Education Partnership Initiative, School of Medicine, University of Botswana, Gaborone, Botswana.
Oarabile Makgabana-Dintwa, training coordinator, Health Systems Research Unit, Botswana Medical Education Partnership Initiative, School of Medicine, University of Botswana, Gaborone, Botswana.
Poloko Kebaabetswe, director, Health Systems Research Unit, Botswana Medical Education Partnership Initiative, School of Medicine, University of Botswana, Gaborone, Botswana.
Ludo Badlangana, lecturer, Department of Biomedical Sciences, School of Medicine, University of Botswana, Gaborone, Botswana.
Mpho Mogodi, lecturer, Department of Public Health and Family Medicine, School of Medicine, University of Botswana, Gaborone, Botswana.
Katie Bryant, consultant researcher, Botswana-UPenn Partnership, Gaborone, Botswana.
Oathokwa Nkomazana, associate program director and Botswana Medical Education Partnership Initiative principal investigator, School of Medicine, University of Botswana, Gaborone, Botswana.
References
- 1.World Health Organization. Geneva: WHO; 2006. [Accessed April 17, 2014]. The World Health Report 2006 - working together for health. http://www.who.int/whr/2006/en/. [Google Scholar]
- 2.Chen L, Evans T, Anand S, et al. Human resources for health: Overcoming the crisis. The Lancet. 2004;364(9449):1984–1990. doi: 10.1016/S0140-6736(04)17482-5. [DOI] [PubMed] [Google Scholar]
- 3.Van Lerberghe W. Geneva: World Health Organization; 2008. [Accessed April 17, 2014]. The world health report 2008: Primary health care: Now more than ever. http://www.who.int/whr/2008/en/. [Google Scholar]
- 4.World Health Organization. Geneva: World Health Organisation; 2012. [Accessed April 17, 2014]. World Health Statistics 2012. http://www.who.int/gho/publications/world_health_statistics/2012/en/. [Google Scholar]
- 5.Clemens MA, Pettersson G. New data on African health professionals abroad. Human Resources for Health. 2008;6(1):1–11. doi: 10.1186/1478-4491-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tankwanchi ABS, Özden Ç, Vermund SH. Physician emigration from Sub-Saharan Africa to the United States: Analysis of the 2011 AMA Physician Masterfile. PLoS Medicine. 2013;10(9):e1001513. doi: 10.1371/journal.pmed.1001513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen C, Buch E, Wassermann T, et al. A survey of Sub-Saharan African medical schools. Human Resources for Health. 2012;10(4) doi: 10.1186/1478-4491-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hawthorne L, Hamilton J. International medical students and migration: The missing dimension in Australian workforce planning? Medical Journal of Australia. 2010;193(5):262–265. doi: 10.5694/j.1326-5377.2010.tb03903.x. [DOI] [PubMed] [Google Scholar]
- 9.Kirigia JM, Gbary AR, Muthuri LK, et al. The cost of health professionals' brain drain in Kenya. BMC Health Services Research. 2006;6(1):89. doi: 10.1186/1472-6963-6-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Curran V, Rourke J. The role of medical education in the recruitment and retention of rural physicians. Medical Teacher. 2004;26(3):265–272. doi: 10.1080/0142159042000192055. [DOI] [PubMed] [Google Scholar]
- 11.Wilson N, Couper I, De Vries E, et al. A critical review of interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas. Rural Remote Health. 2009;9(2):1060. [PubMed] [Google Scholar]
- 12.Wood DF. ABC of learning and teaching in medicine: Problem based learning. British Medical Journal. 2003;326(7384):328–330. doi: 10.1136/bmj.326.7384.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dolmans DH, De Grave W, Wolfhagen IH, Van Der Vleuten CP. Problem-based learning: Future challenges for educational practice and research. Medical Education. 2005;39:732–741. doi: 10.1111/j.1365-2929.2005.02205.x. [DOI] [PubMed] [Google Scholar]
- 14.Worley P, Prideaux D, Strasser R, Magarey A, March R. Empirical evidence for symbiotic medical education: A comparative analysis of community and tertiary-based programmes. Medical Education. 2006;40:109–116. doi: 10.1111/j.1365-2929.2005.02366.x. [DOI] [PubMed] [Google Scholar]
- 15.Frenk JL, Chen Bhutta A, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. The Lancet. 2010;376(9756):1923–1958. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt HG, Rotgans JI, Yew EHJ. The process of problem-based learning: what works and why. Medical Education. 2011;45:792–806. doi: 10.1111/j.1365-2923.2011.04035.x. [DOI] [PubMed] [Google Scholar]
- 17.Jennifer Kasper FB. Brain drain in sub-Saharan Africa: contributing factors, potential remedies and the role of academic medical centres. Archdischild. 2012 doi: 10.1136/archdischild-2012-301900. 10.1136/archdischild-2012-301900. [DOI] [PubMed] [Google Scholar]
- 18.Wynford-Thomas D, Stewart P, Mathieson P, et al. Organisation and management of medical schools: A survey of ten UK Universities. [accessed April 17, 2014];Medical Schools Council. 2012 Aug; http://www.medschools.ac.uk/Publications/Documents/Organisation_and_Management_of_Medical_Schools.pdf.