Abstract
Context:
The management of heart failure (HF) is challenging, with high rates of readmission and no single solution. MaineHealth, a health care system serving southern Maine, has shown initial success with home health nurses partnering with physicians in the management of complex patients with HF using the MaineHealth Home Diuretic Protocol (HDP).
Objective:
To demonstrate that augmented diuretic therapy, both oral and intravenous, an evidence-based treatment for care of patients with HF experiencing fluid retention, can be delivered safely in the home setting using the HDP and can improve outcomes for recently hospitalized patients with HF.
Design:
In late 2011, the MaineHealth HDP was implemented in two hospitals and in the home health agency serving those hospitals. The patient population included recently hospitalized patients with a diagnosis of advanced HF, eligible for home health services and telemonitoring.
Main Outcome Measures:
Home health nurses reported data on the patients managed using the protocol, including interventions made, physical findings, lab values, and patient disposition after each episode of care. Questionnaires were used to determine patient and clinician satisfaction.
Results:
Sixty patients meeting the criteria above were enrolled between November 2011 and January 2014. The protocol was initiated 84 times for 30 of these patients. Sixteen patients had multiple activations. The readmission rate was 10% and no adverse outcomes were observed. Clinician and patient satisfaction was 97% or greater.
Conclusion:
The MaineHealth HDP can be delivered effectively and safely to improve outcomes, reducing readmissions and allowing patients to remain at home.
Introduction
Heart failure (HF) is one of the primary causes of hospitalization and rehospitalization in Maine and the nation.1–3 Care of these patients is complex.4 After an admission for HF, nearly 25% of patients are readmitted within 30 days, and by 6 months this proportion reaches nearly 50%.5,6
MaineHealth, a nonprofit health system in Maine, works through its Heart Failure Workgroup (Workgroup) to promote best practices across the care continuum to improve quality, to optimize patient outcomes, and to make the best use of health care resources. Readmission rates serve as indicators of quality. Reducing avoidable readmissions for HF patients is a systemwide improvement objective.
Home health nurses, as members of the Workgroup, identified difficulty obtaining timely physicians’ orders as one contributor to avoidable readmissions. Anecdotal accounts cited frequent instances when the home health nurse believed a patient would benefit from diuresis but instructions from the physician were delayed. In these cases, the patient’s symptoms often progressed, resulting in an Emergency Department visit and hospital readmission. Workgroup consensus was that this scenario was frequently observed and, with approximately 75% of eligible HF patients referred to home health, represented an important opportunity for improvement.7 The Workgroup further identified that a factor in these cases was timely adjustment of diuretic medications and that these adjustments might be conducted in the home via a standing order, including intravenous (IV) administration when warranted.
In response to this opportunity, the Workgroup developed the MaineHealth Home Diuretic Protocol (HDP), through which home health nurses respond to worsening HF symptoms using predetermined orders for diuretic administration to reduce delays, improve management of fluid retention, improve patient quality of life, and reduce readmissions.
The Workgroup, a quality-improvement forum that includes clinicians, managers, and quality-improvement professionals from across care settings, is led by the Director of the Maine Medical Center Heart Failure Program and a MaineHealth Senior Medical Director. In 2010, the Workgroup established the following objective: to demonstrate that diuretic therapy, including diuretics administered intravenously, can be delivered safely and effectively in the home health setting to address symptoms and signs of decompensation in HF patients using the HDP and standing orders.
Methods
The HDP was derived from existing standards of care for HF. From the patient’s perspective, the treatment they received was routine practice, with no special consent required and no risks beyond usual care. No patient was denied appropriate treatment. The institutional review board of the Maine Medical Center determined that this was a nonresearch project and not subject to its review.
The project was implemented in two hospitals in the health system (Maine Medical Center and Southern Maine Medical Center) and the primary home health agency serving those hospitals (Home Health Visiting Nurses). The Workgroup created a Home Diuretic Task Force to develop and implement a stepwise protocol. The task force was led by the Director of the Maine Medical Center Heart Failure Program and included a primary care physician, a home health nurse/telehealth coordinator, an inpatient HF nurse, a cardiology nurse practitioner, an emergency physician (the MaineHealth Senior Medical Director), a nurse clinical specialist, and the program manager.
A literature search uncovered five studies from Europe and the US between 1993 and 2010 related to diuretic protocols for HF. Four studies involved a clinic setting whereas one was designed with home diuretic administration by advanced practice nurses.8–12 These studies each provided evidence that diuretic protocols can be safe and effective outside the hospital setting despite comorbidities such as renal dysfunction. These studies also demonstrated cost-effectiveness, reduced hospital readmissions, and improved quality-of-life scores.
Starting with these examples, the Task Force developed an algorithm focused on patient safety and best practices for patient care. Hospitalized patients with advanced HF (New York Heart Association Class III/IV) were enrolled in the HDP in conjunction with an order for home nursing and telehealth monitoring. The HDP then remained dormant until the patient met the weight gain threshold, triggering activation of the standing orders. The HDP included monitoring of vital signs and laboratory test values, physician supervision, and a stepwise approach to diuretic therapy. Patient safety was of paramount importance, with physician consultation for abnormal laboratory test results and prompt referral to physician or hospital in any case of progressive symptoms, unstable vital signs, or worsening examination results (Table 1).
Table 1.
Overview of MaineHealth Home Diuretic Protocola
| Enrollment criteria | Heart failure admission Advanced heart failure (NYHA Class III/IV) Eligible for home health services Telehealth monitoring ordered |
|
| Protocol initiation criteria | Weight gain of 2 pounds overnight or 5 pounds in one week | |
| Day and criteria | Action | Follow-Up |
| 1 If initiation criteria met |
Double oral dose of diuretic Check serum electrolytes, renal function, magnesium Physical assessment |
Physician notified when:
Immediate physician or hospital referral if:
|
| 2 If patient above baseline weight |
Double oral dose of diuretic Administer metolazone Check serum electrolytes, renal function, magnesium Physical assessment |
|
| 3 If patient above baseline weight |
IV administration of diuretic, 1.5 times usual oral dose up to maximum Check serum electrolytes, renal function, magnesium Physical assessment |
|
| 4 If patient above baseline weight |
Immediate physician or hospital referral | |
The current version of the protocol itself, along with other supporting materials, can be found at www.mainehealth.org/home-diuretic.
IV = intravenous; NYHA = New York Heart Association.
Education and training to support implementation of the program included inpatient nurses, discharge planners, cardiologists, hospitalists, home health nurses, and primary care physicians. Presentations were conducted to inform and engage stakeholders and to solicit their feedback on the HDP and its implementation. Training of home health nurses included clinical updates on HF care and implementation of the HDP itself. Detailed information was provided to individual primary care physicians when their patients were enrolled in the HDP.
A primary purpose of evaluation was to demonstrate whether the HDP could be implemented safely. The next question to be answered was whether implementation was feasible without significant modification to existing resources, including staff and equipment. Evaluation was also designed to provide information on the success of HDP at meeting the needs of physicians, nurses, and patients and its impact on readmission rates.
Main outcome measures included the number of patients enrolled, HDP adherence, physical findings, lab values, patient disposition after each episode of care, and patient and clinician satisfaction. The home health telehealth coordinator compiled data provided by the nurses caring for the patient in the home. Vital signs data were recorded, including weight, temperature, blood pressure, pulse, respiratory rate, pulse oximetry, and laboratory values, including serum electrolytes, renal function, and magnesium. Data were also collected on patient symptoms, including dyspnea, orthopnea, rales, peripheral edema, early satiety, abdominal bloating, and chest pain. Actions taken by the home health nurse—direct clinician contact, laboratory testing, and medication administration, as well as patient disposition and outcome—were also recorded. Questionnaires to nurses, patients, and physicians solicited feedback regarding HDP ease of use, opportunities for improvement, patient’s perception of care, impact on patient safety, and responsiveness to patients’ needs. Blinded data were submitted for analysis only in aggregated form. No patient-identifying information was shared with program staff.
Results
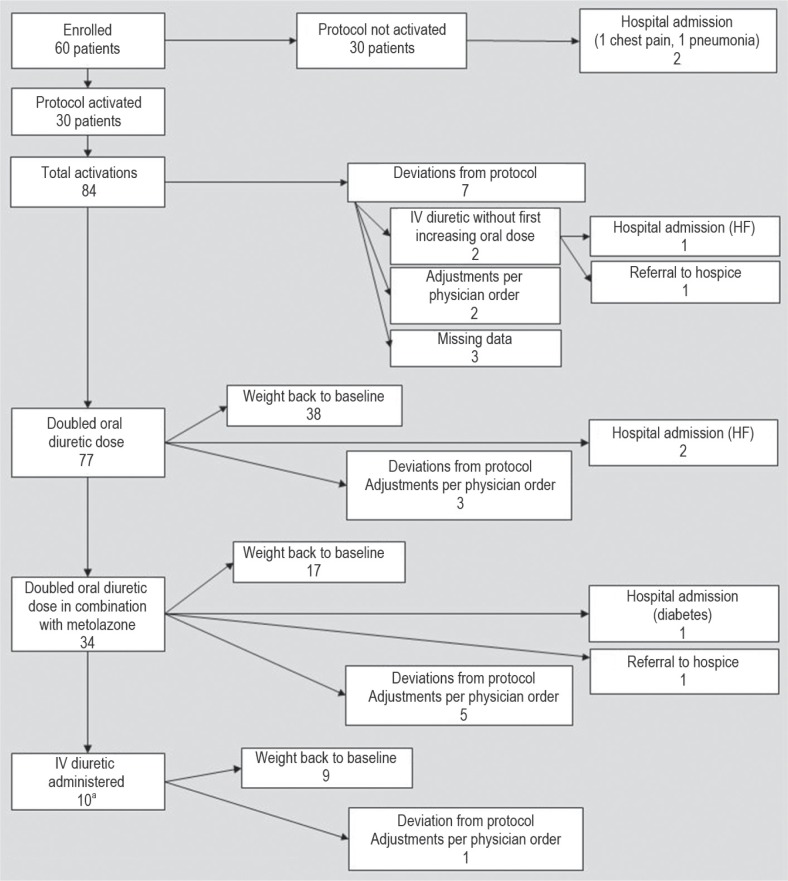
Sixty patients were enrolled in the HDP between November 2011 and January 2014. The HDP was activated 84 times for 30 of these patients, with multiple activations for 16 patients. In 16 (19%) of the activations, HDP deviations occurred, primarily in the form of physician orders to respond to changes in patients’ status, with 1 patient hospitalized and 1 patient referred to hospice. In 38 (45%) of the 84 activations, the patient’s weight returned to baseline with a doubling of their usual diuretic dose. Baseline weight was achieved 17 times (20%) after doubling the oral diuretic dose combined with metolazone. On 9 (11%) of these 84 activations, the patient’s weight returned to baseline after receiving IV diuretic administration. Overall, a return to baseline weight was achieved in 64 of the 84 HDP activations. Of the 68 activations for which the HDP was followed without deviation, a return to baseline weight occurred in 64 (94%), with only 6 hospitalizations. Two patients were referred for hospice care. A flowchart of these outcomes is provided in Figure 1.
Figure 1.
Actions and Outcomes on MaineHealth Home Diuretic Protocol.
aIV administered a total of 13 times within these 10 activations, with 3 patients receiving IV diuretic on 2 consecutive days.
IV diuretic also administered on two other activations as first step, as noted under “deviations” above. HF = heart failure; IV = intravenous.
The readmission rate was 10%, with a total of 6 readmissions for the 60 patients enrolled. This compares favorably with the readmission rate among MaineHealth HF patients receiving home health care services (25%) as well as with the Maine Medical Center readmission rate of 20.6% and the national readmission rate of 23% among Medicare patients with a discharge diagnosis of HF.3 Of the 6 readmissions, 3 were for HF, whereas the other 3 were for pneumonia, chest pain, and complications of diabetes.
One key safety question was whether complex patients with kidney disease could be managed safely under the HDP; therefore, renal function was monitored closely. Creatinine levels were abnormal at baseline in 27 cases. Of these, 13 abnormal creatinine levels worsened whereas 14 improved under the HDP. Abnormal lab values sometimes resulted in modifications of the algorithm to optimize therapeutic effect. These modifications, with close management of these patients to ensure safety, frequently resulted in effective diuretic adjustments and in some cases prompted the scheduling of next-day appointments with physicians, including with a nephrologist. No patient was admitted for renal failure while under the HDP.
The safety and feasibility of IV administration of diuretics in the home environment were questioned by several stakeholders. IV administration of diuretics was relatively infrequent (17%) and was performed by home health nurses without compromising patient safety or quality of care. Most patients did not progress to IV administration, with 67% of patients returning to baseline with oral treatment alone.
Nurses overwhelmingly reported that the HDP was easy to follow and that it helped them respond quickly to patient needs. Patients uniformly indicated that the nurse responded quickly and that the care they received helped them to stay out of the hospital. Only three physicians responded to the request for feedback and each of their responses bears mention here. One physician stated, “This protocol is a nightmare,” expressing concern about excessive phone exchanges regarding changes in the patient status. Further investigation indicated that some of these calls were necessary to safely manage complex patients, whereas other calls reflected a lack of experience with the HDP on the part of home health nurses. This led both to additional training of home health staff and to clarifying expectations among physicians. The message was reframed to stress that, rather than reducing communications about complex patients, this HDP allows physicians to partner with the home health nurse to more effectively manage these patients and to prevent Emergency Department visits and hospital admissions. A second physician expressed the opinion that the protocol improved the patient’s safety as a result of the increased attention inherent in the HDP. The third response declared the HDP “an outstanding program” and a very positive experience for this patient, contributing to keeping the patient out of the hospital.
Medication supply was challenging, with the plan for providing IV medications and supplies requiring several improvement cycles. IV medications and supplies were not readily available for patients through community or hospital pharmacies. A strategy involving a regional supplier of infusion services has proved successful, being cost-effective and reliable.
Discussion
Controversy continues regarding the true effectiveness of home monitoring in the management of HF. A Cochrane review13 in 2010 concluded that telemonitoring and structured telephone support do reduce all-cause mortality as well as rehospitalizations, whereas a randomized controlled trial inclusive of 1653 patients published that same year failed to demonstrate any such benefits.14 Desai15 similarly questioned the relationship between intensive home monitoring and outcomes, suggesting that emerging technologies may provide opportunities to remotely assess hemodynamic parameters and thereby improve disease management. Konstam,16 on the other hand, has argued that home monitoring should be considered an integral part of chronic disease management, particularly with HF, given its ever-increasing prevalence and costs.
The recognition that telemonitoring, if it is to be effective, has to be linked to timely intervention led to the development of the MaineHealth HDP. Although clearly a case series description rather than a randomized controlled trial, the HDP results to date suggest that home health nurses empowered with a structured protocol permitting a titrated increase in home diuretic dosages can safely and effectively manage homebound patients with advanced HF. MaineHealth’s integrated approach to improving the care of HF patients provided a structure within which to develop and implement the project. Committed engagement by the home health agency leadership was essential to its success, as was careful oversight by cardiologists and primary care physicians. Essential also was the clinical expertise and continued engagement of the members of the task force. The MaineHealth Heart Failure Program had the structure, staffing, and engagement of HF professionals from across the care continuum to coordinate and support this work well. Specially trained and experienced telehealth nurses played a central role in implementing the HDP.
The most significant limitation of this study is the lack of comparison data for the participant population. Since not all eligible patients were referred and no randomization process was used, it is likely that the discretion of referring physicians resulted in significant variation in the characteristics of patients recruited. Although historic data on the readmission rates for HF patients receiving home health services are available, these data do not differentiate those patients receiving telemonitoring services. Without comparative data for non-HDP patients, the relative impact of the HDP versus the impact of telemonitoring alone cannot be determined. Other limitations include the relatively small number of patients as well as the lack of racial diversity (all White).
From the beginning, patient safety has been the primary consideration and has not been compromised for any study participant. The daily physical examination, close monitoring of signs and symptoms, and laboratory results supported this goal. The effectiveness of the HDP was demonstrated by the return to baseline weight of most patients. The reduction in readmissions was better than anticipated, although no specific target was established for readmission reduction. Fewer patients than anticipated were recruited to the intervention during the study period. Patient recruitment may have been limited by reluctance among physicians to change practice, and by the introduction of a new electronic medical record system in the midst of the study period, creating challenges in the referral process.
The intervention was carried out with existing clinical staff, with no additional resources provided other than the support of quality-improvement staff. There were additional clinical inputs and associated costs, however, including telehealth equipment and home health telehealth coordinator and nursing time, and the extra time required by physicians to actively manage the most complex patients. Going forward, MaineHealth must develop a strategy to account for these additional costs and to allocate resources to scale and sustain the HDP, particularly as the cost savings that result from reduced rates of readmission will probably result in a decrease in revenue. Others considering such an intervention are advised to plan accordingly. This calculus will probably change as more organizations move toward “accountable care” and assume more financial responsibility and risk in providing care for the populations they serve.
Despite the challenges encountered and recognizing the relatively small number of patients enrolled, the MaineHealth HDP has demonstrated that diuretic therapy can be delivered safely and effectively in the home health setting and can improve patient experience outcomes while reducing readmissions. Given its apparent safety and effectiveness, MaineHealth plans to introduce the HDP in additional communities and to adapt it for use in other care settings, most notably skilled and long-term care. Recommendations for further study include using concurrent versus historic comparison data, as well as establishing a patient recruitment process that supports improved comparison of intervention versus control populations.
Acknowledgments
The authors would like to thank the members of the MaineHealth Heart Failure Workgroup and the MaineHealth Home Diuretic
Task Force for their diligence and endurance in pursuing improved outcomes for the patients we all serve as well as Neil Korsen, MD, for generously sharing his experience and guidance.
Mary Corrado, ELS, provided editorial assistance.
Footnotes
Disclosure Statement
Authors received no assistance in study design, data collection, data analysis, or manuscript preparation. The author(s) have no other potential conflicts of interest to disclose.
Practical Lessons
The most important practical lesson that can be given to nurses is to teach them what to observe—how to observe— what symptoms indicate improvement—what the reverse— which are of importance—which are of none—which are the evidence of neglect—and of what kind of neglect.
— Florence Nightingale, OM, RRC, 1820–1910, celebrated English social reformer and statistician, founder of modern nursing
References
- 1.Hall MJ, DeFrances CJ, Williams SN, Golosinskiy A, Schwartzman A. National health statistics reports, no. 29. National hospital discharge survey: 2007 summary [Internet] Hyattsville, MD: National Center for Health Statistics; 2010. Oct 26, [cited 2014 Apr 10] Available from: www.cdc.gov/nchs/data/nhsr/nhsr029.pdf. [PubMed] [Google Scholar]
- 2.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009 Apr;360(14):1418–28. doi: 10.1056/NEJMsa0803563. DOI: http://dx.doi.org/10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 3. Medicare.gov: hospital compare [Internet] Baltimore, MD: Centers for Medicare & Medicaid Services; [updated 2014 Jan 16 cited 2014 Jan 27]. Available from: www.medicare.gov/hospitalcompare. [Google Scholar]
- 4.ACC/AHA update guideline for management of heart failure [Internet] Dallas, TX: American Heart Association; 2013. Jun 5, [cited 2014 Apr 10]. Available from: http://newsroom.heart.org/news/acc-aha-update-guideline-for-management-of-heart-failure. [Google Scholar]
- 5.Ross JS, Chen J, Lin Z, et al. Recent national trends in readmission rates after heart failure hospitalization. Circ Heart Fail. 2010 Jan;3(1):97–103. doi: 10.1161/CIRCHEARTFAILURE.109.885210. DOI: http://dx.doi.org/10.1161/CIRCHEARTFAILURE.109.885210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Butler J, Kalogeropoulos A. Worsening heart failure hospitalization epidemic we do not know how to prevent and we do not know how to treat! J Am Coll Cardiol. 2008 Aug 5;52(6):435–7. doi: 10.1016/j.jacc.2008.04.037. DOI: http://dx.doi.org/10.1016/j.jacc.2008.04.037. [DOI] [PubMed] [Google Scholar]
- 7.MaineHealth Heart Failure database, calendar year 2010. Portland, ME: Maine Health; [Google Scholar]
- 8.Ryder M, Murphy NF, McCaffrey D, O’Loughlin C, Ledwidge M, McDonald K. Outpatient intravenous diuretic therapy; potential for marked reduction in hospitalisations for acute decompensated heart failure. Eur J Heart Fail. 2008 Mar;10(3):267–72. doi: 10.1016/j.ejheart.2008.01.003. DOI: http://dx.doi.org/10.1016/j.ejheart.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 9.Durango LF, Katz SD, Hung-Kei L, Wencker D. Abstract 1891: continuous furosemide infusion is safe and effective in outpatient treatment of refractory heart failure [meeting abstract, Internet] Circulation. 2006 [cited 2014 Apr 10];114:II_375-II_376. Available from: http://circ.ahajournals.org/cgi/content/meeting_abstract/114/18_MeetingAbstracts/II_375-d. [Google Scholar]
- 10.Rai M, Zaeem F, Giedrimiene D, et al. Effectiveness of aggressive heart failure management despite cardiorenal syndrome in the outpatient setting: symptom improvement and prevention of readmission [abstract] J Am Coll Cardiol. 2010 Mar 9;55(10 Suppl):A33, E315. DOI: http://dx.doi.org/10.1016/S0735-1097(10)60316-6. [Google Scholar]
- 11.van de Wetering H, de Zwaan M, Wienke A, van ‘t Hof AWJ. Feasibility and effects of home based intravenous diuretic therapy in NYHA class III/IV CHF patients [Internet]. Proceedings of ESC 2009 Barcelona; 2009 Sep 2; Barcelona, Spain. Zwolle, Netherlands. Isala kliniekin; 2009. [cited 2014 Apr 10]. Available from: spo.escardio.org/eslides/view.aspx?eevtid=33&id=5006. [Google Scholar]
- 12.Mueller TM, Vuckovic KM, Knox DA, Williams RE. Telemanagement of heart failure: a diuretic treatment algorithm for advanced practice nurses. Heart Lung. 2002 Sep-Oct;31(5):340–7. doi: 10.1067/mhl.2002.126048. DOI: http://dx.doi.org/10.1067/mhl.2002.126048. [DOI] [PubMed] [Google Scholar]
- 13.Inglis SC, Clark RA, McAlister FA, et al. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev. 2010 Aug 4;(8):CD007228. doi: 10.1002/14651858.CD007228.pub2. DOI: http://dx.doi.org/10.1002/14651858.CD007228.pub2. [DOI] [PubMed] [Google Scholar]
- 14.Chaudhry SI, Mattera JA, Curtis JP, et al. Telemonitoring in patients with heart failure. N Engl J Med. 2010 Dec 9;363(24):2301–9. doi: 10.1056/NEJMoa1010029. DOI: http://dx.doi.org/10.1056/NEJMoa1010029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Desai AS. Home monitoring heart failure care does not improve patient outcomes: looking beyond telephone-based disease management. Circulation. 2012 Feb 14;125(6):828–36. doi: 10.1161/CIRCULATIONAHA.111.031179. DOI: http://dx.doi.org/10.1161/CIRCULATIONAHA.111.031179. [DOI] [PubMed] [Google Scholar]
- 16.Konstam MA. Home monitoring should be the central element in an effective program of heart failure disease management. Circulation. 2012 Feb 14;125(6):820–7. doi: 10.1161/CIRCULATIONAHA.111.031161. DOI: http://dx.doi.org/10.1161/CIRCULATIONAHA.111.031161. [DOI] [PubMed] [Google Scholar]