Abstract
Surgical management of ovarian lesions vary considerably depending on the nature of the lesion. As the preoperative imaging and serum tumor marker levels are of limited value in the proper categorization of ovarian lesions, intraoperative pathological assessment is commonly requested for a primary diagnosis. Aim of the study is to assess the accuracy of the frozen section in the diagnosis of ovarian masses in our center and to analyze the causes of diagnostic discrepancies. In this retrospective study, frozen section diagnosis of 233 cases of ovarian masses was compared with the permanent section diagnosis. The overall accuracy of frozen section was 91.85 %. The sensitivity of frozen section diagnosis for benign, borderline and malignant tumors was 99.2, 88.46 and 82.95 % respectively. The corresponding specificity was 96.5, 93.23 and 99.3 %. There were 19 discordant cases including 18 false negative cases and one false positive case. Frozen section is an important diagnostic tool to determine the nature of ovarian masses. Careful macroscopic examination, evaluation of multiple sections along with clinical and radiological findings helps to reduce false positive and false negative results. Frozen section examination has limitations especially in cases of borderline tumors. This modality is most effective when the pathologist and surgeon are aware of the advantages and limitations.
Keywords: Frozen section, Intraoperative assessment, Ovarian neoplasm
Introduction
Ovarian tumors constitute a heterogeneous group of lesions which include benign, borderline and malignant tumors [1]. A diagnostic tool which helps to identify various ovarian lesions with high degree of accuracy will help the surgeon to choose appropriate operating procedure [2, 3]. Preoperative diagnostic modalities include serum tumor marker level estimation and imaging. The serum tumor marker- CA 125 is not specific. CA 125 level can be normal in early stages of ovarian carcinoma and can be raised in nonneoplastic conditions like endometriosis and pelvic inflammatory disease [4]. Imaging also has limitations in the accurate diagnosis of ovarian masses especially in large heterogeneous lesions. As the preoperative diagnostic techniques are of limited value in identifying the nature of the ovarian masses, intraoperative frozen section examination is crucial in giving rapid histological diagnosis thus helping the surgeon to plan appropriate surgical management. Frozen section examination is having some limitations especially in cases of borderline tumors.
Materials and Methods
Two hundred and thirty three cases of ovarian masses in which intraoperative frozen section examination was done from 2009 to 2012 were included in this study. The following parameters were noted-age of the patient, size of the tumor, unilateral/bilateral, solid/cystic/solid and cystic. After gross examination, two to five sections were taken depending on the size and heterogeneity of the lesions. Sections of 4–5 microns were taken and rapid hematoxylin and eosin staining was done. After the frozen section analysis tissues were put in formalin and routine processing was done. The results of frozen section diagnosis were compared with the permanent section diagnosis. The lesions included nonneoplastic and neoplastic entities. The neoplastic lesions were categorized into benign, borderline and malignant. The neoplastic lesions included epithelial tumors, germ cell tumors, sex cord stromal tumors and metastatic tumors. The cases which underwent torsion with extensive hemorrhage and infarction were excluded from the study. Overall accuracy was defined as the percentage of concordance between frozen and final diagnosis i.e., total number of cases in which there is concordance between frozen section diagnosis and final tissue diagnosis divided by the total number of patients with ovarian masses expressed as percentage. The sensitivity, specificity, positive predictive value and negative predictive value in diagnosing each category were calculated. The cases with diagnostic discrepancies were reviewed and the possible causes of diagnostic errors analyzed.
Results
During the study period of 2009 to 2012, frozen section examination was done in 237 cases of ovarian lesions. The diagnosis was deferred in four cases due to extensive hemorrhage and infarction. These four cases were excluded from the study. Of the remaining 233 cases, the frozen section diagnosis was concordant in 214 cases and discordant in 19 cases. Overall accuracy was 91.85 % (214/233).
The age group ranged from 14 to 86 years and the mean age was 46 years. The mean size of the tumors was 14 cm and ranged from 3 to 36 cm. In 29 cases, the lesions were bilateral.
The distribution of various ovarian lesions according to permanent section result were as follows–27 nonneoplastic lesions, 153 epithelial tumors, 16 sex cord stromal tumors, 30 germ cell tumors and seven metastatic tumors (Table 1). Serous tumors were the most frequent epithelial tumor and constituted 45.1 % of all epithelial tumors. There were 119 benign cases, 26 borderline cases and 88 malignant cases (Table 2).
Table 1.
Histological types according to permanent section results
| Histopathology Diagnosis | Number | Percentage |
|---|---|---|
| Nonneoplastic lesions | 27 | 11.58 |
| Epithelial tumors | 153 | 65.67 |
| Sex cord stromal tumors | 16 | 6.9 |
| Germ cell tumors | 30 | 12.87 |
| Metastasis | 7 | 3 |
Table 2.
Comparison between frozen section diagnoses and final diagnoses
| Frozen Diagnosis | Histopathology diagnosis | |||
|---|---|---|---|---|
| Benign | Borderline | Malignant | Total | |
| Benign | 118 | 3 | 1 | 122 |
| Borderline | 0 | 23 | 14 | 37 |
| Malignant | 1 | 0 | 73 | 74 |
| Total | 119 | 26 | 88 | 233 |
One hundred twenty two cases were diagnosed as benign by frozen section. In 118 cases the diagnoses were concordant with the final diagnosis. There were four discordant cases in which the final histopathology showed borderline serous tumor in two cases, borderline mucinous tumor in one case and low grade serous adenocarcinoma with benign and borderline areas in one case.
A diagnosis of borderline ovarian tumor was made in frozen section analysis in 37 cases. 23 cases were concordant with the final histopathology whereas 14 cases were reclassified as malignant. The borderline tumors were a major cause of diagnostic discrepancy in this study.
Seventy four cases were classified as malignant by frozen section examination. There was one false positive case (Table 2).
The sensitivity, specificity, positive predictive value and negative predictive value of each category were calculated (Table 3).
Table 3.
Sensitivity, Specificity, PPVa and NPVb of Frozen section diagnoses
| Benign | Borderline | Malignant | |
|---|---|---|---|
| Sensitivity | 99.2 % | 88.46 % | 82.95 % |
| Specificity | 96.5 % | 93.23 % | 99.3 % |
| PPVa | 96.72 % | 62.16 % | 98.65 % |
| NPVb | 99.1 % | 98.47 % | 90.57 % |
a PPV positive predictive value
b NPV negative predictive value
Discussion
As the preoperative diagnostic modalities like tumor marker values and imaging are not completely specific, an accurate frozen section result is crucial in planning appropriate surgical management. Overdiagnosis during frozen section examination can lead to unnecessary widening of surgical field and thereby increasing morbidity and mortality. Underdiagnosis can lead to second surgery and possible tumor spread [5].
A number of nonneoplastic conditions can mimic malignancy. The nonneoplastic lesions identified during frozen section examination in this study included endometriotic cyst, corpus leuteal cyst, granuloma and follicular cyst. All these diagnoses were confirmed on final histopathology. There were four cases of granulomatous lesions which mimicked malignancy clinically and radiologically. Two cases showed extensive lesions. Computerized tomography showed complex cystic ovarian masses with deposits in the whole of peritoneum, surface of intestine, and liver. CA 125 level was raised in these cases to more than 1,000 units/ml. Peroperative findings were also in favor of an advanced stage of ovarian carcinoma with the whole of peritoneum, liver, bowel mesentery, surface of intestine and subdiaphragmatic area studded with deposits. Frozen section examination showed multiple granulomas composed of epithelioid histiocytes and giant cells (Fig. 1). Areas of caseation necrosis suggested tuberculous granuloma. In these cases unnecessary widening of surgical field was avoided due to the accurate intraoperative diagnosis.
Fig. 1.
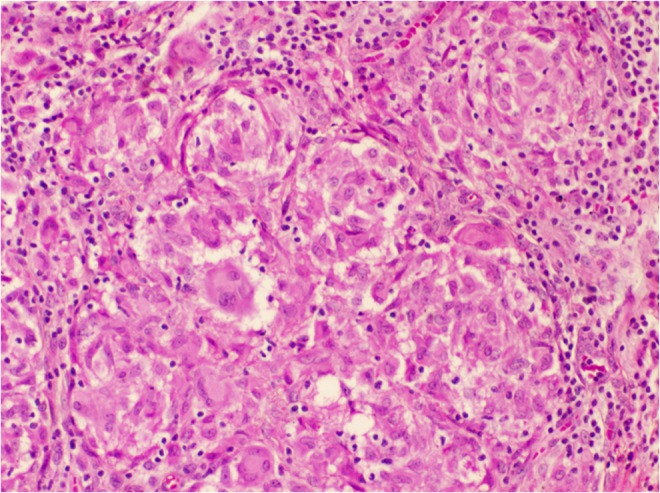
Microscopy showing granuloma composed of epithelioid histiocytes and giant cells. (H&E X400)
The benign epithelial tumors in this study included serous cystadenoma, mucinous cystadenoma, serous cystadenofibroma, mixed tumors- combination of serous cystadenofibroma and mucinous tumor, mucinous cystadenoma and Brenner tumor and mucinous cystadenoma and mature teratoma. Sex cord stromal tumors-fibrothecoma and fibroma were accurately identified during frozen section examination. The diagnosis of mature cystic teratoma and struma ovarii also helped to limit the extent of surgical procedure.
Frozen section examination can diagnose the benign conditions with a high degree of accuracy. Out of 122 cases reported as benign on frozen section analysis, diagnostic discrepancy occurred in four cases. In three cases there were focal borderline areas in addition to the predominant benign component. One case showed a combination of benign, borderline and focal low grade invasive carcinoma. The sensitivity, specificity, positive predictive value and negative predictive value of frozen section in diagnosing benign conditions in this study were 99.2, 96.5, 96.72 and 99.1 % respectively.
Borderline ovarian tumors constitute 10–20 % of all ovarian malignancies [6]. The borderline ovarian tumors usually occur in younger age group and the long term prognosis is significantly better [7, 8]. The accurate diagnosis is critical to avoid overtreatment or undertreatment. The diagnosis of borderline ovarian tumor in older age group will lead the surgeon to do hysterectomy, bilateral salpingo-opherectomy and surgical staging. With the same diagnosis in reproductive age group, where the incidence of borderline tumors are high, the surgical management is fertility conserving surgery- unilateral salpingo-oopherectomy or even cystectomy with surgical staging [9].
Borderline ovarian tumors were a major cause of diagnostic discrepancy in this study. Although there are well defined criteria for the diagnosis of borderline tumors, the diagnosis by frozen section examination is relatively difficult. Thirty seven cases were diagnosed as borderline tumors by frozen section examination. In 23 cases the diagnosis was confirmed on final histopathology. Fourteen cases were reclassified as malignant on final histopathology. The sensitivity, specificity, positive predictive value and negative predictive value of frozen section in diagnosing borderline conditions in this study were 88.46, 93.23, 62.16 and 98.47 % respectively.
Diagnostic discrepancy was greater in cases of serous tumors with a borderline diagnosis on frozen section. Among the eight false negative serous tumors, five showed borderline serous tumor with foci of invasive carcinoma. This highlights a major limitation of frozen section examination. Around 20 % of serous tumors may contain small foci of low grade serous carcinoma which may not be picked up in frozen section examination. The small foci of carcinoma could escape the limited sampling during frozen section examination. KK Shih et al. in their study noted that if micropapillary features are present on frozen section analysis, there is greater chance of reclassification on final histopathology [10]. In our series, there were three cases of serous carcinoma with micropapillary features of which one was diagnosed as carcinoma and the other two were diagnosed as borderline during frozen section examination.
Of the 19 cases which were diagnosed as mucinous borderline tumors, six turned out to be mucinous carcinoma on final histopathology. Mucinous borderline tumors are notorious for diagnostic discrepancy because of the large size of the tumors and because of the heterogeneous histology with benign, borderline and malignant areas present in the same lesion [11, 12]. The gross appearance of borderline mucinous tumors can be quite alarming. The large size, intricately honeycomb appearance or solid areas composed of multiple tiny cysts can lead to the gross diagnosis of a carcinoma [13, 14, 5].
Most of the well differentiated mucinous carcinomas have a bland histological appearance which prevents the diagnosis of malignancy. In the present study, three discrepant cases were diagnosed as low grade mucinous carcinoma on final histopathology. The low grade nuclear features with no obvious destructive stromal invasion prevented from giving a malignant diagnosis during frozen section examination. In their study, Shih et al. found intestinal type of mucinous tumors are prone to frozen section misdiagnosis and they recommend the term ‘borderline on representative’ and to inform the surgeon that some of these lesions may be reclassified as carcinoma on final diagnosis [10].
Borderline mucinous tumors may contain small foci of invasive carcinoma. The paraffin section has the advantage of examining multiple sections from different areas, which will lead to the accurate diagnosis in a heterogeneous lesion. During frozen section examination it is nearly impossible to sample large masses extensively. In two discrepant cases in the present study, there were predominant mucinous borderline areas with focal areas of invasion which were missed during frozen section. One case of teratoma showed foci of atypical mucinous epithelial proliferation during frozen section and the diagnosis of a combined tumor-mature teratoma and borderline mucinous tumor was offered. Multiple paraffin embedded sections revealed focus of adenocarcinoma arising in a mature cystic teratoma.
Seventy four cases were diagnosed as malignant during frozen section examination. 60 were diagnosed as epithelial malignancies which included serous carcinoma, mucinous carcinoma, clear cell carcinoma, endometrioid carcinoma, poorly differentiated carcinoma and metastasis. In most cases the final diagnosis of individual types of carcinoma was concordant with the frozen section diagnosis. There were seven cases of dysgerminoma and two cases of immature teratoma which were accurately diagnosed by frozen section examination. In this study, frozen section examination showed a sensitivity of 82.95 %, specificity of 99.3 %, positive predictive value of 98.65 % and negative predictive value of 90.57 % in diagnosing malignant ovarian tumors.
There was one false positive case where a 56 year old lady, with a past history of unilateral salpingoopherectomy for borderline ovarian tumor eight years back, presented with a large ovarian mass in the contralateral ovary. Gross examination showed predominantly solid areas with focal cystic change. Frozen section examination showed cells arranged in glandular pattern with focal increased cellularity and minimal atypia. The stroma showed focal fibrosis (Fig. 2). With these findings, a diagnosis of low grade adenocarcinoma was offered. But the final histopathology showed struma ovarii with foci of increased cellularity, nuclear atypia and degenerative changes including fibrosis and cystic change.
Fig. 2.
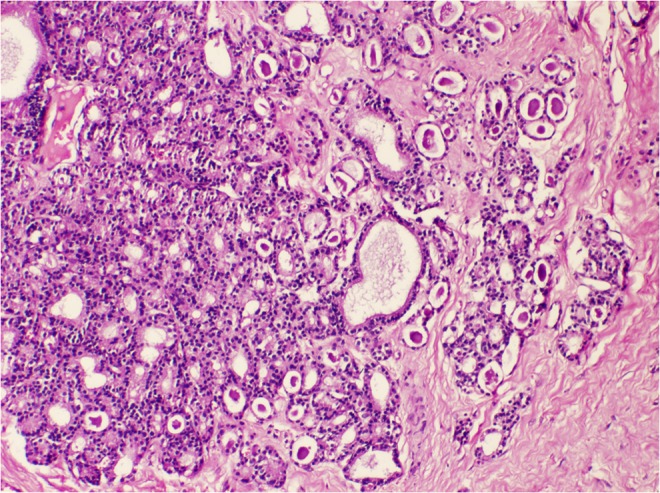
Struma ovarii interpreted as low grade adenocarcinoma intraoperatively. Frozen section showed closely packed glands in a fibrotic stroma. (H&E X200)
There were seven cases of metastasis. The primary sites were stomach, breast, appendix and large intestine. Four cases were diagnosed as metastasis by frozen section examination. Bilateral solid ovarian tumors, bilateral mucinous tumors, multinodular growth pattern involving the cortex and malignant cells haphazardly arranged as glands, small nests and singly scattered in a desmoplastic stroma suggested a metastatic nature of the lesions. The histological features were correlated with the clinical history, imaging findings and tumor marker values. The remaining three cases were diagnosed as adenocarcinoma on frozen. Examination of multiple sections and immunohistochemistry helped in the identification of metastatic nature of the tumors on final diagnosis.
Nineteen cases in this study showed diagnostic discrepancy between frozen section diagnosis and final diagnosis. The major cause of misdiagnosis, in 12 cases, was the heterogeneity of lesions where the same tumor contained benign, borderline and/malignant areas. In these cases the paraffin section has the advantage of examining multiple sections. In a heterogeneous lesion it is recommended to take multiple sections from different areas during frozen section and inform the surgeon about the possibility of reclassifying the lesion during final diagnosis. In six cases the diagnostic error was due to interpretative error where the low grade bland nuclear features prevented a straightforward diagnosis of invasive carcinoma. In such cases frozen section diagnosis of ‘atypically proliferating tumor, low grade malignancy cannot be excluded’ will be more appropriate in guiding the surgeon to decide on the surgical management.
Literature search shows the overall accuracy of frozen section in the diagnosis of ovarian tumors range from 86 to 97 % [8, 11, 16]. In this study, overall accuracy of frozen section diagnosis was 91.85 %. Geomini et al. done a meta-analysis of 18 studies and found that the sensitivity of frozen section in diagnosing ovarian lesions ranged from 65 to 97 % for benign and from 71 to 100 % for malignant lesions. They also found specificity ranged from 97 to 100 % for benign and from 98.3 to 100 % for malignant tumors [16]. In the current study the sensitivity in diagnosing benign lesions was 99.2 % and that for malignant lesions was 82.95 %. The specificity was 96.5 and 99.3 % in diagnosing benign and malignant lesions respectively. Tempfer et al. reviewed three large studies investigating the accuracy of frozen section examination in diagnosing borderline ovarian tumors and found an overall sensitivity of 71.1 % and positive predictive value of 84.3 % [5]. In the present study the sensitivity and positive predictive value of frozen section analysis in diagnosing borderline tumors was 88.46 and 62.16 % respectively. Our study showed a false positive rate of 0.4 % and false negative rate of 7.7 %. Literature search shows false positive rates ranging from 2.2 to 10.7 % and false negative rates ranging from 5.4 to 29.3 % [17, 18].
The major limitations of frozen section examination are limited number of sections that can be examined, thicker sections compared to permanent sections and freezing artifacts that obscure the finer details. The diagnostic errors can be due to sampling error, misinterpretation or suboptimal slide preparation. In the present study the major causes of diagnostic discrepancy were due to heterogeneous nature of the lesions (sampling error) and low grade nuclear features (interpretive error).
Diagnostic accuracy rate for frozen section analysis is high for benign and malignant ovarian tumors, but remain relatively low for borderline ovarian tumors. The possible predictive factors affecting false positive or false negative diagnosis should carefully be taken into consideration to reduce the diagnostic discrepancies. Regular reevaluation regarding the disagreement between frozen section diagnosis and final paraffin section diagnosis should be conducted as a part of quality assurance.
References
- 1.Tavassoli FA, Devilee P, editors. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the breast and Female Genital organs. Lyon: IARC Press; 2003. [Google Scholar]
- 2.Malipatil R, Crasta JA. How Accurate is Intraoperative Frozen Section in the Diagnosis of Ovarian Tumors? J Obstet Gynaecol Res. 2013;39:710–713. doi: 10.1111/j.1447-0756.2012.02039.x. [DOI] [PubMed] [Google Scholar]
- 3.Baker P, Oliva EA. Practical Approach to Intraoperative Consultation in Gynecological Pathology. Int J Gynecol Pathol. 2008;27:353–365. doi: 10.1097/PGP.0b013e31815c24fe. [DOI] [PubMed] [Google Scholar]
- 4.Wakahara F, Kikkawa F, Nawa A, Tamakoshi K, Ino K, Maeda O, Kawai M, Mizutani S. Diagnostic Efficacy of Tumor Markers, Sonography and Intraoperative Frozen Section for Ovarian Tumors. Gynecol Obstet Invest. 2001;52:147–152. doi: 10.1159/000052963. [DOI] [PubMed] [Google Scholar]
- 5.Tempfer CB, Polterauer S, Bentz EK, Reinthaller A, Hefler LA. Accuracy of Intraoperative Frozen Section Analysis in Borderline Tumors of the Ovary: a Retrospective Analysis of 96 Cases and Review of the Literature. Gynecol Oncol. 2007;107:248–252. doi: 10.1016/j.ygyno.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 6.Trope CG, Kristensen G, Makar A. Surgery of Borderline Tumor of the Ovary. Semin Surg Oncol. 2000;19:69–75. doi: 10.1002/1098-2388(200007/08)19:1<69::AID-SSU11>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 7.Skírnisdóttir I, Garmo H, Wilander E, Holmberg L. Borderline Ovarian Tumors in Sweden 1960–2005: Trends in Incidence and age at Diagnosis Compared to Ovarian Cancer. Int J Cancer. 2008;123:1897–1901. doi: 10.1002/ijc.23724. [DOI] [PubMed] [Google Scholar]
- 8.Medeiros LR, Rosa DD, Edelweiss MI, Stein AT, Bozzetti MC, Zelmanowicz A, et al. Accuracy of Frozen-Section Analysis in the Diagnosis of Ovarian Tumors: a Systematic Quantitative Review. Int J Gynecol Cancer. 2005;15:192–202. doi: 10.1111/j.1525-1438.2005.15203.x. [DOI] [PubMed] [Google Scholar]
- 9.Ilvan S, Ramazanoglu R, Ulker Akyildiz E, Calay Z, Bese T, Oruc N. The Accuracy of Frozen Section (Intraoperative Consultation) in the Diagnosis of Ovarian Masses. Gynecol Oncol. 2005;97:395–399. doi: 10.1016/j.ygyno.2005.01.037. [DOI] [PubMed] [Google Scholar]
- 10.Shih KK, Garg K, Soslow RA, Chi DS, Abu-Rustum NR, Barakat RR. Accuracy of Frozen Section Diagnosis of Ovarian Borderline Tumor. Gynecol Oncol. 2011;123:517–521. doi: 10.1016/j.ygyno.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 11.Rakhshan A, Zham H, Kazempour M. Accuracy of Frozen Section Diagnosis in Ovarian Masses: Experience at a Tertiary Oncology Center. Arch Gynecol Obstet. 2009;280:223–228. doi: 10.1007/s00404-008-0899-6. [DOI] [PubMed] [Google Scholar]
- 12.Tangjitgamol S, Jesadapatrakul S, Manusirivithaya S, Sheanakul C. Accuracy of Frozen Section in Diagnosis of Ovarian Mass. Int J Gynecol Cancer. 2004;14:212–219. doi: 10.1111/j.1048-891X.2004.014202.x. [DOI] [PubMed] [Google Scholar]
- 13.Stewart CJ, Brennan BA, Hammond IG, Leung YC, McCartney AJ. Intraoperative assessment of ovarian tumors: a 5-year review with assessment of discrepant diagnostic cases. Int J Gynecol Pathol. 2006;25:216–222. doi: 10.1097/01.pgp.0000215295.45738.ed. [DOI] [PubMed] [Google Scholar]
- 14.Kurman RJ, Ellenson LH, Ronett BM. Blaustein’s Pathology of the Female Genital Tract. 6. New York: Springer; 2011. [Google Scholar]
- 15.Yarandi F, Eftekhar Z, Izadi-Mood N, Shojaei H. Accuracy of Intraoperative Frozen Section in the Diagnosis of Ovarian Tumors. Aust N Z J Obstet Gynaecol. 2008;48:438–441. doi: 10.1111/j.1479-828X.2008.00873.x. [DOI] [PubMed] [Google Scholar]
- 16.Geomini P, Bremer G, Kruitwagen R, Mol BW. Diagnostic Accuracy of Frozen Section Diagnosis of Adenexal Mass: a Meta-Analysis. Gynecol Oncol. 2005;96:1–9. doi: 10.1016/j.ygyno.2004.09.042. [DOI] [PubMed] [Google Scholar]
- 17.Gol M, Baloglu A, Yigit S, Dogan M, Aydin C, Yensel U. Accuracy of Frozen Section Diagnosis in Ovarian Tumors: is there a Change in the Course of Time? Int J Gynecol Cancer. 2003;13:593–597. doi: 10.1046/j.1525-1438.2003.13389.x. [DOI] [PubMed] [Google Scholar]
- 18.Houck K, Nikrui N, Duska L, Chang Y, Fuller AF, Bell D, et al. Borderline Tumors of the Ovary: Correlation of Frozen and Permanent Histopathologic Diagnosis. Obstet Gynecol. 2000;95:839–843. doi: 10.1016/S0029-7844(99)00656-0. [DOI] [PubMed] [Google Scholar]


