Abstract
Background:
Meniscal repair and preservation are the goal, when possible, of the treatment of meniscal injury. Current research on second-generation all-inside repair systems has been limited to a maximum of three years of follow-up. The purpose of this study was to evaluate the mid-term clinical success (at more than five years) of meniscal repair performed with a second-generation all-inside repair device, both as an isolated procedure and with a concomitant anterior cruciate ligament (ACL) reconstruction.
Methods:
This is a retrospective review of patients who underwent meniscal repair with use of the all-inside FAST-FIX Meniscal Repair System (Smith & Nephew Arthroscopy, Andover, Massachusetts) from December 1999 to January 2007. Eighty-three meniscal repairs (in eighty-one patients) were identified, and follow-up data were obtained for seventy-five (90%). Twenty-six (35%) of the meniscal repairs were performed as isolated procedures. Clinical failure was defined as repeat surgical intervention involving resection or revision repair. Clinical outcomes were also assessed with the Knee injury and Osteoarthritis Outcome Score (KOOS), International Knee Documentation Committee (IKDC) score, and the Marx activity score.
Results:
The minimum duration of follow-up was five years (average, seven years). Twelve patients (16%) had failure of the meniscal repair, at an average of forty-seven months (range, fifteen to ninety-five months). The data did not offer enough statistical evidence, at alpha = 0.05, to establish a difference in average patient age, patient sex, or number of sutures utilized between successful repairs and failures. There was no difference in the failure rate between isolated repairs (12%; 95% confidence interval [CI]: −0.76% to 23.76%) and those performed with concurrent ACL reconstruction (18%; 95% CI: 7.47% to 29.13%), and the average time to failure was similar between these two groups (48.1 months versus 46.6 months, p = 0.939). Postoperative KOOS and IKDC outcome scores were also similar between the groups.
Conclusions:
This report of mid-term follow-up results of primary second-generation all-inside meniscal repair demonstrates its effectiveness both as an isolated procedure and when it is performed with concurrent ACL reconstruction. After a minimum of five years of follow-up, 84% of the patients continued to demonstrate successful repair. Treatment success was further supported by favorable results on patient-based outcome measures.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
The menisci play an important role in the health of the knee. They function to improve joint congruency, add stability, and evenly distribute contact forces across the joint. Injury to the meniscus is common, both in isolation and in association with concomitant ligament injury, making arthroscopic meniscectomy the most frequently performed orthopaedic procedure in the United States1. Given the chondroprotective properties of the meniscus, meniscal preservation and repair are attempted when possible2,3.
Several meniscal repair techniques, including open, outside-in, inside-out, and all-inside, have been described4,5. The all-inside meniscal repair is the most recently introduced of these techniques and is frequently utilized given its ease of use, minimal invasiveness, and reduced risk of nerve injury or irritation6. Early all-inside repair designs were noted to be at risk for complications, including damage to articular cartilage by implant prominence and migration7-9. Second-generation devices were designed to more closely resemble inside-out suture techniques and improve outcomes with less risk and fewer complications. Short-term follow-up of second-generation all-inside meniscal repair systems have demonstrated excellent outcomes, with successful repair in 80% to 96% of patients10-12; however, the mid-term success (at more than five years) has not been described, to our knowledge. Additional limitations of available studies include mixed cohorts of isolated repairs and those combined with ligament reconstruction. It is important to distinguish between these two cohorts given the data suggesting improved healing with concomitant ligament reconstruction6.
We evaluated the mid-term clinical success of a second-generation all-inside meniscal repair system used both for isolated meniscal repairs and for repairs with concurrent anterior cruciate ligament (ACL) reconstruction. Our hypothesis was that the use of second-generation devices would decrease mid-term failure rates compared with those of first-generation devices and equal those of inside-out, outside-in, and open repair techniques.
Materials and Methods
Study Overview
From December 1999 to January 2007, eighty-one consecutive patients underwent a total of eighty-three meniscal repairs with the all-inside FAST-FIX Meniscal Repair System (Smith & Nephew Arthroscopy, Andover, Massachusetts). Isolated meniscal repairs were identified through a search of the surgical billing records of the senior author (R.W.W.) . A query of an established prospective database (Multicenter Orthopaedic Outcomes Network [MOON]) was utilized to identify patients, treated by the senior author, with combined meniscal repair and ACL reconstruction. Patients with a prior repair of the affected meniscus were excluded. Patient demographics and intraoperative data, including tear location, morphology, and number of sutures utilized for the repair, were obtained via a retrospective chart review and prospective database review.
Failure of meniscal repair was defined as repeat surgical intervention involving revision, repair, or resection of the affected meniscus. For all patients, failure was also determined via telephone interview and patient-based outcome questionnaires. For the patients who underwent ACL reconstruction, this information was part of the MOON database. At the time of follow-up, patient-rated outcome scores, including the Knee injury and Osteoarthritis Outcome Score (KOOS), International Knee Documentation Committee (IKDC) score, and Marx activity score, were also obtained. The final cohort included seventy-five meniscal repairs performed in seventy-three patients. Twenty-six repairs were isolated and forty-nine were performed with concurrent ACL reconstruction. Thirty-seven patients were males and thirty-six were females, and their average age was 26.8 years (range, 14.1 to 53.5 years). Follow-up regarding meniscal failure was obtained for 90% of the patients, and 88% of the patients completed the postoperative patient-rated outcome questionnaires. The average duration of follow-up was seven years (range, 5.0 to 12.5 years).
Operative Technique
Every meniscal tear was assessed for stability and repairability. The decision to repair a given tear was based on the characteristics of the tear and was independent of the presence of a concomitant ACL reconstruction. Menisci were repaired if they both demonstrated instability and had a tear in a region with sufficient vascularity to support healing. These tears were all classified as either longitudinal or bucket-handle in orientation and involved either the red/red or red/white meniscal zones. All meniscal repairs were performed arthroscopically by a single experienced sports medicine fellowship-trained surgeon utilizing the FAST-FIX all-inside repair device (Smith & Nephew Endoscopy) according to the manufacturer’s described technique13. Sutures were placed until the desired stability was achieved. Twenty-six meniscal repairs were isolated, and forty-nine were performed in combination with ACL reconstruction. Two patients, both of whom had ACL reconstruction, underwent medial and lateral meniscal repair. The medial meniscus was repaired in fifty knees (sixteen treated with isolated repair and thirty-four, with concurrent ACL reconstruction) and the lateral meniscus was repaired in twenty-five (ten treated with isolated repair and fifteen, with concurrent ACL reconstruction). The postoperative protocol for isolated meniscal repairs included weight-bearing as tolerated in a knee immobilizer for six weeks. Patients treated with combined meniscal repair and ACL reconstruction were allowed weight-bearing as tolerated without bracing. Straight-line running was started at three months, and return to sports was allowed at six months.
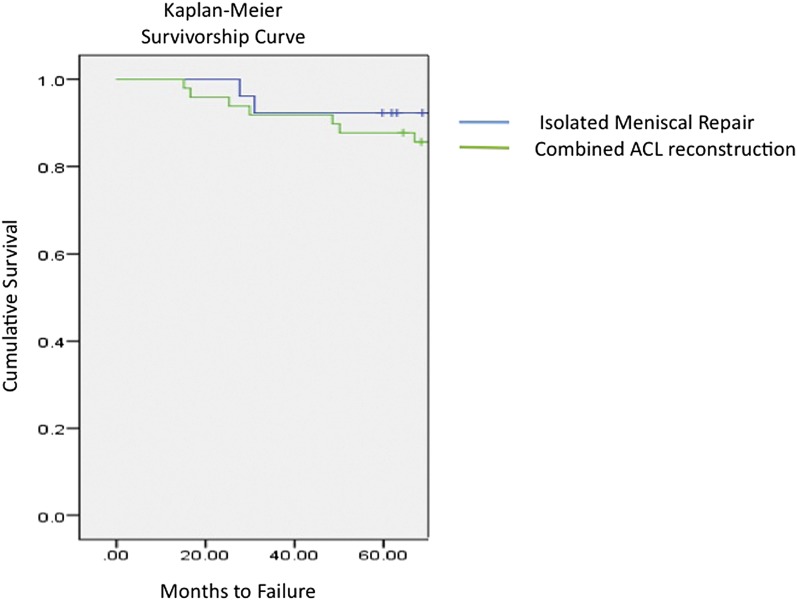
Statistical Analysis
The failure rate of meniscal repair was calculated for isolated repairs and those combined with ACL reconstruction, with 95% confidence intervals (CIs). Comparison of categorical variables (sex and meniscal location) was performed with use of the Fisher exact test. The paired Student t test was used for analysis of quantitative data (patient age, duration of follow-up, and number of sutures utilized). Survivorship analysis was performed with use of the Kaplan-Meier method (Fig. 1). Time to failure was defined as the interval between the index meniscal repair and repeat meniscal repair or meniscectomy. The log-rank test was utilized to compare the survival of isolated repairs with that of repairs combined with ACL reconstruction. SPSS version 21 (IBM, Armonk, New York) was used for survivorship analysis. All other statistical analyses were performed with the WINPEPI statistical program, version 11.26 (School of Public Health and Community Medicine, Hebrew University, Jerusalem, Israel). Significance was defined as p < 0.05.
Fig. 1.
Kaplan-Meier survivorship curve for all-inside meniscal repair, both as an isolated procedure and as performed with concurrent ACL reconstruction.
Source of Funding
This study was supported in part by National Institutes of Health (NIH)/National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) Grant RO1 AR053684 (L.J.H.).
Results
Successful Versus Failed Meniscal Repair
Twelve patients (16%) had failure of the meniscal repair. The average time between the primary repair and the reoperation was forty-seven months (range, 15.2 to ninety-five months). The data did not offer enough statistical evidence at alpha = 0.05 to establish a difference in average age between patients with successful and those with failed meniscal repair (success: 26.3 years [range, 14.1 to 53.5 years] versus failure: 29.0 years [range, 14.6 to 46.7 years], p = 0.437). These patients were also similar with regard to sex (success: 46% male versus failure: 66% male, p = 0.222), location of the meniscal repair (medial meniscus failure: 18.0% [95% CI: 7.35% to 28.65%] versus lateral meniscal failure: 8.0% [95% CI: −2.63% to 18.63%]), average number of sutures utilized for repair (success: 2.1 ± 1.19 sutures versus failure: 1.9 ± 1.08 sutures, p = 0.662), and average duration of follow-up (success: 6.8 ± 1.2 years versus failure: 6.7 ± 0.4 years, p = 0.741).
Isolated Meniscal Repairs Versus Meniscal Repairs Combined with ACL Reconstruction
The patients with isolated meniscal repair and those with combined meniscal repair and ACL reconstruction were similar in age at the time of surgery, sex, location of meniscal involvement, and duration of follow-up (Table I). However, more sutures were utilized for isolated repair (mean and standard deviation, 2.4 ± 1.4 sutures) than for the combined procedures (1.9 ± 1.0 sutures, p < 0.046). There was no difference in the rate of failure between isolated repairs (12% [95% CI: −0.76% to 23.76%]) and those combined with ACL reconstruction (18% [95% CI: 7.47% to 29.13%]) or in the average time to failure (48.1 ± 32.5 months versus 46.6 ± 27.4 months, p = 0.939). The failure rates of medial meniscal repairs were similar regardless of whether they were performed in isolation (19% [95% CI: −5.36% to 11.36%]) or combined with ACL reconstruction (18% [95% CI: −1.76% to 13.76%]).
TABLE I.
Demographics for Isolated Meniscal Repairs Versus Meniscal Repairs Combined with ACL Reconstruction
| Isolated Repair | Repair Combined with ACL Reconstruction | P Value | |
| Age* (yr) | 27.1 ± 12.1 | 26.5 ± 10.6 | 0.814 |
| Sex (% male) | 62 | 43 | 0.148 |
| Meniscus (% medial) | 62 | 69 | 0.608 |
| Duration of follow-up* (yr) | 7.1 ± 1.7 | 7.7 ± 1.2 | 0.0945 |
| Time to failure* (mo) | 48.1 ± 32.5 | 46.6 ± 27.4 | 0.939 |
The values are given as the mean and standard deviation.
Successful Versus Failed Isolated Meniscal Repairs
Subgroup analysis of the isolated-repair group alone did not establish a significant difference between successful repairs and failures in terms of average age (success: 26.2 years versus failure: 34.8 years, p = 0.253), sex (success: 61% male versus failure: 67% male, p = 1.0), or average duration of follow-up (success: 7.1 years versus failure: 6.9 years, p = 0.805). There were three failures of isolated meniscal repairs and all involved the medial meniscus; thus, the overall rate of failure of isolated medial meniscal repair was 19% (95% CI: −5.36% to 11.36%). There were no failures of isolated lateral meniscal repairs. Successful repair of isolated tears was associated with an increased number of sutures (2.6 versus 1.0), but the small numbers limited calculation of significance.
Successful Versus Failed Meniscal Repairs Combined with ACL Reconstruction
The data on the patients with combined meniscal repair and ACL reconstruction did not offer enough statistical evidence to establish a difference between successful repairs and failures in terms of average age (success: 26.4 years versus failure: 27.1 years, p = 0.854), sex (success: 38% male versus failure: 66% male, p = 0.146), or average duration of follow-up (success: 7.6 years versus failure: 8.1 years, p = 0.250). The failure rate of the medial meniscal repairs (18% [95% CI: −1.76% to 14%]) was similar that of the lateral meniscal repairs (20% [95% CI: −5.63% to 11.63%]) performed with concurrent ACL reconstruction. A similar number of sutures was also utilized in both groups (success: 1.8 versus failure: 2.2, p = 0.219).
Patient-Outcome Scores for Successful Meniscal Repairs
Patient-rated outcome-score questionnaires were completed and activity level was determined at the time of follow-up. There was no significant difference in the average postoperative KOOS subscale scores or IKDC scores between patients with a successful isolated meniscal repair and those with a successful repair combined with ACL reconstruction (Table II). Activity level, as defined by the Marx scale, was higher on average for the patients with isolated meniscal repair (9.1 ± 5.4) than for those with the combined procedure (4.6 ± 4.0, p = 0.03).
TABLE II.
Postoperative KOOS and IKDC Scores After Successful Meniscal Repairs: Isolated and Combined with ACL Reconstruction
| Outcome Score | Isolated Repair* | Repair Combined with ACL Reconstruction* | P Value |
| KOOS subscores | |||
| Stiffness | 83.8 ± 15.2 | 84.0 ± 17.1 | 0.933 |
| Pain | 91.2 ± 9.9 | 91.3 ± 13.4 | 0.993 |
| Activities of daily living | 95.4 ± 8.9 | 90.9 ± 11.1 | 0.351 |
| Sports | 83.5 ± 22.8 | 63.6 ± 26.6 | 0.619 |
| Quality of life | 85.7 ± 16.5 | 76.2 ± 22.1 | 0.132 |
| IKDC | 87.6 ± 14.8 | 80.9 ± 15.7 | 0.235 |
The values are given as the mean and standard deviation.
Discussion
Meniscal repair with a second-generation all-inside repair system is a reliable technique with good longevity of results. In our series, 84% of the patients had continued success at a minimum of five years (average, seven years) after the repair. Success rates were similar for isolated repairs and repairs performed in conjunction with ACL reconstruction and were not impacted by patient age or sex. The findings of a successful repair were supported by good to excellent results on patient-rated outcomes, including the IKDC and KOOS.
Success rates of the all-inside technique, and more specifically repairs performed with the FAST-FIX repair system, have been described in the literature, but the results have been limited to short-term follow-up data (maximum, three years). In a combined series of isolated repairs and repairs performed with ACL reconstruction, Barber et al. reported successful repair in 83% of patients after a minimum of one year of follow-up14. In a similar group, repeat follow-up at two years demonstrated clinically effective repair in 88% of patients10. The success rates after isolated repair and after repair combined with ACL reconstruction were 80% and 91%, respectively10. In a study with the longest follow-up of which we are aware (three years), successful repair was noted in 97% of patients12.
Our mid-term results of second-generation all-inside repair demonstrate improved success compared with first-generation implants and results equivalent to those seen with inside-out, outside-in, and open repair techniques. In a recent systematic review evaluating five-year outcomes of meniscal repairs performed with a variety of techniques, the pooled failure rate of first-generation all-inside repair was 24% whereas pooled failure rates of 22.2%, 23.9%, and 23.1% were found for inside-out, outside-in, and open meniscal repairs, respectively15.
Few studies analyzing meniscal repairs have been performed with validated patient-based outcome measures. The KOOS and IKDC scores in our study were high after both isolated repairs and those with concomitant ACL reconstruction. The Marx activity scale scores were lower for the patients who had associated ACL reconstruction, which is consistent with the decreased activity over time demonstrated by previous analysis of the MOON cohort16,17.
Strengths of our study include the duration of follow-up, evaluation of both isolated repairs and those performed in conjunction with ACL reconstruction, and utilization of validated patient-based outcome measures. An additional strength is a 90% follow-up rate, which limited attrition bias. We believe that our cohort of meniscal repairs is the third largest evaluated beyond five years and that we are the first to report the five-year success of second-generation all-inside repairs. In our study, meniscal repair failure was noted to occur as late as seven years postoperatively, with the typical time to failure being four years. The average time to failure in our study was longer than the longest follow-up period in any previous study of second-generation devices12, to our knowledge. Studies limited to shorter follow-up may underestimate the extent of repair failure. In contrast to the findings of previous reports18,19, we did not observe improved healing when the meniscal repair had been performed with ACL reconstruction. Overlapping confidence intervals demonstrated that the 6.8% difference in failure rate observed between isolated repairs and those performed concurrently with ACL reconstruction lacked significance in our study. The data also demonstrated no difference in failure rate between medial and lateral meniscal repairs, regardless of whether they were performed in isolation or combined with ACL reconstruction. Our results confirm the findings of Nepple et al., who at five years demonstrated similar failure rates for isolated repairs and those combined with ACL reconstruction as well as similar failure rates for medial and lateral meniscal repairs15. Their systematic review did show a trend toward decreased failure after lateral meniscal repairs. (Their analysis did not distinguish between isolated lateral repairs and lateral repairs combined with ACL reconstruction.) A similar finding was seen in our cohort of isolated repairs, in which no failures of the lateral meniscus were noted. Limited sample size in both our study and the studies evaluated in the systematic review may limit identification of a possible significant difference in failure rate between lateral and medial meniscal repairs.
This study has several limitations. It was a retrospective review and vulnerable to the bias associated with such reviews. Additionally, meniscal failure was defined as the need for revision repair or partial meniscectomy. This may underestimate failure, but it represents the currently accepted definition of failure as acknowledged by Lozano et al. in their systematic review of all-inside repairs20. It is currently difficult to use second-look arthroscopy or magnetic resonance arthrography to assess failure because of cost and patient-safety concerns. Thus, it is possible there were clinically asymptomatic failures of meniscal repairs within the cohort. A power analysis was not performed for this retrospective review, and it is possible that the number of patients, despite being comparable with those in other reports of mid-term results of meniscal repair, may have been insufficient to detect a difference between isolated repairs and repairs combined with ACL reconstruction.
The all-inside meniscal repair technique is a reliable treatment option for both isolated meniscal tears and those that occur in conjunction with ACL injury. Successful repair can be expected in >80% of patients. Continued success of these repairs was shown after a mid-term follow-up period averaging more than seven years, with excellent patient-reported outcomes and high patient-reported activity.
Acknowledgments
Note: The authors thank Christopher C. McAndrew, MD, for his assistance with the statistical analysis.
Footnotes
Investigation performed at the Department of Orthopaedic Surgery, Washington University School of Medicine, St. Louis, Missouri
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Garrett WE Jr, Swiontkowski MF, Weinstein JN, Callaghan J, Rosier RN, Berry DJ, Harrast J, Derosa GP. American Board of Orthopaedic Surgery practice of the orthopaedic surgeon: Part-II, certification examination case mix. J Bone Joint Surg Am. 2006March;88(3):660-7 [DOI] [PubMed] [Google Scholar]
- 2.Schwarz B, Heisel J, Mittelmeier H. [Significance of early meniscectomy in the etiology of severe arthritis of the knee]. Aktuelle Traumatol. 1986June;16(3):84-9 [PubMed] [Google Scholar]
- 3.Hart R, Janecek M, Siska V, Kucera B, Stipcák V. [Correlation of long-term clinical and radiological results after meniscectomies]. Acta Chir Orthop Traumatol Cech. 2005;72(5):304-7 [PubMed] [Google Scholar]
- 4.Henning CE, Clark JR, Lynch MA, Stallbaumer R, Yearout KM, Vequist SW. Arthroscopic meniscus repair with a posterior incision. Instr Course Lect. 1988;37:209-21 [PubMed] [Google Scholar]
- 5.Warren RF Arthroscopic meniscus repair. Arthroscopy. 1985;1(3):170-2 [DOI] [PubMed] [Google Scholar]
- 6.Grant JA, Wilde J, Miller BS, Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: a systematic review. Am J Sports Med. 2012February;40(2):459-68 Epub 2011 Jul 07 [DOI] [PubMed] [Google Scholar]
- 7.Anderson K, Marx RG, Hannafin J, Warren RF. Chondral injury following meniscal repair with a biodegradable implant. Arthroscopy. 2000October;16(7):749-53 [DOI] [PubMed] [Google Scholar]
- 8.Wilmes P, Lorbach O, Brogard P, Seil R. [Complications with all-inside devices used in reconstructive meniscal surgery]. Orthopade. 2008November;37(11):1088-9: 1091-5: 1097-8 [DOI] [PubMed] [Google Scholar]
- 9.Gliatis J, Kouzelis A, Panagopoulos A, Lambiris E. Chondral injury due to migration of a Mitek RapidLoc meniscal repair implant after successful meniscal repair: a case report. Knee Surg Sports Traumatol Arthrosc. 2005May;13(4):280-2 Epub 2004 Oct 20 [DOI] [PubMed] [Google Scholar]
- 10.Haas AL, Schepsis AA, Hornstein J, Edgar CM. Meniscal repair using the FasT-Fix all-inside meniscal repair device. Arthroscopy. 2005February;21(2):167-75 [DOI] [PubMed] [Google Scholar]
- 11.Tachibana Y, Sakaguchi K, Goto T, Oda H, Yamazaki K, Iida S. Repair integrity evaluated by second-look arthroscopy after arthroscopic meniscal repair with the FasT-Fix during anterior cruciate ligament reconstruction. Am J Sports Med. 2010May;38(5):965-71 Epub 2010 Mar 02 [DOI] [PubMed] [Google Scholar]
- 12.Chiang CW, Chang CH, Cheng CY, Chen AC, Chan YS, Hsu KY, Chen WJ. Clinical results of all-inside meniscal repair using the FasT-Fix meniscal repair system. Chang Gung Med J. 2011May-Jun;34(3):298-305 [PubMed] [Google Scholar]
- 13.Sgaglion N, Caborn D. Meniscal repair with the FasT-Fix suture system. Smith & Nephew, Inc. 2002. http://www.smith-nephew.com/global/assets/pdf/products/surgical/ultra_fastfix_kne_1061031c.pdf. Accessed 2014 Feb 5 [Google Scholar]
- 14.Barber FA, Schroeder FA, Oro FB, Beavis RC. FasT-Fix meniscal repair: mid-term results. Arthroscopy. 2008December;24(12):1342-8 Epub 2008 Oct 10 [DOI] [PubMed] [Google Scholar]
- 15.Nepple JJ, Dunn WR, Wright RW. Meniscal repair outcomes at greater than five years: a systematic literature review and meta-analysis. J Bone Joint Surg Am. 2012December19;94(24):2222-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dunn WR, Spindler KP; MOON Consortium. Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010October;38(10):2040-50 Epub 2010 Aug 13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spindler KP, Huston LJ, Wright RW, Kaeding CC, Marx RG, Amendola A, Parker RD, Andrish JT, Reinke EK, Harrell FE Jr, Dunn WR; MOON Group. The prognosis and predictors of sports function and activity at minimum 6 years after anterior cruciate ligament reconstruction: a population cohort study. Am J Sports Med. 2011February;39(2):348-59 Epub 2010 Nov 17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cannon WD Jr, Vittori JM. The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. Am J Sports Med. 1992Mar-Apr;20(2):176-81 [DOI] [PubMed] [Google Scholar]
- 19.Tenuta JJ, Arciero RA. Arthroscopic evaluation of meniscal repairs. Factors that effect healing. Am J Sports Med. 1994Nov-Dec;22(6):797-802 [DOI] [PubMed] [Google Scholar]
- 20.Lozano J, Ma CB, Cannon WD. All-inside meniscus repair: a systematic review. Clin Orthop Relat Res. 2007February;455(455):134-41 [DOI] [PubMed] [Google Scholar]