Sir,
Acinetobacter spp. have emerged as an important cause of Health care Associated Infection in recent years. There are complications in the infection control and treatment of patients who were infected with Acinetobacter spp. because of the extraordinary ability of this bacterium to survive in environment for long periods and its propensity to acquire multiple antibiotic resistance mechanisms.[1] This cross-sectional study was performed for determination prevalence of clinical isolates of Acinetobacter spp., antibiotic resistance pattern and risk factors associated with acquisition of colonization/infection with extensively drug resistant (XDR) Acinetobacter spp. in the specialty teaching hospital, in Isfahan, Iran.
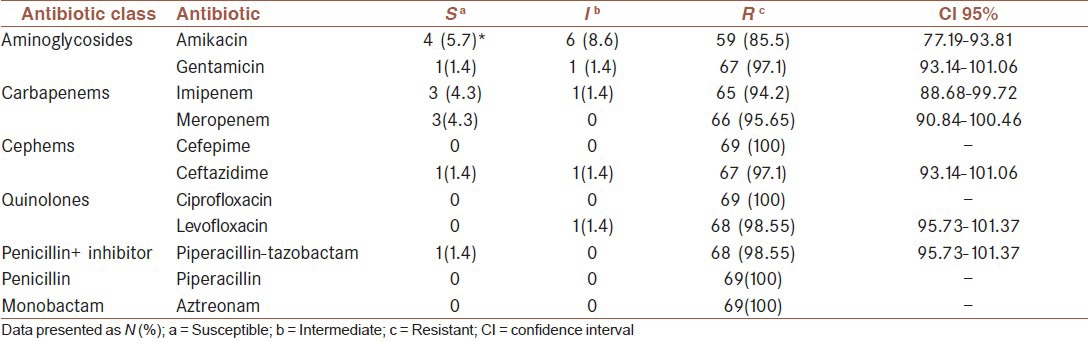
During the 4 month period between October 2011 and Jan 2012, we collected 865 clinical specimens, including different clinical specimens from various wards. Acinetobacter was identified by conventional methods. Antimicrobial susceptibility testing was done using the disk diffusion method according to Clinical Laboratory and Standards Institute (CLSI-2011) guidelines.[2] A total of 69 Acinetobacter spp. were isolated. A total of 36 patients (52.17%) were female. Most of Acinetobacter spp. were isolated from tracheal tube secretion with 14 (20.3%) positive cultures. In surveillance of antibiotic susceptibility tests, we founded that 60 (86.95%) isolates were XDR, because of their resistance to all of 11 antibiotics [Table 1]. This is comparable with a report from USA that showed 46% of isolates were resistant to all of conventional antibiotics.[3] Totally, 66 isolates (95.65%) were carbapenem-resistant. In the six patients, Acinetobacter was isolated from multiple sites or one site for several times. It should be mentioned that all of six patients were infected or colonized with XDR strains, died during our study. Thus, this presumption exists that in some cases death was related to Acinetobacter infection or infection had accelerated patients’ death rate. Significant risk factors for colonization/infection with XDR-strains were hospitalized duration (P = 0.048), underlying disease (P = 0.016), and corticosteroid usage (P = 0.030). In this study prevalence of Acinetobacter spp. was 7.98% while in Korea was 6.6%.[4] Many investigations reported prevalence of Acinetobacter particularly in the intensive care unit (ICU) ward. Prevalence of Acinetobacter spp. in the ICU ward of a hospital in Tehran was 22.4% and was most frequently isolated organism,[5] while in our study was 71.0%. This discrepancy may be due to several factors such as the condition of patients, management of infection control programs, type of strains and antibiotic resistance pattern of isolates that it is effective in increasing of survival rate of them in the environment and colonization on the body of patients.
Table 1.
Antibiotic susceptibility pattern of Acinetobacter spp
With increasing in prevalence of Acinetobacter spp. infections specially XDR-isolates, it is critical utilization of procedures that can reduce emersion and prevalence of XDR-Acinetobacter spp. among hospitalized patients.
AUTHORS CONTRIBUTION
Dr. Bahram Nasr Esfahani was co-author of study and coordinated preparation of manuscript. Arezoo Pourdad coordinated collection and surveillence of demographic and medical data of patients of study and experimental studies. Mojtaba Akbari performed statistical analysis of data. Tahere Motallebi Rad coordinated design of study and performed clinical and experiments studies and achieved Data of work. Manuscript is written by her. Dr. Hossein Fazeli designed the study and procedures and methods and contributed to editing of manuscript.
ACKNOWLEDGEMENT
The authors are grateful to Vice-chancellor for Research, Isfahan University of medical sciences for financial support of the present study (research project number 390454).
REFERENCES
- 1.Harris AD, McGregor JC, Furuno JP. What infection control interventions should be undertaken to control multidrug-resistant gram-negative bacteria? Clin Infect Dis. 2006;43:S57–61. doi: 10.1086/504479. [DOI] [PubMed] [Google Scholar]
- 2.Wayne P. Vol. 31. Clin Laboratory Standards Institute; 2011. Performance standards for antimicrobial susceptibility testing; Twenty-first Informational Supplement; pp. M100–S21. [Google Scholar]
- 3.Dent LL, Marshall DR, Pratap S, Hulette RB. Multidrug resistant Acinetobacter baumannii: A descriptive study in a city hospital. BMC Infect Dis. 2010;10:196. doi: 10.1186/1471-2334-10-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee K, Kim MN, Kim JS, Hong HL, Kang JO, Shin JH, et al. Further increases in carbapenem-, amikacin-, and fluoroquinolone-resistant isolates of Acinetobacter spp. and P. aeruginosa in Korea: KONSAR study 2009. Yonsei Med J. 2011;5:793–802. doi: 10.3349/ymj.2011.52.5.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mohammadtaheri Z, Pourpaki M, Mohammadi F, Namdar R, Masjedi MR. Surveillance of antimicrobial susceptibility among bacterial isolates from intensive care unit patients of a tertiary-care university hospital in Iran: 2006-2009. Chemotherapy. 2010;56:478–84. doi: 10.1159/000321032. [DOI] [PubMed] [Google Scholar]


