Abstract
Attrition can jeopardize both internal and external validity. The goal of this secondary analysis is to examine predictors of attrition using baseline data of 432 participants in the Rural Breast Cancer Survivors study. Attrition was conceptualized by demographic, social, cancer treatment, physical health, and mental health characteristics. Baseline measures were selected using this conceptualization. Bivariate tests of association, discrete-time Cox regression models and recursive partitioning techniques were used in analysis. Results showed that 100 participants (23%) dropped out by Month-12. Non-linear tree analyses showed that poor mental health and lack of health insurance were significant predictors of attrition among participants. Findings contribute to future research efforts to reduce attrition among rural underserved populations.
Keywords: attrition, predictors of attrition, longitudinal research, secondary analysis, methodological research, underserved populations, rural women, breast cancer survivors
Attrition is typically defined as the loss of a research participant prior to study completion (Deeg, 2002). Attrition can threaten internal validity because it is difficult to determine whether group differences result from the intervention or dropout (Cook & Campbell, 1979). Attrition can jeopardize external validity because participants who completed a study may significantly differ from those who dropped out (Deeg, 2002; Demark-Wahnefried, Bowen, Jabson, & Paskett, 2011; Ribisl, Walton, Mowbray, Boostsmiller, 1996).
Attrition is also an underreported problem. Nearly 20 years ago, Ribisl et al. (1996) documented that few investigators even bothered to report attrition or patterns of attrition. More than a decade later in 2007, Robinson and colleagues (Robinson, Dennison, Wayman, Pronovost & Needham, 2007) noted the continued persistence of the problem.
As previously suggested, attrition can jeopardize validity (Clough-Gorr, Fink, Silliman, 2008). Validity threats can be problematic in longitudinal research with breast cancer survivors. Breast cancer is the most common female cancer with a five-year relative survival rate of 90% with the vast majority becoming long-term survivors (American Cancer Society, 2013). Longitudinal research in cancer survivorship helps investigators to better understand the processes and changes occurring among survivors over time, and to identify natural time points for intervention.
The NIH Office of Women’s Health data indicate that roughly one third of women in the United States live in rural areas (Whitten-Goldstein, 2003). Yet, rural residents typically do not participate in research (Bolen et al, 2006; Baquet, Commiskey, Daniel Mullins, & Mishra, 2006; Paskett et al., 2002). Thus, improving our knowledge and understanding of study participation among rural women with breast cancer who enroll in a longitudinal research study, and an examination of descriptors and predictors of attrition in this underserved population is warranted.
The purpose of this study is to determine predictors of attrition using baseline characteristics among 432 participants in the Rural Breast Cancer Survivors (RBCS) study. Using secondary analysis of the collected baseline data, the specific aims are to: (a) describe sociodemographic, cancer treatment, physical health, and mental health characteristics at baseline; (b) describe attrition among rural women participating in the RBCS study; (c) determine whether baseline characteristics predict risk of attrition in the RBCS study; and (d) discuss opportunities and challenges to reducing attrition among underserved rural women.
Attrition as a Concept
There is a gap in the literature concerning conceptual frameworks in which to explore attrition (Marcellus, 2004; Robinson, Dennison, Wayman, Pronovost, & Needham, 2007). Thus, the authors conceptualized attrition based on demographic, social, cancer treatment, physical health, and mental health characteristics of the study population of rural breast cancer survivors.
Demographic Characteristics
Demographic variables predicted attrition in previous longitudinal studies (Chatfield, Brayne, & Matthews, 2005; Young, Powers & Bell, 2006; de Graaf, van Dorsselaer, Tuithof, & Ten Have, 2013). Chatfield, Brayne, and Matthews (2005) conducted a systematic review of attrition occurring among the elderly after baseline in longitudinal studies. The review was limited to epidemiologic, population-based studies with a minimum of 1,000 participants aged 65 years and older. The investigators found three significant factors predicting attrition from baseline data: advancing age, lower education, and cognitive impairment.
Haring and colleagues (2009) used data from a longitudinal population-based study of health among more than 7,000 residents of the Pomerania region of Germany. They found that older age, lower educational level and unemployment were significant demographic and social predictors of attrition. In their conclusion, the authors suggested that when recruiting potentially underserved populations, special techniques should be considered to increase the efficiency of response.
Rural residence influences study recruitment (Baquet, Commiskey, Mullins & Mishra, 2006; Paskett et al. 2002). Baquet and colleagues uncovered serious gaps in efforts to recruit rural residents in clinical trials, and found rural residence as a signficant predictor of study participation among rural residents in Maryland’s Eastern and Western Shore. Paskett et al (2002) developed an intervention program consisting of rapid tumor-reporting system, nurse facilitation, quarterly newsletter communication, and health education to improve recruitment of North Carolina rural participants in cancer clinical trials. Yet, they found that the intervention was ineffective in improving rural participation, and similar to Baquet et al, confirmed thorny problems in rural recruitment.
Social Characteristics
Positing that social characteristics may be associated with risk of attrition, Young, Powers, and Bell (2006) investigated patterns of attrition in the Australian Longitudinal Study on Women’s Health (ALSWH). The participants comprised a nationally representative sample of young women (age 18–23), middle age women (age 45–50), and older women (age 70–75). Recognizing the paucity of rural participation, the investigators oversampled women living in rural and remote Australian regions. Findings showed that social characteristics were related to attrition. The major reason for attrition occurred most strikingly among young women (21%) compared with older women (2%). Younger and middle age women who dropped out were more likely to be single (i.e., separated, divorced or widowed), and experiencing financial difficulty. Clough-Gorr, Fink, and Silliman (2008), in a longitudinal study of older breast cancer survivors, also noted that lack of finances was associated with attrition.
Cancer Treatment Characteristics
Clough-Gorr et al. (2008) found that advanced stage of disease at diagnosis and hormonal therapy (i.e., tamoxifen) were associated with attrition. However, we recognize the paucity of evidence in the literature on how cancer treatment characteristics relate to attrition in behavioral, longitudinal studies.
Physical Health Characteristics
Physical health is associated with attrition. Clough-Gorr, et al. (2008) found that a larger number of comorbid condition was associated with higher attrition due to death or being lost to follow-up. Among those who died, poorer health and worse tumor characteristics were noted. Similarly, Van Beijsterveldt, van Boxtel, Bosma, Houx, Buntinx, and Jolles (2002) found that poor overall health predicted attrition.
Mental Health Characteristics
Poor mental health is associated with attrition (Clough-Gorr et al 2008; Ribisl et al., 1996; Young et al, 2006). In a prospective study of cardiovascular prevention, Bambs et al (2013) found that participants with CES-D scores indicative of clinical depression were more likely to be lost to follow-up. Stressful life events such as caregiving and uncontrollable events (i.e. natural disasters, family deaths) that influence mental health appeared to increase drop-out or withdrawal (Ribisl et al, 1996; Young et al, 2006). Depression was also identified as a predictor of attrition by Lee, Hayes, McQuaid, and Borrelli (2010) in their study on a smoking cessation program. Individual participants who had lower depressed mood scores were more likely to complete the program as opposed to those with higher levels (Lee, et al, 2010).
In summary, a multi-dimensional concept of attrition containing demographic, social, cancer treatment, physical health, and mental health characteristics were associated with attrition.
Materials and Methods
Study Population
The present study is a secondary analysis of data from the Rural Breast Cancer Survivors Study (RBCS), a population-based study of psychoeducational support interventions among rural Florida-dwelling women. A three-pronged approach using state cancer registry data with both active and passive recruitment techniques was used for recruitment. Eligibility criteria were: women diagnosed with Stage 0–III breast cancer, living in rural areas of Florida, within the first three years of completion of primary breast cancer treatment, at least 21 years of age, and with telephone or cellphone access. Women receiving anti-hormonal therapy (i.e., tamoxifen or aromatase inhibitor) or anti-HER2 treatment at the time of study initiation were also eligible. Women with metastatic disease at the time of study contact, men with a breast cancer diagnosis, and those having no telephone or cellphone access were excluded from participation.
Rural eligibility was established based on one of two criteria: (1) residence in one of 33 Florida rural counties designated by Florida statute (Florida Department of Health, 2007); or (2) residence in a rural pocket of one of 34 Florida urban with an Index of Research Access (IRA) score equal to or greater than 4. This score can be roughly translated into a criterion that women had at least four times the difficulty in securing face-to-face post-treatment support than women who lived within one mile of the nearest treatment facility. Details and calculations for the IRA score have been reported in detail elsewhere (the Authors, 2012). The IRA was particularly suitable for recruitment of rural residents because it provides a more detailed determination of rurality that cannot be obtained by county residence alone.
Once enrolled, participants were randomized to either the Experimental (early intervention) or Wait Control (late intervention) groups. Study participation lasted over twelve months. The specific details of the processes of study recruitment, enrollment, randomization, retention, and intervention are described in detail elsewhere (the Authors, 2013; the Authors, under review). The authors recognize that these processes and concepts are related. However, the present investigation focuses on predictors of attrition.
Analytic Variables
For this secondary analysis, participants’ demographic, social and cancer treatment characteristics and baseline values for three study measures were selected to examine predictors of attrition based on the conceptualization of attrition, and empirical evidence from the literature.
Demographic Characteristics
The Breast Cancer Survivor Sociodemographic and Treatment Survey contains 12 demographic variables including: age, race, ethnicity, education level, marital status, type of health insurance, work status, and number of people living in the home. This measure has been used in prior studies by the authors.
Social Characteristics
The Medical Outcomes Study Social Support Index (MOS-SSS) was used to assess social characteristics (Sherbourne & Stewart, 1991). The MOS-SSS contains an overall functional social support index with scores range from 0 to 100. Higher scores indicate more social support. In the present study, the MOS-SSS overall functional social support index had alpha reliability of 0.96.
Cancer Treatment Characteristics
The Sociodemographic and Treatment Survey contains 12 cancer treatment items related to breast cancer treatment including months since diagnosis and time since end of treatment, type of breast cancer surgery, radiation therapy, chemotherapy, hormonal therapy, and/or anti-HER2 therapy.
Physical Health
The Medical Outcomes Survey Short Form v1 (SF-36) is a commonly used measure of physical health and function (Ware & Sherbourne, 1992). The SF-36 has 36 items that aggregate into eight subscales consisting of 2–10 items, and two overall summary scores that aggregate the eight subscales. The two overall summary scores are the Physical Component Summary score (PCS) and the Mental Component Summary score (MCS). Four health concepts (i.e., physical functioning, role-physical, body pain, and general health form the aggregate PCS score.
Mental Health
Two measures of mental health were used in the present study. First, the SF-36 v1 previously described contains four health concepts (i.e. vitality, social functioning, role-emotional, and mental health) that form the aggregate MCS score. The SF-36 v1 norm scores range from 0 to 100, where higher scores indicate better physical health and mental health, respectively. A norm score of 50 indicates a level comparable to that of the average adult in the U.S. population. In the present study, the PCS and the MCS summary scores had alpha reliability of .93 and .90 respectively.
The second measure of mental health used was the Center for Epidemiologic Studies Depression Scale (CES-D), a widely used short self-report scale to measure depressive symptoms in the general population (Radloff, 1977). Total score ranges from 0 to 60, where higher scores indicate higher depressive symptomatology. Scores ≥ 16 suggest clinically significant levels of psychological distress. In the RBCS study, the CES-D had Cronbach alpha reliability of 0.91.
Analytic Strategy
To determine potential predictors of attrition, baseline demographic, social, cancer treatment, physical health, and mental health characteristics were tabulated. The time point for the last data collection was tabulated for all participants, and was used as the indicator of retention (if completed the Month-12 battery of measures or attrition (if the last completed battery of measures was at baseline or Month-3). Among those who dropped out, the median last data collection time point was computed. First, descriptive statistics for the variables of interest were computed at each of three study time points (i.e., baseline, median last data collection time point, and Month-12).
Second, using bivariate tests of association, baseline participant characteristics were tested for differences between those retained and those who dropped out by the median last data collection time point, and by the end of the study (Month 12), with the purpose of identifying individual predictors that were consistently associated with attrition across the study period.
Third, a time-to-event analysis was performed. Discrete-time Cox regression models were used to assess the association between the baseline characteristics, when considered simultaneously, and the instantaneous risk or hazard of attrition (i.e. the probability that a participant dropped out from the study at a certain time point, given that the participant had been retained up to that time point) (Allison, 2010). An initial model with all covariates (i.e., a saturated model) was fitted. Next, a reduced model was fitted using a step-wise procedure that minimized the Akaike Information Criterion (AIC). A likelihood ratio test was conducted to obtain a formal test of difference in goodness-of-fit between the saturated and reduced models. Wald tests were used to assess the significance of regression coefficients in the final model and extract interpretations in terms of hazard ratios. The proportional hazards assumption was tested in the final model by fitting time-by-covariate interactions and using a linear contrast to conduct an overall test for these interaction terms.
A second exploratory analysis was conducted to identify rules that would allow a classification of participants at risk for attrition. To this end, recursive partitioning techniques were used to construct classification tree models for attrition status using baseline characteristics as predictors (Everitt, 2009; Su, McNees, Meneses, & Johnson, 2011). Classification trees are useful alternative models for identifying relevant combinations of predictors that cannot be uncovered using traditional statistical models that assume linearity of predictors. Unlike linear models, tree models are not easily described using equations and therefore are typically shown graphically.
All the above analyses were conducted using SAS v9.3 statistical software, except for the tree analysis that was conducted using the package Party in the R statistical software (Hothorn, 2006; R-statistical-software-v2.15.00., 2008; SASv9-3., 2010). Statistical significance was held at the 0.05 level.
Results
Characteristics at Baseline
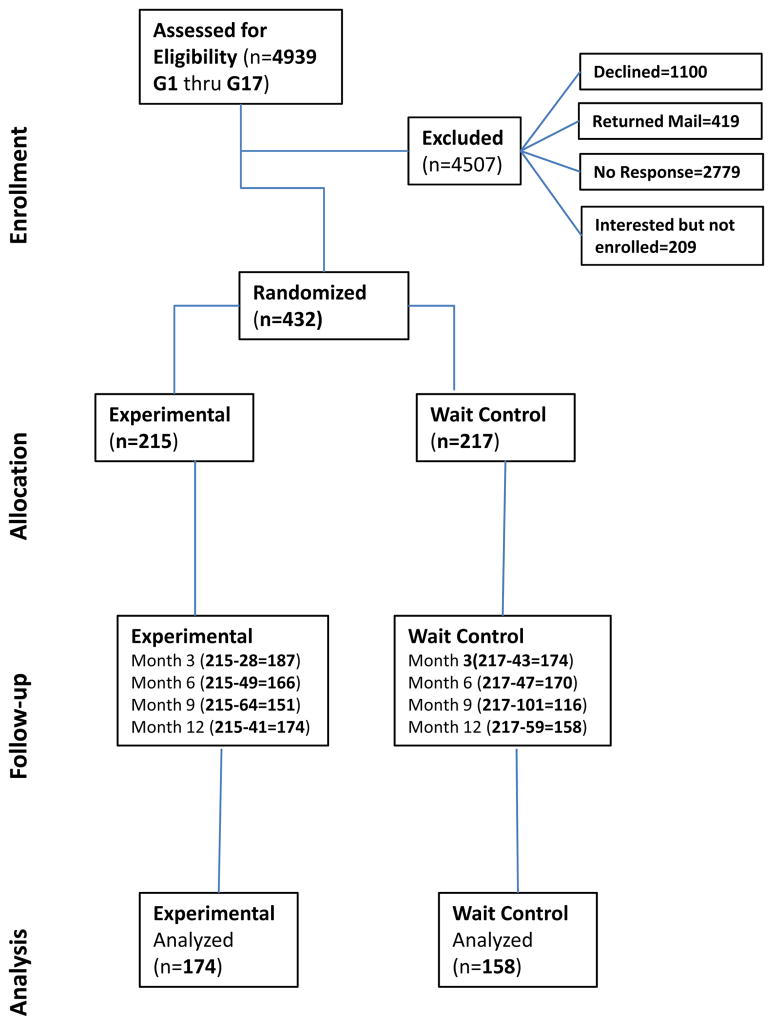
The CONSORT diagram is shown in Figure 1. A total of 641 (13.5%) rural breast cancer survivors responded with interest in study participation. Of these, 432 (67.4%) subsequently enrolled in the RBCS and were randomized to one of two study arms. Attrition was defined as non-completion of the study by Month 12. A total of 100 RBCS participants (23%) dropped out from the study.
Figure 1.
RBCS CONSORT
Copyright 2013, the author
Table 1 (left column) lists demographic, cancer treatment and some social characteristics of the 432 RBCS participants at baseline study entry. Missing data were detected in the household income variable with 64 (14.8%) declining to provide information on income. The sample was predominately Caucasian, with a mean age of 63.1 years, married/partnered, and educated at the trade school/some college level. More than 30% had household incomes less than $30,000. The majority of participants were retired, and more than 94% had health insurance. The average time since diagnosis to study entry was 25.6 months (SD=7.9) with an average time since completion of primary breast cancer treatment of 18.8 months (SD=7.9). The majority (56.9%) had lumpectomy and radiation therapy for control of local disease, and chemotherapy (57.9%) for control of regional systemic disease. More than 66% received hormonal blocking agents to reduce the risk for recurrence.
Table 1.
Baseline Sociodemographic, Treatment, and Selected Psychometric Measures for RBCS Participants, Compared by Attrition Status at Month 3 and 12
| Overall (N=432) | Month 3 | Month 12 | ||||
|---|---|---|---|---|---|---|
| Retained (n=361) | Dropped (n=71) | P*a | Retained (n=332) | Dropped (n=100) | P*b | |
| Group Assignment | 0.056 | 0.0592 | ||||
| Wait Control (n=217, 50.2%) | 174 (48.2%) | 43 (60.6%) | 158 (47.6%) | 59 (59%) | ||
| Experimental (n=215, 49.8%) | 187 (51.8%) | 28 (39.4%) | 174 (52.4%) | 41 (41%) | ||
|
| ||||||
| Age (M=63.1, SD=10.5) | M=63.7, SD=10.5 | M=60.2, SD=10.1 | 0.0105 | M=63.8, SD=10.2 | M=60.7, SD=11.1 | 0.011 |
|
| ||||||
| Race | 0.5698 | 0.4832 | ||||
| Caucasian (n=408, 94.4%) | 342 (94.7%) | 66 (93%) | 315 (94.9%) | 93 (93%) | ||
| Other (n=24, 5.6%) | 19 (5.3%) | 5 (7%) | 17 (5.1%) | 7 (7%) | ||
|
| ||||||
| Annual Income | 0.8444 | 0.1377 | ||||
| ≤$30,000 (n=131, 30.3%) | 107 (29.6%) | 24 (33.8%) | 94 (28.3%) | 37 (37%) | ||
| $30,001 – $50,000 (n=80, 18.5%) | 66 (18.3%) | 14 (19.7%) | 58 (17.5%) | 22 (22%) | ||
| >$50,000 (n=157, 36.4%) | 133 (36.9%) | 24 (33.8%) | 127 (38.2%) | 30 (30%) | ||
| No response (n=64, 14.8%) | 55 (15.2%) | 9 (12.7%) | 53 (16%) | 11 (11%) | ||
|
| ||||||
| Marital Status | 0.0536 | 0.0459 | ||||
| Married/partnered (n=315, 72.9%) | 270 (74.8%) | 45 (63.4%) | 250 (75.3%) | 65 (65%) | ||
| Other (n=117, 27.1%) | 91 (25.2%) | 26 (36.6%) | 82 (24.7%) | 35 (35%) | ||
|
| ||||||
| Employment | 0.1249 | 0.142 | ||||
| Full-time (n=111, 25.7%) | 85 (23.5%) | 26 (36.6%) | 77 (23.2%) | 34 (34%) | ||
| Part-time (n=62, 14.3%) | 54 (15%) | 8 (11.3%) | 47 (14.2%) | 15 (15%) | ||
| Retired (n=196, 45.4%) | 170 (47.1%) | 26 (36.6%) | 159 (47.9%) | 37 (37%) | ||
| Other (n=63, 14.6%) | 52 (14.4%) | 11 (15.5%) | 49 (14.7%) | 14 (14%) | ||
|
| ||||||
| Education | 0.4777 | 0.0574 | ||||
| < High School (n=24, 5.6%) | 22 (6.1%) | 2 (2.8%) | 21 (6.3%) | 3 (3%) | ||
| High School grad (n=97, 22.4%) | 81 (22.4%) | 16 (22.5%) | 73 (22%) | 24 (24%) | ||
| Trade school/ Some college (n=149, 34.5%) | 119 (33%) | 30 (42.2%) | 104 (31.3%) | 45 (45%) | ||
| College grad (n=104, 24.1%) | 90 (24.9%) | 14 (19.7%) | 86 (25.9%) | 18 (18%) | ||
| Postgraduate (n=58, 13.4%) | 49 (13.6%) | 9 (12.7%) | 48 (14.5%) | 10 (10%) | ||
|
| ||||||
| Health Insurance | 0.0102 | 0.0118 | ||||
| Yes (n=408, 94.4%) | 346 (95.8%) | 62 (87.3%) | 319 (96.1%) | 89 (89%) | ||
| No (n=24, 5.6%) | 15 (4.2%) | 9 (12.7%) | 13 (3.9%) | 11 (11%) | ||
|
| ||||||
| Mo's since Dx (M=25.6, SD=7.9) | M=25.5, SD=7.8 | M=25.8, SD=8.1 | 0.7564 | M=25.5, SD=7.8 | M=25.8, SD=8 | 0.727 |
|
| ||||||
| Mo's since end of Tx (M=18.8, SD=8.6) | M=18.8, SD=8.6 | M=18.6, SD=8.5 | 0.7708 | M=18.9, SD=8.7 | M=18.6, SD=8.1 | 0.7729 |
|
| ||||||
| Surgery | 0.2629 | 0.331 | ||||
| Lumpectomy (n=246, 56.9%) | 208 (57.6%) | 38 (53.5%) | 192 (57.8%) | 54 (54%) | ||
| Mastectomy (n=128, 29.6%) | 109 (30.2%) | 19 (26.8%) | 100 (30.1%) | 28 (28%) | ||
| Bilateral mastectomy (n=58, 13.5%) | 44 (12.2%) | 14 (19.7%) | 40 (12.1%) | 18 (18%) | ||
|
| ||||||
| Chemotherapy | 0.442 | 0.9761 | ||||
| Yes (n=250, 57.9%) | 206 (57.1%) | 44 (62%) | 192 (57.8%) | 58 (58%) | ||
| No (n=182, 42.1%) | 155 (42.9%) | 27 (38%) | 140 (42.2%) | 42 (42%) | ||
|
| ||||||
| Radiation Therapy | 0.0526 | 0.0695 | ||||
| Yes (n=304, 70.4%) | 261 (72.3%) | 43 (60.6%) | 241 (75.6%) | 63 (63%) | ||
| No (n=128, 26.9%) | 100 (27.7%) | 28 (39.4%) | 91 (27.4%) | 37 (37%) | ||
|
| ||||||
| Hormonal Therapy | 0.147 | 0.0666 | ||||
| Yes (n=288, 66.7%) | 246 (68.1%) | 42 (59.1%) | 229 (31%) | 59 (59%) | ||
| No (n=144, 33.3%) | 115 (31.9%) | 29 (40.8%) | 103 (69%) | 41 (41%) | ||
|
| ||||||
| Depression CES-D (M=10.5, SD=10.2) | M=9.7, SD=9.6 | M=14.3, SD=11.8 | 0.0029 | M=9.6, SD=9.6 | M=13.6,SD=11.3 | 0.0016 |
|
| ||||||
| MOS Overall Social Support (M=79.1, SD=21.2) | M=79.4, SD=20.4 | M=77.6, SD=24.4 | 0.5656 | M=79.3,SD=20.5 | M=78.2, SD=23.3 | 0.6261 |
|
| ||||||
| SF-36 PCS (M=45, SD=10.6) | M=45.3, SD=10.3 | M=42.9, SD=11.6 | 0.0801 | M=45.5, SD=10.1 | M=43.1, SD=11.7 | 0.073 |
|
| ||||||
| SF-36 MCS (M=48.8, SD=11.5) | M=49.7, SD=10.9 | M=44.2, SD=13 | 0.0013 | M=49.9, SD=10.7 | M=44.9, SD=13 | 0.0006 |
Chi-squared, Fisher's exact, or t tests, as appropriate;
test of difference in baseline characteristics between retained and dropped-out by month 3;
test of difference in baseline characteristics between retained and dropped-out at the end of the study (month 12)
Copyright, The Authors, 2013
Participants reported minor to moderate levels of depressive symptomatology (M=10.5, SD=10.2), but below clinically significant levels of depression (CES-D cut score of 16). Overall social support was good at 79% of the maximum scores. The SF-36 PCS and MCS composite scores were slightly below the general U.S. population average estimate.
Table 1 (middle and right columns) further demonstrates the bivariate tests of association between baseline characteristics and attrition at Month-3 and at Month-12. Of the baseline characteristics including group assignment, demographics, social, cancer treatment, physical health, and mental health across the study period, the characteristics that were consistently and significantly associated with attrition included: not having health insurance, higher depressive symptomatology, lower mental health, and younger age.
Table 2 shows the time to event analysis for the last data collection time point and includes the initial saturated Cox model and the reduced Cox model. In the initial saturated model, baseline characteristics significantly associated with attrition hazard were: full-time employment, not having health insurance, social support, and lower mental health. However, in the final reduced model, five characteristics remained, showing that full time employment, education at the trade school/some college level, not having health insurance, lower mental health, and hormonal therapy were significantly associated with the attrition hazard. Participants with these baseline characteristics had significantly higher attrition compared with retained participants. Per the AIC criterion, the reduced model provided a better balance between number of predictors and model accuracy than the saturated model. Goodness of fit was not significantly different between the two models (P=.0714). The proportional hazards assumption was not significantly violated by any of the predictors in the final model (linear contrast χ2(5)=4.95, P=.422).
Table 2.
Time-to-Event Analysis for the Last Data Collection Time-Point Among RBCS Participants
| Covariate | Saturated Model | Reduced Model | ||
|---|---|---|---|---|
| Hazard Ratio (95% CL) | P | Hazard Ratio (95% CL) | P | |
| Group Assignment | ||||
| Experimental | 0.65 (0.42, 1.01) | 0.0646 | - | - |
| Wait Control | Ref | |||
|
| ||||
| Age* | 0.71 (0.5, 1.01) | 0.0641 | - | - |
|
| ||||
| Race | ||||
| Caucasian | 0.72 (0.29, 1.79) | 0.552 | - | - |
| Other | Ref | |||
|
| ||||
| Annual Income | ||||
| ≤$30,000 | 1.36 (0.62, 3.01) | 0.4468 | - | - |
| $30,001 – $50,000 | 1.61 (0.71, 3.63) | 0.256 | - | - |
| >$50,000 | 0.96 (0.42, 2.15) | 0.9549 | - | - |
| No response | Ref | |||
|
| ||||
| Marital Status | ||||
| Married/partnered | 0.64 (0.37, 1.13) | 0.1372 | - | - |
| Other | Ref | |||
|
| ||||
| Employment | ||||
| Full-time | 2.65 (1.23, 5.73) | 0.0174 | 1.71 (1.1, 2.65) | 0.0173 |
| Part-time | 2.2 (0.91, 5.35) | 0.1038 | - | - |
| Retired | 1.98 (0.83, 4.72) | 0.1479 | - | - |
| Other | Ref | |||
|
| ||||
| Education | ||||
| < High School | 0.54 (0.13, 2.21) | 0.4298 | - | - |
| High School grad | 1.3 (0.55, 3.05) | 0.5632 | - | - |
| Trade school/ Some college | 1.41 (0.64, 3.07) | 0.4228 | 1.58 (1.03, 2.41) | 0.0345 |
| College grad | 0.97 (0.42, 2.22) | 0.9459 | - | - |
| Postgraduate | Ref | |||
|
| ||||
| Health Insurance | ||||
| Yes | 0.37 (0.16, 0.85) | 0.0251 | 0.4 (0.2, 0.83) | 0.013 |
| No | Ref | |||
|
| ||||
| Mo's since Dx* | 1.42 (0.97, 2.08) | 0.0812 | - | - |
|
| ||||
| Mo's since end of Tx* | 0.7 (0.47, 1.03) | 0.0807 | - | - |
|
| ||||
| Surgery | ||||
| Lumpectomy | 1.18 (0.53, 2.6) | 0.7253 | - | - |
| Mastectomy | 0.74 (0.36, 1.52) | 0.3933 | - | - |
| Bilateral mastectomy | Ref | |||
|
| ||||
| Chemotherapy | ||||
| Yes | 0.74 (0.43, 1.27) | 0.3011 | - | - |
| No | Ref | |||
|
| ||||
| Radiation Therapy | ||||
| Yes | 0.53 (0.28, 0.99) | 0.0642 | - | - |
| No | Ref | |||
|
| ||||
| Hormonal Therapy | ||||
| Yes | 0.69 (0.45, 1.08) | 0.1253 | 0.65 (0.42, 0.99) | 0.0433 |
| No | Ref | |||
|
| ||||
| Depression CES-D* | 0.99 (0.7, 1.42) | 0.9618 | - | - |
|
| ||||
| MOS Overall Social Support* | 1.33 (1.02, 1.74) | 0.0468 | - | - |
|
| ||||
| SF-36 PCS * | 0.79 (0.62, 1) | 0.0669 | - | - |
|
| ||||
| SF-36 MCS * | 0.68 (0.49, 0.96) | 0.0387 | 0.73 (0.6, 0.89) | 0.0018 |
|
| ||||
| Fit statistics | ||||
| AIC | 683.924 | 673.059 | ||
| -2LogLikelihood (model parameters)† | 631.924 (26) | 663.059 (5) | ||
Notes: AIC, Akaike Information Criterion. Smaller values indicate a better trade-off between the accuracy of a model and the number of predictors included in the model
Hazard ratio for a standard deviation increase
Used to test the difference in fit between models: χ2(21)=31.135, P=0.0714
Copyright, The Authors, 2013
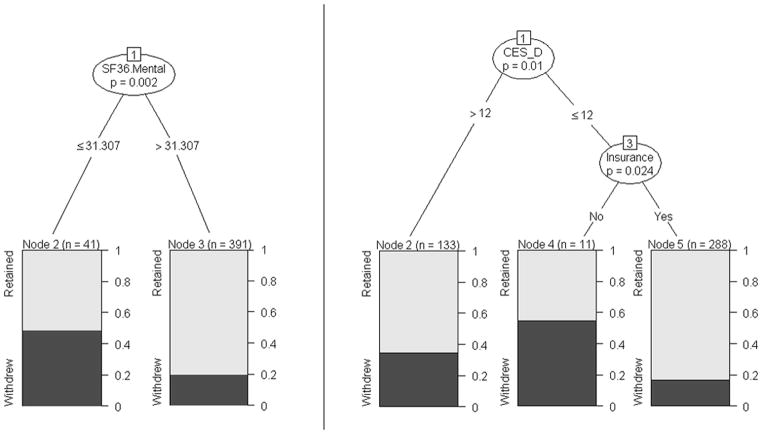
An initial exploratory classification tree model indicated that lower mental health at baseline was a characteristic strongly associated with the risk of attrition (Figure 2, left panel). Approximately 49% of participants with SF-36 MCS scores at or below 31.307 dropped out, compared to 20.5% among those with MCS scores greater than 31.307. Because computing norm scores for the SF-36 v1 requires specialized scoring algorithms, using this scale as a screening device to identify rural participants at risk for attrition may not be practical. However, a strong association between the CES-D and the SF-36 MCS scores was observed (Pearson r= −0.77, p<.0001). Thus, a second exploratory classification tree model was fitted after removing the SF-36 MCS scores from the pool of predictors.
Figure 2.
Classification Tree Models for Attrition Proportion
This second model (Figure 2, right panel) used baseline CES-D scores and health insurance status to identify rural breast cancer survivors at risk for attrition. Approximately 35% of participants with higher levels of depressive symptomatology (i.e., CES-D scores greater than 12) dropped out of the study. However, 17% of participants reporting lower levels of depressive symptomatology (i.e., CES-D scores less than or equal to 12) and health insurance dropped out compared with 54% of participants reporting lower levels of depressive symptomatology and no health insurance.
Discussion
Outcomes from this secondary analysis of RBCS data have implications for future work in attrition among the rurally underserved, and may inform the design of future post-treatment support service design. Findings from the time-to-event modeling indicated that rural breast cancer survivors at risk for early attrition from a psychoeducational program had the following characteristics: lower mental health (that was strongly associated with higher depressive symptomatology), lack of health insurance, full time employment, education at trade school/some college level, and no hormonal therapy. However, across the differential testing and modeling analyses, the two baseline characteristics that robustly predicted higher attrition were lower mental health and lack of health insurance.
Forty-nine percent of participants reporting lower mental health (Figure 2, left panel) dropped out of the study. This significant predictor of attrition supports previous work by other investigators (Bambs et al. 2013; Clough-Gorr et al 2008; Ribisl et al., 1996; Young et al, 2006). Bambs, in particular, found that depressive symptomatology and lower number of social networks were associated with attrition. To our knowledge, this is the first study to report lower mental health as a predictor of attrition specifically among rural residents. While Young et al (2006) included rural residents in their study population, they did not specifically separate rurality as a predictor. It may be that lower mental health increased the burden of daily activities and mental resources leaving less time and availability to remain engaged and participate in a longitudinal research study.
Lack of health insurance was the second major predictor of attrition in the RBCS. Bambs et al (2013), in their prospective study of cardiovascular prevention, also found that lack of health insurance was also reported as a significant predictor of attrition. Young et al (2006) and Clough-Gorr et al (2008) did not specifically determine a lack of health insurance, but rather that inadequate finances and financial difficulties were associated with attrition. Costs for medical follow-up and routine cancer surveillance such as mammography, blood studies, and DEXA scans may require continued employment to maintain health insurance coverage which may take precedence over a rural breast cancer survivor’s ability or desire to remain in a research study over time.
Those who dropped out of the present study reported higher depressive symptomatology. While depressive symptomatology and lack of health insurance were each independent predictors of attrition, the combination of the two characteristics significantly increased the likelihood of attrition. Nearly three times the proportion of RBCS participants reporting higher depressive symptomatology dropped out if they had no health insurance (54%) compared with those also reporting depressive symptomatology, yet having health insurance (17%) (Figure 2, right panel). In a previous study of urban breast cancer survivors, findings showed that the combination of worry about health insurance and out of pocket costs was problematic (the Authors, 2012). The authors found a significant increase in insurance premiums was reported by breast cancer survivors within the first year of cancer treatment, and an increase in economic events was significantly associated with poor quality of life (the Authors, 2012). A difficult reality for some cancer survivors is that lack of health insurance added economic burden to out of pocket costs, particularly among those with lower income (Pisu, Azuero, Meneses, Burkhardt, & McNees, 2011).
Full time employment, education at the trade school/some college level, and no hormonal therapy were associated with attrition in the time-to-event models. Full time employment and/or return to full time work status after breast cancer treatment may take priority leaving less available time for continued study participation. Alternatively, the demands of full time employment may have spurred survivors to move on with their lives after treatment ended.
The RBCS showed that lower education predicted attrition among rurally underserved breast cancer survivors. Findings support previous work by Chatfield et al (2005) and Haring et al (2009) who also found that lower education predicted attrition in their longitudinal epidemiologic observation studies. Study findings are similar to Clough-Gorr et al (2008) who identified that hormonal therapy was associated with attrition. However, in their study, receipt of hormonal therapy was associated with advanced disease and higher likelihood of attrition.
Contrary to other longitudinal studies with the elderly, older age was not associated with attrition in the RBCS study. Our findings are consistent with those of Van Beijsterveldt and colleagues (2002) who did not find higher attrition among older participants. They attributed the age discrepancy to having relatively healthy older adults who could participate and compliance-promoting measures to maintain retention in their study.
Implications and Future Considerations
The challenges faced over the course of this study provided valuable information concerning how to manage attrition in future work with rural residents and in breast cancer survivorship research.
Ribisl et al (1996) categorized attrition into two areas: participant characteristics and study characteristics. Participant characteristics include demographic, social, physical, and mental health features that are specific to the study population (Ribisl et al. 1996). We recommend that investigators start to document and report participant characteristics associated with attrition in their longitudinal observational and interventional studies. Reporting attrition data will aid in improving our conceptual understanding, and can further determine baseline characteristics of attrition. The authors proposed a beginning model conceptualizing the characteristics of attrition. Additional work in conceptual development through empirical findings that detail the relationship between attrition and recruitment, enrollment, and retention in longitudinal studies is warranted.
Second, reports of attrition patterns occurring in longitudinal studies particularly those who are hard to reach such as rural residents and other underserved populations are extremely vital. Planned recruitment and oversampling of participants with baseline study characteristics that predict attrition such as higher depressive symptomatology and lack of health insurance, as was found in the present study, may be considered to potentially manage attrition. Chatfield et al (2005) also suggested proxy interviews to help reduce attrition.
Study characteristics include design issues, methodologic strategies, and analytic schemes (Ribisl et al. 1996). Study characteristics are largely under the control and oversight of the researcher who can actively implement retention strategies to reduce future attrition. Fayter et al., (2007) suggested that prospective monitoring of study characteristics to manage and maintain study retention may help reduce attrition bias over time. Finally, Deeg (2002) suggested that attrition must be monitored for several reasons. First, the reasons for attrition can change over time in a longitudinal study which may ultimately influence estimates of change. Second, in intervention studies, attrition can still reduce power. Thus, attrition should continue to be monitored.
Strengths and Limitations
Strengths of this study include a population-based sample of rural breast cancer survivors. Previous studies have not reported attrition specifically in rural residents. A limitation is that the authors acknowledge use of the common definition of attrition which is tied to study endpoint. However, in longitudinal studies there are other important concerns and other questions, such as the immediacy versus durability (or sustainability) of effects over time. Such analyses are beyond the scope of the present work and remain an important topic of future investigation.
Conclusion
Attrition is an expected outcome in any longitudinal study. Gaining an understanding of demographic, social, treatment, physical healthy, mental health and other characteristics of study participants enrolled in longitudinal studies can help identify those at risk of early attrition and dropout. Our findings showed that lower mental health and lack of health insurance together were significant predictors of retention among rural breast cancer survivors. These defining attrition characteristics should also be considered when designing future post-treatment support services. Since more than 30% of women reside in rural areas, understanding and improving methods to retain rural breast cancer survivors and their participation in cancer control research are warranted. The benefits could be realized not only in terms of richer data; but also support services that are more responsive to women who exhibit the salient characteristics articulated in the present study versus those who do not exhibit those characteristics.
Acknowledgments
The authors are indebted to our breast cancer survivor participants; and also thank research team members: Silvia Gisiger-Camata, Madeline Harris, Lauren Hassey, Ann Wooten, and Ziqin Yang.
Funding source: National Cancer Institute, RO1CA-120638-07
Footnotes
Disclosure: The Florida cancer incidence data used in this report were collected by the Florida Cancer Data System under contract with the Department of Health (DOH). The views expressed herein are solely those of the author(s) and do not necessarily reflect those of the contractor or DOH.
References
- Allison P. Survival analysis using SAS: A practical guide. 2. Cary, North Carolina: SAS Institute Inc; 2010. [Google Scholar]
- American Cancer Society. Cancer Facts & Figures, 2013. 2013 Retreived on September 9, 2013, from http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-036845.pdf.
- Transition from treatment to survivorship: effects of a psychoeducational intervention on quality of life in breast cancer survivors. Oncology Nursing Forum. 2007;34(5):1007–016. doi: 10.1188/07.ONF.1007-1016. Authors. 334345R3225M1702 [pii] [DOI] [PubMed] [Google Scholar]
- Does economic burden influence quality of life in breast cancer survivors? Gynecologic Oncology. 2012;124(3):437–443. doi: 10.1016/j.ygyno.2011.11.038. Authors. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Authors. Applied Nursing Research. 2013. Sep 11, Research strategies to retain rural breast cancer survivors. pii: S0897–1897(13)00075-X. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Authors. Recruiting and enrolling rural breast cancer survivors in cancer control research. (under review) [Google Scholar]
- Bambs CE, Kip KE, Mulukutla SR, Aiyer AN, Johnson C, McDowell LA, Matthews K, Reis SE. Sociodemographic, clinical, and psychological factors associated with attrition in a prospective study of cardiovascular prevention: the Heart Strategies Concentrating on Risk Evaluation study. Annals of Epidemiology. 2013;23(6):328–333. doi: 10.1016/j.annepidem.2013.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baquet CR, Commiskey P, Daniel Mullins C, Mishra SI. Recruitment and participation in clinical trials: socio-demographic, rural/urban, and health care access predictors. Cancer Detection and Prevention. 2006;30(1):24–33. doi: 10.1016/j.cdp.2005.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolen S, Tilburt J, Baffi C, Gary TL, Powe N, Howerton M, Bass E. Defining “success” in recruitment of underrepresented populations to cancer clinical trials: moving toward a more consistent approach. Cancer. 2006;106(6):1197–1204. doi: 10.1002/cncr.21745. [DOI] [PubMed] [Google Scholar]
- Clough-Gorr KM, Fink AK, Silliman RA. Challenges associated with longitudinal survivorship research: attrition and a novel approach of re-enrollment in a 6-year follow-up study of older breast cancer survivors. Journal of Cancer Survivorship. 2008;2:95–103. doi: 10.1007/s11764-008-0049-y. [DOI] [PubMed] [Google Scholar]
- Chatfield MD, Brayne CE, Matthews FE. A systematic literature review of attrition between waves in longitudinal studies in the elderly shows a consistent pattern of dropout between differing studies. Journal of Clinical Epidemiology. 2005;58(1):13–19. doi: 10.1016/j.jclinepi.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Cook TD, Campbell DT. Quasi-experimentation: design and analysis issues for field settings. Boston, MA: Houghton-Mifflin; 1979. The conduct of randomized experiements; pp. 341–386. [Google Scholar]
- de Graaf R, van Dorsselaer S, Tuithof M, Ten Have M. Sociodemographic and psychiatric predictors of attrition in a prospective psychiatric epidemiological study among the general population. Result of the Netherlands Mental Health Survey and Incidence Study-2. Comprehensive Psychiatry. 2013 doi: 10.1016/j.comppsych.2013.05.012. [DOI] [PubMed] [Google Scholar]
- Deeg DJH. Attrition in longitudinal population studies: Does it affect the generalizability of the findings? An introduction to the series. Journal of Clinical Epidemiology. 2002;55(3):213–215. doi: 10.1016/S0895-4356(01)00472-3. Pii S0895-4356(01)00472-3. [DOI] [Google Scholar]
- Demark-Wahnefried W, Bowen DJ, Jabson JM, Paskett ED. Scientific bias arising from sampling, selective recruitment, and attrition: the case for improved reporting. Cancer Epidemiology, Biomarkers, & Prevention. 2011;20(3):415–418. doi: 10.1158/1055-9965.EPI-10-1169. [DOI] [PubMed] [Google Scholar]
- Everitt BHT. A handbook of statistical analyses using R. 2. Boca Raton, FL: Chapman & Hall/CRC; 2009. [Google Scholar]
- Fayter D, McDaid C, Eastwood A. A systematic review highlights threats to validity in studies of barriers to cancer trial participation. Journal of Clinical Epidemiology. 2007;60(10):990–1001. doi: 10.1016/j.jclinepi.2006.12.013. [DOI] [PubMed] [Google Scholar]
- Florida Department of Health. Vital Statistics Annual and Provisional Report: Population. 2007 Retrieved October 15, 2012 from http://www.flpublichealth.com/VSBOOK/VSBOOK.aspx.
- Ford JG, Howerton MW, Lai GY, Gary TL, Bolen S, Gibbons MC, Bass EB. Barriers to recruiting underrepresented populations to cancer clinical trials: a systematic review. Cancer. 2008;112(2):228–242. doi: 10.1002/cncr.23157. [DOI] [PubMed] [Google Scholar]
- Haring R, Alte D, Volzke H, Sauer S, Wallaschofski H, John U, Schmidt CO. Extended recruitment efforts minimize attrition but not necessarily bias. Journal of Clinical Epidemiology. 2009;62(3):252–260. doi: 10.1016/j.jclinepi.2008.06.010. [DOI] [PubMed] [Google Scholar]
- Hothorn T, Hornik K, Zeileiswere A. Unbiased recursive partitioning: A conditional inference framework. Journal of Computational and Graphical Statistics. 2006;15(3):651–674. [Google Scholar]
- Lee CS, Hayes RB, McQuaid EL, Borrelli B. Predictors of retention in smoking cessation treatment among Latino smokers in the Northeast United States. Health Education Research. 2010;25(4):687–697. doi: 10.1093/her/cyq010. [DOI] [PubMed] [Google Scholar]
- Marcellus L. Are we missing anything? Pursuing research on attrition. Canadian Journal of Nursing Research. 2004;36(3):82–98. [PubMed] [Google Scholar]
- Paskett ED, Cooper MR, Stark N, Ricketts TC, Tropman S, Hatzell T, Atkins J. Clinical trial enrollment of rural patients with cancer. Cancer Practice. 2002;10(1):28–35. doi: 10.1046/j.1523-5394.2002.101006.x. [DOI] [PubMed] [Google Scholar]
- Pisu M, Azuero A, Meneses K, Burkhardt J, McNees P. Out of pocket cost comparison between Caucasian and minority breast cancer survivors in the Breast Cancer Education Intervention (BCEI) Breast Cancer Research and Treatment. 2011;127(2):521–529. doi: 10.1007/s10549-010-1225-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R-statistical-software. R Foundation for Statistical Computing. 2008. R statistical software v2.15.00. [Google Scholar]
- Radloff IS. The CES-D Scale: a self-report depression scale for research in the general population. Applied Psychological Mesurement. 1977;1:385–401. [Google Scholar]
- Ribisl KM, Walton MA, Mowbray CT, Luke DA, Davidson WS, Bootsmiller BJ. Minimizing participant attrition in panel studies through the use of effective retention and tracking strategies: Review and recommendations. Evaluation and Program Planning. 1996;19(1):1–25. doi: 10.1016/0149-7189(95)00037-2s. [DOI] [Google Scholar]
- Robinson KA, Dennison CR, Wayman DM, Pronovost PJ, Needham DM. Systematic review identifies number of strategies important for retaining study participants. Journal of Clinical Epidemiology. 2007;60(8):757–765. doi: 10.1016/j.jclinepi.2006.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SASv9-3. Cary, North Carolina: SAS Institute, Inc; 2010. [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS social support survey. Social Science & Medicine. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Su X, Meneses K, McNees P, Johnson W. Interaction trees: exploring the differential effects of an intervention programme for breast cancer survivors. Journal of the Royal Statistical Society: Series C (Applied Statistics) 2011;60(3):457–474. doi: 10.1111/j.1467-9876.2010.00754.x. [DOI] [Google Scholar]
- Van Beijsterveldt CE, van Boxtel MP, Bosma H, Houx PJ, Buntinx F, Jolles J. Predictors of attrition in a longitudinal cognitive aging study: the Maastricht Aging Study (MAAS) Journal of Clinical Epidemiology. 2002;55(3):216–223. doi: 10.1016/s0895-4356(01)00473-5. [DOI] [PubMed] [Google Scholar]
- Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- Whitten-Goldstein K. Science Meets Reality: Recruitment and retention of women in clinical studies and the critical role of relevance. Bethesda, MD: NIH Office of Research on Women’s Health; 2003. Rural Populations: Challenges in recruitment , retention, and relevance; pp. 121–123. [Google Scholar]
- Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annual Review of Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
- Young AF, Powers JR, Bell SL. Attrition in longitudinal studies: who do you lose? Austrailian and New Zealand Journalof Public Health. 2006;30(4):353–361. doi: 10.1111/j.1467-842x.2006.tb00849.x. [DOI] [PubMed] [Google Scholar]