Abstract
Objective
The Subaxial Injury Classification (SLIC) system has been developed to improve injury classification and guide surgical decision making yet clinical validation remains necessary.
Methods
We evaluated the validity and safety of the SLIC system prospectively in patients treated for subaxial cervical spine trauma (SCST) between 2009 and 2012. Patients with four or more points were surgically treated, whereas patients with less than 4 points were conservatively managed.
Outcome measures
Neurological status was assessed as the primary outcome of successful treatment.
Results
Non-surgical group – Twenty-three patients were treated non-surgically, 14 (61%) of them with some follow-up at our institution. Follow-up ranged from 3 to 5 months (mean of 4.42; median 4). The SLIC score ranged from 0 to 6 points (mean and median of 1). One patient with a SLIC of 6 points refused surgery. Surgical group: Twenty-five patients were operated, but follow-up after hospital discharge was obtained in 23 (92%) patients (range from 1 to 24 months, mean of 5.82 months). The SLIC score in this group ranged from 4 to 9 points (mean and median of 7). No patients had neurological worsening. Eight of 13 patients with incomplete deficits had some improvement in American Spinal Injury Association score.
Conclusions
This is the first prospective application of the SLIC system. With regard to our primary outcome, neurological status, the SLIC system was found to be a safe and effective guide in the surgical treatment of SCST.
Keywords: Spinal cord injuries, Subaxial cervical spine trauma, SLIC
Introduction
The Subaxial Injury Classification (SLIC) and scoring system has been recently proposed as a guide to treatment of the subaxial cervical spine trauma (SCST), from C3 to C7.1 This new system proposes three major injury characteristics as indicators of treatment: (i) Injury morphology as determined by the pattern of spinal column disruption on available imaging studies; (ii) integrity of the discoligamentous soft tissue complex (DLC) represented by both anterior and posterior ligamentous structures as well as the intervertebral disc and posterior supporting ligaments; and (iii) the patient's neurological status. These three injury characteristics are recognized as predictors of clinical outcome and influence treatment recommendations.
Within each of the three categories, subgroups have been identified and graded from least to most severe.1 Morphology is graded: 0, no abnormality; 1, compression; 2, burst; 3, distraction; and 4, translation or rotation. The integrity of the DLC components (intervertebral disc, anterior and posterior longitudinal ligaments, interspinous ligaments, facet capsules, and ligamentum flavum) is classified as intact (0), indeterminate (1), and disrupted (2). Finally, the neurological status, the third component of the system and probably the most influential predictor of treatment, receives the following: intact (0), root injury (1), complete (2), incomplete (3), and persistent compression receives an extra +1 point. As such, the presence of an incomplete neurologic injury, particularly in the presence of ongoing root or cord compression leads to the highest point score.
Surgical versus non-surgical treatment is suggested by a threshold value of the SLIC severity score. If the total score is <4 (1–3), non-operative treatment is recommended. If the total is ≥5, operative treatment is recommended. This treatment may consist of realignment, neurological decompression (if indicated), and stabilization.1 Cases with a total score of 4 may be treated either operatively or non-operatively based upon surgeon and patient preferences and considering confounding factors, as the presence of ankylosing spondylitis, diffuse idiopathic hyperostosis, osteoporosis, previous surgery, and degenerative disease.
Given the potential benefits of this new system, prospective application and assessment of the SLIC for validity and safety is needed. The purpose of this paper is to evaluate the results of a series of consecutively treated patients based on the prospective application of the SLIC system.
Methods
We analyzed all the patients older than 17 years of age consecutively treated for SCST from 2009 to 2012 by one of the authors (A.F.J.). The SLIC system was prospectively applied to all patients at the time of initial evaluation. Patients with a SLIC score of four or more points were referred for surgical treatment. We adopted a threshold of four points for surgical treatment because this group included patients with central cord syndrome (most of them with four points in the score) and our clinical practice routinely includes surgical treatment for these injuries. Clinical and radiological data were evaluated, classifying the injury according to American Spinal Injury Association (ASIA) neurological status and the SLIC score system. The neurological status, based on the ASIA Impairment Scale (AIS), was the main outcome measurement of treatment success.2
Demographic data including age and sex were recorded. Injury and treatment details were also recorded, including fracture level, surgical approach, and complications. Follow-up included clinical assessment of the neurological status, at least on post-operatory computed tomographic scan with reconstruction to check the instrumentation and serial plain radiographs. Institutional ethical committee approval was obtained to perform this study (1297/2011). There were no external funding sources.
Results
A total of 48 cases were treated between 2009 and 2012. Thirty-seven had some follow-up and were included in this study: 14 in the non-surgical and 23 in the surgical group.
Non-surgical group – 14 patients
There were 23 cases treated non-surgically with a rigid cervical collar (Table 1). Two patients with severe traumatic brain injury died during hospital admission and the remaining seven patients were lost to follow-up. After excluding these nine patients, 14 patients (61%) had some follow-up in our institution and were reported in this study. Follow-up ranged from 3 to 5 months (mean of 4.42; median 4). Of these, age ranged from 24 to 75 years (mean 36.5, median 29). Twelve (85.7%) were male and 2 (14.2%) were female. Regarding the level of injury, three patients (21.4%) had the injury at C4, three (21.4%) at C5, three at C6 (21.4%), and five at C7 (35.7%). All the patients were neurologically intact (ASIA E). The SLIC score in this group ranged from 0 to 6 points (mean of 1 and median of 1). One patient with unilateral locked facet joint had a SLIC of 6 points (more than 3 points) but refused surgery and was treated with a cervical collar. At 5 months of follow-up he had continued axial cervical pain but did not want surgery. An illustrative case treated non-surgically was present in Fig. 1.
Table 1 .
Distribution of the 14 patients conservatively treated patients according to age and the SLIC system – all of them were neurologically intact
| Age | SLIC score | |
|---|---|---|
| Mean (range) | 36.5 | 1.07 |
| Median | 29 | 1 |
| Range | 24–75 | 0–6 |
Figure 1 .
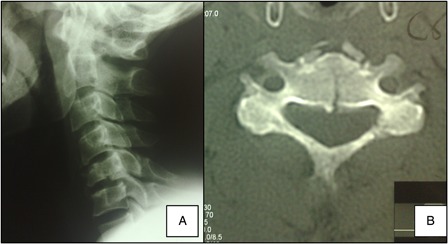
A 51-year-old man was involved in a car accident. He had a C5 linear burst fracture without facet joints injuries or dislocations (A and B). He was also neurologically intact with mild cervical pain. His SLIC was 2 points (burst) for morphology + 0 points for DLC status + 0 points for neurological status – total of 2 points. He underwent conservative treatment with a cervical collar for 8 weeks and was totally asymptomatic after 4 months of follow-up.
Surgical group – 23 patients
Data for the 25 cases of cervical spine trauma treated surgically based on the SLIC score are presented in Table 2. Follow-up was obtained in 23 patients, ranging from 1 to 24 months (mean of 5.82; median 5). Two patients were lost to follow-up and were not included in our results: one was transferred for another hospital at day 2 after surgery and one patient died during the same hospital admission (sepsis and concomitant traumatic brain injury). Patients’ age ranged from 23 to 71 years (mean 41.2, median 43). Twenty (87%) were male and three (13%) were female.
Table 2 .
Clinical and neurological data obtained in our surgical series of 25 patients operated based on the SLIC score
| Age | SLIC score | |
|---|---|---|
| Mean (range) | 41.2 | 7 |
| Median | 43 | 7 |
| Range | 23–71 | 4–9 |
Regarding the level of injury, four patients (17%) had the trauma at C3, five (21%) at C4, eight at C5 (34%), and six at C6 (26%). In 12 patients the trauma was caused by motor vehicle accidents and seven patients fallen from the height. In one case each, we had a patient struck by a car, one with a sport injury (martial arts), one direct trauma, and one dive into shallow water.
Preoperatively, 10 patients (43%) were ASIA E, 5 (22%) ASIA D, 4 (17%) ASIA C, 2 (8%) ASIA B, and 2 (8%) ASIA A. No patients had neurological worsening. At the final follow-up, the ASIA score was 13 (52%) ASIA E, 6 (24%) ASIA D, 2 (8%) ASIA C, and 2 (8%) ASIA A (the two lost to follow-up were both ASIA A). Although the two patients with ASIA classification of A maintained their ASIA status, both demonstrated upper extremity motor improvement during the follow-up. A total of 8 of 11 (72%) patients with incomplete neurological deficit (ASIA B–D) improved their ASIA status during the follow-up (Table 3).
Table 3 .
Neurological status of the 23 patients surgically treated distributed according to preoperative status and last follow-up evaluation
| ASIA | Pre | Post |
|---|---|---|
| A | 2 | 2 |
| B | 2 | – |
| C | 4 | 2 |
| D | 5 | 6 |
| E | 10 | 13 |
| 23 | 23 |
The SLIC score in this group ranged from 4 to 9 points (mean and median of 7). The two patients with a SLIC of 4 points had a central cord syndrome. Sixteen patients (64%) had rotational injuries, four (18.1%) distractive injuries and two (9%) had burst fractures. One patient had a traumatic disk herniation.
Twelve patients underwent an anterior approach, nine a posterior approach and two a combined approach, with the objectives of spinal realignment, stabilization, and decompression. Only one patient underwent surgical treatment in the first 24 hours after trauma. The time for decompression and surgery range from 1 to 14 days (mean of 4 days) and no preoperative traction was used in any case of this series.
Two patients had wound infections requiring debridement, both initially treated with an instrumented posterior fusion. One patient had a deep venous thrombosis prior to surgery and received an inferior vena cava filter prior to surgical treatment.
An illustrative case treated surgically was present in Fig. 2.
Figure 2 .
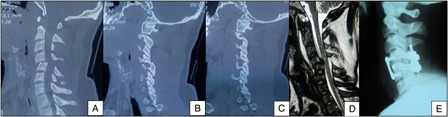
A 23-year-old man had a sport injury (judo fight) and presented neurologically intact. (A) Computed tomographic scan with posterior dislocation of C4 into the spinal canal. (B) A locked C4–5 right facet joint and (C) A perched C4–5 left facet joint. (D) Sagittal T2 MRI with a hipersignal in the spinal cord. The SLIC was 4 points for morphology (rotation) + 2 points for DLC injury + 0 for neurological status = total of 6 points – surgical treatment was performed. The patient underwent an anterior discectomy without reduction, followed by a posterior direct reduction and C4–5 lateral mass fixation with autograft and then anterior arthrodesis with a titanium cage with autologous bone graft and plating.
Discussion
This study is the first reported prospective application of the SLIC system in sub-axial cervical trauma. In our consecutive series of 37 patients with SCST, the prospective application of the SLIC classification system to define injuries and guide surgical decision making was identified as being safe and effective at preventing neurological deterioration and, in most patients, lead to clinically relevant improvements in neurological function.
Similar to other authors, most of our patients were male and young adults.3,4 The high rate of rotational/translational injuries in this series, with 16 (64%) patients, can be explained because as our tertiary trauma center is responsible for high energy and complex trauma cases.
Although we have a relative short follow-up, ranging from 1 to 24 months, the majority of significant neurological improvement after spinal cord injury occurs in the first 6 months after trauma.5–7 During our follow-up, none of our patients had neurological deterioration, attesting to the security and validity in the use of the clinical use of the SLIC system to both surgical and non-surgical treatment. Patients with incomplete deficits presented improvements in ASIA score in 72%. Patients with ASIA A injuries, excepting those two lost to follow-up, had improvements in motor strength above their neurological level but did not convert to incomplete spinal cord injuries.
There were two patients with central cord syndrome, with SLIC score of four points each, both with neurological improvement after surgery; one of them, despite his improvement, maintained the same AIS grade (D). While there is some literature to suggest that patients with central cord syndrome can improve without surgical treatment, there is additional evidence that ultimate neurological and functional outcomes are poor.8,9 As such we routinely indicate patients with central cord syndrome for surgical management. Once patients with a SLIC of 4 points can be treated either conservatively or surgically according to the proponents of the system, multi-center prospective studies would be of value to clarify the best treatment option in these cases.
Limitations
Our study has several limitations: its small sample size, single surgeon experience, and the limited clinical follow-up of the subjects. However, our study demonstrates validity, safety, and efficacy regarding the clinical use of the SLIC system and neurological preservation. The limited follow-up could result in under-reporting of failures and complications in the both groups. In our coverage area in Brazil, our institution is the primary tertiary surgical hospital. As such, we believe that individuals who failed conservative care and require delayed surgical treatment would have been seen and treated at our institution. None were identified. Nevertheless, patients treated conservatively did have incomplete data to report.
The small number of patients enrolled and the single institution involved in this study may limit generalizability of the findings. We had previously reported a prior clinical study from the trauma database at the University of Utah, Salt Lake City, UT, USA, wherein the SLIC system was retrospectively applied to 24 patients treated surgically for SCST. In this group we identified a concordance of SLIC score with treatment in 92% of cases.10 This demonstrated validity served as a foundation for our prospective application of the system. It may be practical, therefore, for other institutions to retrospectively review treated previous patients prior to prospectively applying the SLIC system. This may identify educational opportunities as well as updates to clinical practice at each individual institution.
Conclusions
Our study is the first prospective application of the SLIC system to a consecutive series of patients. It suggests that the SLIC system can be a useful clinical tool to help the treating physician in both surgical and non-surgical decision making. Patients in both treatment groups were treated successfully with no neurological deterioration. Nonetheless, larger prospective studies are needed to clarify the value of the SLIC system according to patient reported outcomes and cost efficiency.
References
- 1.Vaccaro AR, Hulbert RJ, Patel AA, Fisher C, Dvorak M, Lehman RA Jr, et al. The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976) 2007;32(21):2365–74 [DOI] [PubMed] [Google Scholar]
- 2.Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE, et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003;26(1):50–6 [DOI] [PubMed] [Google Scholar]
- 3.Wu Q, Li YL, Ning GZ, Feng SQ, Chu TC, Li Y, et al. Epidemiology of traumatic spinal cord injury in Tianjin, China. Spinal Cord 2011;49(3):386–90 [DOI] [PubMed] [Google Scholar]
- 4.Lenehan B, Street J, Kwon BKNoonan VZhang HFisher CG, et al. The epidemiology of traumatic spinal cord injury in British Columbia, Canada. Spine (Phila Pa 1976) 2012;37(4):321–9 [DOI] [PubMed] [Google Scholar]
- 5.Bracken MB, Shepard MJ, Collins WF, Holford TR, Young W, Baskin DS, et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury. Results of the Second National Acute Spinal Cord Injury Study. N Engl J Med 1990;322(17):1405–11 [DOI] [PubMed] [Google Scholar]
- 6.Bracken MD, Shepard MJ, Holford TR, Leo-Summers L, Aldrich EF, Fazl M, et al. Administration of methylprednisolone for 24 or 48 hours or tirilazad mesylate for 48 hours in the treatment of acute spinal cord injury. Results of the Third National Acute Spinal Cord Injury Randomized Controlled Trial. National Acute Spinal Cord Injury Study. JAMA 1997;277(20):1597–604 [PubMed] [Google Scholar]
- 7.Geisler F, Coleman W, Grieco G, Poonian D. The Sygen multicenter acute spinal cord injury study. Spine (Phila Pa 1976) 2001;26(24):87–98 [DOI] [PubMed] [Google Scholar]
- 8.Chen TY, Dickman CA, Eleraky M, Sonntag VK. The role of decompression for acute incomplete cervical spinal cord injury in cervical spondylosis. Spine (Phila Pa 1976) 1998;23(22):2398–403 [DOI] [PubMed] [Google Scholar]
- 9.Guest J, Eleraky MA, Apostolides PJ, Dickman CA, Sonntag VK. Traumatic central cord syndrome: results of surgical management. J Neurosurg 2002;97(1):25–32 [DOI] [PubMed] [Google Scholar]
- 10.Joaquim AF, Lawrence B, Daubs M, Brodke D, Patel AA. Evaluation of the subaxial injury classification system. J Craniovert Jun Spine 2011;2(2):67–72 [DOI] [PMC free article] [PubMed] [Google Scholar]


