Abstract
The association between housing and HIV has been widely demonstrated, although inquiry into HIV testing has been largely limited to the homeless. This study examines correlates of HIV testing within the past 6 months with housing stability and residential transience (moving 2 or more times in the past 6 months) among 620 low-income urban African Americans. Unstably housed and transient participants were more likely to participate in high-risk sex behaviors than stably housed participants and non-transient participants, respectively. In multivariate analyses, residential transience was positively associated with recent HIV testing; however, persons unstably housed were not more likely to have recently been tested for HIV despite their increased vulnerability and risk. While structural interventions are necessary to address the HIV disparities related to housing, increased community-based and mobile testing centers may be able to improve access to HIV testing among unstably housed.
Keywords: HIV testing, housing, transience, homeless
Introduction
Great benefits exist for HIV testing for identifying persons infected with HIV in the United States (US). Morbidity and mortality can be greatly reduced through the initiation of treatment with combination antiretroviral therapy (Panos et al., 2008); mother to child transmission can be significantly reduced during pregnancy (Mofenson, 2003); and HIV positive individuals can reduce the risk of transmitting the virus to others (Porco et al., 2004). As HIV infected individuals learn of their status, they often decrease their sexual risk behaviors, which also reduces transmission to others (Marks, Crepaz, Senterfitt, & Janssen, 2005). Conversely, the majority of incident cases of HIV have been hypothesized to be spread by people unaware of their serostatus (Mark, Crepaz, & Jenssen, 2006). Thus, it is well understood that HIV testing is important for treatment and care as well as prevention. Increasing the number of HIV-infected persons who are diagnosed and linked to effective treatment and support may significantly reduce new HIV infection over time (Campsmith, Rhodes, Hall, & Green, 2010). However, 20% of the estimated 1,178,350 adults and adolescents living with HIV in 2008 did not know they were infected, and persons of minority racial or ethnic status were more likely to be undiagnosed compared to Whites. For example, 21.4% of Blacks/African Americans were undiagnosed compared to 18.5% of Whites (CDC, 2011). Additionally, of all HIV infections diagnosed among African Americans, 31% were diagnosed with AIDS within one year. This is of great concern, as African Americans are more likely to become infected with, and die from, HIV/AIDS than any other ethnic or racial group in the US (CDC, 2010).
The HIV epidemic among African Americans is complex, but the disproportionate rates of lower socioeconomic status and poverty among African Americans enables individual- and structural-level risk factors for HIV and creates barriers to access for health care services (Laurencin, Christensen, & Taylor, 2008; Adimora & Schoenbach, 2005). Unstable housing and/or homelessness are important consequences of low socioeconomic status among African Americans, and housing has been associated with various high-risk sexual activities (Aidala, Cross, Stall, Harre, & Sumartojo, 2005; Weir, Bard, O'Brien, Casciato, & Stark, 2007; Corneil et al., 2006; Royse et al., 2000; Wenzel, Tucker, Elliot, & Hambarsoomians, 2007; Aidala, Lee, Garbers, & Chiasson, 2006)
Findings consistently demonstrate that homeless individuals, including those in living homeless shelters, have higher rates of HIV infection compared to general populations (Smereck & Hockman, 1998; Corneil et al., 2006; Culhane, Gollub, & Kuhn, 2001; Robertson et al., 2004), and that HIV and AIDS incidence is inversely associated with economic wellbeing, even across gender and racial/ethnic groups (Zierler et al., 2000; Hankins et al., 1998). When considering homelessness, unstable housing, and residential transience - defined here as moving two or more times in the past 6 months (German, Davey, & Latkin, 2007; Davey-Rothwell, German, & Latkin, 2008) – significant associations have been found between housing and HIV risk behaviors.
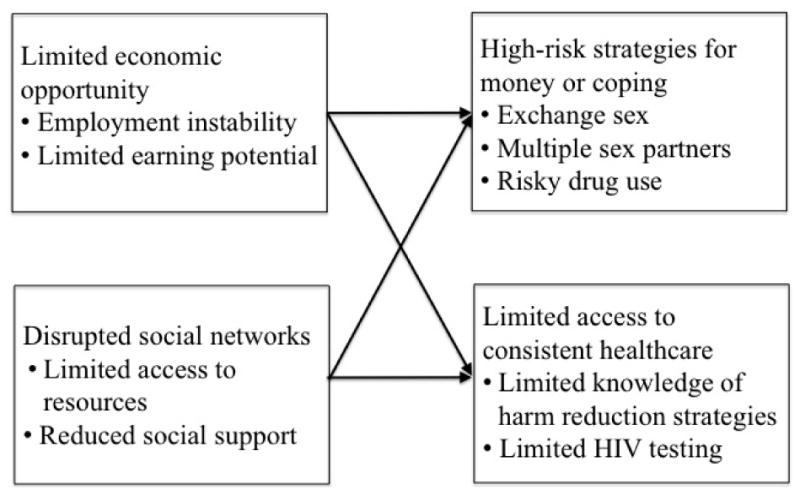
A number of possible mechanisms that may influence the sexual risk taking behaviors by persons unstably housed have been noted (Figure 1) that create barriers to the formation of stable partnerships (Browning & Olinger-Wilbon, 2003; Castel, 2000), chronic stress (Mizuno et al., 2003; Reilly & Woo, 2003), exposure to trauma and violence including victimization (Bourgois, 1998; Wenzel et al., 2004), and limited economic opportunity (Seagert & Evans, 2003; Shaw, 2004).
Figure 1. Potential Pathways Between Unstable Housing and Residential Transience and HIV Testing.
Housing stability has been associated with exchange sex (Aidala, et al., 2005; Weir et al., 2007; Corneil et al., 2006; Royse et al., 2000), multiple partners (Wenzel et al., 2007), and unprotected sex (Weir et al., 2007; Aidala et al., 2006). Weir and colleagues (2007) found that moving twice or more in 6 months was associated with unprotected sexual intercourse and exchanging sex for money or drugs. Among injection drug users, transience has been associated with sharing needles and attending shooting galleries (German et al., 2007). Finally, Davey-Rothwell and colleagues (2008) found that depression was more common among transient men and women.
National surveys have demonstrated that people with unstable housing have poorer access to health care than the general population with stable housing (Reid, Vittinghoff, & Kushel, 2008; Kushel, Gupta, Gee, & Haas, 2006), and past research has shown that having a regular source of medical care is one of the strongest predictors of access to health care services in general (Blindman, Grumbach, Osmond, Vranizan, & Stewart, 1996). Not surprisingly, therefore, having regular access to health care is an important predictor of HIV testing among homeless and low-income housing unit residents (Herndon et al., 2003; Tucker, Wenzel, Elliott, Hambarsoomian, & Golinelli, 2003). Herndon and colleagues (2003), for example, found that testing for HIV among homeless women was predicted by pregnancy in the past year and having a regular source of health care.
Investigations related to HIV testing among populations without stable housing have generally been limited to prevalence studies, testing feasibility studies, and less frequently research considering associations between HIV testing and housing among persons who are homeless and/or residing in homeless shelters. Since those lacking stable housing in general, and not just those who are currently homeless, are more likely to partake in high-risk HIV behaviors and may face numerous barriers to service utilization, an exploration of the associations of unstable housing and residential transience with HIV testing is warranted. Thus, the goal of this study is to evaluate the relationship between homelessness, housing stability, residential transience, and recent HIV testing among urban low-income African Americans.
Methods
This study utilized data from the CHAT Project, a social network based HIV/STI prevention study targeted at women in Baltimore, Maryland. The CHAT Project was designed to train women to become peer mentors, who would then discuss HIV and STI risk reduction strategies with their social network members. (For more details about the intervention see Davey-Rothwell, Tobin, Yang, Sun, & Latkin, 2011). Participants were recruited though targeted street outreach, flyers, and referrals from health clinics and community agencies (although only 1.5% of eligible index recruits were referred through agencies). Eligibility criteria for index participants included: 1) female, 2) between the ages of 18 and 55 years, 3) self-reported heterosexual sex in the past six months, and 4) have one of the following risk behaviors: more than one sex partner in the past six months, have a risky partner who engages in risky behavior (e.g. injection drug user, HIV positive partners, or male who had sex with other men), or snorted/sniffed or smoked heroin or cocaine. Index participants referred their social network members to the study. To be eligible as a network participant, the individual had to be 18 years or older and one of the following: injected drugs within the past six months, had sex with the index in the last 90 days, or the index felt comfortable discussing HIV and STIs with the network participant and interacted with that network participant at least several times a month. Network participants could be men or women.
Both index and network participants completed the same baseline survey, administered through trained interviewers and Audio Computer Assisted Software (ACASI), and were provided HIV antibody testing (OraSure HIV testing). Participants were compensated with $35 for completion of the visit. The Johns Hopkins Bloomberg School of Public Health Institutional Review Board approved the study protocol and materials. The current study focused on baseline data collected from September 2005 through July 2007. Participants were included in the analysis if they were African American, reported a date of last HIV test (or reported never having a HIV test), received the result of their last test if ever tested, and had never been told they were HIV positive. Participants were instructed to report the date of their last test prior to the survey; HIV test dates matching the survey date were excluded.
Measures
Socio-demographics
Socio-demographic questions assessed sex, educational attainment, current employment, income in the past 30 days, incarceration in past 6 months, current main sex partner, and depression. Depression was assessed using the Center for Epidemiologic Depression Scale (CES-D) (Radloff, 1977). A CES-D score of 16 or higher was used as a cutoff score for having a high level of depressive symptoms.
Housing
Four types of housing variables were assessed. First, participants were asked about their current housing situation. A participant's housing was considered stable if they lived in a house or apartment that they rented or owned. Housing was considered unstable if participants rented a room or space in someone else's house, stayed with someone else for free, or lived in a transitional, recovery, or drug treatment house, lived on the street, or stayed at two or more places a week. Participants were also asked the number of times they had moved in the past 6 months, and were considered transient if they had moved 2 or more times in the past 6 months (German et al., 2007; Davey-Rothwell et al., 2008).
HIV Risk
HIV risk was assessed through consideration of recent STI diagnosis, participant sexual and drug use behaviors, and participant's sexual partners' sexual and drug use behaviors. High risk sex behaviors included in this report are reporting more than one sexual partner in the past 9 months, exchanging sex in the 90 days, and having sex with a high-risk partner in the past 90 days. Exchange sex was defined as having sex in exchange for food, money, shelter, or drugs. High-risk sex partners were assessed by asking the participant about each sex partner in the past 90 days and identifying one or more partners with the following characteristics or behaviors: injects drugs, smokes crack, has sex with men, is HIV positive or has another STI. Partner characteristics and behaviors were known or suspected by the participant. High-risk drug use behaviors include injection drug use and use of heroin, crack or cocaine (any administration) in the past 6 months.
Health Service Utilization
Participants were asked where they most commonly go to receive health care services (e.g., public health department, community health clinic, VA). They were also asked how many times they saw a general doctor who treats a variety of illnesses or a primary care doctor for a check up in the past 6 months, and this was dichotomized as seeing a doctor in the past 6 months or not.
HIV Testing
Participants were asked when they were last tested for HIV, if they got the result of this test, the result of the test, and if this was their first HIV test. Testing was dichotomized in the analysis as tested within the past 6 months and last HIV test longer than 6 months ago or never tested.
Anayses
Univariate, bivariate, and multivariate analyses were conducted with SPSS Software (version18.0). Chi-squares and t-tests were conducted to consider the unadjusted bivariate relationship between the following groups: 1) stable vs. unstably housed, and 2) non-transient vs. transient. Two multivariate logistic regression models were constructed to examine the associations between unstable housing and transience with recent HIV testing, accounting for current homelessness and other covariates identified from the literature. Covariates included were sex, age, education, income, recent incarceration, depression, and utilization of health care services in the past 6 months. Interaction effects of dependent variables were tested. Since behaviors and other variables among the index and recruited network participants could be correlated with each other, all analyses used generalized estimating equations (GEE) to obtain odds ratios and confidence intervals, using the index and recruited network members as the cluster (Zeger & Liang, 1986).
Results
A total of 746 eligible participants completed the baseline survey. Of the 721 African Americans who completed the baseline survey, 97 reported being HIV-positive and 4 reported being HIV-negative but did not report an HIV date. Thus, 620 of these participants met the inclusion criteria for the current analysis. Women comprised 77.7% of the sample.
Hosuing Stability
Over half (58.5%) of the participants were unstably housed at the time of the survey. Socio-demographic characteristics, housing characteristics, HIV risk behaviors, access to healthcare, and HIV testing characteristics for the participants by housing stability are presented in Table 1. Unstably house participants were slightly younger (t = 2.15, p = 0.03), less likely to have an income greater than $500 in the past 30 days (χ2 = 45.8, p < 0.001), and were more likely to have been in jail or prison in the past 6 months (χ2 = 9.0, p = 0.003) compared to stably housed participants.
Table 1.
Comparison of participants based on housing stability among CHAT study participants, 2005-2007.
| Stable (n = 257) |
Unstable (n =363) |
Total (n = 620) |
Test statistica (p value) |
|
|---|---|---|---|---|
| Socio-demographics | ||||
| Sex: Female | 198 (77.0) | 284 (78.2) | 482 (77.7) | 0.12 (0.725) |
| Age, mean (sd) | 43.0 (8.7) | 41.4 (8.7) | 42.1 (8.8) | 2.15 (0.032) |
| Education: High school/GED | 144 (56.3) | 182 (50.4) | 326 (52.8) | 2.05 (0.153) |
| Employed full- or part-time | 64 (24.9) | 64 (17.6) | 128 (20.6) | 4.86 (0.028) |
| Income in past 30 days less than $500 | 80 (31.1) | 213 (58.7) | 293 (47.3) | 45.82 (<0.001) |
| In jail or prison in past 6 months | 24 (9.3) | 65 (17.9) | 89 (14.4) | 8.98 (0.003) |
| Currently has main sex partner | 200 (77.8) | 263 (72.5) | 463 (74.7) | 2.29 (0.130) |
| Depression score >= 16 | 184 (71.6) | 274 (75.5) | 458 (73.9) | 1.18 (0.278) |
| Housing | ||||
| Currently homeless | 0 (0.0) | 35 (9.6) | 35 (5.6) | 26.26 (<0.001) |
| Times moved in past 6 months, mean (sd) | 0.68 (6.3) | 0.96 (1.5) | 0.84 (4.2) | -0.70 (0.485) |
| HIV risk | ||||
| Diagnosed with nonHIV STI in past 9 months | 11 (4.3) | 44 (12.1) | 55 (8.9) | 11.44 (0.001) |
| Sex with >1 person in past 9 months | 117 (45.5) | 224 (61.7) | 341 (55.0) | 15.92 (<0.001) |
| Exchange sex in past 90 days | 43 (18.6) | 87 (26.6) | 130 (23.3) | 4.84 (0.028) |
| Injected drugs in past year | 11 (4.3) | 27 (7.4) | 38 (6.1) | 2.61 (0.106) |
| Used heroin, crack or cocaine in past year | 152 (82.6) | 276 (89.3) | 428 (86.6) | 4.54 (0.033) |
| Sex with high risk partner in past 90 days | 114 (44.4) | 191 (52.6) | 305 (49.2) | 4.11 (0.043) |
| Access to Health Care | ||||
| Usual source of health care | 15.85 (0.070) | |||
| Public health department | 7 (2.7) | 18 (5.1) | 25 (4.1) | |
| Community based clinic | 124 (48.6) | 175 (49.2) | 299 (48.9) | |
| Private doctor | 16 (6.3) | 20 (5.6) | 36 (5.9) | |
| Hospital clinic | 72 (28.2) | 65 (18.3) | 137 (22.4) | |
| Emergency room | 26 (10.2) | 53 (14.9) | 79 (12.9) | |
| Other | 10 (4.0) | 25 (6.9) | 35 (5.8) | |
| Seen a general or primary care doctor within the past 6 months | 175 (69.4) | 252 (70.2) | 427 (69.9) | 0.04 (0.842) |
| HIV Testing | ||||
| Ever tested for HIV | 251 (97.7) | 352 (97.0) | 603 (97.3) | 0.27 (0.601) |
| Tested for HIV only once | 53 (21.1) | 52 (14.8) | 105 (17.4) | 4.04 (0.045) |
| Time since last HIV test | 6.78 (0.079) | |||
| ≤ 6 months | 121 (47.1) | 201 (55.4) | 322 (51.9) | |
| 6-12 months | 40 (15.6) | 58 (16.0) | 98 (15.8) | |
| > 1 year | 90 (35.0) | 93 (25.6) | 183 (29.5) | |
| Received result of last HIV test | 197 (75.8) | 289 (82.1) | 486 (80.6) | 1.23 (0.268) |
χ2 test statistics are provided for dichotomous variables and t test statistics are provided for continuous variables
Unstably housed participants were more likely than stably housed participants to have been diagnosed with any STI in the past 9 months (χ2 = 11.4, p = 0.001), have more than one sex partner in the past 9 months (χ2 = 15.9, p < 0.001), exchange sex in the past 90 days (χ2 = 4.84, p = 0.03), and to have a high risk sex partner in the past 90 days (χ2 = 4.11, p = 0.04). No differences were observed in drug use in the past 6 months.
No difference was observed for the reported source of usual health care, and the majority of both stably and unstably housed participants (69.4% and 70.2%, respectively) had seen a general or primary care doctor within the past 6 months. Most participants had been tested for HIV at least once (97.3%), and only 17.4% reported their last HIV test was their first. Half (51.9%) had their last test within the past 6 months at the time of the survey, and 80.6% received the results of this test.
Table 2 presents the bivariate and multivariate model considering recent HIV testing and housing stability. Participants unstably housed were 1.4 times more likely to have been tested for HIV in the past 6 months (OR = 1.40, 95% CI: 1.01, 1.93, p = 0.045); however, when controlling for other factors, housing stability was not associated with testing for HIV in the past 6 months. Those currently homeless, though, were twice as likely to have recently been tested for HIV (AOR = 2.34, 95% CI: 1.06, 5.17, p = 0.04). Individuals seeing a health care provider in the past month were 2.5 times as likely to receive and HIV test (AOR = 2.46, 95% CI: 1.70, 3.56, p < 0.001). Interaction effects of housing, education, and income were not significant.
Table 2.
Multivariate regression analysis of the associations between housing stability and HIV testing in the past 6 months by CHAT study participants, 2005-2007.
| Unadjusted odds ratio (95% CI) |
Adjusted odds ratio a (95% CI) |
|
|---|---|---|
| Unstable Housing | 1.40b (1.01, 1.93) | 1.28 (0.89, 1.83) |
| Currently homeless | 2.42b (1.17, 5.03) | 2.34b (1.06, 5.17) |
| Age | 0.98c (0.96, 0.99) | 0.97b (0.95, 0.99) |
| Sex: Female | 1.80 (1.25, 2.60) | 1.72b (1.13, 2.61) |
| High school diploma/GED | 1.00 (0.78, 1.38) | 1.11 (0.78, 1.57) |
| Income in past 30 days less than $500 | 1.13 (0.82, 1.56) | 0.90 (0.62, 1.30) |
| Depression score >= 16 | 0.79 (0.56, 1.12) | 0.68b (0.46, 1.00) |
| Seen a general or primary care doctor within the past 6 months | 2.41d (1.69, 3.43) | 2.46d (1.70, 3.56) |
Adjusted model includes all variables listed in the table
p ≤ 0.05,
p ≤ 0.01,
p ≤ 0.001
Residential Transience
Residential transience was experienced by 104 (16.8%) of the study participants within the 6 months prior to completing the survey. Socio-demographic characteristics, housing characteristics, HIV risk behaviors, access to health care, and HIV testing characteristics for the participants based on residential mobility are presented in Table 3. Transient participants were more likely to be female (χ2 = 4.43, p = 0.04) and younger (t = 4.17, p < 0.001) than non-transient participants. Transient participants were less likely to have a high school diploma or GED (χ2 = 9.73, p = 0.002), more likely to have a monthly income of less than $500 (χ2 = 8.89, p = 0.003), more likely to have been in jail or prison in the past 6 months (χ2 = 7.73, p = 0.005), and more likely to have a CES-D score of 16 or more (χ2 = 5.04, p = 0.03). Transient participants moved an average of 3.88 times in the past 6 months, significantly more often than non-transient participants (t = -3.87, p < 0.001).
Table 3.
Comparison of participants based on residential transience among CHAT study participants, 2005-2007.
| Non-transient (n = 516) |
Transient (n =104) |
Total (n = 620) |
Test statistica (p value) |
|
|---|---|---|---|---|
| Socio-demographics | ||||
| Sex: Female | 393 (76.2) | 89(85.6) | 482 (77.7) | 4.43 (0.035) |
| Age, mean (sd) | 42.7 (8.6) | 38.8 (8.8) | 42.1 (8.8) | 4.17 (<0.001) |
| Education: High school/GED | 286 (55.6) | 40 (38.8) | 326 (52.8) | 9.73 (0.002) |
| Employed full- or part-time | 111 (21.5) | 17 (16.3) | 128 (20.6) | 1.41 (0.235) |
| Income in past 30 days less than $500 | 230 (44.6) | 63 (60.6) | 293 (47.3) | 8.90 (0.003) |
| In jail or prison in past 6 months | 65 (12.6) | 24 (23.1) | 89 (14.4) | 7.73 (0.005) |
| Currently has main sex partner | 390 (75.6) | 73 (70.2) | 463 (74.7) | 1.33 (0.249) |
| Depression score >= 16 | 372 (72.1) | 86 (82.7) | 458 (73.9) | 5.04 (0.025) |
| Housing | ||||
| Currently homeless | 26 (5.0) | 9 (8.7) | 35 (5.6) | 2.12 (0.145) |
| Times moved in past 6 months, mean (sd) | 0.23 (0.4) | 3.88 (9.6) | 0.84 (4.2) | -3.87 (<0.001) |
| HIV risk | ||||
| Diagnosed with nonHIV STI in past 9 months | 37 (7.2) | 18 (17.3) | 55 (8.9) | 11.00 (0.001) |
| Sex with >1 person in past 9 months | 265 (51.4) | 76 (73.1) | 341 (55.0) | 16.50 (<0.001) |
| Exchange sex in past 90 days | 95 (20.5) | 35 (36.8) | 130 (23.3) | 11.75 (0.001) |
| Injected drugs in past year | 34 (6.6) | 4 (3.8) | 38 (6.1) | 1.13 (0.287) |
| Used heroin, crack or cocaine in past year | 346 (86.5) | 82 (88.2) | 428 (86.8) | 0.18 (0.668) |
| Sex with high risk partner in past 90 days | 245 (47.5) | 60 (57.7) | 305 (49.2) | 3.61 (0.057) |
| Access to Health Care | ||||
| Usual source of health care | 9.96 (0.354) | |||
| Public health department | 18 (3.5) | 7 (6.9) | 25 (4.1) | |
| Community based clinic | 248 (48.7) | 51 (50.0) | 299 (48.9) | |
| Private doctor | 32 (6.3) | 4 (3.9) | 36 (5.9) | |
| Hospital clinic | 121 (23.8) | 16 (15.7) | 137 (22.4) | |
| Emergency room | 61 (12.0) | 18 (17.6) | 79 (12.9) | |
| Other | 29 (5.8) | 6 (5.9) | 35 (5.8) | |
| Seen a general or primary care doctor within the past 6 months | 357 (70.1) | 70 (68.6) | 427 (69.9) | 0.09 (0.762) |
| HIV Testing | ||||
| Ever tested for HIV | 499 (96.7) | 104 (100) | 603 (97.3) | 3.52 (0.061) |
| Tested for HIV only once | 88 (17.7) | 17 (16.3) | 105 (17.4) | 0.11 (0.746) |
| Time since last HIV test | 7.82 (0.050) | |||
| ≤ 6 months | 257 (49.8) | 65 (62.5) | 322 (51.9) | |
| 6-12 months | 84 (16.3) | 14 (13.5) | 98 (15.8) | |
| > 1 year | 158 (30.6) | 25 (24.0) | 183 (29.5) | |
| Received result of last HIV test | 399 (80.0) | 87 (83.7) | 486 (80.6) | 0.75 (0.386) |
χ2 test statistics are provided for dichotomous variables and t test statistics are provided for continuous variables
Transient participants were more likely than non-transient participants to have been diagnosed with an STI (χ2 = 11.0, p = 0.001) and have sex with more than one partner (χ2 = 16.50, p < 0.001) in the past 9 months, and have exchange sex in the past 90 days (χ2 = 11.75, p = 0.001). No differences were observed in drug use.
Transient participants and non-transient participants did not differ in their source of usual health care, both most often going to community-based clinics (48.9%), and the majority of transient and non-transient participants had seen a general or primary care doctor in the past 6 months (68.6% and 70.1%, respectively). Transient participants were more likely to report that their last HIV test was within the past 6 months compared to non-transient participants (χ2 = 7.82, p = 0.05).
Table 4 presents the bivariate and multivariate models considering recent HIV testing and residential transience. When controlled for other factors, transient participants were 1.7 times more likely to have tested for HIV in the past 6 months (AOR = 1.65, 95% CI: 1.03, 2.64, p = 0.04). Those currently homeless were 2.5 times more likely to recently have tested for HIV compared to those who were not homeless while controlling for transience (AOR = 2.51, 95% CI: 1.14, 5.54, p = 0.02). Participants seeing a health care provider in the past 6 months were also 2.5 times as likely to have been tested fir HIV in the past 6 months (AOR = 2.48, 95% CI: 171, 3.59, p < 0.001). Interaction effects of transience, education, and income were not significant.
Table 4.
Multivariate regression analysis of the associations between residential transience and HIV testing in the past 6 months by CHAT study participants, 2005-2007.
| Unadjusted odds ratio (95% CI) |
Adjusted odds ratio a (95% CI) |
|
|---|---|---|
| Transient | 1.68b (1.08, 2.61) | 1.65b (1.03, 2.64) |
| Currently homeless | 2.42b (1.17, 5.03) | 2.51b (1.14, 5.54) |
| Age | 0.98c (0.96, 0.99) | 0.97b (0.95, 0.99) |
| Sex: Female | 1.80c (1.25, 2.60) | 1.67b (1.10, 2.52) |
| High school diploma/GED | 1.00 (0.72, 1.38) | 1.14 (0.81, 1.62) |
| Income in past 30 days less than $500 | 1.13 (0.82, 1.56) | 0.92 (0.64, 1.32) |
| Depression score >= 16 | 0.79 (0.56, 1.12) | 0.67b (0.41, 0.98) |
| Seen a general or primary care doctor within the past 6 months | 2.41d (1.69, 3.43) | 2.48d (1.71, 3.59) |
Adjusted model includes all variables listed in the table
p ≤ 0.05,
p ≤ 0.01,
p ≤ 0.001
Discussion
This study examined the relationship between housing stability, residential transience, and recent HIV testing through a cross-sectional analysis of urban African Americans living in a high-risk environment in Baltimore, Maryland. Our findings demonstrate that among low-income populations, instability housed and transient individuals differ from those who are stably housed and not mobile, respectively, in many important ways. Transient individuals, for example, were significantly different from non-transient individuals in several sociodemographic characteristics; they were more likely to be female, of younger age, less educated, receive lower income, have been incarcerated in the past 6 months, and to score high on the depression scale. These findings are consistent with those from sample of injection drug users in Baltimore, Maryland (German et al., 2007; Davey-Rothwell et al., 2008). Additionally, this study is consistent with previous research demonstrating that unstably housed and transient individuals are more likely to engage in HIV risk behaviors compared to those who are stably housed and non-transient, respectively (Aidala et al., 2005; Aidala et al., 2006; Weir et al., 2007; Corneil et al., 2006; Royse et al., 2000; German et al., 2007).
Housing instability and transience has been recognized as a structural barrier to HIV prevention (Rhodes et al., 2005; Parker, Easton, & Klein, 2000). HIV risk among homeless individuals tends to be greater than among those unstably housed, and both groups are at increased risk of HIV than persons stably housed suggesting a dose-response relationship (Aidala et al., 2005; Aidala & Sumartojo, 2007; Weir et al., 2007). Typically, housing stability has been defined in terms of whether a person is currently housed or not, with some researchers providing a third category of unstably housed for persons sharing space with someone else, living in a single room occupancy hotel, or housed in a recovery or transitional home. These categorizations distinguish whether or not a person has their basic housing needs met; however, because housing stability (and instability) is impacted by various aspects of housing, the presence of a home may not adequately account for the known associations between HIV and housing (Weir et al., 2007). Thus, researchers have increasingly utilized broader conceptualizations of housing stability that include subjective housing stability, supportive housing, and transience (Weir et al., 2007; German et al., 2007; Davey-Rothwell et al., 2008). Our findings considering HIV testing and housing provide additional evidence that more nuanced categorization of housing stability should be considered beyond the most recognized categories of stably housed, unstably housed, and homeless.
Currently, the Centers for Disease Control and Prevention (CDC) recommends HIV testing among adults, adolescents, and pregnant women occur for all patients after notification unless the patient declines. Persons at increased risk for HIV, which includes those unstably housed or transient, should be tested at least annually. Additionally, retesting should be recommended after a single recent high-risk event in populations with high prevalence of HIV, and before initiating a new sexual relationship (CDC, 2009).
Thus, given the risk of HIV in this urban low-income population, it is encouraging that 97.3% of the study participants had been tested at least once for HIV (80.6% of whom received the result of their last test), and 82.6% had been tested more than once in their lifetime. However, the percentage of respondents who had been tested for HIV in our study is likely higher than the general population. This is consistent though with other investigations that have shown that inner city residents with high risk of HIV are more likely to have been tested for HIV than other individuals (Herndon et al., 2003). Time since last test was also encouraging, with just over half of the study participants tested within the past 6 months. At the time of this study, rapid testing was not as widely used as it is now, and almost 20% of participants did not receive the results of this test. There was no difference between those who did and did not receive the results of their test except those who did not were more likely to have been incarcerated in the past 6 months and were less likely to be employed (data not shown).
Although unstably housed individuals were more likely to be at risk of HIV, they were not more likely to be recently tested; transient individuals were more likely to be recently tested in the multivariate model. In both models, homeless individuals were more likely to have been recently tested. Having seen a doctor in the past 6 months also increased the chance of being tested for HIV in both models. This is consistent with previous investigations with homeless and low-income women finding that a regular source of care is associated with HIV testing (Herndon et al., 2003; Tucker et al., 2003). Our sample of low-income urban African Americans did not demonstrate differences with location of usual source of care based on housing stability or residential mobility; almost half reported using a community-based clinic and almost a quarter reported using hospital clinics. Additionally, almost 70% had seen a health care provider in some capacity in the previous 6 months. However, no data was collected about the nature of these clinical interactions. Our sample included only low-income participants; however, differing access to primary health care and/or inappropriate use of health care services based on housing stability has been observed elsewhere in more general population samples (Kushel, Vitinghoff, & Hass 2001; Kushel et al., 2006, Reid et al., 2008; Aday, 2001).
Our findings report only on health services with a health care provider. It is possible that homeless and transient individuals utilize other service providers (e.g., for food or other resources) more frequently then those who are unstably housed, and HIV testing and/or referral for testing may occur in these locations as well. Service providers may not recognize unstably housed individual's risk for HIV as clearly as a homeless individual's risk since “the homeless” have been identified as a special risk group with respect to HIV and other negative health outcomes (Schwartz & Carpenter, 1999; Aidala & Sumartojo, 2007). Additionally, literal homelessness is the extreme among a range of unstable housing arrangements and is the most recognizable for service providers. Thus, service providers may not facilitate HIV testing in the same manner with unstably housed individuals as they do for their homeless clients.
Since individuals who are unstably housed and/or transient may face barriers to health care and are often found to be less likely to engage the conventional primary care setting, primary prevention and testing in nonclinical settings, including community-based clinics and organizations, remains crucial. Studies have shown that offering HIV testing and counseling in community or outreach settings can be effective for engaging individuals at high risk of HIV and identifying unrecognized HIV infection (CDC, 2007; Liang et al., 2005; Bucher, Thomas, Guzman, Riley, Dela Cruz, & Bangsberg, 2007; Clark, Bowles, Song, & Heffelfinger, 2008). Many community-based organizations provide services to populations vulnerable to HIV infection, and thus are well positioned to offer HIV testing and counseling in their communities (Kelly et al., 2000). However, to address the potential differences in use of HIV prevention and testing opportunities in these sites among homeless, transient, and unstably housed clients as noted above, further investigation is warranted.
While continued increases in HIV testing opportunities and increased recognition of the vulnerabilities among all individuals located within the spectrum of unstable housing may help promote HIV testing for high risk populations, housing needs beyond homelessness must be recognized as an intermediate structural factor that is created by and contributes to social and economic inequalities. Policy makers should be encouraged to attend to laws and policies that negatively impact housing opportunities for subpopulations, including drug users and formerly incarcerated individuals (Rhine, 2008; Lazzarini & Klitzman, 2002). Health care providers should place greater emphasis on immediate housing needs, identifying and recognizing unstable housing as a vulnerability to be addressed through linkage to social services or case management services. This can have important implications, as several studies have demonstrated that improvements in housing are associated with reduced risk of HIV and improved health care outcomes (Weir et al., 2007; Elifson, Sterk, & Theall, 2007; Aidala et al., 2005).
A major strength of this paper is that it moves beyond assessing HIV risk among urban low-income populations with unstable housing and/or residential transience to consider associations with recent HIV testing. However, the data should be interpreted in light of the following limitations. The results may not be generalizable to other racial and ethnic groups, or to African Americans in low-risk environments or rural areas, since this research included only low-income urban African American women residing in a community with high HIV prevalence and levels of drug use. The behaviors considered were self-reported, and may be subject to recall and social desirability bias. We did not ask transient individuals why they moved, although mobility is motivated by numerous factors. Detailed information regarding the participant's last HIV test were not obtained, and thus we cannot present on the quality of HIV counseling or the testing location. We are also unable to report on the reasons for not receiving test results or to use the last test for which results were received as the time of most recent test. Also, since the study sample consisted of individuals who signed up to be part of an HIV prevention study, it is possible that they may be more likely to participate in health promoting activities such as getting an HIV test. Additionally, it possible that there was differential attraction to the original intervention study based on group categorization (stable vs. unstable and/or transient vs. not transient), potentially comprimising the internal validity of the study. Finally, the study was cross-sectional and therefore limits the ability to make causal inferences.
Conclusion
Housing needs beyond homelessness must be recognized as an intermediate structural factor that is created by and contributes to social and economic inequalities that increase vulnerability to HIV/AIDS. While the broader processes contributing to poverty and equality must be addressed for long-term solutions, increased need exists for the testing and counseling of individuals who are unstably housed, transient, and/or homeless. Priority should be given to the development and/or sustainability of community programs that reduce barriers to health care for unstably housed and transient individuals and encourage HIV testing and counseling among unstably housed and transient individuals. Increased efforts for HIV testing in community settings, including mental health centers, utilizing outreach methods by community-based organizations and the use of rapid HIV tests may increase testing among unstably housed individuals and remove barriers to return for test results for unstably housed, transient, and/or homeless individuals (CDC, 2007; Liang et al., 2005; Bucher et al., 2007; Clark et al., 2008). Testing centers that identify HIV positive individuals who are unstably housed, transient, and/or homeless must be able to provide services to ensure that these individuals quickly get into care as well as programs to ensure that they can maintain medical care.
Acknowledgments
This work was funded by the National Institute on Mental Health (Grant# R01 MH66810 and K01MH096611).
References
- Aday L. At risk in America: The health and health needs of vulnerable populations in the United States. San Fransisco, CA: Jossey-Bass; 2001. [Google Scholar]
- Adimora AA, Schoenbach VJ. Social context, sexual networks, and racial disparities in rates of sexually transmitted infections. J Infect Dis. 2005;191(Suppl 1):S115–S122. doi: 10.1086/425280. [DOI] [PubMed] [Google Scholar]
- Aidala AA, Cross JE, Stall R, Harre D, Sumartojo E. Housing status and HIV risk behaviors: Implications for prevention and policy. AIDS & Behavior. 2005;9(3):251–256. doi: 10.1007/s10461-005-9000-7. [DOI] [PubMed] [Google Scholar]
- Aidala AA, Lee G, Garbers S, Chiasson MA. Sexual behaviors and sexual risk in a prospective cohort of HIV-positive men and women in New York City, 1994-2002: implications for prevention. AIDS Education and Prevention. 2006;18(1):12–32. doi: 10.1521/aeap.2006.18.1.12. [DOI] [PubMed] [Google Scholar]
- Aidala AA, Sumartojo E. Why housing? AIDS & Behavior. 2007;11(Suppl 2):S1–S6. doi: 10.1007/s10461-007-9302-z. [DOI] [PubMed] [Google Scholar]
- Blindman AB, Grumbach K, Osmond D, Vranzian K, Stewart AL. Primary care and receipt of preventative services. Journal of General Internal Medicine. 1996;11(5):269–276. doi: 10.1007/BF02598266. [DOI] [PubMed] [Google Scholar]
- Bourgois P. The moral economies of homeless heroin addicts: confronting ethnography, HIV risk, and everyday violence in San Francisco shooting encampments. Substance Use and Misuse. 1998;33(11):2323–2351. doi: 10.3109/10826089809056260. [DOI] [PubMed] [Google Scholar]
- Browning CR, Olinger-Wlbon M. Neighborhood structure, social organization, and number of short-term sexual partnerships. Journal of Marriage and Family. 2003;65(3):730–745. [Google Scholar]
- Bucher JB, Thomas KM, Guzman D, Riley E, Dela Cruz N, Bangsberg DR. Community-based rapid HIV testing in homeless and marginally housed adults in San Francisco. HIV Medicine. 2007;8(1):28–31. doi: 10.1111/j.1468-1293.2007.00423.x. [DOI] [PubMed] [Google Scholar]
- Campsmith ML, Rhodes PH, Hall HI, Green TA. Undiagnosed HIV prevalence among adults and adolescents in the United States at the end of 2006. Journal of Acquired Immune Deficiency Syndromes. 2010;53(5):619–624. doi: 10.1097/QAI.0b013e3181bf1c45. [DOI] [PubMed] [Google Scholar]
- Castel R. The roads to disaffiliation: insecure work and vulnerable relationships. International Journal of Urban and Regional Research. 2000;24(3):519–535. [Google Scholar]
- Center for Disease Control and Prevention (CDC) Rapid HIV testing in outreach and other community settings – United States, 2004-2006. Morbidity and Mortality Weekly Report. 2007;56(47):1233–1237. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) HIV prevalence estimates – United States, 2006. Morbidity and Mortality Weekly Report. 2008;57(39):1073–1076. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Meeting summary: Consultation on revised guidelines for HIV counseling, testing, and referral in non-health-care settings. 2009 Online: http://www.cdc.gov/hiv/topics/testing/resources/other/consultation.htm.
- Centers for Disease Control and Prevention (CDC) Diagnosis of HIV infection and AIDS in the United States and dependent areas, 2010. 2010 Online: http://www.cdc.gov/hiv/surveillance/resources/reports/2010report/index.htm.
- Centers for Disease Control and Prevention (CDC) HIV Surveillance – United States, 1981-2008. Morbidity and Mortality Weekly Report. 2011;60(21):689–693. [PubMed] [Google Scholar]
- Clark HA, Bowles KE, Song B, Heffelfinger JD. Implementation of rapid HIV testing program in community and outreach settings: perspectives from staff at eight community-based organizations in seven U.S. cities. Public Health Reports. 2008;123(Suppl 3):86–93. doi: 10.1177/00333549081230S311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corneil TA, Kuyper LM, Shoveller J, Hogg RS, Spittal PM, Schechter MT, et al. Unstable housing, associated risk behaviour, and increased risk for HIV infection among injection drug users. Health & Place. 2006;12(1):79–85. doi: 10.1016/j.healthplace.2004.10.004. [DOI] [PubMed] [Google Scholar]
- Culhane DP, Gollub E, Kuhn R. The co-occurrence of AIDS and homelessness: results from the integration of administrative databases for AIDS surveillance and public shelter utilization in Philadelphia. Journal of Epidemiology and Community Health. 2001;55(7):515–520. doi: 10.1136/jech.55.7.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey-Rothwell MA, German D, Latkin CA. Residential transience and depression: does the relationship exist for men and women? Journal of Urban Health. 2008;85(5):707–716. doi: 10.1007/s11524-008-9294-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey-Rothwell MA, Tobin K, Yang C, Sun CJ, Latkin CA. Results of a randomized controlled trial of a peer mentor HIV/STI prevention intervention for women over an 18 month follow-up. AIDS & Behavior. 2011;15(8):1654–1663. doi: 10.1007/s10461-011-9943-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elifson KW, Sterk CE, Theall KP. Safe living: the impact of unstable housing conditions on HIV risk reduction among female drug users. AIDS & Behavior. 2007;11(Suppl 6):45–55. doi: 10.1007/s10461-007-9306-8. [DOI] [PubMed] [Google Scholar]
- German D, Davey MA, Latkin CA. Residential transience and HIV risk behaviors among injection drug users. AIDS & Behavior. 2007;11(Suppl 6):S21–S30. doi: 10.1007/s10461-007-9238-3. [DOI] [PubMed] [Google Scholar]
- Hankins C, Tran T, Hum L, Laberge N, Lepine D, Monpetit M, et al. Socioeconomic geographical links to human immunodeficiency virus seroprevalence among childbearing women in Montreal, 1989–1993. International Journal of Epidemiology. 1998;27(4):691–697. doi: 10.1093/ije/27.4.691. [DOI] [PubMed] [Google Scholar]
- Herndon B, Asch SM, Kilbourne AM, Wang M, Lee M, Wenzel SL, Andersen R, Gelberg L. Prevalence and predictors of HIV testing among a probability sample of homeless women in Los Angeles County. Public Health Reports. 2003;118(3):261–269. doi: 10.1093/phr/118.3.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JA, Heckman TG, Stevenson LY, Williams PM, Ertl T, Hays RB, et al. Transfer of research-based HIV prevention interventions to community service providers: fidelity and adaptation. AIDS Education and Prevention. 2000;12(Suppl 5):87–98. [PubMed] [Google Scholar]
- Kushel MB, Vitinghoff E, Hass JS. Factors associated with the health care utilization of homeless persons. Journal of the American Medical Association. 2001;285(2):200–206. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. Journal of General Internal Medicine. 2006;21(1):71–77. doi: 10.1111/j.1525-1497.2005.00278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurecin CT, Christensen DM, Taylor ED. HIV/AIDS and the African-American community: a state of emergency. Journal of the National Medical Association. 2008;100(1):35–43. doi: 10.1016/s0027-9684(15)31172-x. [DOI] [PubMed] [Google Scholar]
- Liang TS, Erbelding E, Jacob CA, Wicker H, Christmyer C, Brunson S, Richardson D, Ellen JM. Rapid HIV testing of clients of a mobile STD/HIV clinic. AIDS Patient CARE and STDs. 2005;19(4):253–257. doi: 10.1089/apc.2005.19.253. [DOI] [PubMed] [Google Scholar]
- Lizzarini Z, Klitzman R. HIV and the law: integrating law, policy, and social epidemiology. Journal of Law, Medicine & Ethics. 2002;30(4):533–547. doi: 10.1111/j.1748-720x.2002.tb00424.x. [DOI] [PubMed] [Google Scholar]
- Marks G, Crepaz N, Janssen RS. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS. 2006;20(10):1447–1450. doi: 10.1097/01.aids.0000233579.79714.8d. [DOI] [PubMed] [Google Scholar]
- Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention. Journal of Acquired Immune Deficiency Syndromes. 2005;39(4):446–453. doi: 10.1097/01.qai.0000151079.33935.79. [DOI] [PubMed] [Google Scholar]
- Mizuno Y, Purcell D, Borkowski TM, Knight K, the SUDIS Team The life priorities of HIV-seropositive injection users: findings from a community-based sample. AIDS and Behavior. 2003;7(4):395–403. doi: 10.1023/b:aibe.0000004731.94734.77. [DOI] [PubMed] [Google Scholar]
- Mofenson LM. Advances in the prevention of vertical transmission of human immunodeficiency virus. Seminars in Pediatric Infectious Diseases. 2003;14(4):295–308. doi: 10.1053/j.spid.2003.09.003. [DOI] [PubMed] [Google Scholar]
- Panos G, Samonis G, Alexiou VG, Kavarnou GA, Charatsis G, Falagas ME. Mortality and morbidity of HIV infected patients receiving HAART: a cohort study. Current HIV Research. 2008;6(3):257–260. doi: 10.2174/157016208784324976. [DOI] [PubMed] [Google Scholar]
- Parker RG, Easton D, Klein CH. Structural barriers and facilitators in HIV prevention: a review of international research. AIDS. 2000;14(S1):S22–S32. doi: 10.1097/00002030-200006001-00004. [DOI] [PubMed] [Google Scholar]
- Porco TC, Martin JN, Page-Shafer KA, Cheng A, Charlebois E, Grant RM, et al. Decline in HIV infectivity following the introduction of highly active antiretroviral therapy. AIDS. 2004;18(1):81–88. doi: 10.1097/01.aids.0000096872.36052.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Reid KW, Vittinghoff E, Kushel MB. Associations between level of housing instability, economic standing and health care access: a meta-regression. Journal of Health Care for the Poor and Underserved. 2008;19(4):1212–1228. doi: 10.1353/hpu.0.0068. [DOI] [PubMed] [Google Scholar]
- Reilly T, Woo G. Access to services and maintenance of safer sex practices among people living with HIV/AIDS. Social Work and Health Care. 2003;36(3):81–95. doi: 10.1300/j010v36n03_05. [DOI] [PubMed] [Google Scholar]
- Rhine SS. Criminalization of housing: a revolving door that results in boarded up doors in low-income neighborhoods in Baltimore, Maryland. University of Maryland Law Journal of Race, Religion, Gender & Class. 2009;9:333–371. [Google Scholar]
- Rhodes T, Kimber J, Small W, Fitzgerald J, Kerr T, Hickamn M, et al. Public injecting and the need for ‘safer environment intervention’ in the reduction of drug-related harm. Addiction. 2006;10(10):1384–1393. doi: 10.1111/j.1360-0443.2006.01556.x. [DOI] [PubMed] [Google Scholar]
- Robertson MJ, Clark RA, Charebois ED, Tulsky J, Long HL, Bangsberg DR, et al. HIV seroprevalence among homeless and marginally housed adults in San Francisco. American Journal of Public Health. 2004;94(7):1207–1217. doi: 10.2105/ajph.94.7.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royse D, Leukefeld C, Logan TK, Dennis M, Wechsberg W, Hoffman J, et al. Homelessness and gender in out-of-treatment drug users. American Journal of Drug & Alcohol Abuse. 2000;26(2):283–296. doi: 10.1081/ada-100100605. [DOI] [PubMed] [Google Scholar]
- Schawrtz S, Carpenter KM. The right answer for the wrong question: Consequences of type III error for public health research. American Journal of Public Health. 1999;89(8):1175–1180. doi: 10.2105/ajph.89.8.1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seagert S, Evans GW. Poverty, housing niches, and health in the United States. Journal of Social Issues. 2003;59(3):569–589. [Google Scholar]
- Shaw M. Housing and public health. Annual Review of Public Health. 2004;25:397–418. doi: 10.1146/annurev.publhealth.25.101802.123036. [DOI] [PubMed] [Google Scholar]
- Smereck GA, Hockman EM. Prevalence of HIV infection and HIV risk behaviors associated with living place: on-the-street homeless drug users as a special target population for public health intervention. American Journal of Drug & Alcohol Abuse. 1998;24(2):299–319. doi: 10.3109/00952999809001714. [DOI] [PubMed] [Google Scholar]
- Tucker JS, Wenzel SL, Elliott MN, Hambarsoomian K, Golinelli D. Patterns and correlates of HIV testing among sheltered and low-income housed women in Los Angeles County. Journal of Acquired Immune Deficiency Syndromes. 2003;34(4):415–422. doi: 10.1097/00126334-200312010-00009. [DOI] [PubMed] [Google Scholar]
- Weir BW, Bard RS, O'Brien K, Casciato CJ, Stark MJ. Uncovering patterns of HIV risk through multiple housing measures. AIDS & Behavior. 2007;11(Suppl 6):S31–S44. doi: 10.1007/s10461-007-9284-x. [DOI] [PubMed] [Google Scholar]
- Wenzel SL, Tucker JS, Elliot MN, Hambarsoomian K, Perlman J, Becker K, et al. Prevalence and co-occurrences of violence, substance use and disorder, and HIV risk behavior: a comparison of sheltered vs. low-income housed women in Los Angeles County. Preventative Medicine. 2004;39(3):317–624. doi: 10.1016/j.ypmed.2004.02.027. [DOI] [PubMed] [Google Scholar]
- Wenzel SL, Tucker JS, Elliot MN, Hambarsoomians K. Sexual risk among impoverished women: Understanding the role of housing status. AIDS & Behavior. 2007;11(Suppl 6):S9–S20. doi: 10.1007/s10461-006-9193-4. [DOI] [PubMed] [Google Scholar]
- Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]
- Zierler S, Krieger N, Tang Y, Coady W, Siegfried E, DeMaria A, et al. Economic deprivation and AIDS incidence in Massachusetts. American Journal of Public Health. 2000;90(7):1064–1073. doi: 10.2105/ajph.90.7.1064. [DOI] [PMC free article] [PubMed] [Google Scholar]


