Abstract
Background
Contemporary teaching in sub-Saharan African medical schools is largely through didactic and problem-based approaches. These schools face challenges from burgeoning student numbers, severe faculty shortages, faculty without instruction in teaching methods, and severe infrastructure inadequacies. Team-based learning (TBL) is a pedagogy which may be attractive because it spares faculty time. TBL was piloted in a module on ectoparasites at the Kilimanjaro Christian Medical University College (KCMU Co).
Methods
TBL orientation began 6 weeks before starting the module. Students were issued background readings and individual and group readiness assessment tests, followed by module application, discussion, and evaluation. At completion, student perceptions of TBL were assessed using a 5-point Likert scale evaluating 6 domains, with a score of 5 being most favorable. Strength of consensus measures (sCns) were applied. Final examination scores were compiled for 2011 (didactic) and 2012 (TBL).
Results
158 students participated in the module. The mean student scores across the 6 domains ranged from 4.2–4.5, with a high degree of consensus (range 85–90%). The final examination scores improved between 2011 and 2012
Conclusions
KCMU Co student perceptions of TBL were very positive, and final exam grades improved. These observations suggest future promise for TBL applications at KCMU Co and potentially other schools.
Introduction
Team-based learning™ (TBL) is an instructional process that emphasizes course concepts and their application (Michaelsen & Sweet 2008, Michaelsen, Parmalee et al. 2008) TBL is a learner-centered, instructor–led method that requires student acquisition of course concepts independently prior to class. Within class, TBL emphasizes the role of teams and team discussions as effective mechanisms for teaching and learning, thus actively reinforcing the concepts studied prior to class. At each stage, individually and as a team, they undergo assessments of their knowledge with a test.
For TBL to succeed, faculty and students need to understand fully the underlying philosophy because in TBL the role of the instructor and the student differs substantially from conventional didactic teaching. In pedagogic TBL, the instructor transforms from being a dispenser of information and concepts to being a course designer who manages the entire instructional process. Whereas in traditional didactic learning the student is a passive recipient of information and concept, in TBL the individual student is responsible for the initial acquisition of the course concepts. In the second phase of TBL, the same students come to share the knowledge with other students in teams, and in this way, instructors and students become accountable and are mutually responsible for their separate but interrelated roles in TBL.
TBL may have relevance to teaching health care professionals, especially within schools of medicine. When TBL is introduced properly in medical schools, faculty and students readily accept it as a reasonable and interactive way of teaching (Michaelsen & Sweet 2008). Schools of medicine in sub-Saharan Africa (SSA) face daunting challenges including burgeoning numbers of admitted students, severe faculty shortages, faculty without formal instruction in teaching methods, and severe inadequacies in educational infrastructure as revealed in 2 recent reviews by Mullan (2011) and Chen (2012). Both authors cited the use of innovative teaching methods in sub-Saharan medical schools including TBL, problem-based learning (PBL) and community-based learning (CBL), although detailed descriptions of the use of these pedagogies were not provided.
TBL may be an attractive option for schools of medicine in SSA because it spares faculty time, reducing the need for a large faculty and preserving faculty time for other activities. We piloted the use of TBL at the Kilimanjaro Christian Medical University College (KCMU Co) to teach the module on ectoparasites, and sought to quantify student perceptions and monitor examination performance.
Practice points
In TBL students acquire knowledge first on their own before they are taught.
Sub-Saharan African medical schools (SSMS) have been teaching medical education mainly by the traditional didactic method or a mix of traditional lecturing, PBL and TBL.
These sub-Saharan medical schools experience perennial increase in student admission with little corresponding growth in the number of instructors. These two opposing elements place SSMS in a crisis situation.
There are good reasons to believe that SSMS can mitigate their teaching crisis by adopting TBL.
TBL is a strategy that effectively engages a large student population in small learning groups or teams.
In TBL students first write the examination as individuals, and later they re-visit the same examination in teams in order to learn where they went wrong. This process may make TBL a superior learning process compared to the didactic teaching method.
We have shown in this report that TBL can easily be adopted teaching a large group of students (up to 200).
We recommend that SSMS consider adoption of TBL as a method of managing rapidly increasing student class sizes. As a collateral benefit, faculty may find that their teaching career will become more satisfying.
Methods
Setting
The Kilimanjaro Christian Medical University College (KCMU Co) is a constituent college of Tumaini University Makumira supported by the Evangelical Lutheran Church of Tanzania. It is one of five medical schools in Tanzania, was established in 1997 and is located in Moshi facing Mount Kilimanjaro. The medical school class size has experienced rapid growth since its establishment, especially in the past 5 years; in 2011, there were 156 students in the first-year medical school class. In addition to the KCMU Co School of Medicine, 15 other health-related degrees are offered by the College. There are 102 faculty to support teaching within KCMU Co.
At KCMU Co the medical parasitology and entomology course is taught jointly to the second-year medical (MD2) and second-year Bachelors’ of Science in Health Laboratory Sciences (BScHLS) students. The parasitology course contains a module on ectoparasites, which is taught late in the academic year.
Introduction of TBL
TBL was introduced to KCMU Co faculty in a 3-day workshop presented by faculty from the Duke-National University of Singapore Graduate Medical School (Duke-NUS) and the Duke University School of Medicine (DUSOM). The first author (MN) and an instructor in community health who developed a strong interest in TBL attended a one-week intensive workshop on TBL at Duke-NUS. Upon returning to KCMU Co, an effort was undertaken with the faculty teaching parasitology to pilot the teaching of the ectoparasite module using TBL in July 2012.
Teams
Teams consisting of 10 students were carefully formed with faculty input with the desire to achieve gender balance, a mix of prior medical exposures, and ethnicity to assure interactive team participation among all members as recommended by Michaelsen and Sweet (2008) and Parmelee et al. (2012).
Orientation
Students were oriented to TBL for about 4 hours through required lectures and videotapes from these lectures were posted at YouTube. Students were encouraged to address questions about TBL to participating faculty.
Folder
A folder prepared from published book chapters on ectoparasites (mites, fleas, black flies, mosquitoes, lice, bed bugs, kissing bugs, soft and hard ticks, sandflies, jiggers and chiggers) was prepared. Instructors explained briefly the contents of the folder.
Individual and Group Readiness Assurance Tests (iRAT and gRAT)
Forty-five days after receiving the folder, students completed a 90-minute individual readiness assurance test (iRAT) consisting of 49 multiple-choice questions (MCQ). This was followed by a 3-hour group readiness assurance test (gRAT). After the gRAT there was a long discussion session, and students were given the opportunity to give their opinions on the folder and the iRAT. Then the student teams answered 3 application questions on unknown clinical scenarios over 4 hours. Lastly instructors responded to student appeals regarding the correct answers on the iRAT, gRAT and clinical scenario applications, followed by module evaluation.
Student perceptions of TBL
A 6-domain questionnaire was developed to assess student perceptions of the use of TBL to teach the ectoparasite module based upon a previously validated instrument (Abdelkhalek et al. 2010). The 6 domains were focused on the learning process, course content and knowledge, educational environment, assessment, instructors, and efficiency, and the questionnaire utilized a 5-point Likert scale (Taste, Russell and Wierman 2005), with 5 being the most favorable score. Multiple questions were asked within each domain. Descriptive statistics and a strength of consensus measure (sCns) were applied. The strength of consensus measure describes shared group agreement on a particular item and a sCns above 80% is considered strong consensus (Chen et al. 2012). Final examination scores for 2011 (didactic) and 2012 (TBL) were compiled.
Results
Students and their perceptions of TBL
Participants
Four faculty members taught the ectoparasite module, (MN, JK, JM and PF). A total of 158 students participated (121 MD2 students and 37 BScHLS students). No student failed to complete the questionnaire at the end of the application session. The 2011 final examination grades for the ectoparasite module taught by didactic methods were used for comparison. The students in 2011 (didactic) and 2012 (after TBL) represented different populations and the examinations were not the same.
Questionnaire Results
Table 1 shows the mean student perception scores and the sCns. The mean scores ranged from 4.3 to 4.5, and the sCns measures from 85–90%.
Table 1.
Mean and strength of consensus measures (sCns) of student perceptions of TBL in 6 domains using the 5-point Likert scale.
| Domain | Mean | % sCsn |
|---|---|---|
| Learning process | 4.4 | 87 |
| Course content | 4.5 | 90 |
| Educational environment | 4.4 | 87 |
| Assessment | 4.3 | 85 |
| Instructors | 4.5 | 90 |
| Efficiency | 4.5 | 90 |
Examination scores and range
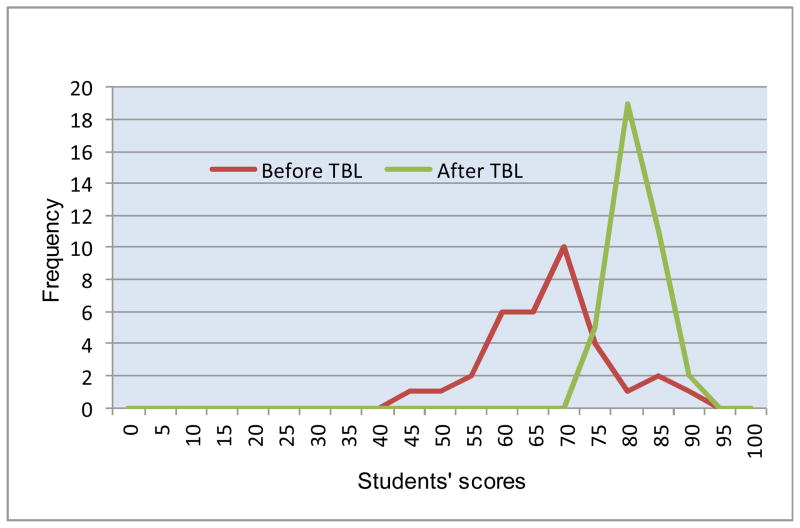
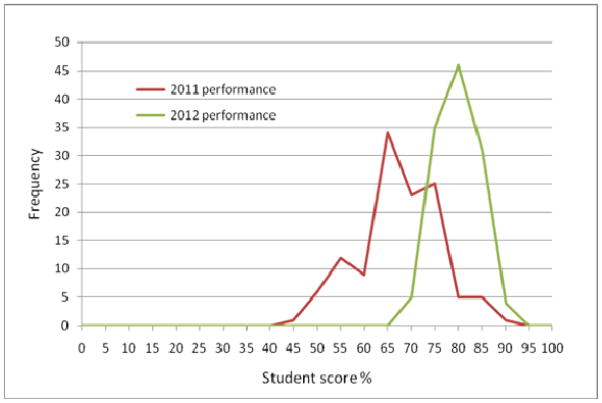
Frequency distribution of final exam scores
Figure 1 displays the frequency distribution of final exam scores for BScHLS students in 2011 (didactic) and 2012 (TBL), and Figure 2 presents the frequency distribution of final exam scores for MD2 students in 2011 and 2012. There is a clear change in frequency distributions between 2011 and 2012, with a much tighter distribution at a higher score in 2012. The mean, median, maximum and minimum scores and standard deviation values are given in Table 2.
Figure 1.
Frequency distribution of BScHLS student scores.
Figure 2.
Frequency distribution of MD student scores.
Table 2.
Comparison of student scores with didactic teaching (2011) and after TBL (2012)
| BScHLS students | Medical students | ||||
|---|---|---|---|---|---|
| Year | 2011 (didactic) | 2012 (after TBL) | 2011 (didactic) | 2012 (after TBL) | Remarks |
| Mean score | 65% | 79% | 65% | 77% | There is an increase in the mean score in both groups (MD and BScHLS 2012) after using TBL. |
| Median score | 65% | 79% | 64% | 77% | The median score after TBL has increased in both groups (MD and BScHLS 2012). |
| Maximum score | 87% | 88% | 87% | 88% | There is little difference in the maximum scores before and after TBL in both groups (MD and BScHLS 2012). |
| Minimum score | 43% | 72% | 42% | 68% | There is a great improvement in the minimum scores after using TBL in both groups (MD and BScHLS 2012). |
| Standard deviation | 9.57 | 3.40 | 8.58 | 4.03 | The standard deviation has decreased in both groups (MD and BScHLS) indicating less variability after TBL. |
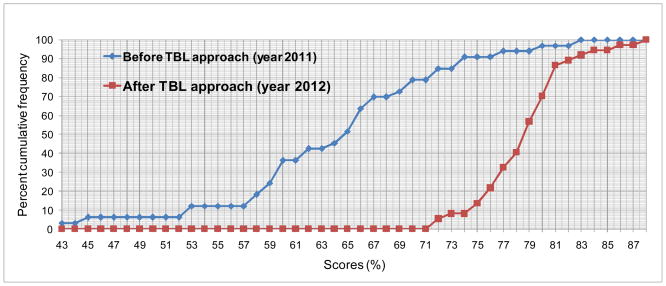
Quartile scores for the BScHLSc students
The first/lowest quartile (lowest 25% of the students) received a score of 59% in 2011; in 2012 this score improved to 77% (Figure 3). In the second 50% quartile the score was 65% in 2011 but increased to 79% in 2012. For the third quartile, the score was 69% in 2011 and 80% in 2012. Lastly, for the top quartile the score was 83% in 2011 and 88% in 2012.
Figure 3.
Percent cumulative score frequency distribution for BScHLSc class.
Pre- TBL (2011) scores were as follows: first quartile 59%, the second interquartile 65% and third quartile 70%. The median interquartile range was 64 (60–71%). After TBL the percent score cumulative frequency was: first quartile 77%, second quartile 79% and third quartile 81%. The median interquartile range was 79 (77–81%).
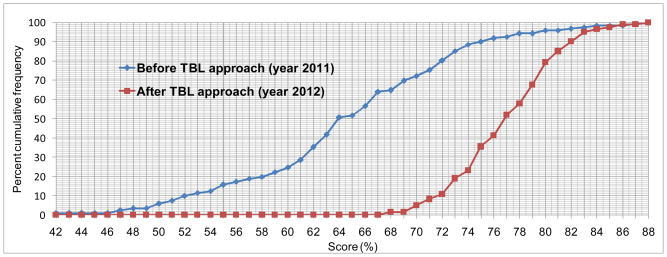
Quartile scores for the MD2 students
The first quartile of the 2011 MD2 class received a score of 60%, and in 2012 this score improved to 71% (Figure 4). For the second quartile, the median student scores increased from 65% in 2011 and improved to 74% in 2012. Similarly for the third quartile, the student scores increased from 71% in 2011 to 80% in 2012. Lastly, for the top quartile the score was 87% in 2011 and 88% in 2012.
Figure 4.
Percent cumulative score frequency distribution of MD class.
Before TBL (2011) scores were as follows; first quartile was 60%. the second quartile 64% and third quartile 71%. The median interquartile range was 64 (60–71). After TBL the percent score cumulative frequency was; first quartile 74%, second quartile 77% and third quartile was 79.5%. The median interquartile range was 77 (71–80).
Changes in the lowest scores for BScHLSc and MD2 students
In 2012 the lowest score for BScHLSc students was 72%; in 2011 80% of students scored 72% or lower. Similarly in 2012 the lowest score for MD2 students was 65%; in 2011 50% of students scored 65% or lower.
Discussion
The study results demonstrate a high degree of student acceptance of TBL methods with a strong consensus in teaching a module on ectoparasites of medical importance at KCMU Co. In addition, between 2011 and 2012 the frequency distribution of student final examination grades dramatically changed, with much higher scores for the lower half of both MD2 and BScHLS students. The observed changes cannot necessarily be attributed to the introduction of TBL, but certainly the temporal association bears further investigation. If confirmed, TBL may offer advantages to faculty teaching health professions in similar resource-limited settings.
Confounders in our observations must be considered. Two different groups of students were studied in 2011 (before TBL) and 2012 (after TBL), and it is possible that population differences contributed to the results. The final examinations were different in the 2 years, and could have affected the student scores, although in the opinions of three faculty members (MN, JK and JM) who taught the module pre-TBL and with TBL, the questions were similar in difficulty. It is also possible that the provision of reading materials to students taught with TBL in 2012 impacted the results, although the same reading list was provided in 2011. All these observations notwithstanding, the results obtained in this study are similar to those reported by other workers (McInerney and Fink 2003, Neider et al. 2005, Chung et al. 2009, Vasan et al. 2009, Abdelkhalek et al. 2010). Finally, 10 students per group is higher than the recommended 5–7 students per group for TBL. The larger group size could have impacted our results in a negative manner by failing to provide the most conducive environment for discussion, or in positive manner by increasing the numbers of students to participate in answering questions.
Challenges, innovations and emerging trends in medical education in SSA have been reviewed by Mullan et al. (2011) and Chen et al. (2012). These reviews revealed that in SSA medical schools many teaching innovations including TBL, problem–based learning, community-based learning, and multidisciplinary learning, were being practiced to enhance health system education in basic and clinical sciences. However, no other study in SSA has sought to quantify student perceptions of TBL and observed test score performance similar to our study.
A collateral benefit of TBL may be enhanced faculty satisfaction with teaching. Larry K. Michaelsen (1998), the founding father of TBL, acknowledges that after adopting TBL following years of conventional teaching, the impact on student learning and his pleasure in teaching was profound. His professional feelings are similar to those of Kenny (2003) an instructor who taught a taxation module by TBL in an Australian college. It is interesting that the 3 instructors out of 4 who taught the ectoparasites pedagogically at KCMU Co for 6 weeks as reported in this study have similar feelings. In this case one of them (MN) taught ectoparasites didactically for 15 years, and the other 2 (JK and JM) have taught the same module didactically for 8 years. Their overall impression on shifting from didactic teaching to TBL is that TBL prepares students better academically and practically. At the end of the module, the instructors’ anecdotal job satisfaction was enhanced.
In addition to the previously mentioned limitations, the current study adhered to many TBL recommendations but did not include peer review. Guidelines for reporting TBL activities in the health science education literature are available (Haidet et al. 2012). Concerns about the heterogeneous way TBL activities have been previously reported were raised, making it difficult to critique approaches and compare results. With the goal of standardizing an approach to TBL conduct and reporting, seven core guidelines, including team formation, readiness assurance tests, immediate feedback, sequencing of in-class problem solving, the 4 S’s (same problem, significant problem, specific choice, simultaneously report), incentive structure and peer review were outlined. In our study peer review (Goo, 2011) was not done due to time constraints and inherent problems in peer review methods. We were also unable to conduct intra-team or student-tutor peer– assessments because students were not oriented toward this exercise. Possible disadvantages of these exercises have been identified including resentment of peer–assessment by learners, abuse of intra-team peer-assessment ending with limited value and fostering distrust and excess competitiveness in the classroom environment if peer assessments are not implemented professionally as discussed by Cestone et al. (2008).
The Duke-National University of Singapore medical educators (Kamei et al. 2012) recently described a novel learning strategy called TeamLEAD (Learn, Engage, Apply, and Develop) which utilizes TBL principles. It is an adaptation of TBL in that additionally it consists of Faculty lead discussion and content expert lecture. Comparatively, Team LEAD might be a better strategy in medical schools than classical TBL because it engages the student even more in the learning process and makes the faculty more responsible for the teaching materials they provide.
We have introduced TBL at KCMU Co in teaching an ectoparasite module for the first time with promising results. Future studies will expand the subject matter taught with TBL, including randomized trials to rigorously assess TBL impact. If confirmed, TBL may offer SSA medical schools powerful tools in improving educational outcomes despite continuing faculty shortages. It is expected that the results obtained from teaching ectoparasitology with TBL presented in this study will inspire instructors in the KCMU Co and other medical schools to adopt this novel method of teaching health practitioners in SSA.
Acknowledgments
The authors acknowledge the contributions of the Duke-National University of Singapore Graduate Medical School and the Duke University School of Medicine for guidance in team-based learning skills and editorial review. This study was supported by Health Resources and Services Administration (HRSA) grant T84HA21123 Medical Education Partnership Initiative. Dr. Bartlett receives salary support from US National Institutes of Health awards P30AI64518, U01AI067854, D43CA153722, and D43TW06732.
Footnotes
Declaration of Interest: The authors report no declaration of interest.
Notes on contributors
Dr. Nyindo is Associate Professor of Parasitology, Entomology and Immunology, Kilimanjaro Christian Medical University College (KCMU Co.)
Mr. Kitau is Assistant Lecturer, KCMU Co.
Dr. Lisasi is Monitoring and Evaluation Officer, Kilimanjaro Christian Medical Center Medical Education Partnership Initiative (KCMC MEPI)
Mr. Kapanda is Lecturer, KCMU Co and Biostatistician KCMC, MEPI.
Mr. Matowo is Assistant Lecturer, KCMU Co.
Mr. Patrick is Tutorial Assistant, KCMU Co.
Dr. Bartlett is Professor of Medicine, Global Health and Nursing, Duke University Medical Center, Durham, NC.
References
- Abdelkhalek A, Hussein A, Gibbs T, Hamdy H. Using team-based - learning to prepare medical students for future problem-based learning. Medical Teacher. 2010;32:123–129. doi: 10.3109/01421590903548539. [DOI] [PubMed] [Google Scholar]
- Cestone CM, Levine RE, Lane DR. Peer Assessment and Evaluation in Team- Based Learning. New Directions for teaching and learning. 2008;(116) doi: 10.1002/tl.334. [DOI] [Google Scholar]
- Chen C, Buch E, Wassermann T, et al. A survey of Sub-Saharan medical schools. Human Resources for Health. 2012;10:4. doi: 10.1186/1478-4491-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung EK, Rhee JA, Baik YH, AOS The effect of team-based learning in medical ethics education. Med Teach. 2009;31(11):1013–17. doi: 10.3109/01421590802590553. [DOI] [PubMed] [Google Scholar]
- Goo AB. Team-based learning and social loafing in Higher Education. University of Tennessee Honors Thesis Project. 2011 http:trace.tennessee.edu/utk_chanhonopro/1423.
- Haidet P, Levine RE, Parmelee DX, Crow S, Kennedy F, Kelly PA, Perkowski L, Michaelsen L, Richards BF. Guidelines for Reporting Team-Based Learning Activities in the Medical and Health Sciences Education Literature. Academic Medicine. 2012;87(3):292–299. doi: 10.1097/ACM.0b013e318244759e. [DOI] [PubMed] [Google Scholar]
- Kamei RK, Cook S, Puthucheary J, Starmer CF. 21st century learning in medicine: Traditional Teaching versus Team-based learning. Med Sci Edu. 2012;22 (2):57–64. [Google Scholar]
- Kenny P. Assessing the impact of Team based learning and the examination performance of undergraduate taxation law students. 2003 http//Sydney.edu//law/parsons/ATT/docs.
- McInerney MJ, Fink LD. Team-based learning enhances long- retention and critical thinking in an undergraduate microbial physiology. 2003. doi:1128/jmbe.v4.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaelsen LK, Parmalee D, McMahon K, Levine R, Billings D. Team-based learning for health professions education. Stylus Publishing LLC; 2008. [Google Scholar]
- Michaelsen LK, Sweet M. The essential elements of team-based learning. New directions for teaching and learning. 2008;2008(116):7–27. doi: 10.1002/tl.330. [DOI] [Google Scholar]
- Michaelsen KL. Three keys to using learning groups effectively. Teaching Excellence: Towards the best in the Academy. 1997–1998;9(5) AMES IA::POD. Network. Ames, IA, Rev 10/107. [Google Scholar]
- Mullan F, Frehywot S, Omaswa F, et al. Medical Schools in sub-Saharan Africa. The Lancet. 2011;377:1113–1121. doi: 10.1016/S0140-6736(10)61961-7. doi:1016/SO140-6736(10)61961-7. [DOI] [PubMed] [Google Scholar]
- Neider GL, Parmelee DX, Stolfi A, Hudes PD. Team-based learning in a medical gross anatomy and embryology course. Clinical Anatomy. 2005;18(1):56–53. doi: 10.1002/ca.20040. [DOI] [PubMed] [Google Scholar]
- Parmelee D, Michaelsen LK, Cook S, Hudes PD. Team-based learning: A practical guide: AMEE Guide No. 65. Medical Teacher. 2012;34(5):e275–87. doi: 10.3109/0142159X.2012.651179. [DOI] [PubMed] [Google Scholar]
- Tastle W, Russell J, Wierman MJ. A new measure to analyze student performance using the Likert Scale. Proc ISECON. 2005;22:1–7. [Google Scholar]
- Vasan NS, DeFouw DO, Compton S. A survey of student perceptions of team- based learning in anatomy curriculum: Favorable views unrelated to grades. Anat Sci Educ. 2009;2:150–155. doi: 10.1002/ase.91. [DOI] [PubMed] [Google Scholar]