Abstract
Long-term granulocyte-colony stimulating factor treatment has been shown to be safe and effective in severe chronic neutropenia patients. However, data on its use during pregnancy are limited. To address this issue, we analyzed all pregnancies reported to the European branch of the Severe Chronic Neutropenia International Registry since 1994. A total of 38 pregnancies in 21 women with chronic neutropenia (16 pregnancies in 10 women with congenital, 10 in 6 women with cyclic, 12 in 5 women with idiopathic neutropenia) were reported. Granulocyte-colony stimulating factor was administered throughout pregnancy in 16 women and for at least one trimester in a further 5 women. No major differences were seen between treated and untreated women with respect to pregnancy outcome, newborn complications and infections. In addition, we evaluated the genetic transmission of known or suspected genetic defects in 16 mothers having 22 newborns as well as in 8 men fathering 15 children. As a proof of inheritance, neutropenia was passed on to the newborn in 58% from female and in 62% from male patients with ELANE mutations, but also to some newborns from parents with unknown gene mutation. Based on our results, granulocyte-colony stimulating factor therapy has been shown to be safe for mothers throughout pregnancies and for newborns without any signs of teratogenicity. With an increasing number of adult patients, genetic counseling prior to conception and supportive care of mothers during pregnancy are crucial. The acceptance of having affected children may reflect the high quality of life obtained due to this treatment.
Introduction
Severe chronic neutropenia is a heterogeneous group of inherited and acquired rare disorders with a common hematologic and clinical phenotype. It is characterized by peripheral blood absolute neutrophil counts below 0.5×109/L and early onset of bacterial infections.
Prior to the availability of recombinant human granulocyte-colony stimulating factor (G-CSF), patients with severe chronic neutropenia experienced frequent bacterial infections and required multiple antibiotic courses.
Data from the Severe Chronic Neutropenia International Registry (SCNIR) have demonstrated that more than 90% of all treated patients respond well to granulocyte-colony stimulating factor with a sustained increase in absolute neutrophil counts. Thus, patients are significantly less prone to bacterial infections. As a consequence, life expectancy is prolonged and our first patients have reached adulthood with the desire for parenthood being an emerging issue.1–3 Patients and physicians often ask about the benefits and safety of G-CSF treatment during pregnancy and this led us to initiate this survey.
So far, only limited data are available on the risk of developing severe bacterial infections during pregnancy for women suffering from severe chronic neutropenia (including congenital, cyclic and idiopathic neutropenia) with or without G-CSF treatment.
Because of the clinically distinguishable entities, in this paper we discriminate between congenital and cyclic neutropenia. While congenital neutropenia patients present with persistent neutropenia, patients with cyclic neutropenia have a cycling pattern of blood counts (neutrophils, platelets, reticulocytes, monocytes). For practical reasons, we use the term congenital neutropenia patients with non-cyclic congenital neutropenias and the term cyclic neutropenia for patients with cyclic hematopoiesis.
Current data on the molecular causes indicate that congenital neutropenia is a genetic disorder with more than 10 underlying gene mutations described to date. However, in approximately 30% of patients the genetic basis of congenital neutropenia is still unknown. Gene mutations responsible for congenital neutropenia follow an autosomal dominant, autosomal recessive or X-linked pattern of inheritance depending on the type of mutation. Genetic analyses in autosomal dominant and sporadic cases of congenital neutropenia indicate that the majority of these cases are attributable to mutations in the elastase 2 (ELANE) gene encoding neutrophil elastase. Thirty-two percent of congenital (CN) and 80% of cyclic (CyN) neutropenia patients harbor ELANE mutations (ELANE-CN vs. ELANE-CyN), as reported by the European branch of the Severe Chronic Neutropenia International Registry. Although some mutations are related to both congenital and cyclic neutropenia, the clinical phenotype and course of disease differ significantly: ELANE-CN patients have severe chronic neutropenia with a substantial risk of life-threatening infections and a high risk for secondary leukemias. They require higher G-CSF doses and may develop G-CSF receptor (CSF3R/colony stimulating factor 3 receptor) mutations during life. In contrast, ELANE-CyN patients respond to lower G-CSF doses and show the typical cycling of neutrophil counts throughout their life without malignant transformation. Recessive inheritance of congenital neutropenia is related to HAX1 gene mutations (Kostmann syndrome patients) and a number of other rare mutations that are mainly associated with multi-organ involvement, for example, SBDS, G6PT (SLC37A4), G6PC3 and p14 (LAMTOR2, MAPBPIP). In X-linked subtypes, mutations in TAZ or WAS may be detected.4–11 The clinical status in newborns of mothers and fathers with different genetic subtypes of congenital neutropenia has not yet been reported.
Acquired neutropenias may be due to different reasons, e.g. drug- or virus-induced or anti-granulocyte antibody-related. Patients with acquired neutropenia for unknown reasons are classified as idiopathic neutropenia.
In this study, we assessed the outcome of pregnancies reported to the SCNIR in Europe since 1994 with regard to:
use of G-CSF and dosing during pregnancy;
the impact of G-CSF treatment on pregnancy outcome, maternal and newborn complications (e.g. infections during pregnancy and fetal teratogenicity) in all neutropenia subtypes;
the transmission of inherited neutropenia to newborns of mothers and fathers with different genetic neutropenia subtypes.
Methods
Severe Chronic Neutropenia International Registry
Between November 1987 and August 2013, 601 patients with different subtypes of severe chronic neutropenia were enrolled in the Severe Chronic Neutropenia International Registry (SCNIR) in Europe, based in Hannover, Germany. As a basis for our analysis, out of the 601 patients, we identified 329 adults (female n=172; male n=157) aged 18 years or over who were hence considered to be of a reproductive age. The study was conducted in accordance with the Declaration of Helsinki, under the auspices of the Human Subjects Committee of the Medical School in Hannover, Germany, and other participating institutions.
Patients were enrolled on referral from cooperating hematologists, pediatricians and other physicians in Europe using standard enrollment procedures.1 At the time of enrollment, clinical and laboratory information was reviewed by an expert clinician associated with the Severe Chronic Neutropenia International Registry (SCNIR). Annual follow-up information was entered into a standardized database. Data on complications during pregnancy, pregnancy outcome and newborn complications have been gathered by a survey using specific questionnaires.
All G-CSF dose data (in micrograms per kilogram per day, μg/kg/d) were obtained from the visit closest in time prior to pregnancy and were compared to the doses reported for each trimester during pregnancy.
Statistical analysis
We restricted our analysis to adult male and female patients (age ≥ 18 years), with reported father- or motherhood, respectively. Each analysis was carried out using all subjects with available data. We estimated the effect of G-CSF treatment during pregnancy by comparing infectious events and maternal as well as fetal and newborn complications in treated versus untreated women. We compared the median G-CSF dose values in pregnant women by trimester for each pregnancy versus the median G-CSF dose prior to pregnancy according to neutropenia subtype using the Wilcoxon rank sum test.12 The mean absolute neutrophil counts of treated and untreated mothers were compared with an independent samples t-test.
The incidence of inherited neutropenia was calculated for each genetic subtype based on the newborn absolute neutrophil count and/or molecular genetic testing.
Results
Out of a total of 601 patients with different subtypes of severe chronic neutropenia enrolled in the Severe Chronic Neutropenia International Registry (SCNIR) in Europe, 329 patients aged 18 years and above (female n=172; male n=157), considered to be of a reproductive age, were available for our study. Out of the female cohort (172 patients), 38 pregnancies were reported in 21 women (16 pregnancies in 10 women with congenital neutropenia, 10 pregnancies in 6 women with cyclic neutropenia, 12 pregnancies in 6 women with idiopathic neutropenia). In addition, we collected data on 9 men fathering 16 children (8 children of 5 fathers with congenital neutropenia, 7 children of 3 fathers with cyclic neutropenia, one child of a father with idiopathic neutropenia) (Figure 1).
Figure 1.
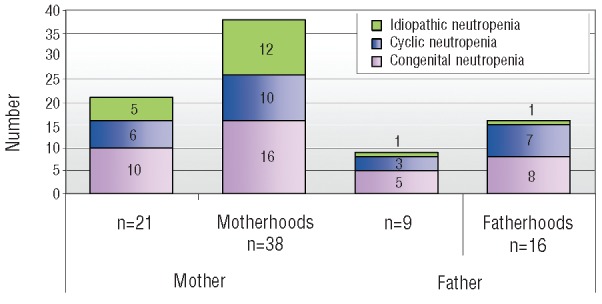
Distribution of mother- and fatherhood by neutropenia subtype. Congenital neutropenia in purple; cyclic neutropenia in blue and idiopathic neutropenia in green. The first two columns of the figure show the total number of pregnant women (column 1) and the number of reported pregnancies (column 2) for those women. The third column indicates the number of fathers and the fourth column the number of fatherhoods.
The median age of the mothers at delivery was 29 years with a maximum age of 35 years. Hence, there were no women with age-related high-risk pregnancies in our analysis; this has been reported to be significantly increased from age 35–40 years and even higher in women aged over 40 years.13,14
Use of G-CSF and dosing during pregnancy
Data on the use of G-CSF were available in 35 of the 38 pregnancies. As shown in Figure 2, G-CSF was administered in 21 pregnancies of 14 women (congenital neutropenia: 13 pregnancies of 9 women; cyclic neutropenia: 5 pregnancies of 3 women; idiopathic neutropenia: 3 pregnancies of 2 women). Whereas the majority (81%) of pregnant women diagnosed with congenital neutropenia received G-CSF for at least one trimester, only 50% of the women with cyclic neutropenia and 25% of women with idiopathic neutropenia were treated. One mother with cyclic neutropenia re-started G-CSF treatment for the last seven weeks of her pregnancy after she had stopped treatment more than one year prior to pregnancy.
Figure 2.
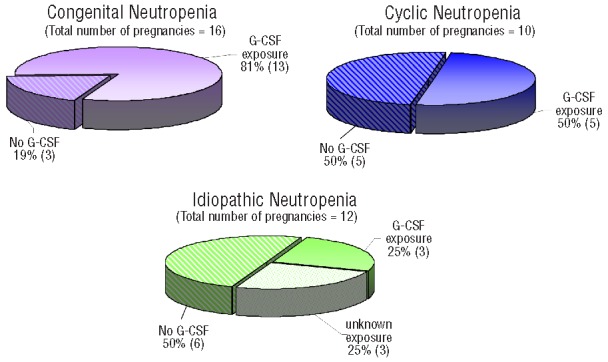
G-CSF Treatment of mothers during pregnancy by neutropenia subtype. The pie charts show the maternal G-CSF exposure (G-CSF exposure, no G-CSF, unknown exposure) by neutropenia subtype for each pregnancy: congenital neutropenia in purple, cyclic neutropenia in blue and idiopathic neutropenia in green.
Three patients suffering from congenital neutropenia did not receive G-CSF treatment for at least six months prior to as well as during their pregnancy: One of these women became pregnant prior to the availability of G-CSF, one woman withdrew treatment despite history of severe infections, and one woman stopped G-CSF for family planning. One woman with cyclic neutropenia stopped G-CSF treatment prior to pregnancy and developed a serious uterine infection followed by septic abortion (see below).
Figure 3 shows the G-CSF doses during pregnancy for each trimester. For this analysis, patients were divided according to neutropenia subtype comparing the median G-CSF dose prior to pregnancy (μg/kg/d) to the dose for each trimester. Sixteen women received G-CSF throughout their entire pregnancy. In all but one woman with a stable long-term G-CSF dose G-CSF was continued during the first trimester of the pregnancy independent of the neutropenia subtype. Seven of the 12 women with congenital neutropenia continued G-CSF during the second and third trimesters. Two women re-started treatment only for the last trimester. Four women with cyclic neutropenia received G-CSF treatment throughout their pregnancy and one only for the last trimester. One out of the 3 idiopathic neutropenia women discontinued G-CSF treatment for the second and third trimesters.
Figure 3.
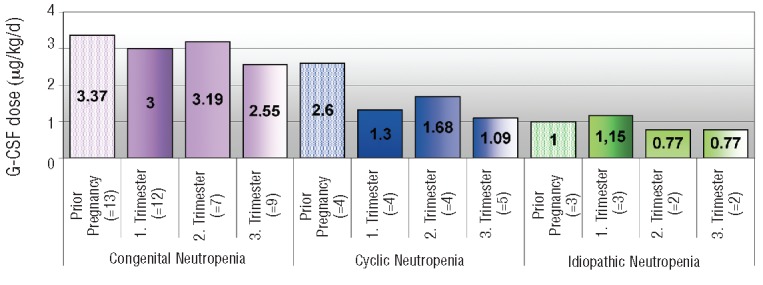
Median G-CSF dose prior and during pregnancy by neutropenia subtype. In the figure the median G-CSF doses (μg/kg/d) for each neutropenia subtype (congenital neutropenia in purple; cyclic neutropenia in blue and idiopathic neutropenia in green) prior to pregnancy (first column) are compared to the median G-CSF dose during pregnancy divided into the three trimesters (2–4 columns of each color).
In general, patients with congenital neutropenia require higher median G-CSF doses than those with cyclic or idiopathic neutropenia due to the severity of the underlying disease. This was also observed in our survey. Intriguingly, in all pregnancies, the G-CSF dose used was lower than the median dose prior to pregnancy indicating that patients were monitored more carefully during pregnancy and G-CSF was dosed as low as possible.
Absolute neutrophil counts were available in 18 of 21 women (13 treated and 5 untreated) of our cohort. A total of 37 complete blood counts (CBC) were available in the treated women showing a mean absolute neutrophil count of 4572 and a median of 2600. In the 16 CBC of untreated women the mean absolute neutrophil count was 615 and the median was 475. The mean absolute neutrophil counts differ significantly between treated and untreated women (P=<0.01).
Impact of G-CSF treatment on pregnancy outcome, maternal and newborn complications (e.g. infections during pregnancy and fetal teratogenicity) in all neutropenia subtypes
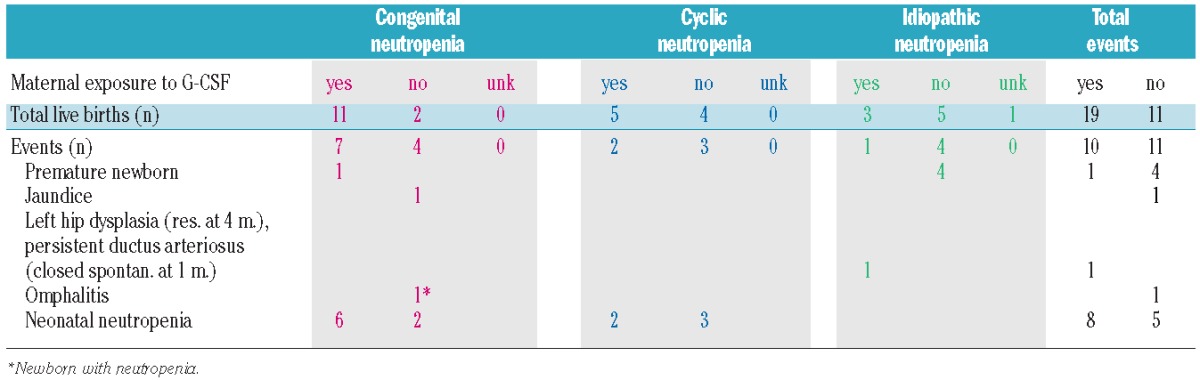
The European branch of the SCNIR gathered all pre- and postnatal complications concerning mothers and children in correlation with G-CSF as shown in Tables 1 and 2.
Table 1.
Reported maternal and fetal complications.
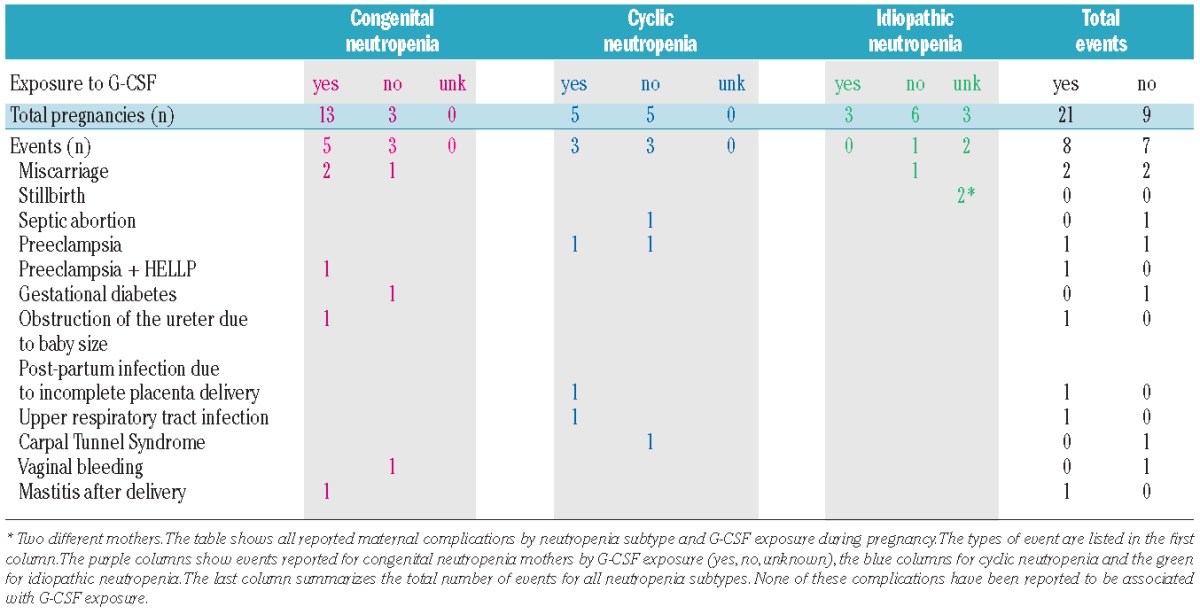
Table 2.
Reported newborn complications.
Pregnancy outcome
Miscarriages, defined by the World Health Organization (WHO) as the premature loss of a fetus up to 23 weeks of pregnancy and weighing up to 500g,15 were reported in both pregnancies with (2 of 21) and without (3 of 14) G-CSF treatment: In G-CSF treated women with congenital neutropenia 2 of 16 (age of mothers: 24 and 27 years) pregnancies resulted in spontaneous miscarriages in weeks six and 11, respectively; none were reported in treated women suffering from cyclic or idiopathic neutropenia. One untreated 28-year old woman with congenital and one untreated 31-year old women with idiopathic neutropenia had one miscarriage each. One untreated 24-year old woman with cyclic neutropenia had a septic abortion (Table 1).
Two stillbirths were reported in women with idiopathic neutropenia. Unfortunately, no information on G-CSF treatment during these pregnancies was available. One of these women had 3 premature newborns in later pregnancies. She delivered one child at 30 weeks of gestation and premature twins (26 weeks of gestation) in another pregnancy. One of the twins died on Day four after birth for unknown reasons. A second untreated woman with idiopathic neutropenia delivered her baby at 36 weeks of gestation. One treated congenital neutropenia patient with SBDS mutation gave birth to a 25+4 week old newborn. In summary, a total of 5 preterm deliveries were reported in our cohort (Table 1).
Maternal complications
Preeclampsia was the most frequent reported maternal complication and occurred in treated as well as untreated women (Table 1). In a 23-year old woman with Shwachman-Diamond Syndrome, preeclampsia with HELLP syndrome led to delivery of a 25+4 week premature healthy baby (see above). Other maternal complications were rare. Gestational diabetes was reported in a 26-year old woman suffering from congenital neutropenia who was not exposed to G-CSF. She also reported vaginal bleeding in her second trimester. An obstruction of the ureter due to the size of the baby was documented in one treated 22-year old woman with congenital neutropenia.
One untreated 24-year old woman with cyclic neutropenia who had stopped G-CSF treatment prior to pregnancy developed a serious uterine infection followed by a septic abortion. Another 34-year old woman with cyclic neutropenia required surgery for Carpal Tunnel Syndrome which developed due to peripheral edema while she was not receiving G-CSF. Therapy was re-started for the surgery and maintained for the remaining seven weeks of pregnancy; the pregnancy was later complicated by preeclampsia and upper respiratory tract infection.
After delivery, one treated 29-year old woman with congenital neutropenia developed mastitis and one treated 31-year old woman with cyclic neutropenia experienced an uterine infection due to incomplete placenta delivery.
Newborn complications
Reported newborn complications included jaundice, hip dysplasia, omphalitis and neonatal neutropenia (Table 2).
The transmission of inherited neutropenia to newborns of mothers and fathers with different genetic neutropenia subtypes
To exclude or confirm neutropenia, CBC was taken in 25 of 41 newborns of mothers and fathers suffering from congenital or cyclic neutropenia at birth and in 4 babies later in life. Results are listed in Tables 3 and 4.
Table 3.
Inheritance of neutropenia from affected mothers.
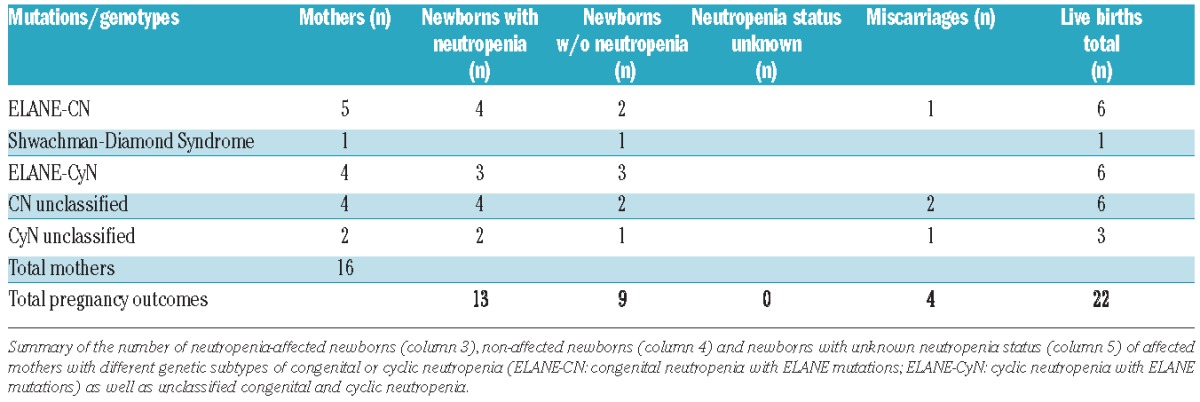
Table 4.
Inheritance of neutropenia from affected fathers.
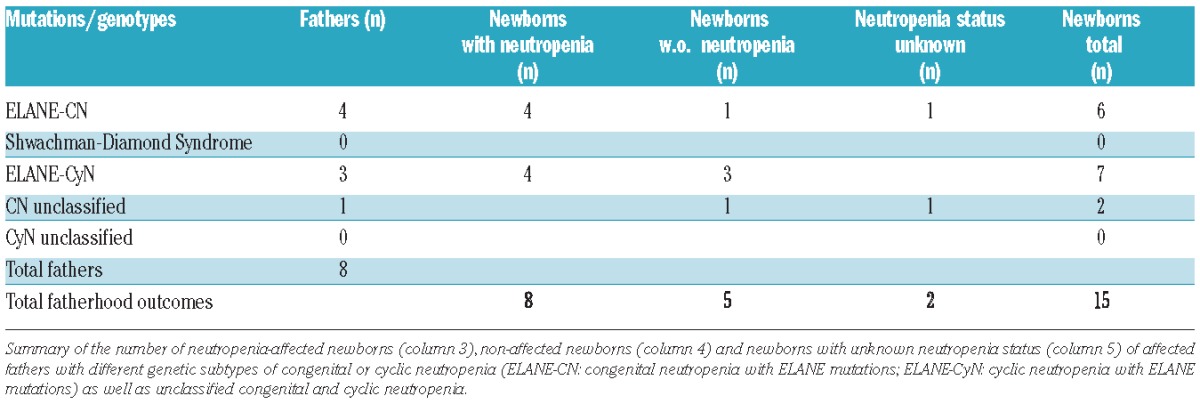
Transmission of neutropenia was evaluated in newborns of 9 mothers and 7 fathers with known neutropenia causing dominant ELANE mutation (congenital and cyclic neutropenia) and in newborns of mothers and fathers with unclassified congenital or cyclic neutropenia (6 women, one man) In 7 of 12 newborns neutropenia was passed on from the mother (58%). In 8 of 13 newborns the neutropenia was passed on from the fathers (62%). One woman suffered from Shwachman-Diamond Syndrome characterized by compound heterozygous SBDS mutations without transmission to her baby, as expected.
Interestingly, neutropenia was not only reported in children of parents with ELANE mutations, but also in 6 of 11 newborns of parents with congenital (4 women, one man) and cyclic neutropenia (2 women, no men) negative for ELANE and HAX1 gene mutation or so far genetically not tested. In one of these 11 newborns, the neutropenia status is unknown. The occurrence of congenital or cyclic neutropenia in these children indicates the transmission of the neutropenia from their parents and suggests that these parents suffer from another autosomal dominant genetic defect.
Discussion
In the past, pregnancy has been a major concern for patients with severe chronic neutropenia, considered to increase the susceptibility to infections for women with severe chronic neutropenia. For example, a 20-year old woman was sterilized in the late 1980s prior to her marriage to prevent infections in the post-partum period. In 1998, this woman became pregnant by in vitro fertilization (IVF). She received G-CSF treatment in the last weeks of her pregnancy and gave birth to a healthy baby without developing any severe bacterial infections pre- and postpartum.16 Interestingly, in reports on 2 women with cyclic neutropenia by Katz17 and Pajor,18 the severity of neutropenia-related symptoms decreased during pregnancy even without G-CSF treatment, suggesting endogenous upregulation of G-CSF and/or other hormones involved in hematopoiesis.
Since the late 1980s, granulocyte-colony stimulating factor (G-CSF) has been shown to be most effective in the treatment of patients with severe chronic neutropenia by increasing the absolute neutrophil counts and decreasing the risk of bacterial infections significantly.3,19,20 In addition, this treatment has prolonged the survival of patients suffering from severe chronic neutropenia, especially congenital neutropenia subtypes, the most severe form that in the past was associated with poor outcome. Under long-term G-CSF treatment, even congenital neutropenia patients have now reached adulthood and, therefore, the desire to have children is now presenting itself.
There are no formal recommendations regarding the use of G-CSF during pregnancy in women suffering from severe chronic neutropenia. However, single case reports documented that the use of G-CSF in pregnant women was safe and well tolerated, although most of the women received G-CSF only during the very last weeks of pregnancy16 or even when labor had already started in order to prevent possible adverse effects on the fetus.21 One woman with acquired chronic neutropenia and severe infectious complications after delivery of her first baby, received G-CSF prophylactically in the second pregnancy from week 37 onwards. Besides a good neutrophil response, she had an uneventful delivery of her second child and no puerperal complications.22 Previous data of the Severe Chronic Neutropenia International Registry (SCNIR) from 2003 indicated that the proportion of live births in mothers receiving G-CSF for a median period of two trimesters was higher than in the untreated women.23 However, numbers were too small to allow reliable recommendations on the use of G-CSF during pregnancy to be developed. In addition, the 2003 study primarily included women with idiopathic neutropenia, whereas our cohort consists mainly of women with severe congenital neutropenia. ELANE mutations were identified in 44% of these women documenting the genetic background of neutropenia.
In general, patients with congenital neutropenia require higher G-CSF doses than patients with cyclic or idiopathic neutropenia and this correlates to the severity of the clinical phenotype (e.g. impaired neutrophil production) and the resulting risk of bacterial infections. In our cohort of 21 women, no bacterial infections were reported during pregnancy, regardless of the administration of G-CSF. In the majority of documented pregnancies, women received G-CSF for a minimum of one trimester. Reflecting the severity of the underlying neutropenia subtype, 81% of congenital compared to 50% of cyclic and 25% of idiopathic neutropenia patients were treated. Fortunately, none of our patients experienced severe bacterial infections. The high proportion of treated women with the most severe clinical phenotype (congenital neutropenia) corresponds to the widely-reported high susceptibility of bacterial infections and the documented risk of death from sepsis in these patients.24
Since G-CSF crosses the placental barrier, G-CSF treatment during the late phase of pregnancy may also prevent newborns with inherited neutropenia from perinatal infections.25 This may be due to a neutrophil response in the baby.
Compared to the doses prior to pregnancy, the median G-CSF doses administered during pregnancy were slightly lower in our cohort. This finding may indicate that women were monitored more carefully during pregnancy in order to adjust the G-CSF dose to the minimal amount needed to maintain the neutrophil count above 1×109/L. Another explanation for sufficient absolute neutrophil numbers under lower G-CSF doses might be the improvement of neutropenia due to intrinsic increased levels of steroid hormones and hematopoietic growth factors including endogenous G-CSF during pregnancy that was reported in cyclic neutropenia patients.26
Our evaluation demonstrates that G-CSF treatment resulted in a significantly higher mean absolute neutrophil count in treated compared to untreated women indicating a better ability to fight bacterial infections.
Thirty-one of the total 38 pregnancies resulted in live births (82%). Our analysis showed a minor difference between the proportion of miscarriages and septic abortions in treated versus untreated mothers (2 vs. 3). Two stillbirths were reported in one untreated mother and one mother with unknown G-CSF exposure, both suffering from idiopathic neutropenia. A significantly higher rate of spontaneous miscarriages in untreated pregnant women with severe chronic neutropenia had been previously reported by Boxer et al. but could not be confirmed in our study, where the difference in the number of miscarriages was not significant.23
In our cohort, we documented 5 preterm deliveries in 3 different women corresponding to an incidence of 13.2%. This incidence is significantly higher than the overall incidence of premature newborns in Europe (2010: 6.2%).27 Advanced age as an additional risk factor for premature delivery could be excluded in our cohort. The median age of the mothers at birth was 29 years (max. 35 years). A significantly increased risk of premature delivery has been reported for women from the age of 35–40 years and is even higher in women aged over 40 years.13,14 In the majority of pregnancies resulting in preterm delivery, no G-CSF was given. One preterm delivery was related to preeclampsia in a woman with Shwachman-Diamond syndrome.
In summary, our evaluation demonstrates that the use of G-CSF throughout pregnancy is safe and well tolerated. No noticeable side effects were reported. Our data support the recommendation to continue G-CSF treatment in women with different types of severe chronic neutropenia throughout pregnancy to prevent major infections and newborn complications. The recommendation is based on the reported high risk for bacterial infections and septic death in severe congenital neutropenia. The risk may be lower for patients suffering from cyclic or idiopathic neutropenia. However, since there is no better predictor for this risk than the absolute neutrophil count, we would recommend offering G-CSF treatment to all patients with absolute neutrophil counts below 0.5×109/L.
Compared to the number of motherhoods, the number of reported fatherhoods is much lower. This may be due to the low median age (23.9 years) of the male cohort. In addition, fatherhoods may be under-reported in the follow-up questionnaires.
The high frequency of inherited neutropenias in newborns from affected congenital neutropenia mothers with autosomal dominant gene mutations may result in a higher risk of puerperal complications. It remains unclear whether G-CSF administration to the mother at the time of delivery can alleviate infections in neutropenic newborns.
In addition to the concern about the safety of G-CSF during pregnancy, the question of transmission of the neutropenia from parent to child has to be addressed. We, therefore, analyzed the occurrence of neutropenia in newborns of congenital and cyclic neutropenia parents with known or unknown germ-line gene mutations. Twenty-five newborns were born to mothers or fathers (congenital and cyclic neutropenia) with known ELANE mutation. Of the 25 newborns, 15 were affected by neutropenia confirming the dominant inheritance of these mutations. This proportion (60%) is higher than statistically expected for dominant inheritance that may be due to the low number of patients. Interestingly, the prevalence of neutropenia in children from parents with unknown inherited gene mutations indicates the existence of a yet unidentified gene mutation.
In general, the number of patients reaching adulthood and developing a desire to have children is increasing, thus the interest in pregnancy has become a crucial issue. Due to the advances in genetic testing, the number of neutropenia-causing gene mutations is still increasing. Genetic counseling should be offered to all affected patients and their families. Inheritance should also be considered in patients with unclassified congenital neutropenia since neutropenia may be passed on by either parent in an autosomal dominant pattern, as shown by our results. The acceptance of having affected children may reflect the high quality of life afforded by G-CSF treatment in affected parents.
Acknowledgments
We thank all colleagues associated with the Severe Chronic Neutropenia International Registry for their continued assistance. We are also grateful to the many physicians worldwide who faithfully and generously submitted data on their patients and the patients for their consent.
Special thanks to those colleagues who shared their data on the patients reported in this publication and to Prof. Sally Kinsey for reviewing the manuscript.
Footnotes
Funding
This work was partially supported by grants from the NIH and the German Ministry of Education and Research.
Authorship and Disclosures
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
- 1.Welte K, Zeidler C. Severe congenital neutropenia. Hematol Oncol Clin North Am. 2009;23(2):307–20 [DOI] [PubMed] [Google Scholar]
- 2.Zeidler C, Germeshausen M, Klein C, Welte K. Clinical implications of ELA2-, HAX1-, and G-CSF-receptor (CSF3R) mutations in severe congenital neutropenia. Br J Haematol. 2009;144(4):459–67 [DOI] [PubMed] [Google Scholar]
- 3.Bonilla MA, Gillio AP, Ruggeiro M, Kernan NA, Brochstein JA, Abboud M, et al. Effects of recombinant human granulocyte colony-stimulating factor on neutropenia in patients with congenital agranulocytosis. N Engl J Med. 1989;320(24):1574–80 [DOI] [PubMed] [Google Scholar]
- 4.Dale DC, Person RE, Bolyard AA, Aprikyan AG, Bos C, Bonilla MA, et al. Mutations in the gene encoding neutrophil elastase in congenital and cyclic neutropenia. Blood. 2000;96(7):2317–22 [PubMed] [Google Scholar]
- 5.Horwitz MS, Duan Z, Korkmaz B, Lee HH, Mealiffe ME, Salipante SJ. Neutrophil elastase in cyclic and severe congenital neutropenia. Blood. 2007;109(5):1817–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klein C, Grudzien M, Appaswamy G, Germeshausen M, Sandrock I, Schäffer AA, et al. HAX1 deficiency causes autosomal recessive severe congenital neutropenia (Kostmann disease). Nat Genet. 2007;39(1):86–92 [DOI] [PubMed] [Google Scholar]
- 7.Boztug K, Appaswamy G, Ashikov A, Schäffer AA, Salzer U, Diestelhorst J, et al. A syndrome with congenital neutropenia and mutations in G6PC3. N Engl J Med. 2009;360:32–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bione S, D’Adamo P, Maestrini E, Gedeon AK, Bolhuis PA, Toniolo D. A novel X-linked gene, G4.5. is responsible for Barth syndrome. Nat Genet. 1996;12(4):385–9 [DOI] [PubMed] [Google Scholar]
- 9.Bohn G, Allroth A, Brandes G, Thiel J, Glocker E, Schäffer AA, et al. A novel human primary immunodeficiency syndrome caused by deficiency of the endosomal adaptor protein p14. Nat Med. 2007;13(1):38–45 [DOI] [PubMed] [Google Scholar]
- 10.Devriendt K, Kim AS, Mathijs G, Frints SG, Schwartz M, Van Den Oord JJ, et al. Constitutively activating mutation in WASP causes X-linked severe congenital neutropenia. Nat Genet. 2001;27(3):313–7 [DOI] [PubMed] [Google Scholar]
- 11.Person RE, Li FQ, Duan Z, Benson KF, Wechsler J, Papadaki HA, et al. Mutations in proto-oncogene GFI1 cause human neutropenia and target ELA2. Nat Genet. 2003;34(3):308–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilcoxon F. Individual comparisons by ranking methods. Biometrics. 1945;1:80–3 [Google Scholar]
- 13.Jolly M, Sebire N, Harris J, et al. The risks associated with pregnancy in women aged 35 years or older. Human Reproduction. 2000;15(11):2433–7 [DOI] [PubMed] [Google Scholar]
- 14.Joseph KS, Allen AC, Dods L, Turner L, Scott H, Liston R. The perinatal effects of delayed childbearing. Obstet Gynecol. 2005;22(5):1410–8 [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. Definitions and indicators in family planning, maternal and child health and reproductive health. WHO Regional Strategy on Sexual and Reproductive Health. 2001 [Google Scholar]
- 16.Kaufmann SJ. Term delivery in a woman with severe congenital neutropenia, treated with growth colony stimulating factor, Case report. Hum Reprod. 1998;13(2):498–9 [DOI] [PubMed] [Google Scholar]
- 17.Katz VL, Egley CC, Bowes WA., Jr Cyclic neutropenia and pregnancy. South Med J. 1988;81(4):527–8 [DOI] [PubMed] [Google Scholar]
- 18.Pajor A, Szakács Z. Pregnancy in Cyclic Neutropenia, Case report. Gynecol Obstet Invest. 1991;32(3):189–90 [DOI] [PubMed] [Google Scholar]
- 19.Zeidler C, Welte K. Hematopoietic growth factors for the treatment of inherited cytopenias. Semin Hematol. 2007; 44(3):133–7 [DOI] [PubMed] [Google Scholar]
- 20.Welte K, Zeidler C, Dale DC. Severe congenital neutropenia. Semin Hematol. 2006; 43(3):189–95 [DOI] [PubMed] [Google Scholar]
- 21.Abe T, Azuma H, Watanabe A, Shigekiyo T, Endou S, Pou R, et al. A patient with cyclic neutropenia complicated by severe persistent neutropenia successfully delivered a healthy baby. Intern Med. 2000; 39(8):663–6 [DOI] [PubMed] [Google Scholar]
- 22.Sangalli MR, Peek M, McDonald A. Prophylactic granulocyte colony-stimulating factor treatment for acquired chronic severe neutropenia in pregnancy, Case report. Aust N Z J Obstet Gynaecol. 2001; 41(4):470–1 [DOI] [PubMed] [Google Scholar]
- 23.Boxer LA, Bolyard AA, Marrero TM, Phan L, Bond JM, Alter BP, et al. Impact of G-CSF on Outcomes of Pregnancy in Women with Severe Chronic Neutropenia. Blood, (ASH Annual Meeting Abstracts) 2010. Abstract 4786 [Google Scholar]
- 24.Rosenberg PS, Alter BP, Bolyard AA, Bonilla MA, Boxer LA, Cham B, et al. The incidence of leukemia and mortality from sepsis in patients with severe congenital neutropenia receiving long-term G-CSF therapy. Blood. 2006;15;107(12):4628–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Medlock ES, Kaplan DL, Cecchini M, Ulich TR, del Castillo J, Andresen J. Granulocyte colony-stimulating factor crosses the placenta and stimulates fetal rat granulopoiesis. Blood. 1993;81(4):916–22 [PubMed] [Google Scholar]
- 26.Polcz TE, Stiller RJ, Whetham JC. Pregnancy in patients with cyclic neutropenia. 1. Am J Obstet Gynecol. 1993;169(2 Pt 1):393–4 [DOI] [PubMed] [Google Scholar]
- 27.Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo JH, et al. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010;88:31–8 [DOI] [PMC free article] [PubMed] [Google Scholar]


