Abstract
Purpose
Alcohol abuse and dependence are collectively referred to as alcohol use disorders (AUD). An AUD is present in up to one third of patients admitted to an intensive care unit (ICU). We sought to understand the barriers and facilitators to change in ICU survivors with an AUD in order to provide a foundation upon which to tailor alcohol-related interventions.
Methods
We utilized a qualitative approach with a broad constructivist framework, conducting semistructured interviews in medical ICU survivors with an AUD. Patients were included if they were admitted to one of two medical ICUs and were excluded if they refused participation, were unable to participate, or did not speak English. Digitally recorded and professionally transcribed interviews were analyzed using a general inductive approach and grouped into themes.
Results
Nineteen patients were included with an average age of 51 [interquartile range (IQR) 36–51] years and an average APACHE II score of 9 [IQR 5–13]; 68% were Caucasian, 74% were male, and the most common reason for admission was alcohol withdrawal (n = 8). We identified five facilitators of change: empathy of the inpatient healthcare environment, recognition of accumulating problems, religion, pressure from others to stop drinking, and trigger events. We identified 3 barriers to change: missed opportunities, psychiatric comorbidity, and cognitive dysfunction. Social networks were identified as either a barrier or facilitator to change depending on the specific context.
Conclusions
Alcohol-related interventions to motivate and sustain behavior change could be tailored to ICU survivors by accounting for unique barriers and facilitators.
Keywords: Intensive care unit, critical illness, alcohol use disorder, brief intervention, motivational interviewing
INTRODUCTION
Alcohol abuse and dependence are collectively referred to as alcohol use disorders (AUDs) and are associated with multiple poor health-related outcomes [1]. The presence of an AUD increases the risk of developing a several diseases commonly cared for in an intensive care unit including acute respiratory distress syndrome (ARDS) [2], septic shock [3], acute respiratory failure[4], severe community acquired pneumonia[5], and hospital-acquired infections [6]. As a result, AUDs are present in up to one-third of patients admitted to an ICU [2, 3, 7, 8]. Because of improvements in care, more than 80% of patients admitted to an ICU survive their hospitalization [9]. However, within one year of hospital discharge 44% of patients with an AUD who required ICU care are readmitted to the hospital or die [10]. As an enforced period of abstinence, admission to the hospital presents an ideal opportunity to address a patient’s underlying AUD and prevent future alcohol-related illness [11].
Brief interventions are 5 to 30 minute sessions spent with a patient addressing their alcohol consumption, identifying goals, and assembling a plan to reduce alcohol-related harm [1, 12]. Such interventions are frequently delivered to patients who are not specifically seeking help for their drinking [13]. These brief interventions have been extensively studied in medical inpatients, trauma patients, and emergency department patients [14–16]. There is general consensus that the efficacy varies between healthcare setting though the precise patient or setting related characteristics associated with the variation in efficacy are unclear [16, 17]. Furthermore, brief interventions have not been studied in medical ICU survivors.
Based upon experts in the field advocating for the development of interventions in a novel setting, we sought to understand how medical ICU survivors with AUDs decide to change their drinking behaviors [18]. Our aim was to identify themes surrounding the decision to change drinking behaviors that could be used to specifically tailor brief interventions for AUDs in medical ICU survivors.
METHODS
Study Design
A broad constructivist framework guided this study where language and meaning connect the experience as shared to its context [19]. A qualitative approach was most appropriate for this study to allow for an in depth exploration of the complexity of human experience and helps build a comprehensive understanding of patients’ choices and influencing factors surrounding alcohol use, potential for changes in behavior, and the impact of the ICU environment. We used a qualitative descriptive approach described by Sandelowski and conducted in-depth individual interviews [20]. This study was reviewed and approved by the local Institutional Review Board (COMIRB protocol # 08-0305) and all patients provided informed consent for participation. Because of the sensitive nature of the interview, a certificate of confidentiality was also obtained from the National Institutes of Health.
Sampling and Recruitment
Patients admitted to two medical ICUs were screened for enrollment in the study. Patients were eligible to participate if they had an Alcohol Use Disorders Identification Test score greater than or equal to 8 or had a history of an AUD, as identified by the treating physician. Patients were excluded if they refused participation in the study, did not speak English, could not provide informed consent, or had a condition that prevented completion of the interview. Purposeful sampling was used to identify information-rich individuals who met criteria for an AUD within the context of an acute medical ICU admission, and who were willing to share detailed knowledge about their choices and perceptions about alcohol, its use and its relationship to their health. Adequacy of the sample size was based on the quality of data and nature of shared experiences [19].
Data Collection
An interview guide was developed based on input from the entire team, clinical experiences and prior research (Table 1). The interview guide was refined as interviews progressed to explore emerging themes [19]. The initial interview template was quickly found to not be sufficiently open-ended and made it difficult to build rapport with some patients. Therefore, during revision, particular attention was paid to begin with questions that would build rapport with the patient and that questions were non-judgmental. For example, instead of beginning the interview by asking the patient whether or not they want to change their drinking, we modified the interview template to ask them to describe their alcohol use. The interview process was supervised by a senior qualitative investigator (JJ) and conducted by BC. A single interview was conducted in person with each patient in a private space within the ICU setting, as a patient’s clinical condition allowed prior to discharge. We verified that the patient was not delirious based on the opinion of the patient’s nurse and primary treating physician. Vigilant attention was paid to the topic focus during the interview but flexibility was balanced to probe new or complex areas of shared experiences. Field notes and analytic memos were maintained throughout the interview process to capture emerging understandings and provide analytic rigor [21]. We conducted semi-structured interviews until we reached thematic saturation [22].
Table 1.
Initial and final templates used to interview patients.
| Initial Interview Template | Final Interview Template |
|---|---|
| Do you want to change your drinking? Why or why not? | Can you describe your alcohol use? |
| Have you every sought help for drinking in the past? | What do you like about it? |
| What did and did not work? | What do you not like about it? |
| What would help you cut down on or stop drinking? | What problems do you associate with it? |
| What influences your drinking? | Can you describe any help you have sought for drinking in the past? |
| What are the biggest problems that you associate with your drinking? | Why do you think it did or did not work? |
| What strategies do you have to cut down on your drinking? | How have people influenced your drinking? |
| When you experience stress, what do you do? | Have you thought about changing your drinking prior to this admission? |
| Were you changing? | |
| What made you more likely to want to change? | |
| What made you less likely to want to change? | |
| How has this changed based on your current illness? | |
| Has anxiety or depression made it difficult for you to change? | |
Qualitative Analysis
Interviews were recorded using a digital recorder and were transcribed by a professional transcriptionist producing 160 pages of text. We used a General Inductive Approach (GIA) to qualitative text data analysis. We grouped codes into themes and explored within case and between case comparisons [23, 24]. Field notes and evolving analytic memos also formed part of the interpretation of data. Credibility and authenticity are enhanced by our team based approach to analysis where unique perspectives, differences in coding and analytic framing are resolved through discussion and consensus [25]. Particular attention was paid to disconfirming or deviant cases to provide alternative interpretations to the emerging conceptual schema [26].
RESULTS
Nineteen interviews with medical ICU patients were conducted between August 2010 and February 2013. Patient characteristics are summarized in Table 2. We could broadly classify themes into barriers or facilitators of change (Table 3). The five key themes that facilitated a decision to stop drinking or to cut down on drinking included: empathy in the inpatient healthcare environment, recognition of alcohol-related problems and risks, religion, pressure from others to stop drinking, and trigger events. Three barriers to cutting down or stopping drinking were missed opportunities, psychiatric comorbidity, and cognitive dysfunction. The patient’s social network was both a facilitator and a barrier, depending on the specific situation.
Table 2.
Baseline characteristics of patients enrolled in the study. IQR, interquartile range; APACHE II, Acute Physiology and Chronic Health Evaluation II; AUDIT, Alcohol Use Disorders Identification Test.
| Age (years, IQR) | 51 [36, 61] |
| Race/Ethnicity (%) | |
| Caucasian | 68 |
| Hispanic | 21 |
| African American | 11 |
| Gender (% male) | 74 |
| APACHE II score (median, IQR) | 9 [5, 13] |
| AUDIT Score (median, IQR) | 17 [10, 27] |
| Reason for admission (%) | |
| Alcohol withdrawal | 8 |
| Gastrointestinal bleeding | 5 |
| Severe sepsis | 2 |
| Other | 4 |
| Length of interview (minutes, IQR) | 24 [21, 32] |
Table 3.
Barriers and facilitators of change in medical intensive care unit survivors with an alcohol use disorder.
| Facilitators | Description | Example |
|---|---|---|
| Empathy of the inpatient healthcare environment | A feeling of understanding and lack of stigmatization from the entire healthcare team as well as family members | “They [nurses] just get it. They are more compassionate. They get it. They get it. They don't come off … Let's put it like this. They don't come off as condescending like the arrogant doctors do.” “And everybody is pulling for my recovery and I don’t feel embarrassed about myself in the least bit.” |
| Recognition of accumulating problems | Awareness of accumulating alcohol related health, legal, and financial consequences preceding admission to the ICU | “Your teeth are all messed up. Your health is lousy. You have trouble sleeping at night. You are always in pain for everything. So… It [alcohol] is not worth it.” “[Alcohol] destroyed my kidneys, my pancreas, my liver.” |
| Religion | Strength from faith in god or from the community provided by a church | “So my faith in my Lord and Savior Jesus Christ, I always rely on Him…And that has given me the help I've needed to now really start making progress.” “And I’m going to stay away from the old crowd I used to hang with. I’m trying to make religious friends.” |
| Pressure from others to stop drinking | An urging from family or friends to stop drinking. | “Cause my sister had been telling me all the time - all you're doing is drinking yourself to death.” “My girlfriend [yelling] at me to stop drinking.” |
| Trigger events | Significant, life changing event related to alcohol use that results in changes in alcohol consumption | “[I decided to stop drinking] when the doctor told me I was sick. Stage 4, which is the highest cirrhosis.” “Once you see blood gushing out of you and like excrement is all blood and you can't walk and you can't eat and you go like a week without eating… it kind of changes your mind about alcohol.” |
| Barriers | ||
| Missed opportunities | Failure to connect patients’ excessive alcohol consumption with reason for hospitalization/severe acute illness | “That's when I started drinking wine….it does control my red blood cells.” “It’s just casual drinking.” |
| Psychiatric comorbidity | Depression/anxiety frequently triggered patients to drink. However, some patients did not seek help for their psychiatric problems because of perceived stigmatization. | “…I used the drinking to medicate myself, I guess, from depression and that sort of thing. I never really sought psychiatric help and I probably should have. “ “That’s how I grieved… with the alcohol.” |
| Cognitive dysfunction | An impaired ability to think clearly. | “And alcohol frying your brain just a little bit more.” |
| Barrier or Facilitator | ||
| Social network | A decision to change was guided by the probability that the patient’s social network would be supportive of their decision | Facilitator: “Well, my boyfriend. He has really, really helped out because I told him, look, my drinking is not about you. If you want to have a beer…that's fine with me. I'm not telling you to stop. But he stopped drinking and it does help me.” Barrier: “One of my best friends…is a heavy drinker. We hung out for years and years and years. That didn't help.” Barrier: “If you hang with the wrong crowd, you end up getting to be like them.” |
Facilitators of Change
Empathy of the inpatient healthcare environment
Empathy refers the capacity to recognize feelings that are being experienced by another person and was sensed by medical ICU patients as an understanding of their AUD by others. In the context of the medical ICU, patients sensed a collective empathy, coming not only from nurses and physicians but also from members of their social network such as family and close friends who supported them during their illness. This empathy was important in facilitating a desire to change and sometimes led to an increased level of confidence that change could occur. On the contrary, when healthcare providers or family were confrontational regarding a patient’s drinking this led to anger and a lack of a desire to change. Overall, an empathic environment in the ICU facilitates a setting in which patients do not feel judged and, thus, feel free to discuss their drinking with others. This is an important aspect of forming a plan to change drinking behaviors following ICU discharge.
Recognition of accumulating problems or risks
Problems or risks associated with excess alcohol consumption are a hallmark of the diagnosis of alcohol abuse or dependence, as defined by the Diagnostic and Statistical Manual, fourth version (DSM-IV). Patients’ problems could be related to a failure to fulfill major role obligations (such as poor work performance or neglect of children), recurrent legal problems, recurrent social or interpersonal problems (such as arguments with a spouse related to alcohol), or medical problems (such as cirrhosis). Patients recognized these problems on their own but expressed an inability to cut down their drinking despite a desire to change. The inability to stop drinking despite consequences is a feature of an AUD. Therefore, recognition of alcohol-related problems may have facilitated a desire to change, but is not sufficient by itself to lead to change.
Pressure from others to change
Pressure to change was brought about prior to hospital admission by others for two main reasons. First, they witnessed the patients’ accumulating problems and risks and were concerned for the health and safety of the patient. Second, the patients’ alcohol-related problems and consequences may have directly affected those who were pressuring the patient to stop drinking. Preceding their illness, the patient may have ignored this pressure to change and tried to exclude those bringing pressure to change from their social network. Frequently, friends and family who exerted pressure to change did so in a confrontational manner thus resulting in a lack of desire to change.
Religion
Religion is important in providing patients with the strength to commit to abstinence or a reduction in alcohol consumption. Patients who had stopped drinking in the past referred to religion in the context of Alcoholics Anonymous. Others found the social network provided by formal religion in the context of a specific church provided a supportive environment for abstinence and change.
Trigger event
A trigger event refers to a significant event that precipitates change. These significant, life-changing events were almost necessary for change to occur. While this is often described as “hitting bottom” for patients with alcohol dependence, this did not necessarily have to be the case for ICU survivors. Frequently, the trigger event was the illness that resulted in admission to the medical ICU. Trigger events could be related to the development of a chronic health condition (such as the diagnosis of cirrhosis) or surviving an acute life-threatening illness such as sepsis. This could sometimes be more accurately described as a “near miss” as opposed to “hitting bottom.” Trigger events do not have to be health-related. They could be related to other consequences of drinking such as a motor vehicle accident, loss of one’s home, or having a child taken away. These may occur prior to hospital admission, prompt the patient to stop drinking and the patient is subsequently admitted to the ICU for treatment of severe alcohol withdrawal. ICU admission is then a time to “dry out” and solidify a plan for change.
Barriers to Change
Missed Opportunities
A missed opportunity is the failure to act in the setting of a favorable junction of circumstances. A missed opportunity could be simply be a failure to identify a patient’s ongoing alcohol consumption. Alternatively, the competing demands on the time of healthcare providers may mean that a discussion regarding plans for change never occurs with the patient. In spite of such discussions, there could also be a failure to connect a patient’s acute illness with their excess alcohol consumption. Without this connection, patients will not factor their acute illness into weighing the pros and cons of continued alcohol consumption and may then decide to continue drinking.
Psychiatric comorbidity
Psychiatric comorbidity is common in patients with an AUD and are associated with poor treatment-related outcomes [27]. Symptoms related to a psychiatric comorbidity such as an anxiety disorder or depression could lead to continued drinking. While the continued drinking may lead to temporary improvement in symptoms, it will ultimately lead to a spiraling effect where drinking leads to worsening psychologic symptoms and psychologic symptoms lead to more drinking. This spiraling may then continue because of the stigma associated with seeking mental health treatment.
Cognitive dysfunction
In patients with an AUD, cognitive dysfunction is well described and may lead to impairments in multiple cognitive domains including problem solving and executive functions. Therefore, cognitive dysfunction may lead to an inability to think about abstract ideas including weighing the pros and cons of continued alcohol consumption. Patients with cognitive dysfunction lacked insight into the problems related to their excess alcohol consumption and did not express a desire to change. Their answers to the interview questions lacked breadth and depth and interviews were typically short (less than 10 minutes).
Social Network
A social network is a network of friends, family, colleagues, and other personal contacts. Members of the patient’s social network encouraged alcohol consumption either through their own behaviors or through facilitating the alcohol-related behaviors of the patient. However, patients who wanted to change also had members of their social network that were abstinent from alcohol themselves, encouraged the patient to abstain from alcohol, and/or did not exhibit behaviors that enabled the patient to continue to drink excessively. Having a social network available that could reinforce abstinence is important for change. In the absence of a change in social network, patients could not commit to change with confidence.
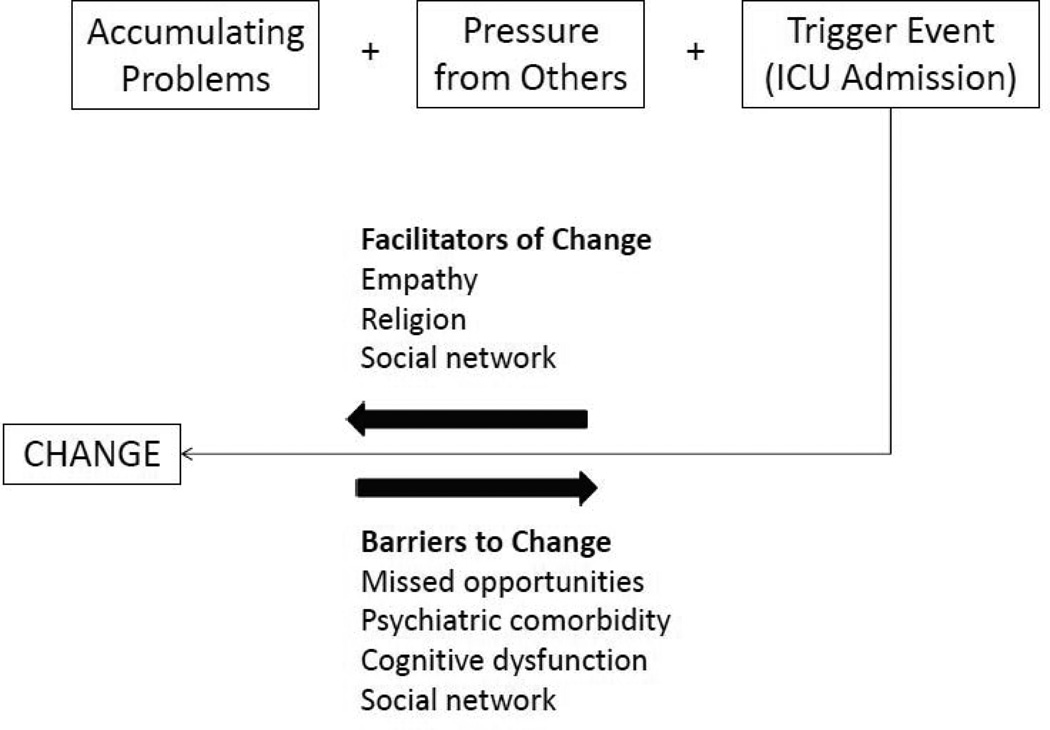
Summarizing Barriers and Facilitators to Change
Figure 1 summarizes how these themes are connected and ultimately result in a decision to change or not change drinking for medical ICU survivors with an AUD. We hypothesize that patients develop an illness necessitating admission to the medical ICU atop a background of accumulating problems related to their alcohol use and pressure from others to stop drinking. Their illness and ICU admission may then act as a trigger event causing them to consider changing their drinking behaviors. Once patients enter this contemplative stage, empathy from others in the inpatient healthcare environment, religion, and social networks that supported abstinence could serve to further facilitate change. On the contrary, missed opportunities, psychiatric comorbidity, cognitive dysfunction, and social networks that directly or indirectly encouraged continued alcohol consumption served as barriers to a decision to change.
Figure 1.
A proposed framework for change in medical intensive care unit survivors with an alcohol use disorder.
DISCUSSION
In the first qualitative study of medical ICU survivors with AUDs, we identified how this unique population of patients approaches a decision to change their drinking behaviors in the context of surviving a critical illness. We identified several patient and system barriers and facilitators to making a decision to change, thus providing a platform for the development of brief interventions in medical ICU survivors with AUDs. With over 3 million ICU survivors in the United States each year and the high prevalence of AUDs in patients admitted to the ICU, developing such a system has the potential to impact future drinking-related outcomes in a large population of patients. Furthermore, our prior work and the findings in this study support the notion that surviving a critical illness may be a “teachable moment” where patients are particularly motivated to change [11, 28]. Our findings are similar to the work by Orford and colleagues in treatment seeking clients with an AUD. This work identified a catalyst system in which “recognition of accumulating problems” and “trigger events” catalyze change that is then sustained with the help of social networks [29]. However, the other barriers and facilitators identified in our study may be unique to ICU patients.
There is substantial evidence for the use of motivational interviewing in a brief intervention [16, 30, 31]. In motivational interviewing, a member of the healthcare team spends 15–30 minutes with a patient discussing the pros and cons of continued alcohol consumption. The use of MI for brief intervention, therefore, could provide a system that addresses several key themes that we identified. MI would allow a healthcare provider to acknowledge accumulating risks and problems as well as pressure from others through incorporating these into a discussion of the pros and cons of continued drinking. Furthermore, an explicit discussion of the patient’s trigger event could be included in weighing the risks and benefits of continued drinking during MI. A key aspect of motivational interviewing is empathy and the lack of confrontation. However, our findings suggest that further efforts to ensure empathy in family and friends in addition to healthcare providers other than the interventionist may be necessary when brief interventions are applied in medical ICU survivors. Finally, incorporating members of the patients’ social network into a brief intervention may be helpful. For example, significant others have been successfully included in brief interventions conducted in the trauma setting demonstrating feasibility though the impact on drinking outcomes remains unclear [32].
The medical ICU is a chaotic environment with several competing demands for healthcare provider’s time. Therefore, it is not surprising that there were missed opportunities to address a patient’s alcohol use. When compared to standardized questionnaires, physicians only identify 52% of hospitalized patients with an AUD [33]. Our prior work extended this finding to the medical ICU setting where physicians fail to identify more than one quarter of patients with excessive alcohol use, even in hospitals with standardized alcohol screening in the emergency department [34]. Systematic ICU based alcohol screening could address this problem. However, future work will need to focus on how this approach can be implemented successfully in the ICU environment.
Finally, it will be important to account for other barriers to change when considering brief interventions for medical ICU survivors. Cognitive dysfunction is prevalent in ICU survivors and in patients with AUDs though its prevalence in ICU survivors with an AUD is unknown [35–37]. When present, cognitive dysfunction is associated with poor treatment outcomes in patients with AUDs [27]. Fortunately cognitive dysfunction can improve with weeks to months of abstinence from alcohol [38]. One possible approach to address cognitive dysfunction would be to alter the timing of an intervention by providing a “booster session” following hospital discharge. This approach has been successfully implemented in the emergency department setting and leads to reduced alcohol consumption when compared to a single intervention alone [39]. Psychiatric comorbidities such as anxiety and depression also serve as a barrier to change. We previously demonstrated that the presence of anxiety, depression, or schizophrenia is independently associated with the time to death or first rehospitalization in medical ICU survivors with alcohol withdrawal [10]. Psychiatric comorbidities are more common in ICU survivors with an AUD and are associated with poor treatment compliance and worse treatment related outcomes in patients with an AUD [40]. Therefore, an important and novel aspect of intervention for medical ICU survivors with AUDs may be bridging to concomitant treatment for psychiatric comorbidities and an AUD.
There are limitations to our study. First, we focused on how medical ICU survivors make a decision to change their drinking behaviors at a single point in time and did not conduct followup interviews after hospital discharge. A decision to change drinking behaviors is fluid and barriers and facilitators to change may fluctuate over time particularly when patients return to their home environment. Therefore, we can only generate themes that brought about a desire to change; identifying themes that actually bring about change will require following patients longitudinally. Importantly, drinking outcomes in medical ICU survivors have not been assessed though rates of abstinence in general medical inpatients approach 30% one year following hospital discharge [41]. Second, a key aspect of a brief intervention is referral to treatment for patients with an AUD. The barriers and facilitators to treatment attendance may be different from the barriers and facilitators to change. For example, a patient may have a desire to change but be unwilling to participate in a particular type of treatment. Alternatively, a patient may have a desire to change, be willing to participate in treatment, but be unable to do so because of financial or logistical reasons. Finally, patients who did not want to change their drinking behaviors may have declined to participate in this study. Therefore, we may have failed to identify key barriers to change.
CONCLUSION
In the first qualitative study in medical ICU survivors with AUDs, we identified key barriers and facilitators to changing drinking behaviors. Addressing these when developing a systematic approach to screening, brief intervention, and referral to treatment for AUDs will result in a system that is tailored to this unique population. Future studies should test the efficacy of a tailored system in this unstudied population.
ACKNOWLEDGEMENTS
This work was paid for by grant 2 K24 HL089223 06 (Marc Moss principal investigator). Dr. Clark would like to acknowledge the generous support of the NIH Loan Repayment Program through the National Institute on Alcohol Abuse and Alcoholism. Dr. Clark was supported by training grant T32 HL 007085 for portions of the study period.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
REFERENCES
- 1.Saitz R. Clinical practice. healthy alcohol use. N Engl J Med. 2005;352:596–607. doi: 10.1056/NEJMcp042262. [DOI] [PubMed] [Google Scholar]
- 2.Moss M, Parsons PE, Steinberg KP, Hudson LD, Guidot DM, Burnham EL, Eaton S, Cotsonis GA. Chronic alcohol abuse is associated with an increased incidence of acute respiratory distress syndrome and severity of multiple organ dysfunction in patients with septic shock. Crit Care Med. 2003;31:869–877. doi: 10.1097/01.CCM.0000055389.64497.11. [DOI] [PubMed] [Google Scholar]
- 3.O'Brien JM, Jr, Lu B, Ali NA, Martin GS, Aberegg SK, Marsh CB, Lemeshow S, Douglas IS. Alcohol dependence is independently associated with sepsis, septic shock, and hospital mortality among adult intensive care unit patients. Crit Care Med. 2007;35:345–350. doi: 10.1097/01.CCM.0000254340.91644.B2. [DOI] [PubMed] [Google Scholar]
- 4.de Wit M, Best AM, Gennings C, Burnham EL, Moss M. Alcohol use disorders increase the risk for mechanical ventilation in medical patients. Alcohol Clin Exp Res. 2007;31:1224–1230. doi: 10.1111/j.1530-0277.2007.00421.x. [DOI] [PubMed] [Google Scholar]
- 5.Saitz R, Ghali WA, Moskowitz MA. The impact of alcohol-related diagnoses on pneumonia outcomes. Arch Intern Med. 1997;157:1446–1452. [PubMed] [Google Scholar]
- 6.Gacouin A, Legay F, Camus C, Volatron AC, Barbarot N, Donnio PY, Thomas R, Le Tulzo Y. At-risk drinkers are at higher risk to acquire a bacterial infection during an intensive care unit stay than abstinent or moderate drinkers. Crit Care Med. 2008;36:1735–1741. doi: 10.1097/CCM.0b013e318174dd75. [DOI] [PubMed] [Google Scholar]
- 7.Marik P, Mohedin B. Alcohol-related admissions to an inner city hospital intensive care unit. Alcohol Alcohol. 1996;31:393–396. doi: 10.1093/oxfordjournals.alcalc.a008168. [DOI] [PubMed] [Google Scholar]
- 8.Mostafa SM, Murthy BV. Alcohol-associated admissions to an adult intensive care unit: an audit. European journal of anaesthesiology. 2002;19:193–196. doi: 10.1017/s0265021502000340. [DOI] [PubMed] [Google Scholar]
- 9.Kim MM, Barnato AE, Angus DC, Fleisher LA, Kahn JM. The effect of multidisciplinary care teams on intensive care unit mortality. Arch Intern Med. 2010;170:369–376. doi: 10.1001/archinternmed.2009.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clark BJ, Keniston A, Douglas IS, Beresford T, Macht M, Williams A, Jones J, Burnham EL, Moss M. Healthcare Utilization in Medical Intensive Care Unit Survivors with Alcohol Withdrawal. Alcoholism Clinical and Experimental Research. 2013 doi: 10.1111/acer.12124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clark BJ, Moss M. Secondary prevention in the intensive care unit: does intensive care unit admission represent a "teachable moment?". Crit Care Med. 2011;39:1500–1506. doi: 10.1097/CCM.0b013e31821858bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grossberg P, Halperin A, Mackenzie S, Gisslow M, Brown D, Fleming M. Inside the physician's black bag: critical ingredients of brief alcohol interventions. Subst Abus. 2010;31:240–250. doi: 10.1080/08897077.2010.514242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heather N. Developing, evaluating and implementing alcohol brief interventions in Europe. Drug Alcohol Rev. 2011;30:138–147. doi: 10.1111/j.1465-3362.2010.00267.x. [DOI] [PubMed] [Google Scholar]
- 14.Gentilello LM, Rivara FP, Donovan DM, Jurkovich GJ, Daranciang E, Dunn CW, Villaveces A, Copass M, Ries RR. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Ann Surg. 1999;230:473–480. doi: 10.1097/00000658-199910000-00003. discussion 480-473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Havard A, Shakeshaft A, Sanson-Fisher R. Systematic review and meta-analyses of strategies targeting alcohol problems in emergency departments: interventions reduce alcohol-related injuries. Addiction. 2008;103:368–376. doi: 10.1111/j.1360-0443.2007.02072.x. discussion 377-368. [DOI] [PubMed] [Google Scholar]
- 16.McQueen J, Howe TE, Allan L, Mains D, Hardy V. Brief interventions for heavy alcohol users admitted to general hospital wards. Cochrane Database Syst Rev. 2011:CD005191. doi: 10.1002/14651858.CD005191.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Field CA, Baird J, Saitz R, Caetano R, Monti PM. The mixed evidence for brief intervention in emergency departments, trauma care centers, and inpatient hospital settings: what should we do? Alcohol Clin Exp Res. 2010;34:2004–2010. doi: 10.1111/j.1530-0277.2010.01297.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Orford J. Asking the right questions in the right way: the need for a shift in research on psychological treatments for addiction. Addiction. 2008;103:875–885. doi: 10.1111/j.1360-0443.2007.02092.x. discussion 886–892. [DOI] [PubMed] [Google Scholar]
- 19.Kettles AM, Creswell JW, Zhang W. Mixed methods research in mental health nursing. Journal of psychiatric and mental health nursing. 2011;18:535–542. doi: 10.1111/j.1365-2850.2011.01701.x. [DOI] [PubMed] [Google Scholar]
- 20.Sandelowski M. What's in a name? Qualitative description revisited. Research in nursing & health. 2010;33:77–84. doi: 10.1002/nur.20362. [DOI] [PubMed] [Google Scholar]
- 21.Cutcliffe JR, McKenna HP. Expert qualitative researchers and the use of audit trails. Journal of advanced nursing. 2004;45:126–133. doi: 10.1046/j.1365-2648.2003.02874.x. discussion 134-125. [DOI] [PubMed] [Google Scholar]
- 22.Baker SE, Edwards R. Book How many qualitative interveiws is enough. City: National Centre for Research Methods; 2012. How many qualitative interveiws is enough. Editor (ed)^(eds) [Google Scholar]
- 23.Thomas DR. A General Inductive Approach for Analyzing Qualitative Evaluation Data. American Journal of Evaluation. 2006;27:237–246. [Google Scholar]
- 24.Saldana J. The coding manual for qualitative researchers. Thousand Oaks, CA: Sage Publications; 2012. [Google Scholar]
- 25.Guest G, MacQueen KM. Handbook for team-based qualitative research. Altamira, Lanham: 2008. [Google Scholar]
- 26.Curry LA, Nembhard IM, Bradley EH. Qualitative and mixed methods provide unique contributions to outcomes research. Circulation. 2009;119:1442–1452. doi: 10.1161/CIRCULATIONAHA.107.742775. [DOI] [PubMed] [Google Scholar]
- 27.Schuckit MA. Alcohol-use disorders. Lancet. 2009;373:492–501. doi: 10.1016/S0140-6736(09)60009-X. [DOI] [PubMed] [Google Scholar]
- 28.Clark BJ, Smart A, House R, Douglas I, Burnham EL, Moss M. Severity of acute illness is associated with baseline readiness to change in medical intensive care unit patients with unhealthy alcohol use. Alcohol Clin Exp Res. 2012;36:544–551. doi: 10.1111/j.1530-0277.2011.01648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Orford J, Hodgson R, Copello A, John B, Smith M, Black R, Fryer K, Handforth L, Alwyn T, Kerr C, Thistlethwaite G, Slegg G, Team UR. The clients' perspective on change during treatment for an alcohol problem: qualitative analysis of follow-up interviews in the UK Alcohol Treatment Trial. Addiction. 2006;101:60–68. doi: 10.1111/j.1360-0443.2005.01291.x. [DOI] [PubMed] [Google Scholar]
- 30.Mello MJ, Nirenberg TD, Longabaugh R, Woolard R, Minugh A, Becker B, Baird J, Stein L. Emergency department brief motivational interventions for alcohol with motor vehicle crash patients. Ann Emerg Med. 2005;45:620–625. doi: 10.1016/j.annemergmed.2005.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. 2005;165:986–995. doi: 10.1001/archinte.165.9.986. [DOI] [PubMed] [Google Scholar]
- 32.Magill M, Mastroleo NR, Apodaca TR, Barnett NP, Colby SM, Monti PM. Motivational interviewing with significant other participation: assessing therapeutic alliance and patient satisfaction and engagement. J Subst Abuse Treat. 2010;39:391–398. doi: 10.1016/j.jsat.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moore RD, Bone LR, Geller G, Mamon JA, Stokes EJ, Levine DM. Prevalence, detection, and treatment of alcoholism in hospitalized patients. JAMA. 1989;261:403–407. [PubMed] [Google Scholar]
- 34.Tomlinson AR, Moss M, Douglas IS, House R, Smart A, Macht M, Clark BJ. Physicians frequently fail to identify medical intensive care unit patients with unealthy alcohol use. Am J Respir Crit Care Med. 2012;185:A1643. [Google Scholar]
- 35.Girard TD, Jackson JC, Pandharipande PP, Pun BT, Thompson JL, Shintani AK, Gordon SM, Canonico AE, Dittus RS, Bernard GR, Ely EW. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med. 2010;38:1513–1520. doi: 10.1097/CCM.0b013e3181e47be1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE, Jr, Inouye SK, Bernard GR, Dittus RS. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753–1762. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 37.Stavro K, Pelletier J, Potvin S. Widespread and sustained cognitive deficits in alcoholism: a meta-analysis. Addiction biology. 2012 doi: 10.1111/j.1369-1600.2011.00418.x. [DOI] [PubMed] [Google Scholar]
- 38.Bartsch AJ, Homola G, Biller A, Smith SM, Weijers HG, Wiesbeck GA, Jenkinson M, De Stefano N, Solymosi L, Bendszus M. Manifestations of early brain recovery associated with abstinence from alcoholism. Brain : a journal of neurology. 2007;130:36–47. doi: 10.1093/brain/awl303. [DOI] [PubMed] [Google Scholar]
- 39.Longabaugh R, Woolard RE, Nirenberg TD, Minugh AP, Becker B, Clifford PR, Carty K, Licsw, Sparadeo F, Gogineni A. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. J Stud Alcohol. 2001;62:806–816. doi: 10.15288/jsa.2001.62.806. [DOI] [PubMed] [Google Scholar]
- 40.Hopkins RO, Key CW, Suchyta MR, Weaver LK, Orme JF., Jr Risk factors for depression and anxiety in survivors of acute respiratory distress syndrome. Gen Hosp Psychiatry. 2010;32:147–155. doi: 10.1016/j.genhosppsych.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 41.Saitz R, Palfai TP, Cheng DM, Horton NJ, Freedner N, Dukes K, Kraemer KL, Roberts MS, Guerriero RT, Samet JH. Brief intervention for medical inpatients with unhealthy alcohol use: a randomized, controlled trial. Ann Intern Med. 2007;146:167–176. doi: 10.7326/0003-4819-146-3-200702060-00005. [DOI] [PubMed] [Google Scholar]