Abstract
Objective
To assess the effect of positive enteric contrast administration on automatic exposure control (AEC) CT radiation exposure in 1) a CT phantom, and 2) a retrospective review of patients.
Materials and Methods
We scanned a CT phantom containing simulated bowel that was sequentially filled with water and positive enteric contrast, and recorded the mean volume CT dose index (CTDIvol). We also identified 17 patients who had undergone 2 technically comparable CT scans of the abdomen and pelvis, one with positive enteric contrast and the other with oral water. Paired student t-tests were used to compare the mean CTDIvol between scans performed with and without positive enteric contrast. Both the phantom and patient CT scans were performed using AEC with a fixed noise index.
Results
The mean CTDIvol for the phantom with simulated bowel containing water and positive enteric contrast were 8.2 ± 0.2 mGy, and 8.7 ± 0.1 mGy (6.1% higher than water, p=0.02), respectively. The mean CTDIvol for patients scanned with oral water and with positive enteric contrast were 11.8mGy and 13.1mGy, respectively (p=0.003). This corresponded to a mean CTDIvol which was 11.0% higher (range: 0.0–20.7% higher) in scans with positive enteric contrast than those with oral water in patients.
Conclusions
When automatic exposure control is utilized for abdominopelvic CT, the radiation exposure, as measured by CTDIvol, is higher for scans performed with positive enteric contrast than those with oral water.
Keywords: radiation exposure, CT, enteric contrast material, automatic exposure control
Introduction
Computed tomography (CT) use has increased dramatically over the last several decades. It is a major source of radiation exposure in the United States and many other industrialized countries. Approximately 75% of diagnostic radiation exposure in the United States has been attributed to CT1. While the clinical benefits of a medically indicated CT study far exceed the potential harmful effects of radiation exposure, greater efforts are clearly needed to minimize radiation exposure from CT.
Radiation dose reduction strategies for CT are broad and varied, and include improved CT hardware, improved image reconstruction technologies, and adjustments in CT protocols2–3. One widely utilized and successful strategy is the adoption of an automatic exposure control system with tube current modulation, which automatically adjusts slice-by-slice radiation exposure based on the thickness and radiodensity of the patient on the scout view(s). The use of automatic exposure control may reduce abdominopelvic CT patient dose by up to 38%4. However, when using such a system, patient preparation may be important for optimal radiation dose reduction. One such variable in patient preparation that may affect radiation exposure is the administration of positive enteric contrast prior to scanning. The positive enteric contrast will appear radiodense on the scout views of the CT scans. The purpose of our study was to assess the effect of positive enteric contrast material on automatic exposure control CT radiation exposure in 1) a CT phantom, and 2) a retrospective review of patients who have undergone a pair of technically comparable abdominopelvic CT scans performed with and without positive enteric contrast material.
Materials and Methods
CT Phantom
A water-filled elliptical abdominal CT phantom, measuring approximately 32 × 27 cm in cross section and 20 cm in length, was cast from the abdomen of a 70 kg male volunteer. The walls of the phantom were made of polyethylene which has a CT number approximating that of fat. This phantom was fixed to the CT table with tape. To simulate bowel, polyethylene corrugated tubing (Hudson RCI, Temecula, California) measuring 130 cm in length and volume of 400 mL was placed into the water-filled CT phantom. The corrugated tubing had rigid maximal and minimal diameters of 2.4 cm and 1.8 cm respectively, and was serially filled with water and positive enteric contrast material (2% diatrizoate meglumine; Hypaque, General Electric Healthcare, Princeton, NJ) for CT scanning.
CT Technique for Phantom Study
The CT phantom was scanned using a 64-detector-row scanner (Lightspeed VCT, General Electric, Milwaukee, WI) using automatic exposure control with tube current modulation (Auto mA, Smart mA, General Electric, Madison, WI). The minimum and maximum tube current was set at 150 and 800 mA respectively. The noise index was set at 32 Hounsfield Units (HU). The other scan parameters were: 120 kVp, 1.25 mm slice thickness, 340 mm field-of-view, 1.375 pitch, 0.5 second rotation time, and helical acquisition mode. The reconstruction kernel was standard. The filter used was large. These are the same parameters that we routinely use in clinical practice for patients being scanned on our 64-detector-row CT scanner. For each simulated bowel content (water or positive enteric contrast), the CT phantom was scanned 5 times using the same scanning parameters. The volume CT Dose Index (CTDIvol) was recorded for each scan.
Patients
This retrospective single-institution study was approved by our Institutional Review Board and compliant with the Health Insurance Portability and Accountability Act. The requirement for written informed consent was waived. An electronic patient information database search was performed to identify all patients over the age of 18 who had undergone 2 CT scans of the abdomen and pelvis, one performed with positive enteric contrast material and one performed with oral water, at our institution between 1/1/2008 to 3/31/2010. Prior to September 2005, our institutional protocol for all routine CT of the abdomen and pelvis included the administration of 800 ml of oral 2% diatrizoate meglumine for bowel opacification prior to CT scanning. Since September 2005, the protocol has been changed to oral administration of 800 ml of water. The protocol change was based on several studies that showed similar diagnostic performance between CT scans performed with and without positive enteric contrast material in various clinical scenarios5–9. Currently at our institution, positive enteric contrast material, such as oral diatrizoate meglumine, is only administered in select cases of suspected bowel perforation or enteric fistula, select cases where intravenous contrast material is not administered, and when it is specifically requested by the ordering physicians.
To assess the effect of positive enteric contrast material on CT radiation exposure, we sought to minimize other factors that might contribute towards any potential differences in radiation exposure between the pair of two CT scans. Therefore we eliminated any pairs of scans that were acquired on different CT scanners or with different scanning parameters (i.e. with different kVp or slice thickness). We also eliminated pairs of scans if one was performed with intravenous contrast material while the other one was performed without intravenous contrast material. We further eliminated any pairs of scans that had variable presence of metallic or other radiodense foreign objects, including external electrocardiogram (EKG) leads, enteric tubes, or drainage tubes. This is because the variable presence of these radiodense objects may lead to differences in tube current modulation with automatic exposure control10.
A total of 17 patients (17 pairs of CT scans) that fulfilled the search criteria were identified. These included 9 men and 8 women (mean age 54 years old, range 22 to 82 years old). The mean duration between the first and second CT scans was 50 days (range: 0 to 144 days). Of the 17 patients, 15 patients received intravenous contrast material administration for both CT scans. The intravenous contrast material administered was 150-mL bolus of iohexol (Omnipaque 350, Nycomed-Amersham, Princeton, NJ). Two of the 17 patients did not receive intravenous contrast material administration for either of the 2 CT scans.
CT Techniques for Patient Scans
The patients were scanned using a 64-slice (n = 5), 16-slice (n = 5) or 4-slice (n = 7) multi-detector row CT scanners (Lightspeed, General Electric, Milwaukee, WI). The images were acquired from the lung bases to the pubic symphysis. The paired CT exams for each patient were performed on the same scanner with the same parameters (slice thickness, kVp, pitch, table speed), and with the same protocol except for the differences in the administration of enteric contrast material. All scans were acquired using automatic exposure control with tube current modulation (Auto mA, Smart mA, General Electric Healthcare, Milwaukee, WI). The minimum and maximum tube current was set at 150 and 400 mA respectively for the 4-slice and 16-slice scanners, and at 150 and 800 mA respectively for the 64-slice scanners. The noise index was set at 12 HU for image acquisitions of 5 mm slice thickness, and 32 HU for image acquisitions of 1.25 mm slice thickness. For all scans, the tube voltage was set at 120 kVp. At our institution, the CT dose report is electronically captured for all CT exams.
Data Analysis
One reader recorded the mean volume CT dose index (CTDIvol) for each scan. The CTDIvol is an expression of radiation dose in CT dosimetry. It averages radiation dose over the x, y, and z directions, and is a dose measure of a single volume within a slice. For the CT phantom study, one radiologist recorded the CTDIvol of the phantom when the simulated bowel contained water or positive enteric contrast material. For the retrospective patient study, one radiologist recorded the CTDIvol for each CT scan. The same radiologist also reviewed all the CT scans to confirm the following: 1) each patient had a pair of 2 scans, one performed with enteric contrast material and one without; 2) there was no variable presence of metallic or other radio-opaque objects (such as overlying EKG leads) between the 2 CT scan for each patient; 3) the CT scanner and scanning parameters (such as kVp and slice thickness) were the same between the 2 CT scans for each patient. The clinical imaging findings for all the CT scans were also recorded. Additionally, the transverse and anterior-posterior dimensions of the abdomen at the level of the superior border of L4 vertebral body was measured on the axial CT images of the paired CT scans for each patient. The transverse and anterior-posterior dimensions of the abdomen were used as an approximate measure of patient body size.
Statistical Analysis
Statistical analysis was performed using a commercial statistical software package Stata (Version 8.0, Stata Corp, College Station, TX). For the phantom study, paired student t-tests were used to compare the mean CTDIvol between scans performed with simulated bowel containing water versus positive enteric contrast material. For the patient study, paired student t-tests were used to compare the mean CTDIvol between CT scans performed with positive enteric contrast material and with oral water. Paired student t-tests were also used to compare the transverse and anterior-posterior dimensions of the abdomen at the level of L4 vertebral body between the paired CT scans. P values < 0.05 were considered significant.
Results
CT phantom
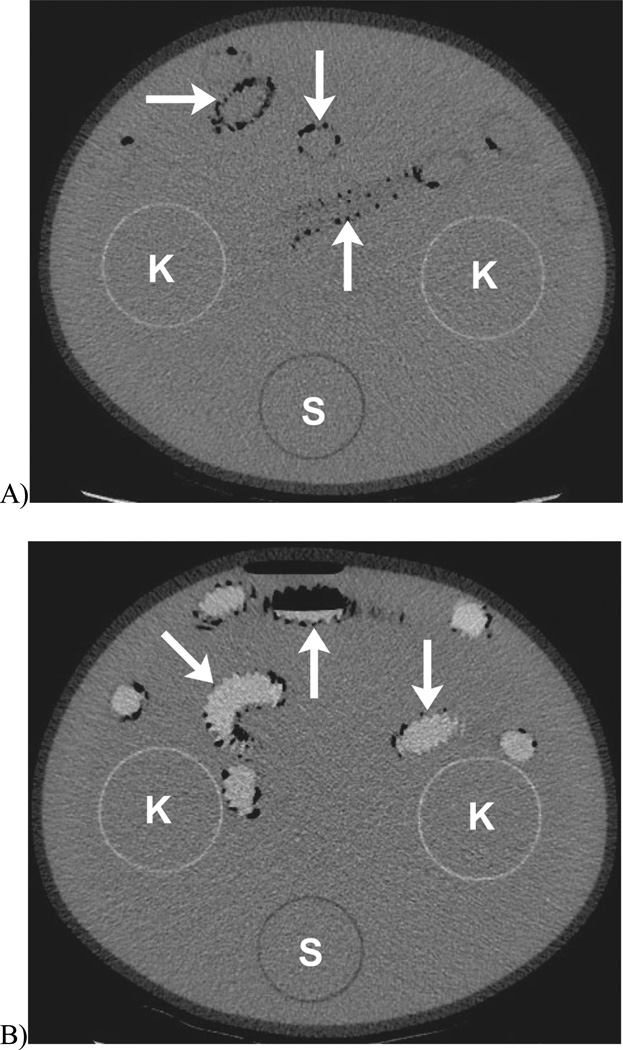
Figure 1 shows representative images from the CT phantom scans. The CTDIvol was 8.2 ± 0.2 mGy and 8.7 ± 0.1 mGy when the simulated bowel was filled with 400 mL water and positive enteric contrast material, respectively. Compared to the water-filled bowel, the enteric contrast-filled bowel resulted in a mean increase in CTDIvol by 6.1% (p = 0.02).
Fig. 1.
CT scan of a phantom shows simulated bowel (arrows) filled with (A) water, or (B) positive enteric contrast material. K: renal compartment, S: spine compartment. Both the renal and spine compartments were filled with water in this study.
Patients
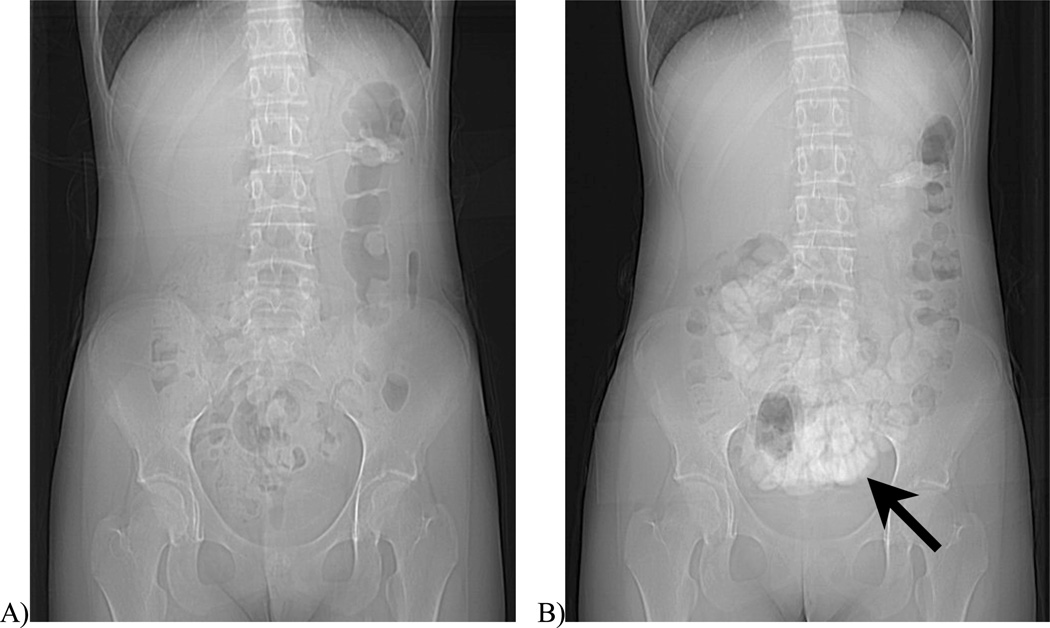
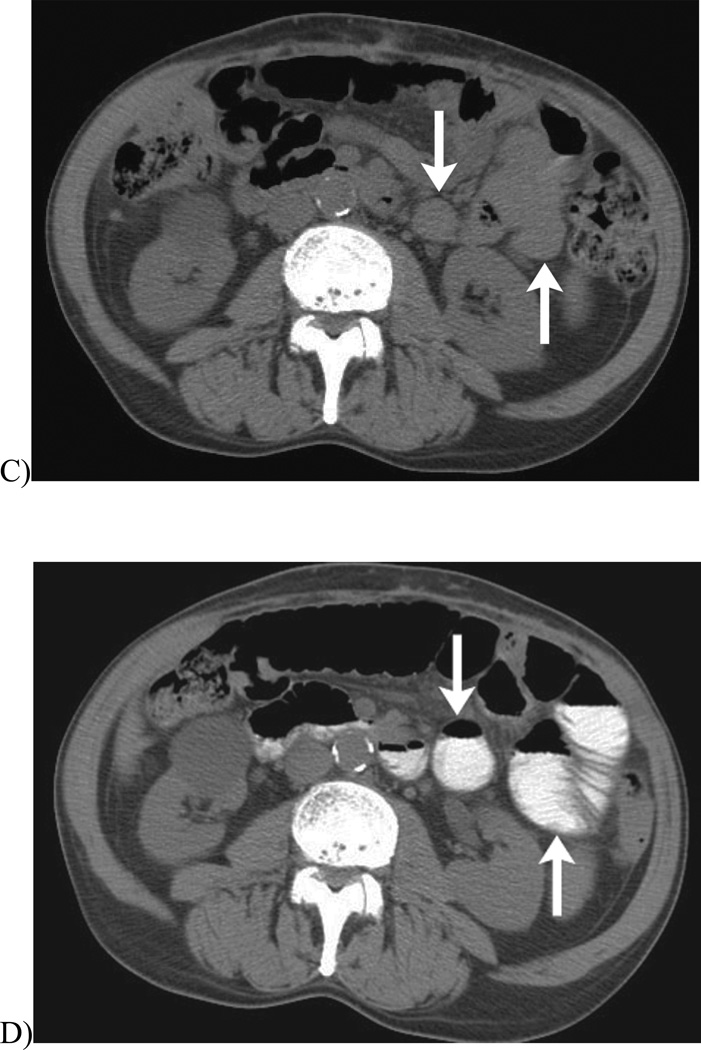
Review of the CT scans in the 17 patients showed the following CT findings: small bowel obstruction (n = 3), colon perforation with small amount of free intra-peritoneal air (n = 1), colitis (n = 2), post operative fluid collections (n = 4), and metastatic cancer (n = 2). The above findings were persistent on all of the pairs of CT scans except for one patient where the small bowel obstruction resolved on the follow up CT study performed with positive enteric contrast material. The remaining 5 patients did not show identifiable pathology at either scan. The mean transverse and anterior-posterior dimensions of the abdomen at the level of L4 vertebral body did not change significantly between the pair of CT scans (transverse dimension: 32.7± 5.1 cm versus 33.0± 5.0 cm; anterior-posterior dimension: 25.2 ± 4.5 cm versus 25.0 ± 4.6 cm; both p values > 0.35). The mean changes in the transverse and anterior-posterior dimensions of the abdomen between the pairs of scans were 0.3 ± 0.1 cm and 0.2 ± 0.1 cm, respectively. Figure 2 shows an example of a pair of CT scans in one patient, one scan performed with positive enteric contrast material, the other performed with oral water.
Fig. 2.
CT scans of a 19 year-old-woman with abdominal pain after bone marrow transplantation. The first CT scan of the abdomen and pelvis was performed with oral water, and the bowel segments (arrows) in the scout (A) and transverse CT image (C) do not show the presence of positive enteric contrast material. The CTDIvol was 9.0mGy. The second CT scan of the abdomen and pelvis was performed seven days later with positive enteric contrast material, which can be seen in the bowel segments (arrows) in the scout (B) and transverse CT image (D). The CTDIvol was 10.5mGy (16.7% higher than the first exam). No cause for abdominal pain was identified on either scan.
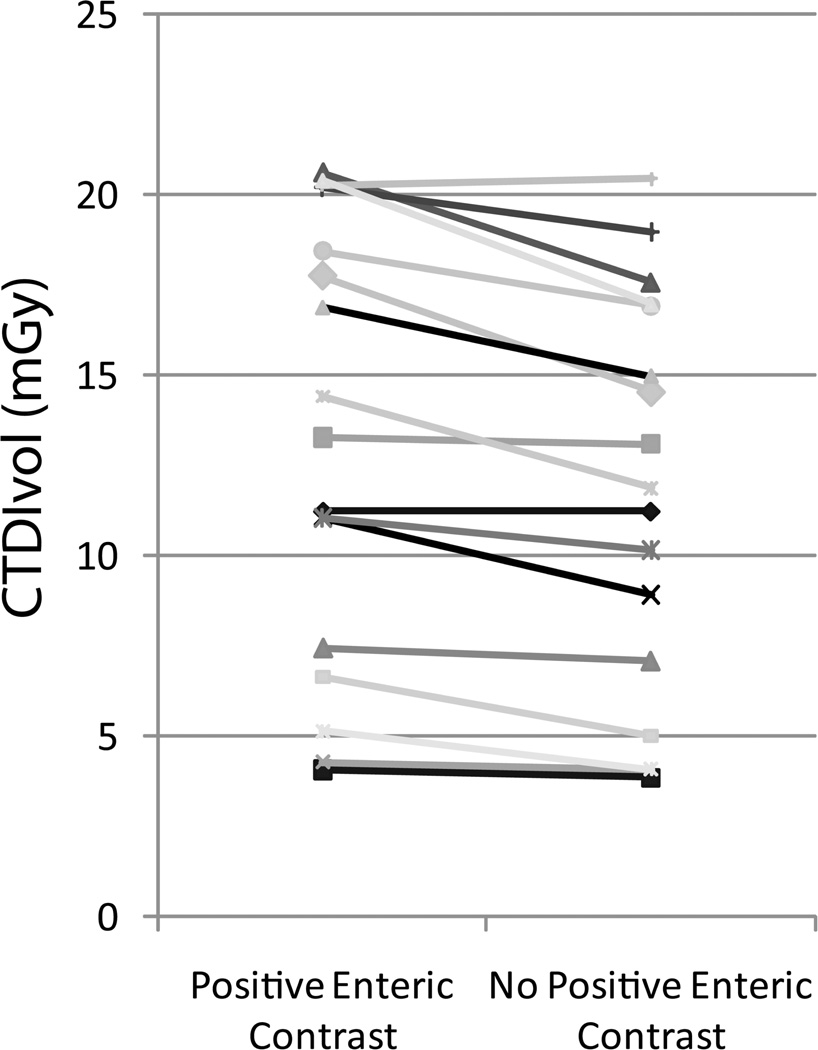
The mean CTDIvol was significantly higher for scans performed with positive enteric contrast material than scans performed with oral water (13.1 ± 6.1 mGy versus 11.8 ± 5.5 mGy, p = 0.003) (Fig.3). This corresponds to a mean CTDIvol increase of 11.0% (range: 0.0 – 20.7%) in scans with positive enteric contrast material than those with oral water.
Fig. 3.
Graph of CTDIvol for pairs of scans performed with positive enteric contrast material and with oral water. The mean CTDIvol was significantly higher for scans performed with enteric contrast material than scans performed with oral water (13.1 ± 6.1 mGy versus 11.8 ± 5.5 mGy, p = 0.003).
Discussion
We found higher radiation exposures, as measured by CTDIvol, in CT scans performed with positive enteric contrast material than those with oral water, both in a CT phantom and in patients. The higher radiation exposure in scans with enteric contrast material can likely be explained by the use of automatic exposure control in our CT studies.
Automatic exposure control is one of the most important and widely implemented technologies used to reduce radiation exposure in CT. It automatically modulates the tube current to accommodate differences in attenuation due to different anatomic regions and patient size in order to produce consistent image quality at the lowest achievable dose. For example, the tube current is modulated to higher levels when scanning through dense osseous structures such as pelvic bones than soft tissue structures, or when scanning large-size than small-size patients. A common way to implement automatic exposure control is to adjust the tube current based on X-ray attenuation and patient thickness as determined on the scout image(s) in order to maintain a user-selected noise level on the CT image (i.e. Auto mA / Smart mA on the General Electric CT equipment). Because positive enteric contrast material will appear radio-dense on the scout image, the tube current will automatically be adjusted to higher levels in the sections containing the contrast-opacified bowel in order to maintain the desired noise index. This results in higher radiation exposure as measured by higher CTDIvol. Interestingly, a recent study on CT colonography performed with automatic exposure control reported that the estimated x-ray attenuation of the tagged stool and fluid in the colon did not significantly affect the mean CTDIvol11. The authors, therefore, concluded that stool and fluid tagging with barium or iodine does not significantly affect radiation exposure11. However, the mean CTDIvol would likely be dependent on both the x-ray attenuation and the volume of tagged stool and fluid in the colon. It is possible that the effect of the high x-ray attenuation tagged stool and fluid on the mean CTDIvol of the scan is obscured if the volume of such stool and fluid is small.
We found higher average percentage increase in CTDIvol with positive enteric contrast in patients compared to phantom. This may in part be explained by the high volume of positive enteric contrast material in the patients’ bowel (patients were asked to ingest 800 mL of positive enteric contrast) than in the simulated bowel in phantom (filled with 400mL of positive enteric contrast). We also found a fairly wide range of percentage increase in CTDIvol when positive enteric contrast material was administered to the patients. This may be explained by the variable amount of positive enteric contrast material that was present in the bowel at the time of the CT scan. While each patient was instructed to ingest 800mL of positive enteric contrast prior to CT scan, the amount of enteric contrast material within the bowel is dependent on the actual amount ingested by the patients and the time delay from ingestion to CT scanning.
Our findings highlight the importance of careful attention to CT protocols in combination with scanner settings for minimizing radiation exposure to patients. The administration of positive enteric contrast material is a routine part of the protocol for abdominal pelvic CT at many radiology practices. However, very little attention has been paid to the effect of such contrast material on radiation exposure when patients are scanned with commonly used CT settings such as automatic exposure control. Our study showed an adverse effect of positive enteric contrast media on patient radiation exposure when combined with automatic exposure control. Our findings raise the question whether positive enteric contrast media should be administered routinely for abdominal and pelvic CT.
The use of positive enteric contrast media at CT was previously thought to be necessary for the optimal delineation of bowel pathology and for the differentiation between contrast-opacified bowel and extraluminal fluid collections. However, several recent studies on newer generation multi-detector row CT scanners have shown similar diagnostic performance between CT scans performed with and without positive enteric contrast media in various clinical scenarios5–9. Additionally, it has been shown that intravenous contrast enhancement of the bowel wall was better evaluated in the absence of positive enteric contrast media in the bowel lumen and such enhancement may be critical to accurate diagnosis of bowel pathology12–13. The administration of positive enteric contrast media is also associated with other problems such as poor patient tolerance, cost, delay in scanning, and rare side effects14. While positive enteric contrast material may be necessary in select cases, its routine use may be unwarranted. The potential harmful effect of positive enteric contrast material with respect to increase radiation exposure may become another reason why such contrast material should not be routinely administered to patients prior to their CT studies.
Our study has several limitations. First, while we attempted to control for the major scanner variables that may affect radiation exposure in our patient study, it is possible that there were other factors that differ between the pair of two CT scans that may have altered the measured CTDIvol. These include changes in patient body size or fluid volume in the bowel as in bowel obstruction, and the amount of lung tissue included on the abdomino-pelvic CT scans. We found no significant changes in the transverse and anterior-posterior dimensions of the abdomen at the level of L4 vertebral body, which were used as an approximate measure of body size, between the pair of CT scans. The presence of bowel obstruction with large amount of fluid in the bowel will likely increase the CTDIvol on scans performed using automatic exposure control. In our series, there were only 3 patients with bowel obstruction. Two of the 3 patients had bowel obstruction persisting on both CT scans; the third patients had small bowel obstruction resolved on the follow up CT study performed with positive enteric contrast material. In this third patient, the presence of bowel obstruction on the first CT scan performed without positive enteric contrast may have caused an underestimation of the CTDIvol increase from positive enteric contrast on the follow up CT scan. It is also difficult to quantify the exact amount of positive enteric contrast present in the bowel at the time of the CT scans in patients as stated previously. Overall, however, we do not believe these factors will significantly affect our results. Additionally, it is possible that there was a small difference in the amount of lung tissues imaged on the paired abdomino-pelvic CT scans. This may have potentially attributed to the difference in the CTDIvol, because the lung tissues are much less radio-dense that the abdominal organs. The aforementioned factors are limitations of retrospective patient studies. However, the results from our patient study are congruent with those from the phantom study. In combination, the patient and phantom studies provide strong evidence that positive enteric contrast material increases radiation exposure when automatic exposure control is utilized. Second, we only evaluated the effect of positive enteric contrast on CT radiation exposure as measured by CTDIvol; we did not assess the absorbed patient radiation dose because the measurement of the absorbed dose is not possible in a retrospective patient study. However, the dose-length product, which is proportional to CTDIvol (DLP = CTDIvol × scan length), is an indicator of the radiation dose of an entire CT exam. Third, our scans were performed using a commonly used automatic exposure control strategy where tube current is modulated based on a prescribed image noise index (Auto mA, Smart mA, General Electric). Future studies evaluating the effect of positive enteric contrast on CT radiation exposure using other automatic exposure control strategies by other vendors are warranted. Fourth, the sample size for our patient study was small. This is partly a reflection of the small number of CT studies performed with positive enteric contrast media at our institution.
Conclusions
Notwithstanding these limitations, we found that when automatic exposure control is utilized for abdominopelvic CT, the radiation exposure, as measured by CTDIvol, is higher for scans performed with positive enteric contrast than those with oral water, both in a CT phantom and in patients. The effect on radiation exposure should be considered in the decision to give positive enteric contrast for CT studies.
References
- 1.Wiest PW, Locken JA, Heintz PH, Mettler FA., Jr CT scanning: a major source of radiation exposure. Semin Ultrasound CT MR. 2002;23:402–410. doi: 10.1016/s0887-2171(02)90011-9. [DOI] [PubMed] [Google Scholar]
- 2.Silva AC, Lawder HJ, Hara A, Kujak J, Pavlicek W. Innovations in CT dose reduction strategy: application of the adaptive statistical iterative reconstruction algorithm. AJR Am J Roentgenol. 2010;194:191–199. doi: 10.2214/AJR.09.2953. [DOI] [PubMed] [Google Scholar]
- 3.Coakley FV, Yeh BM, Gould R, Arenson RL. CT radiation dose: What can you do right now in your practice? AJR Am J Roentgenol. doi: 10.2214/AJR.10.5043. (in press). [DOI] [PubMed] [Google Scholar]
- 4.Mulkens TH, et al. Use of an automatic exposure control mechanism for dose optimization in multi-detector row CT examinations: clinical evaluation. Radiology. 2005;237:213–223. doi: 10.1148/radiol.2363041220. [DOI] [PubMed] [Google Scholar]
- 5.Stuhlfaut JW, et al. Blunt abdominal trauma: performance of CT without oral contrast material. Radiology. 2004;233:689–694. doi: 10.1148/radiol.2333031972. [DOI] [PubMed] [Google Scholar]
- 6.Halsted MJ, et al. Oral contrast agents for CT of abdominal trauma in pediatric patients: a comparison of dilute hypaque and water. AJR Am J Roentgenol. 2004;182:1555–1559. doi: 10.2214/ajr.182.6.1821555. [DOI] [PubMed] [Google Scholar]
- 7.Anderson BA, Salem L, Flum DR. A systematic review of whether oral contrast is necessary for the computed tomography diagnosis of appendicitis in adults. Am J Surg. 2005;190:474–478. doi: 10.1016/j.amjsurg.2005.03.037. [DOI] [PubMed] [Google Scholar]
- 8.Horton KM, Fishman EK. Multidetector-row computed tomography and 3-dimensional computed tomography imaging of small bowel neoplasms: current concept in diagnosis. J Comput Assist Tomogr. 2004;28:106–116. doi: 10.1097/00004728-200401000-00019. [DOI] [PubMed] [Google Scholar]
- 9.Miller FH, Hwang CM. An initial experience: using helical CT imaging to detect obscure gastrointestinal bleeding. Clin Imaging. 2004;28:245–251. doi: 10.1016/S0899-7071(03)00193-1. [DOI] [PubMed] [Google Scholar]
- 10.Rizzo SM, et al. Do metallic endoprostheses increase radiation dose associated with automatic tube-current modulation in abdominal-pelvic MDCT? A phantom and patient study. AJR Am J Roentgenol. 2005;184:491–496. doi: 10.2214/ajr.184.2.01840491. [DOI] [PubMed] [Google Scholar]
- 11.Lim HK, et al. Does the amount of tagged stool and fluid significantly affect the radiation exposure in low-dose CT colonography performed with an automatic exposure control? Eur Radiol. 2010 doi: 10.1007/s00330-010-1922-4. [DOI] [PubMed] [Google Scholar]
- 12.Scholten ET, Ziedses des Plantes BG, Falke TH. Computed tomography of the large bowel wall. Choice of slice thickness and intraluminal contrast medium. Invest Radiol. 1995;30:275–284. doi: 10.1097/00004424-199505000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Jancelewicz T, et al. Predicting strangulated small bowel obstruction: an old problem revisited. J Gastrointest Surg. 2009;13:93–99. doi: 10.1007/s11605-008-0610-z. [DOI] [PubMed] [Google Scholar]
- 14.Seymour CW, Pryor JP, Gupta R, Schwab CW. Anaphylactoid reaction to oral contrast for computed tomography. J Trauma. 2004;57:1105–1107. doi: 10.1097/01.ta.0000133578.57031.97. [DOI] [PubMed] [Google Scholar]