Abstract
Heterosexual HIV transmission remains the leading cause of HIV incidence in adult men and women in sub-Saharan Africa. This study assessed whether an HIV risk-reduction intervention would be more likely to increase sexual barrier acceptability and decrease risk behavior when delivered to couples in gender concordant groups or in an individual format. This study also examined the mutual impact of couple members as a source of influence on acceptability, and assessed whether product acceptability, intimate partner violence (IPV), and/or partner communication predicted sexual barrier use. HIV seroconcordant and serodiscordant couples (n=216) were recruited in Lusaka, Zambia, and randomized to a four session gender-concordant intervention. Participants were assessed at baseline, 6, and 12 months. Willingness to use barriers (p=0.012), acceptability (p<0.001), and barrier use (p<0.001) increased over time in both conditions, and were influenced by gender preferences. IPV decreased (p=0.040) and positive communication increased (p<0.001) in both conditions. Individual and gender concordant group sessions achieved similar increases in sexual barrier use following the intervention. Results highlight the influence of partners as well as product acceptability as predictors of sexual barrier use among couples in sub-Saharan Africa. Future prevention studies should consider both product acceptability and partner influence to achieve optimal sexual risk behavior outcomes.
Introduction
While sub-Saharan Africa accounts for only 10% of the world's population, it bears the majority of new HIV infections, an estimated 1.8 million new cases in 2009. The region accounts for about 68% of the total of those living with HIV, among whom women represent over 50%. Despite educational and behavioral interventions and HIV testing programs, heterosexual HIV transmission is still the leading cause of HIV acquisition in adult men and women in sub-Saharan Africa and the number of serodiscordant couples and infections acquired through heterosexual contact has continued to increase.1 The sub-Saharan nation of Zambia has a population of over 12 million people and had an estimated 980,000 people living with HIV in 2009. In 2009, HIV transmission within the context of mutually monogamous relationships represented 21% of new infections, with rates as high as 60% in urban areas, while condom use was reported by less than half of individuals during their last sex act.1
Many prevention programs designed to limit heterosexual transmission of HIV have been conducted with individuals,2 but recent studies strongly recommend the inclusion of both partners3 as a means of increasing acceptability and use of sexual barrier products (e.g., male and female condoms). Enrolling couple members in sexually-focused interventions including motivational and educational programs has been promoted as more effective than those addressing only individuals,4,5 though most prevention studies have not been analyzed at the dyadic level.6 Instead, these studies have typically conducted analyses on individual genders or ignored the nonindependence between couple members, thereby incorrectly inflating the sample size and violating the assumption of independence. In contrast, dyadic models of health behavior represent both a methodological and statistical framework for assessing the response of the couple to health-based interventions, as well as the interactive influence of the response of dyad members on each other (e.g., effects of “actor” and “partner”7).
Behavioral change in established relationships does not come easily, and requires both partners to make significant changes in firmly entrenched sexual practices. Negotiation regarding safer sex practices may also be hampered by cultural norms for fidelity and the potential for intimate partner violence (IPV).8–10 As power dynamics within relationships influence HIV risk behavior, the member of the couple with the greatest power may more directly influence dyadic decision-making and thereby encourage either safe or risky behaviors.11
Building on previous women-focused research in the US12 and Zambia,13 an evidence-based HIV prevention model for couples was developed and pilot tested in the Zambian context.14 The subsequent study was designed to reduce sexual risk behavior among urban, Zambian HIV-seroconcordant positive and -serodiscordant couples and compared ‘intervention modalities’ to assess whether the HIV risk-reduction intervention would be more likely to increase condom acceptability and decrease risk behavior when delivered to couples in a gender-concordant group or individual format. This study examined the impact of couple members' attitudes and preferences about sexual barriers on each other's level of product acceptability, and assessed the influence of such acceptability on condom use. It was theorized that participants with more positive attitudes would report higher acceptability, and that higher levels of acceptability would predict increased sexual barrier use. In addition, it was theorized that intimate partner violence and sexual communication would also impact sexual barrier acceptability and use.
Methods
Prior to participant recruitment, Research Ethics Committee and Institutional Review Board approval was obtained in accordance with the provisions of the University of Zambia and the University of Miami Miller School of Medicine regarding the conduct of research. Human subjects protections included a referral plan for those reporting domestic or intimate partner violence (IPV). Study candidates currently in heterosexual couple relationships residing in the Lusaka, Zambia urban district were recruited by study staff from clinics in the University Teaching Hospital, local community health centers, and nongovernmental organizations between May 2006 and December 2008. Couples provided verification of seropositive status of one or both members of the couple, and seronegative participants completed voluntary counseling and testing for HIV prior to enrollment. Couples were screened for eligibility by study assessors (i.e., 18 years or older, one member HIV seropositive). Couples status was verified at the study offices to ensure male and female dyads were primary sexual partners. Verification required that couples be interviewed separately and asked to respond to a rotating series of six parallel questions of an intimate and personal nature drawn from a pool of 21 questions; responses were compared for consistency between partners. The majority of candidates (84%) were deemed eligible for study participation.
Participants provided written informed consent at the time of enrollment, were tested for other sexually transmitted infections (STDs: syphilis, chlamydia, gonorrhea15), completed a baseline assessment, and were then randomized to either the group or individual condition in a 1:1 ratio. Randomization was accomplished using a generated table of random numbers; randomization was carried out by the principal investigator, and individuals were assigned to intervention condition by the study coordinator. Assessments were conducted at baseline, 6, and 12 months post-baseline (approximately 4 and 10 months post-intervention); all assessments were conducted using an audio computer-assisted self-interview (ACASI) in English, Nyanja, or Bemba (primary local languages) in a private carrel in the study offices, monitored by study staff available to respond to queries. Study assessors were blind to condition assignment. All data were collected at study offices located at the University Teaching Hospital in urban Lusaka, Zambia. Study IDs were coded to ensure participant confidentiality, and participants received monetary compensation for their time and travel expenses (K50,000 Zambian Kwacha per assessment,=US $10, K25,000 Zambian Kwacha per session,=US $5). In the event of loss of one member of a couple (e.g., illness, death, estrangement), the remaining partner was encouraged to continue to participate but were not permitted to participate with a new partner. The primary causes for partner or couple attrition were employment, separation of the couple, leaving the area, and illness. Sample size was determined from earlier studies conducted by this team, assuming a retention rate of 85%. Additionally, interim analyses were conducted to ensure that intimate partner violence was not exacerbated by study participation. Due to ethical concerns associated with HIV transmission, no control group was included as previous research13 found “usual care” participants to decrease sexual barrier use over the course of the study. Follow-up assessments were completed in February 2010.
Measures
Demographics
Data collected included age, marital status, education, and employment. Date of HIV diagnosis and income were also recorded.
Sexual Activities Questionnaire (SAQ)
This scale was adapted from the Sexual Risk Behavior Assessment Schedule.16 Self-reported sexual behavior was assessed over the last month and included frequency of sexual intercourse with primary and nonprimary partners, and frequency of sexual barrier use [scored using a Likert scale of 0 (never), 1 (once), 2 (sometimes), 3 (half of the time), 4 (most of the time), 5 (all of the time)].
Sexual diary
The incidence of sexual intercourse over the last 7 days and type of sexual barrier method used, if any, was assessed using this pictorial diary. The scale was used to calculate the rate of condom use as a percentage of total occurrences of sexual intercourse with primary and nonprimary partners.
Condom use
The Risk Reduction Strategies scale was used to assess participants' assessment of their typical, or “general,” condom use. Participants are asked how often they used a condom during sex in general, using a 5-point rating scale (5=Every time, 4=Almost every time, 3=Sometimes, 2=Almost never, and 1=Never).
Barrier Questionnaire
This measure was adapted from the University of California at San Francisco Center for AIDS Prevention Studies Barrier Questionnaire, and acceptability of sexual barriers using a Likert-type scale based on specific characteristics (current and previous use: never used=0, like very much=5, like somewhat=4, neutral=3, dislike somewhat=2, strongly dislike=1; from which an aggregated variable was created using the total mean scores for “liking” male condoms, female condoms, gels, and creams). Willingness to use products following previous or current use was scored as not at all willing to use=1, slightly willing=2, moderately willing=3, very willing=4, and an aggregated variable was created for prevention of HIV/STDs, pregnancy, and HIV/STDs plus pregnancy (Cronbach's alpha=0.64). Stem prompts were adapted to state willingness “to use” products. Subscale scores on barrier acceptability were compiled for (1) acceptability of products (2) willingness to use products type following trial use and (3) type of protection provided by product.
Conflict Tactics Scale
This 18-item scale17 was modified to assess current conflict resolution strategies across four domains: positive, negative, violent, and extremely violent, from which violence and extreme violence were classified as IPV. Scores presented indicate the total Likert scale scores of the combined items in four subscales, (a) positive communication, (e.g., discussion of information; subscale alpha in this sample=0.70); (b) negative communication (e.g., swearing or sulking; alpha=0.81); (c) violence (e.g., threatening to hit to hitting; alpha=0.91), and (d) extreme violence (punching to assault with a deadly weapon; alpha=0.76). Participants reported previous experiences with relationship violence and reported their partners' frequency of violence in the last month (scored using a Likert scale of 0 (never), 1 (once), 2 (twice), 3 (3–5 times), 4 (6–10 times), 5 (11–20 times), 6 (more than 20 times), and the type. Subscale scores used in analyses were grand mean centered.
Procedures
Both the group and individual intervention conditions consisted of four structured 2-h sessions delivered weekly by a single female or male facilitator, matched to the gender of the participants, who had been trained by a clinical psychologist in the delivery of the intervention and had at least a nursing degree or HIV counselor training. The intervention was designed with feedback from focus groups and pilot studies in Zambia and adapted to be responsive to the needs of both men and women.14 Though HIV serodiscordant and concordant couples differ with regard to the risk of primary HIV infection, and the focus of risk for HIV+seroconcordant couples may be potential transmission of ART-resistant strains and STIs, the intervention was developed and pilot tested with both groups in mind. For example, the intervention addresses issues of the need for barrier protection within seroconcordant relationships due to the probability and severity of transmission of ART-resistance. Quality assurance (QA) was conducted by review of tape recordings of each intervention session; recordings and session-specific QA checklists were reviewed by the study coordinator, a senior nurse, to monitor fidelity to condition and provide ongoing feedback to facilitators.
The group-based intervention was delivered to 8–10 participants at a time and utilized cognitive behavioral strategies to address HIV risk reduction, and was guided by the theories of reasoned action and planned behavior.18 Within this framework, it was hypothesized that the group intervention would improve individual attitudes and influence norms to impact risk reduction planning and perceived control of sexual risk behavior. The group intervention focused on sexual risk reduction, consistent use of male and female condoms, reducing sexual risk associated with alcohol or substance use, conflict resolution, sexual negotiation, effective communication, and antiretroviral medication adherence. The intervention applied cognitive behavioral strategies to sexual risk reduction (e.g., reframing thoughts, heightening participants' awareness of their reactions to condom use in their sexual relationships, and identifying automatic thoughts that could impede barrier use and communication). Sessions addressed IPV and antecedents to interpersonal conflict and violence; each session included relaxation techniques (deep breathing, imagery, or meditation) to respond to stress. Group strategies included establishment of a safe environment for sharing personal experiences, role-playing negotiation, problem solving and communication skills, and hands-on experiential training with condoms. While all sessions were gender separate, participants were given “couples homework” to address between sessions, and were provided with a week's supply of male and female condoms. Each subsequent week, participants were encouraged to share their experiences and apply cognitive behavioral skills in problem solving.
The individual-based condition was delivered to both partners together in health education sessions by a facilitator. The weekly session content was modeled on the Zambia Voluntary Counseling and Testing Services program. Participants were provided with HIV risk reduction information and counseling, information on sexual barrier use using a hierarchy of safer sex practices, and counseling to assist in making plans for their own behavior change and strategies for ongoing appraisal of their own behaviors. Participants were provided with hands-on condom use training, opportunity for discussion with the facilitator, and a week's supply of male and female condoms at the end of each session. All were encouraged to practice HIV-risk reduction strategies and share their HIV status and information with their partners. Individual sessions were supplemented with HIV-related health education videos to provide time and content equivalence with the group condition. The session represented an enhanced standard of care for HIV seroconcordant and -discordant couples, which is couples-based HIV counseling and testing, though most test individually and return with a partner to re-test.
Male and female condoms were provided during all sessions and participants in both conditions were given the option to come to the study offices to obtain additional condoms during the course of the study. Male and female condoms were available at no cost in all Zambian community health center and hospital clinics. In addition to condoms, both intervention arms offered over-the-counter vaginal creams and gels (i.e., sexual lubricants) as surrogates to assess the potential acceptability of these products as a vehicle for microbicides, products used to inactivate HIV or prevent transmission. All participants were advised at each session that the gel and cream products did not have anti-HIV or anti-STD properties and did not prevent pregnancy.
Statistical analyses
Descriptive analyses were used to characterize participants by demographic and behavioral variables, and correlations were estimated using Pearson correlations. Although all analyses were intention to treat, the analytic sample sizes varied somewhat across demographic and behavioral dimensions due to instances of missing data on questionnaire items. Multilevel analyses were conducted to test for mean differences in barrier acceptability, barrier use, problem solving discussion, and conflict tactics variables. Predictor variables included a factorial combination of condition (individual versus group), time (baseline, 6, and 12 months), and gender. To account for non-independence due to the dyadic nature of the data, all models included random residuals and a cross-partner correlation for the residuals (e.g., if one person had an especially positive attitude towards a method at a particular time point, the other person tended to be positive as well) as well as random intercepts for men and women along with a correlation between these intercepts (e.g., if one person had a consistently positive attitude towards a method over time, the other partner was also consistently positive).
The first set of analyses examined the effects of time, gender, and condition on (a) acceptability (i.e., “liking”) of sexual barrier methods, (b) willingness to use products or methods that prevent pregnancy, HIV/STDs, or both, (c) sexual barrier use over the last month or week, and (d) conflict resolution strategies. The second set of analyses examined whether (a) acceptability of barrier methods, (b) willingness to use these methods, (c) conflict resolution strategies, or (d) communication were predictive of reported general levels of barrier use.
Because acceptability and willingness vary across partners as well as across dyads, these analyses were framed within the Actor-Partner Interdependence Model (APIM) approach.7 Specifically, the effect of a person's own acceptance of a method on that person's reported use was investigated. The effect of a person's predictor on that person's outcome is referred to as an actor effect in the APIM. The effect that the partner's predictor has on the person's outcome, called a partner effect in the APIM, was also estimated. The outcome variables for each of these analyses, including acceptability, willingness, typical condom use, and weekly condom use, as well as other key predictor variables (e.g., IPV, communication), were assessed at baseline, 6, and 12 month follow-up for each of the two partners. All analyses were conducted with Predictive Analytics Software 18 (PASW®, SPSS Microsoft Corp, Chicago, Il).
Results
Demographics
Two hundred sixteen couples (n=432 individuals) completed baseline assessments. Participants were aged 19 to 69 (mean 38±8). Many were not working (n=283, 65%), and the majority reported less than US $5000 of personal income for the previous year (n=350, 81%). Nearly all participants were married (n=417, 97%); some identified as married while their partners did not. Mean number of years of school completed was 8±3. Ninety five percent of participants were HIV-positive (n=410) and 5% (n=22) were negative, resulting in 10% (n=22) of couples being serodiscordant. The mean length of time since HIV diagnosis was 2.6±2.7 years, and most (n=295, 72%) reported that they were on ARV medication at study entry. At baseline, intimate partner violence was reported by 45% (n=194) of participants. Unprotected sex was reported by 53% (n=113) of those participants who were sexually active in the last month (n=213, 49%). Participant demographics at baseline by condition (group vs. individual intervention) are presented in Table 1.
Table 1.
Demographics
| Total | ||||
|---|---|---|---|---|
| Characteristic | N (%) | Group | Individual | |
| (n=432 individuals) | M (sd) | N=216 | N=216 | t, χ2 |
| Age | 38 (8) | 38 (8) | 38 (8) | 0.02 |
| Employment status | 1.2 | |||
| Employed | 149 (35%) | 69 (32) | 80 (37) | |
| Unemployed | 283 (65%) | 147 (68) | 136 (63) | |
| Income (USD annually) | 2.0 | |||
| <5,000 | 350 (81%) | 170 (78) | 180 (83) | |
| 5,000–10,000 | 22 (5%) | 11 (5) | 11 (5) | |
| >10,000 | 60 (14%) | 35 (16) | 25 (12) | |
| Marital status | 1.73 | |||
| Married | 417 (97%) | 211 (98%) | 206 (95%) | |
| Not married | 15 (3%) | 5 (2%) | 10 (5%) | |
| Education (highest grade completed) | 8 (3) | 8 (3) | 8 (3) | 0.64 |
| HIV serostatus | 1.7 | |||
| Positive | 410 (95%) | 208(96) | 202 (94) | |
| Negative | 22 (5%) | 8 (4) | 14 (6) | |
| Length of time since HIV diagnosis (yrs) | 2.6 (2.7) | 2.4 (2.1) | 2.9 (3.1) | 2.0a |
| On ART | 1.0 | |||
| Yes | 295 (72%) | 145 (70) | 150 (74) | |
| No | 115 (28%) | 63 (30) | 52 (26) | |
| Unprotected sex (last month) | 0.28 | |||
| Yes | 113 (53%) | 64 (55%) | 49 (51%) | |
| No | 100 (47%) | 53 (45%) | 47 (49%) | |
| Intimate partner violence | 0.00 | |||
| Yes | 194 (45%) | 97 (45%) | 97 (45%) | |
| No | 238 (55%) | 119 (55%) | 119 (55%) | |
p<0.05.
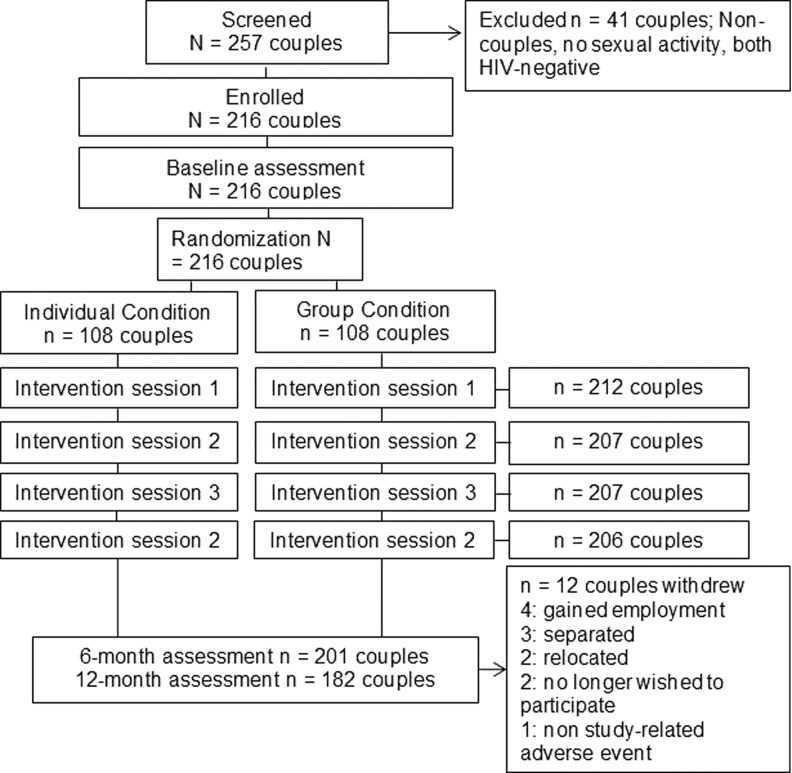
Attendance at intervention sessions was high (range: 95–98%) and retention rates for 6 and 12 month follow-up assessments were 93% and 84%, respectively. Details of participant screening, enrollment, attendance, retention, and withdrawal are presented in Fig. 1.
FIG. 1.
Participant flow diagram.
Barrier acceptability
Participant ratings of how much they liked each of the barrier methods (male condom, female condom, gel, and cream), as well as an overall acceptability measure of all four methods were examined over time. Additionally, participant willingness to use methods that prevent pregnancy alone, sexually transmitted diseases alone, or both was measured over time. Table 2 presents the means and standard deviations for these variables.
Table 2.
Acceptability and Willingness to Use Sexual Barrier Products Over Time
| Baseline | 6-month | 12-month | |
|---|---|---|---|
| m (sd) | follow-up | follow-up | |
| Product acceptability | |||
| Male condoms | 3.84 (1.81) | 4.18 (1.64) | 4.23 (1.58) |
| Female condoms | 1.10 (1.88) | 3.22 (2.00) | 3.32 (1.96) |
| Creams | 0.22 (0.88) | 1.53 (2.11) | 1.45 (2.06) |
| Gels | 0.25 (0.98) | 3.00 (2.08) | 2.87 (2.12) |
| Willingness to use products to | |||
| Prevent pregnancy | 3.42 (1.10) | 3.56 (0.98) | 3.61 (0.93) |
| Prevent STDs, including HIV | 2.77 (1.39) | 3.11 (1.26) | 3.09 (1.27) |
| Prevent pregnancy and STDs, including HIV | 3.53 (1.04) | 3.65 (0.92) | 3.69 (0.87) |
For the aggregate acceptability measure, the only effect was for time, with F(2,400)=405.35, p<0.001. The means in Table 2 clearly show that acceptability was higher at the two post-intervention assessments than at baseline. Neither condition nor gender moderated the effect of time for this aggregate measure.
Examination of the single method variables showed evidence of a similar effect of time (male condom F(2,410)=8.95, p<0.001; female condom F(2,401)=207.12, p<0.001; gel F(2,408)=391.09, p<0.001; cream F(2,403)=93.58). In each case, acceptability of the method increased substantially from baseline. Moreover, these effects appear to remain without diminishing over the 6- to 12-month assessments.
There were some additional effects for acceptability of the four methods. Acceptability of male condoms had a main effect of gender, F(1,213)=38.86, p<0.001, such that men found male condoms to be more acceptable (M=4.40, SD=1.32) than women (M=3.76, SD=1.94), as well as an interaction between time and gender, F(2,411)=4.20, p=0.016. The means over time for men and women show that the overall effect of time was largely driven by an improvement in men's attitude towards male condoms (baseline M=4.01, 6-month M=4.61, 12-month M=4.63) while women's attitudes did not change substantially over time (baseline M=3.67, 6-month M=3.76, 12-month M=3.85). The acceptability of gels also showed a main effect of gender [F (1,214)=5.74, p=0.017]. Gels were more acceptable among women (M=2.10, SD=2.25) than among men (M=1.84, SD=2.13).
Finally, there were several main effects and interactions for acceptability of creams. A main effect of condition, F(1,210)=16.03, p<0.001, showed that on average, creams were more acceptable in the individual condition (M=1.30) than in the group condition (M=0.84). There was also a condition by time interaction, F(2,403)=14.31, p<0.001. This interaction showed that although the effects of time were significant in both conditions, the increase from baseline in the individual condition (baseline M=0.12, 6-month M=1.92, 12-month M=1.86; F(2,206)=85.30, p<0.001) was greater than the same effect in the group condition (baseline M=0.32, 6-month M=1.12, 12-month M=1.07; F(2,195)=18.49, p<0.001).
Participants' reports of their willingness to use methods that prevent pregnancy, STDs, or both also showed main effects of time (see Table 2). For methods that prevent pregnancy alone, the effect of time was F(2,406)=5.90, p=0.003. Post-hoc tests using a Bonferroni correction indicated that 12-month reports were higher than baseline, with 6-month reports falling in between. Willingness to use methods that prevent STDs alone also differed by time with F(2,401)=11.39, p<0.001. In this case, willingness increased significantly at both 6- and 12-month assessments relative to baseline. There was also a gender main effect for this variable such that men reported higher willingness to use these methods (M=3.16) than did women (M=2.81). Finally, willingness to use methods that prevent both pregnancy and STDs showed main effects of time, F(2,403)=4.45, p=0.012, and gender, F(1,197)=3.96, p=0.048. Post-hoc Bonferroni tests showed that 12-month reports were higher than baseline, but the 6-month reports were not different from either baseline or the 12-month follow-up. The gender difference showed that men were somewhat more willing to use these methods (M=3.69) relative to women (M=3.55).
Barrier use
As was the case with barrier acceptability, there were consistent main effects of time that generally reflected an increase in barrier use at both 6- and 12-month follow-up relative to baseline. Table 3 presents the means and standard deviations as a function of time. Rate of condom use during the past week, use of male condoms, use of female condoms, use of some type of protection during vaginal sex in the past month, and frequency of condom use in the past month all showed main effects of time with F(2,316)=15.85, p<0.001; F(2,251)=6.72, p=0.001; F(2,250)=9.54, p<0.001; F(2,238)=11.57, p<0.001; and F(2,408)=28.56, p<0.001, respectively.
Table 3.
Use of Sexual Barrier Products Over Time
| Baseline | 6-month | 12-month | |
|---|---|---|---|
| Product | m (sd) | follow-up | follow-up |
| Male condoms, percent use in past week | 0.77 (0.36) | 0.90 (0.21) | 0.89 (0.25) |
| Male condoms, past montha | 3.99 (1.36) | 4.39 (0.96) | 4.32 (1.06) |
| Female condoms, past month | 1.76 (1.37) | 2.26 (1.28) | 2.30 (1.40) |
| Any type of protection, past month | 3.58 (1.60) | 4.17 (1.33) | 3.97 (1.43) |
| Male and female condom use, in generalb | 4.20 (1.27) | 4.65 (0.81) | 4.62 (0.84) |
Barrier use in the past month was scored using a Likert scale; 5=every time, 4=almost every time, 3=sometimes, 2=almost never, 1=never.
Condom use in general is scored using a Likert scale, scoring is identical to monthly barrier use.
In addition to the consistent main effects over time, there were several other main effects and interactions across the barrier use variables. Use of female condoms showed a main effect of gender, F(1,174)=11.46, p=0.001 such that women reported higher female condom use relative to men. Use of some type of protection during vaginal sex showed evidence of a two-way interaction between gender and condition, F(1,156)=4.11, p=0.044, as well as a three-way interaction between time, gender, and condition, F(2,236)=3.39, p=0.035. Follow-up analyses showed that these interactions occurred because the general pattern of increases over time was evident in the group condition for men [F(2,102)=4.40, p=0.015] and women [F(2,91)=6.87, p=0.002], and in the individual condition for men [F(2,84)=6.71, p=0.002]. However in the individual condition, women did not show the general pattern of increase from baseline to each of the follow-up sessions, F(2,105)=0.12, p=0.887, (baseline M=3.86, SD=1.52; 6-month M=3.81, SD=1.49, 12-month M=3.68, SD=1.63).
Conflict resolution strategies
Results for conflict resolution strategies were somewhat less consistent relative to acceptability and use. Positive communication strategies showed main effects of time [F(2,389)=8.96, p<0.001] and gender [F(1,212)=9.48, p=0.002]. As can be seen in Table 4, the time main effect occurred because use of positive communication strategies was higher at 12-month follow-up relative to baseline and 6-month follow-up. The gender main effect showed that men used more positive communication strategies, M=5.88, SD=4.67, than did women, M=4.89, SD=4.94. Both the condition by gender and time by condition by gender interactions were also statistically significant, F(1,212)=5.56, p=0.019, and F(2,397)=3.64, p=0.027, respectively. In the individual condition, women's positive communication decreased from baseline to 6-month follow-up but then increased dramatically at the 12-month follow-up, F(2,192)=7.74, p=00.001, but the men's communication showed a small, nonsignificant increase over time, F(2,196)=1.92, p=0.150. In contrast, in the group condition men showed a weak pattern of an initial decrease, but then a subsequent increase [F(2,197)=1.22, p=0.297] and it was the women who showed a relatively consistent increase over time [F(2,197)=3.90, p=0.002].
Table 4.
Positive and Negative Communication and Violence Over Time
| Baseline | 6-month | 12-month | |
|---|---|---|---|
| m (sd) | follow-up | follow-up | |
| Positive communication | 5.13 (4.72) | 4.97 (4.63) | 6.10 (5.09) |
| Negative communication | 4.26 (5.21) | 3.72 (5.52) | 3.95 (6.16) |
| Violence | 3.69 (6.33) | 2.77 (6.59) | 2.98 (7.33) |
| Extreme violence | 0.72 (1.98) | 0.60 (2.04) | 0.78 (2.56) |
Although there were no differences for negative communication, there were effects for violence. Violence showed a time main effect, F(2,389)=3.26, p=0.040, and the means in Table 4 suggest that reports of violence decreased at both the 6- and 12-month follow-up sessions relative to baseline. Violence also showed a three-way interaction between time, gender, and condition, F(2,385)=3.17, p=0.043. The means for this interaction indicate that the individual condition women's reports of violence decreased over time, F(2,186)=4.12, p=0.018, but men's did not change, F(2,196)=0.87, p=0.419. In contrast, in the group condition men's reports of violence decreased, F(2,192)=4.57, p=0.011 but women's did not, F(2,200)=0.62, p=0.540. Finally, only the gender main effect was significant for reports of extreme violence, F(1,209)=4.84, p=0.029. Women reported higher scores for extreme violence, M=0.86, SD=2.40, than did men, M=0.54, SD=1.96.
Predicting use of barriers with sexual barrier acceptability
Participants' use of barriers was assessed using a variety of measures. Participants estimated their rate of condom use in the past week and they rated how often they used (a) protection, (b) male condoms specifically, and (c) female condoms specifically during vaginal sex for the past month on a five-point scale (5=all the time; 1=never in the past month). They also used the same endpoints to respond to the question “when you have sex, how often do you use a condom?” The APIM was used for these analyses, and the key predictors were the person's perception of barrier acceptability and the partner's perception of acceptability. Actor and partner effects were examined for both the aggregate acceptability variable as well as acceptability of male and female condoms specifically.
The actor effects for the aggregate acceptability measure were statistically significant for all five use measures, indicating that individuals who found barrier methods to be more acceptable tended to report higher use. There were also two partner effects for rate of condom use in the past week and general condom use during sex. In both of these cases, individuals report higher general condom use when their partners are more accepting of barrier methods.
The effects of acceptability of male condoms and female condoms on the use of those products were examined separately. Individuals who reported more accepting attitudes towards male condoms reported using male condoms and barriers more often; additionally, there was a small nonsignificant negative effect of acceptability of male condoms on female condom use. As was the case with the aggregate acceptability variable, there was evidence that individuals whose partners found male condoms to be more acceptable tended to report higher use. Finally, a similar pattern of actor and partner effects emerged for acceptability of female condoms. In terms of actor effects, individuals who reported higher acceptability of female condoms reported higher use—particularly for use of female condoms. For partner effects, individuals whose partners were more accepting of female condoms reported a higher rate of condom use in the past week and in general.
Predicting use of barriers with willingness to use barriers
The next set of analyses examined whether a person's reported use of barriers could be predicted by the person's and partner's reported willingness to use methods that protect against pregnancy alone, STDs alone, or pregnancy and STDs. There was some evidence that willingness to use methods that prevent both pregnancy and STDs, and those that prevent pregnancy alone, were associated with higher use of these methods. However, there was no evidence that individuals who reported higher willingness to use methods that protect against STDs alone used these methods more. Only two partner effects emerged. Individuals whose partners were more willing to use methods that prevent both pregnancy and STDs reported higher use of protection in the past month, and individuals whose partners were more willing to use methods that prevent STDs alone reported a higher rate of condom use in the past week.
Predicting use of barriers from communication and violence
We also examined whether we could predict a person's reported use of barriers as a function of the person's and partner's reports of the tactics they use during conflicts. The only effect of using positive communication strategies was a negative partner effect for barrier use in the past month, b=− 0.028, β=− 0.091, s.e.=0.013, p=0.034. This suggests individuals whose partners report using positive strategies more tend to report using barriers less frequently. The only effect of negative communication was an actor effect for general condom use during sex, b=− 0.012, β=− 0.067, s.e.=0.005, p=0.024, such that individuals who used more negative communication reported lower general condom use during sex. Finally, reports of use of violence predicted less male condom use within the past week, b=− 0.024, β=− 0.140, s.e.=0.009, p=0.006, as well as less condom use in general, b=− 0.011, β=− 0.070, s.e.=0.005, p=0.021.
Discussion
This study compared whether an HIV risk-reduction intervention would be more likely to increase sexual barrier acceptability, willingness to use barriers, and sexual barrier use when delivered to Zambian couples in a gender matched group or individual format, examining the impact of couple members on each other with regard to acceptability, sexual barrier use, and conflict resolution strategies. The impact of partners' mutual influence on willingness to use barriers, barrier acceptability, and conflict resolution strategies on the prediction of sexual barrier use was examined. Barrier acceptability, willingness to use barriers, and sexual barrier use increased over time in both conditions, and were influenced by gender preferences. In contrast with previous studies,19 acceptability and willingness to use barriers predicted sexual barrier use. Positive communication increased and violence decreased over time in both conditions.
While all couples reported increases in acceptability, willingness to use barriers and sexual barrier use, clear differences in product preferences and improvements in overall preference occurred by gender. Acceptability of male condoms increased most among men and acceptability of gels increased most among women. Interestingly, willingness to use products for prevention of STDs and pregnancy increased the most among men, though willingness to use barriers only to prevent STDs was not associated with their use. Reported use of female condoms increased most among women, while both genders reported increases in male condom use. Despite initially low levels of acceptability of female condoms, use of female condoms may have been undetected by some male partners, and findings may reflect a lack of awareness of female condom use by male partners. Results highlight the importance of addressing the potential influence of couple members on each other's condom use, and as one might expect, among couples in which members had a clear preference for male condoms, female condom use was lower.
Increases in acceptability, willingness to use products, and their use clearly emphasize the impact of exposure to study interventions (including exposure to products) on behavior and preferences. Both group and individual conditions achieved high rates of condom use approaching consistent levels, and in contrast with many previous studies,20 sustained high levels of use at long-term follow up. Most sexual risk reduction interventions have not included both members of the couple; having both members of the couple present may enhance sustained condom use over time. Previous studies have utilized behavioral interventions to reduce risk behavior and prevent HIV transmission;21 results reinforce the use of both types of interventions for dissemination of safer sex strategies. Given the comparability of conditions, the group strategy may represent a more cost-effective method of reaching larger numbers of participants. However, implementing couples-based interventions can be challenging due to high rates of nondisclosure of HIV serostatus between couple members. The strategy utilized in this intervention, intervening on simultaneous gender-concordant groups of mixed HIV serostatus without requiring disclosure to other group members, may be an optimal approach to achieve the benefits of a couples' intervention while simultaneously protecting sensitive information related to those attending the intervention.
Although communication about condoms has been previously identified as a key element in HIV prevention,22 increases in both positive and negative communication were associated with decreased condom use. Results may have been influenced by the requirements for study sample, which recruited only established couples of more than 6 months duration. Future studies should continue to address condom negotiation within high risk seroconcordant and -discordant couples.9,23,24 As longer-term relationships may appear protective but also carry the potential risk of HIV infection, the negotiation of condom use should continue to be addressed within couples-based interventions. Finally, this study found that intimate partner violence predicted decreased condom use. Findings support previous research associating IPV with decreased condom use and increased risk of HIV acquisition among African women.25,26 Interventions to reduce IPV may represent a critical, yet under-utilized, component of HIV prevention in sub-Saharan Africa.
This study has limitations related to the generalizability of acceptability and use outcomes in non-urban populations. In addition, the study relied upon self-report of product use, and though ACASI was used to reduce socially endorsed responses, reports may have been inflated. Additionally, the number of serodiscordant couples in this study was insufficient to enable more complex analyses; future studies targeting serodiscordant couples should continue to address potential differences in responses to sexual risk reduction interventions by serostatus. Finally, although the data presented was collected from 2006 to 2010, similar sexual behavior was reported in subsequent studies by this team in Zambia.24,27
This study presented two approaches to HIV prevention among couples, individual and gender concordant group sessions, that achieved similar increases in sexual barrier use following study interventions. Results provide support for the use of both methods, and highlight the mutual influence of partners and communication on sexual barrier use among couples in sub-Saharan Africa.28,29 Future prevention studies should incorporate both products and partners to achieve optimal outcomes.
Acknowledgments
This study was supported by a grant from NIH, R01MH63630. We would like to acknowledge the NOW2 study team, study participants, and remembrance of Ganapati J. Bhat, MD, and Violet Bwalya, RN, LMW, without whom this study would not have been possible.
Author Disclosure Statement
D. Jones, D. Kashy, N. Chitalu, C. Kankasa, M. Mumbi, R. Cook, and S.M. Weiss declare that they have no conflict of interest.
References
- 1.UNAIDS (2010). Report on the Global AIDS Epidemic 2010. Retrieved from http://www.unaids.org/globalreport/Global_report.htm Accessed November5, 2012
- 2.Johnson BT, Scott-Sheldon LAJ, Smoak ND, et al. Behavioral interventions for African Americans to reduce sexual risk of HIV: A meta-analysis of randomized controlled trials. J Acq Immune Def Syndromes 2009;51:492–501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burton J, Darbes LA, Operario D. Couples-focused behavioral interventions for prevention of HIV: Systematic review of the state of evidence. AIDS Behav 2010;14:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Allen S, Meinzen-Derr J, Kautzman M, et al. Sexual behavior of HIV discordant couples after HIV counseling and testing. AIDS 2003;17:733–740 [DOI] [PubMed] [Google Scholar]
- 5.Jones DL, Weiss SM, Chitalu N, et al. Sexual risk reduction among Zambian couples. SAHARA J 2009;6:69–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El-Bassel N, Wechsberg WM. Couple-based behavioral HIV interventions: Placing HIV risk-reduction responsibility and agency on the female and male dyad. Couple Family Psychol Res Practice 2012;1:94–105 [Google Scholar]
- 7.Kenny DA, Kashy DA, Cook WL. Dyadic Data Analysis. New York, NY: Guilford Press, 2006 [Google Scholar]
- 8.Swan H, O'Connell DJ. The impact of intimate partner violence on women's condom negotiation efficacy. J Interpers Violence 2011;27:775–792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marlow HM, Tolley EE, Kohil R, Mehendale S. Sexual communication among married couples in the context of a microbicide clinical trial and acceptability study in Pune, India. Culture Health Sex 2010;12:899–912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Njau B, Watt MH, Ostermann J, et al. Perceived acceptability of home-based couples voluntary HIV counseling and testing in Northern Tanzania. AIDS Care 2012;24:413–419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Albarracin D, Tannenbaum MB, Glasman LR, Rothman AJ. Modeling structural, dyadic, and individual factors: The inclusion and exclusion model of HIV related behavior. AIDS Behav 2010;14:S239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones D, Weiss SM, Malow RM, et al. A brief sexual barrier intervention for women living with AIDS: Acceptability, use and ethnicity. J Urban Health 2001;78:593–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones DL, Weiss SM, Bhat GJ, et al. Sexual barrier intervention for HIV+/- Zambian women: Acceptability and use of vaginal chemical barriers. J Multicultural Nursing Health 2004;10:27–31 [PMC free article] [PubMed] [Google Scholar]
- 14.Jones D.L, Ross D, Weiss S.M., et al. Influence of partner participation on sexual risk behavior reduction among HIV-positive Zambian women. J Urban Health 2005;82(3 suppl 4):iv92–100 [DOI] [PubMed] [Google Scholar]
- 15.Alcaide M, Jones D, Chitalu N, Weiss SM. Chlamydia and gonorrhea infections in HIV positive women in urban Lusaka, Zambia. J Global Infect Dis 2012;4:141–144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meyer-Bahlberg HFL, Ehrhardt AA, Exner TM, Gruen RS. Sexual Risk Behavior Assessment Schedule: Adult (SERBAS-A-DF-4) Manual. New York, NY: Psychological Press, 1990 [Google Scholar]
- 17.Straus MA. Measuring intrafamily conflict and violence: The Conflict Tactics Scales. J Marriage Family 1979;41:75–88 [Google Scholar]
- 18.Azjen I. The theory of planned behavior. Organ Behav Human Decision Processes 1991;50:179–211 [Google Scholar]
- 19.Minnis AM, Shiboski SC, Padian NS. Barrier contraceptive method acceptability and choice are not reliable indicators of use. Sex Trans Dis 2003;30:556–561 [DOI] [PubMed] [Google Scholar]
- 20.Kalichman SC, Cain D, Weinhardt L, et al. Experimental components analysis of brief theory-based HIV/AIDS risk-reduction counseling for sexually transmitted infection patients. Health Psychol 2005;24:198–208 [DOI] [PubMed] [Google Scholar]
- 21.Scott-Sheldon LA, Huedo-Medina TB, Warren MR, et al. Efficacy of behavioral interventions to increase condom use and reduce sexually transmitted infections: A meta- analysis, 1991 to 2010. J Acq Immune Defic Syndromes 2011;58:489–498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sales JM, Lang DL, DiClemente RJ, et al. The mediating role of partner communication frequency on condom use among African American adolescent females participating in an HIV prevention intervention. Health Psychology 2012;31:63–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stephenson R, Vwalika B, Greenberg L, et al. A randomized controlled trial to promote long-term contraceptive use among HIV-serodiscordant and concordant positive couples in Zambia. J Women's Health 2011;20:567–574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chitalu N, Mumbi M, Cook R, Weiss SM, Jones D. The impact of key HIV intervention components as predictors of sexual barrier use: The Zambia Partner Project. J Intl Assoc Physicians AIDS Care January30, 2014. [Epub ahead of print] doi: 10.1177/2325957414520980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fontenot HB, Fantasia HC, Lee-St John TJ, Sutherland MA. The effects of intimate partner violence duration on individual and partner-related sexual risk factors among women. J Midwifery Women's Health 2014;59:67–73 [DOI] [PubMed] [Google Scholar]
- 26.Lifshay J, Nakayiwa S, King R, et al. Partners at risk: Motivations, strategies, and challenges to HIV transmission risk reduction among HIV-infected men and women in Uganda. AIDS Care 2009;21:715–724 [DOI] [PubMed] [Google Scholar]
- 27.Jones D, Weiss SM, Arheart K, Cook R, Chitalu N. Implementation of HIV prevention interventions in resource limited settings: The Partner Project. J Community Health 2014;39:151–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller AN, Golding L, Kyalo wa N, et al. Couples' communication on sexual and relational issues among the Akamba in Kenya. Afri J AIDS Res 2009;8:51–60 [DOI] [PubMed] [Google Scholar]
- 29.Rispel LC, Cloete A, Metcalf CA, et al. ‘It [HIV] is part of the relationship’: Exploring communication among HIV-serodiscordant couples in South Africa and Tanzania. Culture Health Sex 2012;14:257–268 [DOI] [PubMed] [Google Scholar]