Abstract
Background
The goal of this study was to assess the value of a urinary biomarker profile comprised of Neutrophil Gelatinase-associated Lipocalin (NGAL), Fibroblast Growth Factor-2 (FGF-2), and Epidermal Growth Factor (EGF), to detect acute kidney injury (AKI) in critically ill neonates.
Methods
We conducted a prospective cohort pilot study of at-risk neonates treated in a level IIIC neonatal intensive care unit (NICU) with therapeutic hypothermia (HT) (n = 25) or extracorporeal membrane oxygenation (ECMO) (n=10). Urine was collected at baseline, 48 hours of illness, and > 24 hours post recovery of their corresponding treatments. Control samples were collected from 27 healthy newborns. The data were expressed as urinary concentrations and values normalized for urinary creatinine. AKI was defined as the presence of oliguria >24 hours and/or elevated serum creatinine (SCr), or the failure to improve the estimated creatinine clearance (eCCL) by >50% post recovery. Non-parametric statistical tests and ROC analyses were used to interpret the data.
Results
Fifteen at risk newborns had AKI. In the first 48 hours of illness, the urinary levels of NGAL and FGF-2 had high sensitivity but poor specificity to identify neonates with AKI. At recovery, low urinary EGF levels identified neonates with AKI with a sensitivity of 74% and specificity of 84%. Overall, in the early stages of a critical illness, the urinary levels of NGAL and FGF-2 were sensitive, but not specific, to identify neonates at risk of AKI. Low EGF levels post-recovery, identified critically ill neonates with AKI.
Conclusions
These findings require validation in larger prospective studies.
Keywords: Neonate, Acute Kidney Injury, urinary biomarkers, hypothermia
Introduction
Critically ill neonates frequently suffer significant hypoxic and/or ischemic events resulting in multisystem injury, and are at especially high risk for developing acute kidney injury (AKI) [1–3]. Two such patient groups include infants with hypoxic-ischemic encephalopathy (HIE) requiring therapeutic hypothermia (HT) and infants with neonatal hypoxemic respiratory failure requiring treatment with extracorporeal membrane oxygenation (ECMO) [4, 5]. In these patients, AKI is a major cause of mortality and long term morbidity [1, 5–8].
The diagnosis of neonatal AKI can be problematic as standard clinical criteria used in pediatric and adult patients, such as serum creatinine and urine output, are unreliable in the newborn period [9]. Serum creatinine concentrations are reflective of maternal levels in the first few days of life [10, 11] and subsequent elevations in serum creatinine are seen late in the setting of renal injury. Oliguria (i.e. urine output less than 1ml/kg/hr.), is an insensitive marker of renal function in the newborn, as AKI can be seen in the absence of oliguria [3]. These limitations highlight the need for non-creatinine/oliguria based AKI diagnostic criteria. Novel biomarkers that can detect AKI within hours of an insult may serve to answer this diagnostic dilemma. Urinary biomarkers are of particular interest as they can be measured from an easily accessible biological fluid that is directly derived from the organ of interest.
Among candidate biomarkers, Neutrophil Gelatinase-associated Lipocalin (NGAL) is considered one of the most sensitive biomarkers of AKI [12–14]. Previous studies have shown that the synthesis of NGAL is up-regulated within hours of ischemia-reperfusion injury [14]. Moreover, NGAL accumulates in the proximal tubule of human kidneys after ischemic and acute tubular necrosis [15]. However, NGAL is also produced by normal distal tubular cells and extra-renal tissues, and is highly induced in inflammatory conditions [16, 17]. Thus, the presence of systemic infections and other co-morbidities that induce the non-renal release of NGAL may affect the ability of urinary NGAL to predict AKI.
For these reasons, we undertook this study to determine whether NGAL, in combination with FGF-2 and EGF, will improve our ability to identify AKI in newborns treated with HT or ECMO. We selected both growth factors, because they are involved in the pathogenesis of AKI and the regeneration of renal tubules [18–23]. In fact, FGF-2 is released by injured endothelial cells, and renal endothelial injury plays a key role in the pathogenesis of AKI [24]. Moreover, the urinary levels of EGF are decreased in children and adults with acute or chronic renal tubular injury [21, 22, 25–28]. Therefore, we tested the hypothesis that a urinary biomarker profile comprised of elevated urinary levels of NGAL and FGF-2, in combination with decreased urinary EGF levels, will improve our ability to identify AKI in critically ill neonates treated with HT or ECMO.
Materials and Methods
Study Population
This study was a prospective observational cohort study of neonates at risk for AKI admitted to Children’s National Medical Center’s level IIIC neonatal intensive care unit between 2010 and 2011. Inclusion criteria were all infants who were greater than 36 weeks gestation meeting institutional criteria for either 1) therapeutic HT or 2) ECMO life support. Infants in the HT group were identified and treated according to the National Institutes of Health and Human Development Neonatal Research Network protocol [29]. Criteria for ECMO during the study period included persistent hypoxia (preductal SaO2<85%) despite maximal ventilatory and medical therapy or intractable cardiovascular instability. Infants were excluded from either group if they had major congenital anomalies or suspected chromosomal abnormalities. Urine samples were collected also from 27 healthy full term newborns recruited from The George Washington University Medical Center. This study was approved by the Institutional Review Board of Children’s National Medical Center and a Waiver of Documentation of Informed Consent and Health Insurance Portability and Accountability Act Authorization was obtained to allow for anonymized data collection, after parental verbal agreement was given to collect the samples.
Data and Specimen Collection
Serum creatinine values were obtained in all patients before the initiation of therapy. Urine was collected in study subjects within 24 hours after the initiation of therapy (baseline), at 48hrs after initiation of therapy, and >24 hours post recovery (e.g. post decannulation for ECMO infants and post re-warming for Hypothermia infants). Control samples were collected from healthy term newborns between 24–48 hours of life. Urine was collected either from indwelling urinary catheters (when in place) or otherwise extracted from absorbent diapers. Urine samples were centrifuged and the supernatant was stored at −70°C.
All corresponding clinical information, including the birth weight, gender, gestational age, Apgar scores, and race, were collected. Renal function data were collected for time points corresponding to urine collections including urine output (UOP), blood urea nitrogen (BUN) and serum creatinine (Scr). Urine output was measured according to strict intake and output monitoring protocol per NICU standard of care (i.e. either by quantification of output from an indwelling catheter, or by calculation of corrected diaper weight every 3 hours). Estimated creatinine clearance (eCCl) was calculated using the following formula: CrCl=(k*Ht)/Cr-serum [30]. AKI was defined as; 1. UOP < 1 ml/kg/hr. with SCr >1 mg/dL for 24 hrs. 2. SCr of >1.5mg/dL [10]; or 3. failure to improve eCCL by >50%, since improvement of eCCL was expected with increasing postnatal age and after adequate resuscitation and therapy. These definitions of AKI were selected because we anticipated admitting critically ill newborns of normal gestational age, and to start their respective treatments during the first 72 hours of life, when their SCr. levels reflect the maternal levels. Other definitions of neonatal AKI do not take into consideration the clinical situation of these patients, who may not show an increase in SCr or decrease urine output, but are unable to decrease the SCr levels < 1 mg/dL, or improve their eCCl > 50 % by the end of first week of life. The failure to improve the GFR by > 50 % cut-off point was selected because the pRIFLE injury criteria require a 50% reduction in the eCCl, and this AKI stage appears to be correlated with the clinical outcome of critically ill infants. This definition was not used in patients with normal baseline SCr levels after the fourth day of life, and a minimum SCr of > 0.5 mg/dL was required to diagnose AKI.
Biomarker Assessment
The urinary levels of NGAL, FGF-2, and EGF, were measured using enzyme-linked-immunoabsorbent (ELISA) assay kits that are commercially available. NGAL was measured using the NGAL Rapid ELISA Kit from BioPortoR (Gentofte, Denmark), as described by the manufacturer’s instructions. Inter-and intra-assay coefficient of variation for this assay is 3 −12 %. The urinary levels of FGF-2 and EGF were measurd using ELISA Quantikine Kits from R&D SystemsR. (Minneapolis, MN, USA). The inter- and intra-assay coefficient of variation for the FGF-2 and EGF assays are 3–9 % and 2–8 % respectively, and our measurements were within these ranges, < 5 % and <`10% respectively for both assays. Urinary creatinine levels were determined using the Creatinine Parameter assay kit from R&D Systems. The final results were expressed both in absolute values as a ratio of the urinary creatinine concentration, and as a concentration per mL of urine.
Statistical Analysis
Demographic and clinical data are reported as medians (ranges) and absolute numbers for continuous and categorical variables respectively. Biomarker values are depicted as medians with interquartile ranges (IQR). Differences between cases and controls were analyzed using Mann Whitney U and Chi-square tests where appropriate. Receiver-operating curves were done to determine the biomarker cut-off values for optimal sensitivity and specificity. These cut-off values were then evaluated for their ability to predict renal injury in the at-risk group. Contingency tables were generated using the Graph Pad Prism 4 software. In addition, to determine how the selected biomarkers performed together, multiple logistic regression analysis and combined ROC curves were done using the MedCalc software, as previously described [8]. Other statistical tests were done using SPSS 18.0 software (SPSS Inc).
Results
Patients
A total of 35 subjects (HT n = 25 and ECMO n = 10) and 27 healthy control newborns were enrolled in this study. Their demographic and clinical characteristics are summarized in Table 1. The ECMO group was predominantly male, but otherwise there were no significant differences between groups with regard to baseline characteristics. Clinical data reflecting the renal status of the study subjects are presented in Table 2. Both groups were frequently exposed to nephrotoxic medications (i.e. vancomycin, gentamicin, and furosemide). Hypotension was also common, occurring in nearly half of the patients treated with HT and all patients treated with ECMO. As shown in table 3, fifteen patients (43%) developed AKI.
Table 1.
Demographic and clinical characteristics of critically ill newborns.
|
Controls (N=27) |
Hypothermia (N=25) |
ECMO (N=10) |
|
|---|---|---|---|
|
Birth weight (Kilograms) |
3.3 (2.5–4.0) | 3.5 (2.0–4.7) | 2.9 (2.2–4.8) |
| P value* | 0.455 | 0.551 | |
|
Gender (n male) |
13 | 13 | 8 |
| P value* | 0.127 | 0.080 | |
|
Gestational Age (weeks) |
39 (36–41) | 40 (36–44) | 38 (35–41) |
| P value* | 0.155 | 0.598 | |
| Apgar | |||
| 1minute | n/a | 1 (0–6) | 3 (0–9) |
| 5 minutes | n/a | 4 (1–7) | 6 (3–9) |
| Race (n) | |||
| White | 10 | 9 | 3 |
| Black | 8 | 13 | 6 |
| Other | 9 | 3 | 1 |
| P value* | 0.124 | 0.187 | |
|
Time of Urine Collection (day of life) |
|||
| Baseline | 2 (1–3) | 1 (0–1) | 1.5(1–4) |
| 24–48hr | n/a | 2 (2–3) | 3.5 (2–7) |
| Recovery | n/a | 5 (5–6) | 10 (5–28) |
Data expressed as median (range) unless otherwise indicated.
Comparison to Control Group
Table 2.
Renal Function Data of the Study Subjects
|
Hypothermia (n=25) |
ECMO (n=10) |
P-value |
|
|---|---|---|---|
| Urine Output (mL/kg/hr) | |||
| Baseline | 2 (0.2–4.4) | 4.7 (1.8–9.5) | 0.001 |
| 48hr | 2.5 (0.7–6.4) | 4.2 (2.8–7.1) | 0.014 |
| Recovery | 3.1 (1.1–5.3) | 5.8 (3.6–8.3) | 0.001 |
| Blood Urea Nitrogen (mg/mL) | |||
| Baseline | 11 (5–30) | 12 (4–21) | 0.635 |
| 48hr | 10 (3–27) | 14.5 (12–28) | 0.016 |
| Recovery | 9 (2–19) | 18 (6–31) | 0.001 |
| Serum Creatinine (mg/mL) | |||
| Baseline | 1.2 (0.7–1.8) | 0.8 (0.6–1.2) | 0.031 |
| 48hr | 0.7 (0.3–1.8) | 0.75 (0.5–1.4) | 0.637 |
| Recovery | 0.6 (0.3–1.1) | 0.5 (0.1–0.6) | 0.207 |
| eCCL (mL/min) | |||
| Baseline | 18.7 (12.5–36.6) | 26.4 (16.5–41.2) | 0.041 |
| 48hr | 31.8 (13–81) | 31.8 (15.2–41.2) | 0.695 |
| Recovery | 39.4 (19.2–76.5) | 48.6 (34.1–207) | 0.139 |
| Fluid Balance (ml/d) | |||
| Baseline | 86 (−130, 370) | 124 (−240, 665) | 0.361 |
| 48hr | 65.5 (−117, 261) | 116 (−226, 226) | 0.465 |
| Recovery | 68 (−79, 252) | 40 (−109, 214) | 0.298 |
| Nephrotoxic Medication | 23 | 10 | 0.357 |
| Exposure, n | |||
| Hypotension Requiring | 12 | 10 | 0.004 |
| Vasopressor Therapy, n | |||
| Acute Kidney Injury | 10 | 5 | 0.178 |
| --Oliguria / SCr >1.5, n | 4 | 0 | |
| --eCCLRecovery <50%, n | 9 | 5 | |
Data expressed as median (range) unless otherwise indicated.
Table 3.
NGAL, FGF-2, and EGF concentrations expressed per mL of urine.
|
Control (n = 27) |
Hypothermia (HT) (n = 25) |
ECMO (n = 10) |
P-value* | |
|---|---|---|---|---|
| NGAL (ng/ml) | ||||
| Baseline | 63.85 (4.5 −142) |
929.0 * (290 −1,000) |
358.0* * (164 −592) |
* < 0.0001 |
| ** 0.0007 | ||||
| 48hr | n/a | 577.5* (122 −1,000) |
241.0* * (81– 935) |
* < 0.0001 |
| ** 0.0055 | ||||
| Recovery | n/a | 181.0* (49 – 613) |
37.0* * (21–100) |
* 0.0033 |
| ** 0.9843 | ||||
| FGF (pg/ml) | ||||
| Baseline | 2.1 (1.2 – 6.8) |
10.0* (3.5 – 15.7) |
2.6** (1.8 – 12.1) |
* 0.0095 |
| ** 0.5108 | ||||
| 48hr | n/a | 8.5* (4.5 – 12.6) |
2.5** (0.7 – 7.7) |
* 0.0012 |
| ** 0.8838 | ||||
| Recovery | n/a | 3.6* (0.9 – 8.7) |
2.1* * (0.2 – 3.7) |
* 0.7550 |
| ** 0.2400 | ||||
| EGF (pg/ml) | ||||
| Baseline | 10,768 (5,991–21,906) |
2,141* (1,225 – 4,503) |
5,195** (869 – 12,302) |
* < 0.0001 |
| ** 0.0616 | ||||
| 48hr | n/a | 2,393* (1,515 – 4,377) |
3,789** (2,152 – 4,845) |
* < 0.0001 |
| ** 0.0007 | ||||
| Recovery | n/a | 5,762* (2,911–9,411) | 4,875* * (1,497 – 6,284) |
* 0.0044 |
| ** 0.0016 | ||||
NAGL, Neutrophil Gelatinase-associated Lipocalin; FGF, fibroblast growth factor; EGF, epidural growth factor
Data expressed as median (IQR).
P values (* / ** ) compared to the control group (Mann Whitney test).
Biomarkers levels in healthy controls and newborns treated with HT or ECMO
Compared to controls, both ECMO and HT groups had significantly higher urinary NGAL/UCr values at baseline and 48 hours (Figure 1A). HT infants additionally had higher urinary NGAL/UCr values after recovery (Figure 1A). The urinary levels of FGF-2/UCr were significantly higher in the HT group, compared to controls, both at baseline and 48 hours (Figure 1B). Similar findings were observed when the levels of NGAL and FGF-2 were expressed as their urinary concentration per mL (Table 3). The urinary EGF/UCr levels in the HT group were significantly higher than controls at recovery (Figure 1C). However, these findings were not reproduced when the urinary levels of EGF were expressed as pg/mL of urine. In fact, when the HT and ECMO groups were compared to the control group, the urinary levels of EGF expressed in pg/mL were decreased across all time points (Table 3).
Fig. 1.
Urinary levels of Neutrophil Gelatinase-associated Lipocalin ( NGAL) (A), Fibroblast growth factor-2 (FGF-2 (B), and Epidural Growth Factor (EGF) (C) by group over time. Box and whisker plots show median, interquartile range and values within ±1.5 of interquartile range. Dark gray bars represent Control Group. Light gray bars and white bars represent Hypothermia (HT) and extracorporeal membrane oxygenation (ECMO) groups respectively. Outliers are represented by open circles. Asterisks symbolize significant Mann Whitney U p-values for comparison to control (*p<0.05, **p<0.0001). Dashed line represents control group median for visual comparison.
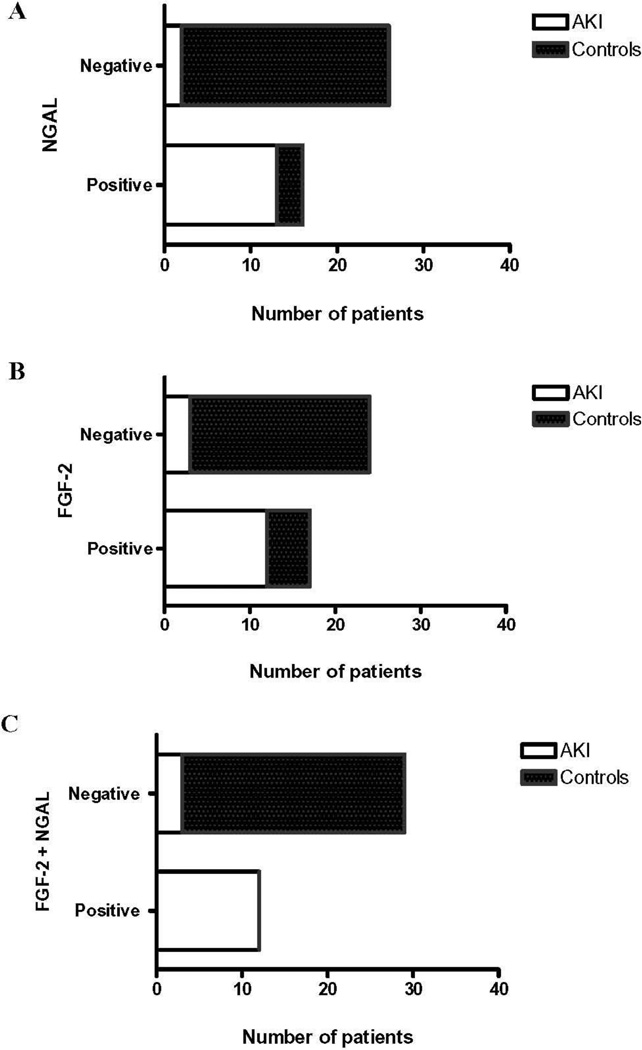
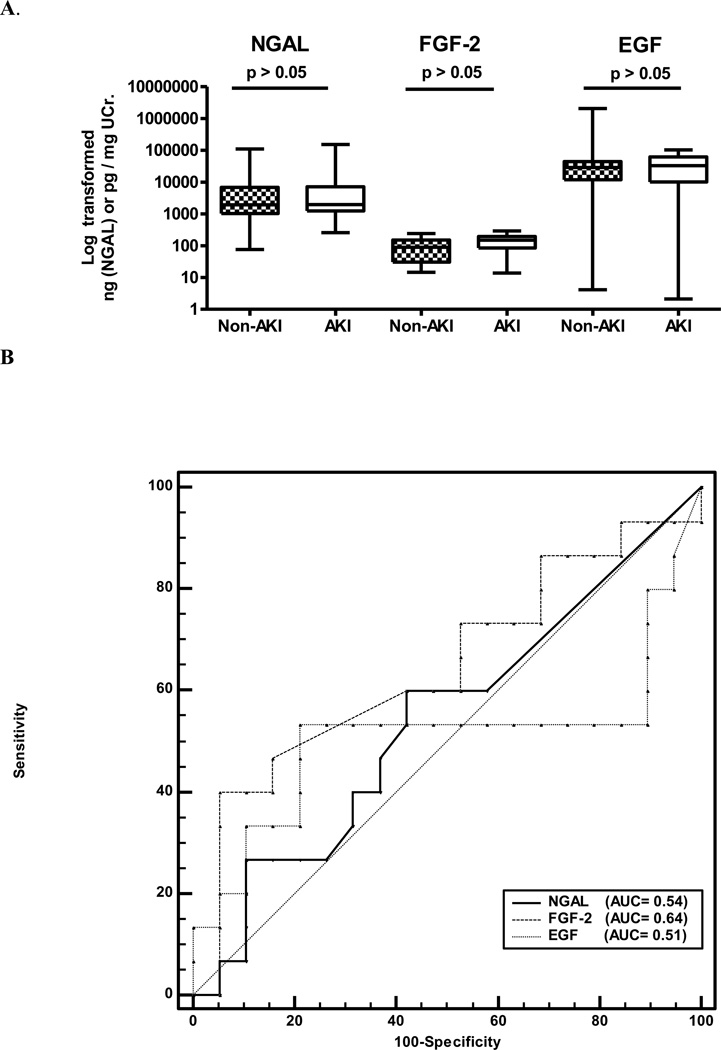
Receiving operating characteristics (ROC) curves were generated to define cut-off values that differentiated at-risk newborns (using baseline levels) from controls. These curves were significant for NGAL and FGF-2 (Figure 2). Cut-off values for the urinary levels of NGAL (> 168 ng/mL) and FGF-2 (> 4 pg/mL) were selected from the coordinates of the ROC curves, to determine their sensitivity, specificity, positive and negative predictive values, as shown in Figure 2. Combining the baseline urinary levels of FGF and NGAL, improved their overall specificity to identify at-risk newborns compared to each biomarker alone (Figure 2). ROC curves generated using NGAL and FGF-2 values expressed as a ratio of the urinary creatinine, also confirmed these findings. A contingency table analysis using cut-off values for NGAL (>1,005 ng/mg UCr) and FGF-2 (>56,20 pg/mg UCr) (Figure 3), showed that NGAL alone had 86 % sensitivity, 88 % specificity, a positive predictive value of 0.81, and a negative predictive value of 0.92 (assuming a 40% prevalence of AKI). FGF-2 alone had 80 % sensitivity, 81% specificity, a positive predictive value of 0.70, and a negative predictive value 0.87. Finally, NGAL and FGF-2 combined, (both values required to be > the cut-off points) showed 80% sensitivity, 100% specificity, a positive predictive value of 1.00, and a negative predictive value of 0.89 (Figure 3). In contrast, the baseline levels of EGF did not differ between at-risk subjects and control newborns, and the ROC curve was not significant (data not shown).
Fig. 2.
Assessment of biomarker utility in predicting acute kidney injury (AKI) in newborns treated with Hypothermia ( HT) or extracorporeal membrane oxygenation (ECMO). Receiver operational characteristic (ROC) curves were generated for Neutrophil Gelatinase-associated Lipocalin (NGAL), fibroblast growth factor-2 (FGF-2), and for both NGAL and FGF-2 combined. The predictive abilities of these biomarkers to detect AKI in these patients were determined using control urine samples collected from healthy newborns, and assuming a 40% prevalence of AKI. The dashed reference line represents a ROC curve for a test with no discriminatory ability. The area under the curve (AUC) for each biomarker is displayed on the graph.
Fig. 3.
The graphs represent the results of contingency tables analyses for Neutrophil Gelatinase-associated Lipocalin (NGAL) alone (A) fibroblast growth factor −2 (FGF-2) alone (B), and both NGAL and FGF-2 combined (C). The predictive abilities of these biomarkers to detect acute kidney injury (AKI) in newborns treated with Hypothermia (HT) or extracorporeal membrane oxygenation (ECMO) were generated using control urine samples collected from healthy newborns, and assuming a 40% prevalence of AKI. The following cut-off values were used at baseline (initiation of therapy: NGAL (1,005 ng/mg UCr) and FGF-2 (56.20 pg/mg UCr).
Biomarker levels in newborns treated with HT or ECMO with and without AKI
AKI occurred in 10 of 35 neonates (43%) treated with HT or ECMO. Ninety five % of these patients (33/35) had their baseline SCr levels measured during the first or second days of life, before the initiation of therapy. The remaining two patients had their baseline SCr levels measured on the 3rd and 4th days of life before treatment. No significant differences in the baseline SCr levels were detected in patients who developed and did not develop AKI (0. 9 ± 0.3 vs. 1.1 ± 0.2 mg/dL, mean ± SD, for AKI vs. Non AKI patients respectively, p>0.05). As expected, the SCr levels at this time point reflected the maternal SCr levels. In contrast, the SCr levels measured when the HT or ECMO treatments were discontinued, were significantly different (0.8 ± 0.4 vs. 0.5 ± 0.3 mg/dL mean ± SD, for AKI vs. Non AKI patients respectively; p < 0.01). As expected, the SCr levels at this time point reflected the renal status of both groups.
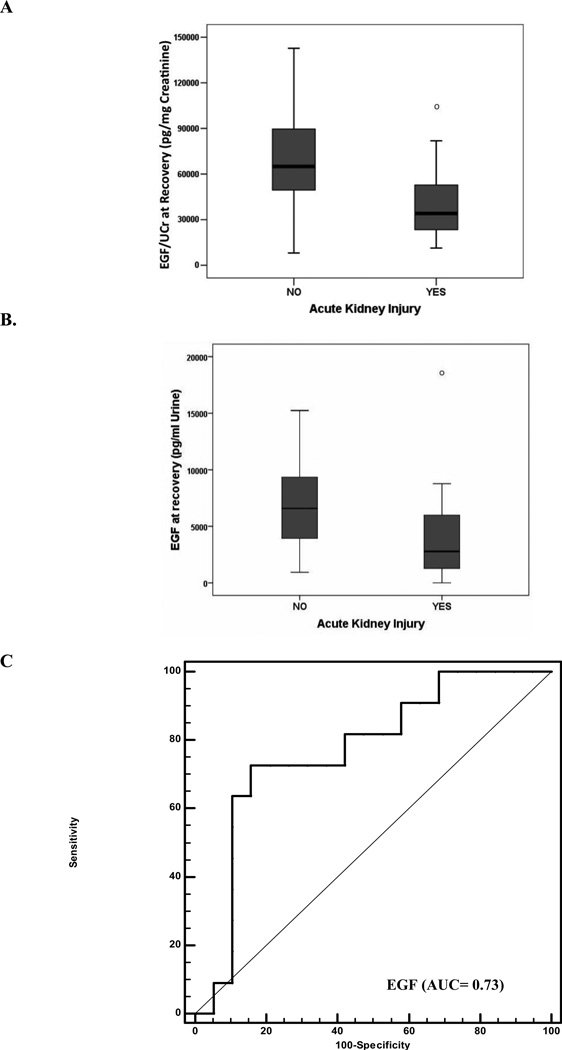
The urinary levels of NGAL and FGF-2, expressed both as a ratio of the urinary creatinine or as a concentration per mL of urine, were elevated, but not significantly different between patients with and without AKI (Figure 4A). Moreover, the ROC curves were not significantly different, and showed poor sensitivity and specificity to identify AKI within the group of newborns treated with HT or ECMO (Figure 4A). In contrast, patients with AKI had significantly lower urinary EGF values at recovery, when compared to those without AKI, and these findings were consistent after expressing the EGF values as a ratio of the UCr or as a concentration per mL of urine (Figure 5A–B). The ROC curve generated for EGF at recovery, to predict failure of eCCL improvement, was significant with an AUC of 0.77 (p= 0.03). EGF at recovery (cut-off < 45,000 pg/mg UCr) predicted AKI with 73% sensitivity, 82% specificity, a positive predictive value of 0.75, and a negative predictive value of 0.82 (assuming a 40% prevalence of AKI). A similar ROC curve and AUC were obtained at recovery using EGF values expressed per mL of urine (Figure 5C). In this case, the urinary EGF cut-off values of < 3,179 pg/mL, had 64% sensitivity, 84% specificity, a positive predictive value of 0.72, and a negative predictive value of 0.78, to identify critically ill children with AKI.
Fig. 4.
Panel A. Box and whisker plots show median and interquantile range log transformed values corresponding to the baseline urinary levels for Neutrophil Gelatinase-associated Lipocalin (NGAL), fibroblast growth factor-2 (FGF-2), and Epidural Growth Factor (EGF), in critically ill newborns with and without acute kidney injury (AKI) (initiation of therapy). Results are expressed in log transformed units corresponding to NGAL (ng/mg UCr) and FGF-2/EGF (pg/mg UCr). Panel B shows receiver operational characteristic (ROC) curves and the area under the curve (AUC) generated for NGAL, FGF-2, and EGE, using urinary values expressed in ng/mL for NGAL and pg/mL for FGF-2 and EGF at the initiation of therapy. The predictive abilities of these biomarkers to detect AKI in newborns treated with Hypothermia (HT) or extracorporeal membrane oxygenation (ECMO) were assessed using control samples collected from newborns who did not develop AKI during the HT and ECMO treatments. The dashed reference line represents a ROC curve for a test with no discriminatory ability. The AUC for EGF is displayed on the graph.
Fig. 5.
The urinary levels of Epidermal Growth Factor (EGF) at recovery are lower in newborns treated with Hypothermia (HT) or extracorporeal membrane oxygenation (ECMO) who developed acute kidney injury (AKI), when compared to those who did not develop AKI. Data represented as both (A) absolute values normalized for urinary creatinine (*p=0.014) and (B) concentration per mL of urine (*p= 0.03). Panel C shows a receiver operational characteristic (ROC) curve and the area under the curve (AUC) for EGF at recovery. Its predictive ability to detect AKI in a group of critically ill newborns treated with HT or ECMO, was assessed using control samples collected from newborns who did not develop AKI during the HT or ECMO treatments (assuming a 40% prevalence of AKI). The dashed reference line represents a ROC curve for a test with no discriminatory ability. The AUC for EGF is displayed on the graph.
Discussion
The current study demonstrates that the urinary levels of NGAL and FGF-2 are elevated in critically ill neonates treated with HT or ECMO when compared to healthy newborns. While the urinary levels of NGAL and FGF-2 combined improved the specificity for the identification of AKI, when using control values derived from healthy newborns, in our study, within the group of critically ill newborns, NGAL/FGF-2 did not identify the patients with AKI. In contrast, the urinary EGF levels post recovery of the acute illnesses, were found to be sensitive and specific to identify ongoing AKI within the group of critically ill newborns. To our knowledge, this is the first study done in critically ill newborns treated with HT or ECMO, demonstrating that the urinary EGF may identify neonates undergoing renal injury while recovering from these treatments.
Of the candidate biomarkers investigated in the current study, NGAL has been studied extensively in neonates [12, 31–33] . Urinary NGAL has shown great promise to detect early AKI in neonates after cardiopulmonary bypass (CPB) [12]. In these patients, the urinary NGAL levels before CPB was started were within the normal range, and a cut-off value of 185 ng/mL identified newborns with AKI [12]. Interestingly, our optimal NGAL cut-off value (> 168 ng/mL) was also sensitive to identify neonates at-risk for AKI from healthy controls. However, we did not confirm that NGAL is further elevated within the subgroup of critically ill neonates with AKI. This may be due to sample size limitations, given the wide variance in NGAL levels in the at-risk newborns, or some infants with subclinical renal injury that were not identified by our defined criteria for AKI. Alternatively, since we have used an exploratory definition of AKI, we can’t exclude the possibility that some patients with mild AKI might have been misclassified. Nevertheless, our findings are consistent with previous studies suggesting that NGAL may be a marker of systemic illness [16, 32], and may have utility as an early sensitive screening marker for newborns at high risk for renal injury [33].
To the best of our knowledge, urinary FGF-2 has not been evaluated as a marker of AKI in neonates. We explored the role of FGF-2 because it is released by injured renal endothelial cells, and unlike NGAL, should provide information regarding the status of renal endothelial cells. In support of this notion, prior studies have demonstrated that FGF-2 may be good candidate urinary biomarker for children with AKI secondary to renal endothelial injury [18, 19, 34]. Here, we found that NGAL and FGF-2 combined, improved the specificity to identify newborns at risk of developing AKI. However, like NGAL, in our study population of critically ill neonates, FGF-2 did not differentiate those with AKI amongst those at-risk. The role of FGF as a marker of systemic illness and/or renal endothelial injury is not fully established by the current study, and further studies are needed to explore this issue.
Finally, EGF showed a promising role as a late biomarker for detecting the recovery of renal function. Previous studies showed that urinary EGF may be a reliable biomarker to follow the outcome of infants with AKI [21–23, 28]. Moreover, the urinary levels of EGF appear to be a predictor of renal function recovery in adults with AKI [27]. Both, EGF and NGAL, are secreted by normal and injured renal tubular epithelial cells. In the context of a critically illness, the urinary excretion of NGAL is affected by changes in its systemic and renal pools [33]. In contrast, the urinary excretion of EGF appears to be more dependent on its renal pool [35–37]. Our findings suggest that EGF may be a more specific biomarker to identify ongoing renal injury in critically ill neonates that are recovering from their respective illnesses.
This study has several limitations. Serial sampling from our control newborns was not feasible. Given evidence that urinary biomarker levels are to some extent influenced by postnatal age and renal growth [21, 31, 35, 36, 38, 39] comparisons between study subjects’ post-recovery levels and control values obtained in the first 48 hours of life must be interpreted with caution. However, we have used cut-off values that are clearly abnormal, even taken into consideration the changes related to postnatal age and renal growth [31, 33, 35, 36, 38, 40, 41]. In addition, our cut-off values are in agreement with those generated in previous larger studies [16, 22, 31, 38–43]. We have also expressed our data both as absolute values corrected for urinary creatinine and as a urinary concentration. The serum levels and tubular secretion of creatinine are changing in patients with AKI, and a rapid decline in the creatinine excretion can affect the urinary biomarker levels. On the other hand, lack of normalization may lead to falsely low levels of the biomarkers in urine samples that are too diluted. Taken into consideration all these issues, we have discussed only the findings that were confirmed by both measurements. In addition, we acknowledge that the use of the Schwartz formula has not been validated in newborns [30]. Thus, in the absence of uniform criteria to define the loss of GFR and/or AKI during the first week of life, our definition of AKI should be considered exploratory, although it was useful to follow the clinical outcome of these patients in the NICU. As discussed above, it is possible that some patients could have been misclassified, in particular those who did not show severe renal failure or reduced urine output. In addition, since the baseline urine samples were collected after the initiation of the HT or ECMO treatments, it could be argued that these treatments per se, may affect the urinary levels and excretion of the selected biomarkers. Nonetheless, it is known that the selected biomarkers are also induced by extra-renal factors, including systemic inflammatory infections, endothelial injury, perinatal asphyxia, liver damage or failure. Thus, they may not be very specific to detect AKI in critically ill neonates under these clinical circumstances. Finally, the small sample size limited our ability to evaluate all potential covariates that could impact the relationship between renal injury and biomarker levels. A larger study will be needed to further establish the role of these candidate urinary biomarkers in the care of critically ill neonates. Long term follow-up post discharge is needed to evaluate if there is a correlation between biomarker data and long-term renal outcomes.
In conclusion, we found that the urinary levels of NGAL and FGF-2 are elevated in critically-ill neonates treated with HT or ECMO when compared to healthy newborns. Urinary NGAL in combination with FGF-2, measured in the first 48 hours of illness, have high sensitivity and improved specificity for identifying newborns at-risk for AKI from healthy controls, and may be useful as an early screening tool. Subsequently, EGF measured during the recovery stage, may identify critically ill newborns with ongoing renal injury. Further studies with longitudinal follow-up are warranted to validate the clinical value of the selected biomarkers in the care of critically-ill neonates treated with HT or ECMO.
Acknowledgements
This study was supported by NIH R0-1 HL-102497 and U54-HD071601.
References
- 1.Gupta BD, Sharma P, Bagla J, Parakh M, Soni JP. Renal failure in asphyxiated neonates. Indian Pediatr. 2005;42:928–934. [PubMed] [Google Scholar]
- 2.Aggarwal A, Kumar P, Chowdhary G, Majumdar S, Narang A. Evaluation of renal functions in asphyxiated newborns. J Trop Pediatr. 2005;51:295–299. doi: 10.1093/tropej/fmi017. [DOI] [PubMed] [Google Scholar]
- 3.Karlowicz MG, Adelman RD. Nonoliguric and oliguric acute renal failure in asphyxiated term neonates. Pediatr Nephrol. 1995;9:718–722. doi: 10.1007/BF00868721. [DOI] [PubMed] [Google Scholar]
- 4.Selewski DT, Jordan BK, Askenazi DJ, Dechert RE, Sarkar S. Acute Kidney Injury in Asphyxiated Newborns Treated with Therapeutic Hypothermia. J Pediatr. 2012 doi: 10.1016/j.jpeds.2012.10.002. pii: S0022–3476(12)01149. [DOI] [PubMed] [Google Scholar]
- 5.Askenazi DJ, Ambalavanan N, Hamilton K, Cutter G, Laney D, Kaslow R, Georgeson K, Barnhart DC, Dimmitt RA. Acute kidney injury and renal replacement therapy independently predict mortality in neonatal and pediatric noncardiac patients on extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2011;12:e1–e6. doi: 10.1097/PCC.0b013e3181d8e348. [DOI] [PubMed] [Google Scholar]
- 6.Mathur NB, Agarwal HS, Maria A. Acute renal failure in neonatal sepsis. Indian J Pediatr. 2006;73:499–502. doi: 10.1007/BF02759894. [DOI] [PubMed] [Google Scholar]
- 7.Agras PI, Tarcan A, Baskin E, Cengiz N, Gurakan B, Saatci U. Acute renal failure in the neonatal period. Ren Fail. 2004;26:305–309. doi: 10.1081/jdi-200026749. [DOI] [PubMed] [Google Scholar]
- 8.Askenazi DJ, Montesanti A, Hunley H, Koralkar R, Pawar P, Shuaib F, Liwo A, Devarajan P, Ambalavanan N. Urine biomarkers predict acute kidney injury and mortality in very low birth weight infants. J Pediatr. 2011;159:907–912. doi: 10.1016/j.jpeds.2011.05.045. e901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaur S, Jain S, Saha A, Chawla D, Parmar VR, Basu S, Kaur J. Evaluation of glomerular and tubular renal function in neonates with birth asphyxia. Ann Trop Paediatr. 2011;31:129–134. doi: 10.1179/146532811X12925735813922. [DOI] [PubMed] [Google Scholar]
- 10.Askenazi DJ, Ambalavanan N, Goldstein SL. Acute kidney injury in critically ill newborns: what do we know? What do we need to learn? Pediatr Nephrol. 2009;24:265–274. doi: 10.1007/s00467-008-1060-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drukker A, Guignard JP. Renal aspects of the term and preterm infant: a selective update. Curr Opin Pediatr. 2002;14:175–182. doi: 10.1097/00008480-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Krawczeski CD, Woo JG, Wang Y, Bennett MR, Ma Q, Devarajan P. Neutrophil gelatinase-associated lipocalin concentrations predict development of acute kidney injury in neonates and children after cardiopulmonary bypass. J Pediatr. 2011;158:1009–1015. doi: 10.1016/j.jpeds.2010.12.057. e1001. [DOI] [PubMed] [Google Scholar]
- 13.Schmidt-Ott KM. Neutrophil gelatinase-associated lipocalin as a biomarker of acute kidney injury--where do we stand today? Nephrol Dial Transplant. 2011;26:762–764. doi: 10.1093/ndt/gfr006. [DOI] [PubMed] [Google Scholar]
- 14.Mishra J, Ma Q, Prada A, Mitsnefes M, Zahedi K, Yang J, Barasch J, Devarajan P. Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. J Am Soc Nephrol. 2003;14:2534–2543. doi: 10.1097/01.asn.0000088027.54400.c6. [DOI] [PubMed] [Google Scholar]
- 15.Mori K, Lee HT, Rapoport D, Drexler IR, Foster K, Yang J, Schmidt-Ott KM, Chen X, Li JY, Weiss S, Mishra J, Cheema FH, Markowitz G, Suganami T, Sawai K, Mukoyama M, Kunis C, D'Agati V, Devarajan P, Barasch J. Endocytic delivery of lipocalin-siderophore-iron complex rescues the kidney from ischemia-reperfusion injury. J Clin Invest. 2005;115:610–621. doi: 10.1172/JCI23056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parravicini E, Nemerofsky SL, Michelson KA, Huynh TK, Sise ME, Bateman DA, Lorenz JM, Barasch JM. Urinary neutrophil gelatinase-associated lipocalin is a promising biomarker for late onset culture-positive sepsis in very low birth weight infants. Pediatr Res. 2010;67:636–640. doi: 10.1203/PDR.0b013e3181da75c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paragas N, Qiu A, Zhang Q, Samstein B, Deng SX, Schmidt-Ott KM, Viltard M, Yu W, Forster CS, Gong G, Liu Y, Kulkarni R, Mori K, Kalandadze A, Ratner AJ, Devarajan P, Landry DW, D'Agati V, Lin CS, Barasch J. The Ngal reporter mouse detects the response of the kidney to injury in real time. Nat Med. 2011;17:216–222. doi: 10.1038/nm.2290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ray P, Acheson D, Chitrakar R, Cnaan A, Gibbs K, Hirschman GH, Christen E, Trachtman H. Basic fibroblast growth factor among children with diarrhea-associated hemolytic uremic syndrome. J Am Soc Nephrol. 2002;13:699–707. doi: 10.1681/ASN.V133699. [DOI] [PubMed] [Google Scholar]
- 19.Ray PE, Liu XH, Xu L, Rakusan T. Basic fibroblast growth factor in HIV-associated hemolytic uremic syndrome. Pediatr Nephrol. 1999;13:586–593. doi: 10.1007/s004670050749. [DOI] [PubMed] [Google Scholar]
- 20.Liu XH, Aigner A, Wellstein A, Ray PE. Up-regulation of a fibroblast growth factor binding protein in children with renal diseases. Kidney Int. 2001;59:1717–1728. doi: 10.1046/j.1523-1755.2001.0590051717.x. [DOI] [PubMed] [Google Scholar]
- 21.Soler-Garcia AA, Rakhmanina NY, Mattison PC, Ray PE. A urinary biomarker profile for children with HIV-associated renal diseases. Kidney Int. 2009;76:207–214. doi: 10.1038/ki.2009.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tsau YK, Sheu JN, Chen CH, Teng RJ, Chen HC. Decreased urinary epidermal growth factor in children with acute renal failure: epidermal growth factor/creatinine ratio not a reliable parameter for urinary epidermal growth factor excretion. Pediatr Res. 1996;39:20–24. doi: 10.1203/00006450-199601000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Chen L, Liu W. Effect of asphyxia on urinary epidermal growth factor levels in newborns. J Tongi Med Univ. 1997;17:144–146. doi: 10.1007/BF02888289. [DOI] [PubMed] [Google Scholar]
- 24.Basile DP. The endothelial cell in ischemic acute kidney injury: implications for acute and chronic function. Kidney Int. 2007;72:151–156. doi: 10.1038/sj.ki.5002312. [DOI] [PubMed] [Google Scholar]
- 25.Kiley SC, Chevalier RL. Urinary biomarkers: the future looks promising. Kidney Int. 2009;76:133–134. doi: 10.1038/ki.2009.124. [DOI] [PubMed] [Google Scholar]
- 26.Grandaliano G, Gesualdo L, Bartoli F, Ranieri E, Monno R, Leggio A, Paradies G, Caldarulo E, Infante B, Schena FP. MCP-1 and EGF renal expression and urine excretion in human congenital obstructive nephropathy. Kidney Int. 2000;58:182–192. doi: 10.1046/j.1523-1755.2000.00153.x. [DOI] [PubMed] [Google Scholar]
- 27.Kwon O, Ahn K, Zhang B, Lockwood T, Dhamija R, Anderson D, Saqib N. Simultaneous monitoring of multiple urinary cytokines may predict renal and patient outcome in ischemic AKI. Ren Fail. 2010;32:699–708. doi: 10.3109/0886022X.2010.486496. [DOI] [PubMed] [Google Scholar]
- 28.Askenazi DJ, Koralkar R, Hundley HE, Montesanti A, Parwar P, Sonjara S, Ambalavanan N. Urine biomarkers predict acute kidney injury in newborns. J Pediatr. 2012;161:270–275. doi: 10.1016/j.jpeds.2012.02.007. e271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, Fanaroff AA, Poole WK, Wright LL, Higgins RD, Finer NN, Carlo WA, Duara S, Oh W, Cotten CM, Stevenson DK, Stoll BJ, Lemons JA, Guillet R, Jobe AH. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med. 2005;353:1574–1584. doi: 10.1056/NEJMcps050929. [DOI] [PubMed] [Google Scholar]
- 30.Schwartz GJ, Feld LG, Langford DJ. A simple estimate of glomerular filtration rate in full-term infants during the first year of life. J Pediatr. 1984;104:849–854. doi: 10.1016/s0022-3476(84)80479-5. [DOI] [PubMed] [Google Scholar]
- 31.Huynh TK, Bateman DA, Parravicini E, Lorenz JM, Nemerofsky SL, Sise ME, Bowman TM, Polesana E, Barasch JM. Reference values of urinary neutrophil gelatinase-associated lipocalin in very low birth weight infants. Pediatr Res. 2009;66:528–532. doi: 10.1203/PDR.0b013e3181baa3dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lavery AP, Meinzen-Derr JK, Anderson E, Ma Q, Bennett MR, Devarajan P, Schibler KR. Urinary NGAL in premature infants. Pediatr Res. 2008;64:423–428. doi: 10.1203/PDR.0b013e318181b3b2. [DOI] [PubMed] [Google Scholar]
- 33.Parravicini E. The clinical utility of urinary neutrophil gelatinase-associated lipocalin in the neonatal ICU. Curr Opin Pediatr. 2010;22:146–150. doi: 10.1097/MOP.0b013e3283369e78. [DOI] [PubMed] [Google Scholar]
- 34.Ray PE, Tassi E, Liu XH, Wellstein A. Role of fibroblast growth factor-binding protein in the pathogenesis of HIV-associated hemolytic uremic syndrome. Am J Physiol Regul Integr Comp Physiol. 2006;290:R105–R113. doi: 10.1152/ajpregu.00492.2005. [DOI] [PubMed] [Google Scholar]
- 35.Watanabe K, Ono A, Hirata Y, Fukuda Y, Kojima T, Kobayashi Y. Maturational changes and origin of urinary human epidermal growth factor in the neonatal period. Biol Neonate. 1989;56:241–245. doi: 10.1159/000243129. [DOI] [PubMed] [Google Scholar]
- 36.Evans NJ, Rutter N, Gregory H. Urinary excretion of epidermal growth factor in the newborn. Early Hum Dev. 1986;14:277–282. doi: 10.1016/0378-3782(86)90190-8. [DOI] [PubMed] [Google Scholar]
- 37.Di Paolo S, Gesualdo L, Stallone G, Ranieri E, Schena FP. Renal expression and urinary concentration of EGF and IL-6 in acutely dysfunctioning kidney transplanted patients. Nephrol Dial Transplant. 1997;12:2687–2693. doi: 10.1093/ndt/12.12.2687. [DOI] [PubMed] [Google Scholar]
- 38.Mattila AL, Perheentupa J, Pesonen K, Viinikka L. Epidermal growth factor in human urine from birth to puberty. J Clin Endocrinol Metab. 1985;61:997–1000. doi: 10.1210/jcem-61-5-997. [DOI] [PubMed] [Google Scholar]
- 39.Bagli DJ, Van Savage JG, Khoury AE, Carr M, McLorie GA. Basic fibroblast growth factor in the urine of children with voiding pathology. J Urol. 1997;158:1123–1127. doi: 10.1097/00005392-199709000-00110. [DOI] [PubMed] [Google Scholar]
- 40.Scott SM, Guardian CM, Angelus P, Backstrom C. Developmental pattern of urinary epidermal growth factor in the premature infant and the influence of gender. J Clin Endocrinol Metab. 1991;72:588–593. doi: 10.1210/jcem-72-3-588. [DOI] [PubMed] [Google Scholar]
- 41.Marler JJ, Fishman SJ, Kilroy SM, Fang J, Upton J, Mulliken JB, Burrows PE, Zurakowski D, Folkman J, Moses MA. Increased expression of urinary matrix metalloproteinases parallels the extent and activity of vascular anomalies. Pediatrics. 2005;116:38–45. doi: 10.1542/peds.2004-1518. [DOI] [PubMed] [Google Scholar]
- 42.Kaplan F, Sawyer J, Connors S, Keough K, Shore E, Gannon F, Glaser D, Rocke D, Zasloff M, Folkman J. Urinary basic fibroblast growth factor. A biochemical marker for preosseous fibroproliferative lesions in patients with fibrodysplasia ossificans progressiva. Clin Orthop Relat Res. 1998;346:59–65. [PubMed] [Google Scholar]
- 43.Gupta GK, Milner L, Linshaw MA, McCauley RG, Connors S, Folkman J, Bianchi DW. Urinary basic fibroblast growth factor: a noninvasive marker of progressive cystic renal disease in a child. Am J Med Genet. 2000;93:132–135. doi: 10.1002/1096-8628(20000717)93:2<132::aid-ajmg10>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]