Abstract
Background
Together, community-based participatory research (CBPR), usercentered design (UCD) and health information technology (HIT) offer promising approaches to improve health disparities in low-resource settings.
Objectives
This article describes the application of CBPR and UCD principles to the development of iDecide/Decido, an interactive, tailored, web-based diabetes medication education and decision support tool delivered by community health workers (CHWs) to African-American and Latino participants with diabetes in Southwest and Eastside Detroit. The decision aid is offered in English or Spanish and is delivered on an iPad in participants’ homes.
Methods
The overlapping principles of CBPR and UCD used to develop iDecide/Decido include: a user-focused or community approach; equitable academic and community partnership in all study phases; an iterative development process that relies on input from all stakeholders; and a program experience that is specified, adapted, and implemented with the target community.
Results
Collaboration between community members, researchers, and developers is especially evident in the program’s design concept, animations, pictographs, issue cards, goal setting, tailoring, and additional CHW tools.
Conclusions
Applying the principles of CBPR and UCD can be successfully employed in developing health information tools that are easy to use and understand, interactive, and target health disparities.
Keywords: Community-based participatory research, health information technology, user-centered design, decision aid, community health worker, health disparities, diabetes
Introduction
African American and Latino adults with diabetes experience a 50-100% higher burden of illness and mortality from diabetes,1 have worse glycemic control,2-7 and experience more barriers to diabetes self-management than non-Latino white adults.8 Successful medication management, a critical component of diabetes treatment, requires a partnership between providers who initiate and titrate effective medications and patients who adhere to the agreed-upon regimen. However, multiple factors can adversely influence medication decision-making, leading to failure to intensify medications and high rates of poor medication adherence,9-11 often leading to disease progression, premature disability, and death.12 Barriers to adherence, including side effects, lack of understanding of and trust in treatments, and regimen complexity are often not identified or addressed.13 Poorer medication adherence partially explains higher rates of poor glycemic and blood pressure control in Latino and African American adults with diabetes.8,14 Further, when adherent patients have poor control, clinicians often do not intensify medication regimens, with even lower rates of intensification among ethnic/racial minority patients.9,14-16
Providing adequate information to patients about potential benefits and costs of medications and discussing treatment preferences are essential for improved adherence and timely medication initiation or intensification.17 However, these conversations can be time-consuming for clinic visits.18 This is especially challenging among low-income racial and ethnic minority adults living in under-resourced communities.19
Health information technology (HIT) can greatly improve health communication and the quality of healthcare (for example, electronic medical records, telemedicine, computerized decision aids) while addressing many of the root causes for disparities, such as language and literacy barriers, fragmented healthcare services, and lack of understanding of culture, beliefs, and medical preferences.20 For example, over 80% of Internet users have searched for health information.21 However, access to this information may not be shared equally across all segments of the population. Low-income, older Hispanic and African Americans with chronic illnesses are less likely to use the Internet than other groups.20
Given these challenges, how can HIT and the Internet narrow health disparities? Community-based participatory research (CBPR) and user-centered design (UCD) offer promising approaches.
CBPR is a partnership approach that equitably involves community and academic partners in all phases of a research process.22 Applying CBPR principles to health interventions enhances the recruitment and retention of study participants, the appropriateness of intervention strategies, and the quality and validity of data.23,24 CBPR can be used effectively to develop iteratively-designed, high-tech web-based interventions with a tested user interface because it involves the generation of ideas and feedback from intended users throughout the research process.22-25,32-34
Along with CBPR, UCD helps ensure that a community-based program is easy to use and meets the needs of the users.29,30 UCD “involves end-users throughout the development process so that technology supports tasks, [is] easy to operate, and [is] of value to users.”31 Utilizing the principles of CBPR and UCD may increase the efficacy of HIT by ensuring that tools are culturally appropriate, beneficial to the users, and easy to use and understand.
To our knowledge, a CBPR approach has been applied in a limited number of studies addressing the development of HIT tools for underserved populations.35-37 We describe here the application of CBPR and UCD principles to the development of a health information tool called iDecide/Decido - an interactive, personally tailored web-based diabetes education and decision support tool for underserved African American and Latino adults with poorly controlled diabetes in Detroit, Michigan.
Methods
The Institutional Review Boards of the participating sites approved all aspects of this study.
Principles of Community-based participatory research and User-centered design
The iDecide/Decido decision aid was developed using the principles of CBPR and UCD.
CBPR, by involving stakeholders in all stages, contributes to the development of culturally appropriate measurement instruments and establishes a mutual trust that enhances data collection and makes projects more effective.38 As with many CBPR-driven projects, the research team chose to include Community Health Workers (CHWs). CHW-led interventions have been shown to improve diabetes self-management.25-27 CHWs also reach populations with limited access to health information.28 One goal of iDecide/Decido is to increase the impact of CHW educational outreach by offering a tool that CHWs can use to present evidence-based, culturally-sensitive information tailored to patients’ needs and health literacy.
UCD is an approach to designing computer systems and software applications that focuses on the user’s needs, wants, and abilities. This focus produces a tool that is intuitive and useful to target users.29,30 Both CBPR and UCD focus on enhancing the development of research systems by involving stakeholders throughout the development process thus increasing accuracy, cultural appropriateness, and relevance of intervention approaches and tools.39
Overlap of the principles of CBPR and UCD are evident in the development of the iDecide/Decido decision aid (Table 1).30,32 Overlapping principles include: a community/user-focused approach; equitable academic and community partnership; an iterative development process with input from all stakeholders; and a program experience that is specified, adapted, and implemented with the target community.30
Table 1.
Intersections of UCD and CBPR Principles in iDecide/Decido Development
| Common Theme | UCD | CBPR |
|---|---|---|
| Community Centered |
|
|
| Partnership in all Phases |
|
|
| Iterative Development |
|
|
| Program Experience |
|
|
These principles led to multiple iterations based on feedback from all partners including CHWs, which was essential to producing a tool that was easy to use and culturally appropriate. Input from all stakeholders assured that the program addressed the needs of the community, and that the interface and program designs were culturally sensitive, appealing, and appropriate for all levels of literacy and numeracy.
The iDecide/Decido program offers:
Information on the pathology and complications of diabetes,
Description of mechanisms of action of participants’ current medications
Opportunities to learn about and discuss other treatments
Discussion of strategies to address medication adherence barriers
Goal setting for therapy and diabetes management
English and Spanish versions were developed by a multi-disciplinary team including content experts, web developers, graphic designers, CHWs, UM researchers and members of Detroit REACH.
Research Partners and their Responsibilities
Decision-making in CBPR projects is sometimes characterized as slow.22,32 Having multiple stakeholders also complicates decision-making and reduces the clarity of feedback.32-34 Therefore, building on existing relationships and having a clear plan for communication was particularly important to the research team.
Building on established relationships facilitates research processes and collaborations.22,32,40 A long-standing relationship exists between University of Michigan (UM) researchers and the REACH Detroit Partnership, which is comprised of community, health system, and academic partners. The Community Health and Social Services (CHASS) Center, Inc., a community partner of REACH, is a federally qualified healthcare center in Detroit. All four CHWs that participated in this project are employees at CHASS. The REACH Detroit Partnership has developed and tested ongoing CHW-led diabetes self-management programs that have significantly improved diabetes clinical outcomes in southwest and eastside Detroit.27,41 Other stakeholders in the development of the tool included researchers at the University of Michigan with expertise in science and experimental design and researchers from the Center for Health Communications Research (CHCR). The CHCR team contributed expertise in health communications and technology.
Design Process
To facilitate partnership, collaboration, and speedy decision-making, weekly meetings were conducted with the multidisciplinary design team. Additional weekly meetings were held with the academic and community researchers; and monthly meetings were conducted with all partners. Content developers delivered program content to investigators and CHWs to review, beginning with the baseline survey, which CHWs helped ensure was culturally appropriate.
It is often difficult for even the most experienced researchers to imagine how a content outline and rough design sketches will become a program. To help everyone visualize the program in its early stages, the development team built rough approximations of how the content would be laid out (called wireframes) in power point and designed flow charts that mimicked the proposed program navigation. Revisions of all content were discussed at weekly meetings and changes were integrated according to group consensus, based on input from all partners.
CHWs reviewed and revised all content drafts. The content, written at an eighth grade reading level, was based on motivational interviewing and used principles of plain language.42-45 This included open-ended questions and change talk elicitation to help participants uncover motivation and address barriers.46
Web developers ensured optimal site functionality by delivering multiple iterations of working software to team members for review and testing. Web developers built flexible program pathways, allowing participants to interact with the content most relevant to them, in their preferred order. There are a limited number of studies that have been published up to date, which incorporate the use of iPads in health-based interventions.47-51 Therefore, an additional technological task was to make the intervention compatible and easy to use on an iPad.
Additional Testing
Focus groups evaluated the interface, ease of use, and comprehensibility of the tool. Participants were peer mentors recruited from the “PEERs” program at CHASS.52-54 “PEERs” are African American or Latino community members with diabetes who have been trained to discuss diabetes with other diabetic CHASS patients. The numeracy and literacy levels of PEERs members are comparable to that of the rest of the CHASS population. Five out of six “PEERs” were able to attend. Participants spent 20-40 minutes going through the Introduction and Issue Cards sections of the program with a CHW. Then, through facilitated group discussion, participants gave feedback on the program, including perceived ease of use and their experience using the iPad. Participants were consented and received $20 in appreciation.
Most participants reported feeling confident using the program. They felt the program was individualized to their needs and would help them discuss treatment options with their doctors. All participants would recommend the program to friends. CHWs also provided feedback as part of testing, since they are program users as well.
Tailoring
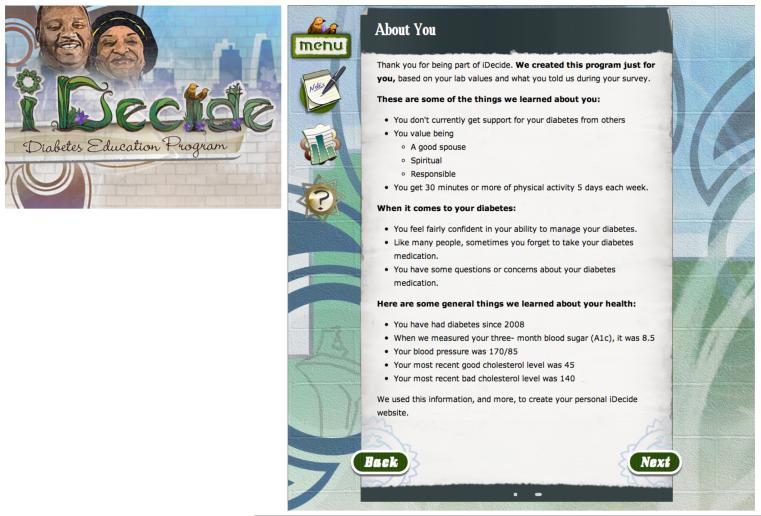
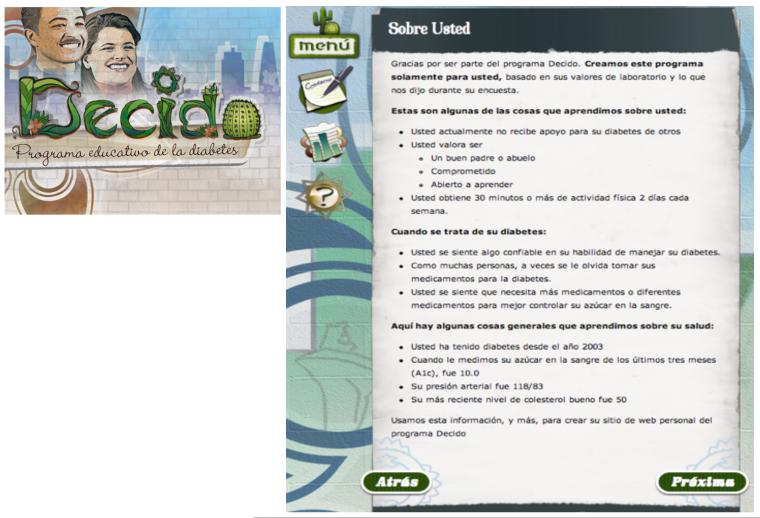
Tailoring was used extensively throughout the program. Tailored programs are directly relevant to a single person based on the characteristics derived from an individual assessment.55 Some of the key tailoring variables in the iDecide/Decido tool are lab values, medications, health insurance status, personal values, and medication adherence barriers. For example, the introduction to the program discusses each participant’s reported personal values, social support, eating habits, confidence and barriers in managing diabetes, year of diabetes diagnosis, and most recent A1c and blood pressure values (Figure 1 and Figure 2). CHWs and CHASS staff worked with content developers to revise tailored content, ensuring that the program was relevant to the target communities. Revisions included the use of common language around diabetes, for example, using the term “high sugar” instead of “high blood sugar”; what questions to ask in goal setting; and which prompts to include for discussion. Tailored content was created in the Michigan Tailoring System (MTS) software, developed by CHCR.56 The tailored content that is incorporated throughout the program aims to facilitate a deeper, more personal discussion between the participants and CHWs regarding their diabetes therapy and goals.
Figure 1.
African American, English Speaking Logo Design
Figure 2.
Latino, Spanish Speaking Logo Design
Results
The resulting product, iDecide/Decido, allows participants to set personal treatment goals, identify treatment preferences and concerns, and understand treatment options for improving their glycemic control. iDecide/Decido is delivered in either English or Spanish to patients on an iPad in their own homes by CHWs. The program is structured as follows:
CHW introduces him/herself, the program, and how to use the iPad
CHW – participant dyad discusses what diabetes is, reviews the participant’s lab values, examines risk of complications
The dyad reviews the participant’s medications, including adherence concerns
Together, the CHW and participant choose whether to discuss changing/adding a medication, taking a higher dose of existing medication, or setting goals to improve adherence
The participant sets goals and receives a printed summary.
The first portion of the program is meant to be linear, however CHWs can access any section at any time, based on the needs of the conversation.
Several program components highlight the benefits of the marriage of UCD and CBPR. These components are summarized in Table 2, and are comprised of: a tailored design concept, animations, pictographs, issue cards, goal setting, tailoring, and additional CHW tools.
Table 2.
Description of Program Components and Functions
| Program Component |
Description | Functions |
|---|---|---|
| Design concept |
A unifying theme across all program features, including:
|
A professional, approachable design helps:
|
| Animations | Three metaphorical cartoons showing:
|
Animations:
|
| Risk pictographs |
Participants can see their own risk, based on their A1c, and also see how risk changes as A1c changes for:
|
Help participant understand the relationship between A1c values and 10-year risk for developing co-morbid complications. |
| Issue cards57 |
Participants identify the 2 issues that are most important to them and see how each class performs. The issues are:
|
Help participant choose a medication class or classes that may work for them. |
| Goal setting | Participants can set goals around:
Goal Setting Sections
|
Goal setting is an important component of Motivational Interviewing. Identifying goals can facilitate participant to build an action plan toward behavior change.44,45 |
| Additional CHW tools |
CHWs identified tools they felt would enhance meaningful interactions with participants. CHW tools include:
|
Working with CHWs to build the tools they need not only improves the program experience for the participant, but also promotes partnership between CHWs and the development team. |
Design Concept
Tailored design provides a unifying theme throughout the program. The design focuses on Detroit’s Latino and African American populations. The logos were inspired by images from previous Detroit REACH curricula, which are highly recognizable to the African-American and Latino populations that they serve. Additionally, CHWs provided photographs of several building murals in Detroit that represent hope and family for inspiration. Two logos were created - African-American and Latino versions. The African-American logo incorporates an African-American couple and two sparrows, which was inspired from a gospel song about overcoming challenges through spiritual faith. The Latino logo includes a Latino couple and a cactus, representing courage and strength through time. CHWs played a significant role in the iterations and the final design of the logos (Figure 1 and Figure 2).
Animations
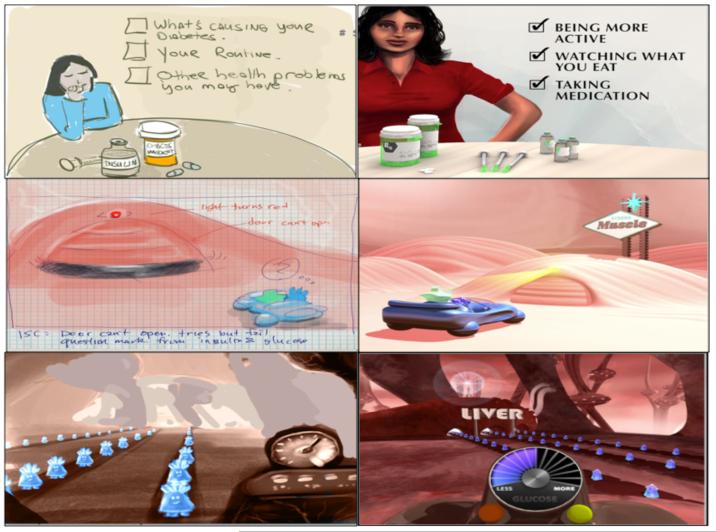
To assist low literacy individuals, three animations were created to explain: what diabetes is, blood sugar, why treatment matters, how treatment works. Animations were developed iteratively and reviewed by all team members. Input and discussion were critical in finalizing an animation concept early on, preventing expensive lost time from late animation modifications. Voice-overs for animations were recorded in English and Spanish. CHWs worked with CHCR researchers in voice over recordings of animations in order to ensure appropriate pronunciation and word choice in recordings. The team used the following process to produce the animations:
Concept - Content developers created concepts that were presented to team members. Team members chose a concept then refined it based on acceptability to community participants.
Animation scripts- Content developers wrote animation scripts containing visual and spoken components. All team members reviewed all drafts.
Character development- Designers created characters that were reviewed and approved by team members (Figure 3).
Storyboards- Designers and content developers created storyboards which were reviewed by all team members. (Figure 4).
Animations- Designers created animations using 3D imaging and modeling (Figure 5).
Figure 3.
Glucose and Insulin Characters
Figure 4.
Storyboard illustrations and animations
Figure 5.
Animations 1 and 2 Web Page
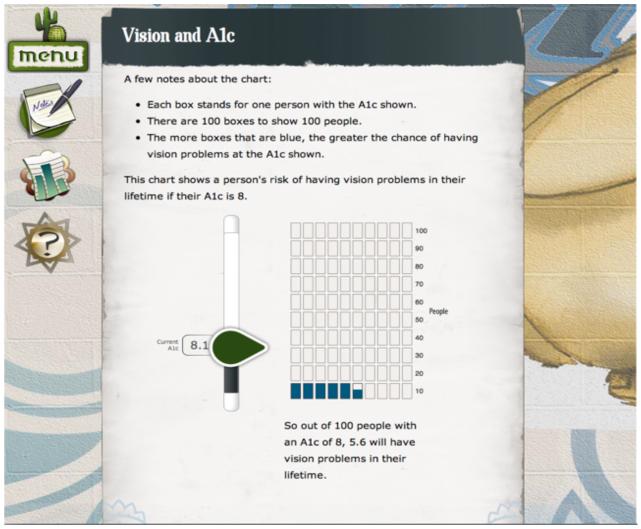
Risk Pictographs
Interactive risk pictographs were created to show risks of complications associated with diabetes. These pictographs were based on the UK Prospective Diabetes Study risk engine.11 Participants could dynamically model how changes in their own A1c influence 10- year risk for kidney disease, vision loss, and amputation by adjusting A1c. Initially, CHWs expressed discomfort with the pictographs. They feared participants would not understand what the pictographs were conveying. As a result, the team added a dynamically updated, written explanation of the pictograph (Figure 6).
Figure 6.
Vision and A1c Risk Pictograph
Issue Cards
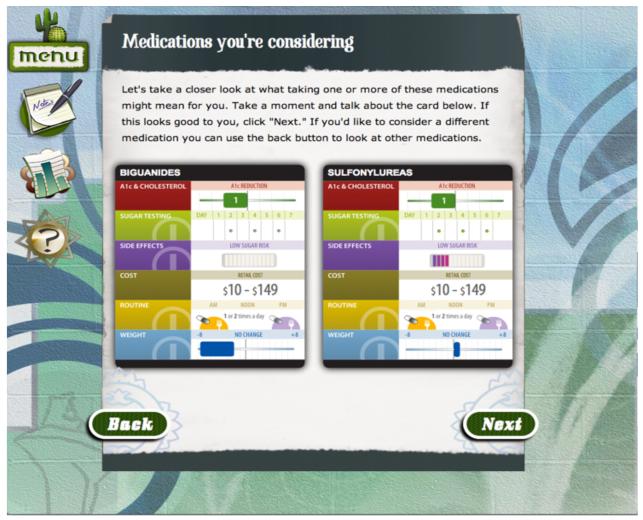
One of the primary goals of iDecide/Decido is to improve participant satisfaction with diabetes medication. To this end, the team built on existing work from Montori et. al. So-called “issue cards” have been previously clinically used as a medication choice decision aid for patients with type 2 diabetes.57 These cards were shown to improve patient involvement in making decisions about diabetes medications and their satisfaction with medication information.58 The iDecide/Decido team developed an interactive, electronic version of the issue cards focusing on costs, side effects, weight changes, dosing and testing schedules, and effects on cholesterol/A1c levels for each class of diabetes medications. Cost is tailored on insurance coverage, showing CHASS, Medicaid, or retail costs. Participants tap the card showing their most important issue and discuss the card with the CHW. Based on that discussion, the participant chooses one or more medication classes that might work for them. Then, the participant chooses a second card. Participants and CHWs compare the content of the two cards side by side. Finally, participants choose the classes of diabetes medications that they might want to discuss with their healthcare provider. After the exercise, participants see a summary card for each selected medication class. All team members gave considerable feedback on the look, content, and functionality of the issue cards (Figure 7).
Figure 7.
Issue cards
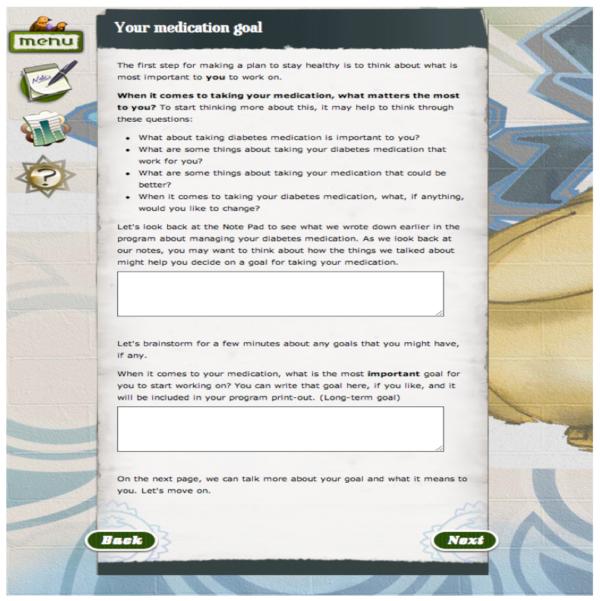
Goal Setting
Action planning and follow-up, two key components of motivational interviewing, were included to encourage conversation about how the patient’s behavior supports or conflicts with their values and to support patients in making therapeutic goals.46 Participants report values and barriers to treatment options, decision-making, lifestyle issues and disease perceptions at baseline. During the program, participants can set medication and lifestyle goals to support conversations with doctors about treatment options, to help improve or maintain medication adherence, and to encourage lifestyle modifications. Participants report how important their goals are and receive tailored feedback. Finally, participants develop an action plan with their CHW. Content developers made modifications based on CHW feedback about goal setting. Goals can be set around medications, physical activity, and healthful eating (Figure 8).
Figure 8.
Medication Goal Setting Web Page
Additional CHW Tools
Several program features were added to the program in response to CHW feedback. Low-literacy, low-numeracy, and poor adherence symbols were discreetly integrated into the site design to alert CHWs to potential sensitivities. CHWs requested a way to keep notes during the conversation. In response, graphic and web developers created a notepad feature, which allowed CHWs to record additional information during the conversation. The notepad page can be printed at the end of the encounter.
Based on CHW recommendations, a list of each participant’s current medications is available for reference during the interaction. Additionally, a medication glossary was included, showing the brand and generic names of all diabetes medications with phonetic pronunciations. These features were implemented based on CHW feedback.
Discussion
The iDecide/Decido program is the first CHW-mediated, iPad-delivered health intervention that integrates research and design methods of CBPR and UCD. Providing communities with health information can be empowering and lead to improved health outcomes. Rapidly advancing technology does not have to lead to wider gaps in health disparities. As we have demonstrated, HIT can be developed not only for specific communities, but by them as well. Processes that solicit and engage users can only increase the effectiveness of the program by delivering information that is relevant and welcomed by community members, thereby promoting positive health outcomes.
In our development process we overcame many challenges associated with CBPR, including inequitable distribution of power and control, and conflicts associated with differences in perspective, priorities, assumptions, values, beliefs, and language.32 We achieved this by ensuring that every decision was brought before the whole team. All opinions were considered and changes were made with consensus of all team members. Regular meetings also fostered relationships amongst the team and aided in clear communication. One strength of the program is the degree to which cultural values and beliefs were incorporated, mainly with the help of CHWs. Language was also a vital component of cultural competence in the program as the English version was translated to Spanish by Spanish-speaking team members and reviewed by Spanish-speaking CHWs to ensure appropriateness for the population.
This decision aid helps bridge the gap in the digital divide in several ways. First, because the program is offered by CHWs on an iPad in participants’ home, individuals who may not have access to computers or web-based tools can interact with a sophisticated multi-media tool. The CHW shows the participant how to use the iPad at the beginning of the session, and participants are able to navigate the iPad as much or as little as they would like during the interaction. Second, CHWs are trained to assist when needed, helping ensure the participant’s comfort. CHWs have extensive experience using the tool and offer guidance in appropriate, sensitive ways which may be more effective than participants using the program alone or with academic researchers. Lastly, the program was created specifically for the African American and Latino communities in Detroit. Program components are individually and culturally tailored to ensure salience, relatedness, sensitivity, and comprehensibility. All of these program characteristics contribute to enhancing the experience for participants. If this tool is found to be effective, we hope to disseminate it to other low-income health centers that use community health workers and other lay workers.
Limitations
There were, however, some challenges in our development process. CBPR can require a slower process. Because of the number of stakeholders, varying availabilities, and desire to ensure equality of participation in the research and development process, it took time to gather feedback, reach consensus on changes, and incorporate feedback. To tackle this, team members made content review a priority in their weekly meetings held in Detroit. Content reviewers did however, find the tailored content difficult to decipher and edit. Rather than reading like a story, tailored content is shown with every possible version of a sentence, in a linear fashion. This poses difficulties visualizing tailored content as it will appear in a web-based program for one participant.
Time constraints also made it difficult for the program to be tested by CHWs earlier in the timeline. For example, wishes for program content or functionality sometimes conflicted with what was possible technologically. We tried to minimize communication barriers through regular interactions and involvement with team members. Finally, we were concerned with the comfort level of participants when using the iPads. To address this concern, we conducted focus groups to get feedback from CHWs and focus group participants.
In conclusion, we found that an integrated methods approach to CBPR facilitated the development of a high-tech, tailored, iPad-delivered diabetes education and decision tool. It is our hypothesis that this program can serve as a model for ameliorating some challenges of developing electronically rendered interventions when conducting CBPR. We are now examining whether this tool improves Latino and African American diabetes patients’ knowledge and satisfaction, reduces decisional conflict, and improves medication decision-making, adherence, and glycemic control through a two-group randomized trial.
Acknowledgements
This research was supported by a grant from the Agency for Healthcare Research and Quality (NCT01427660). We thank the CHASS/REACH Detroit Partnership staff and the REACH Detroit Partnership Steering Committee. The CHASS/REACH Detroit Partnership is affiliated with the Detroit Community-Academic Urban Research Center. We also thank the Center for Health Communications Research staff and University of Michigan researchers.
References
- 1.National Institute of Diabetes and Digestive and Kidney Diseases National Diabetes Statistics fact sheet: General information and national estimates on diabetes in the United States, 2007. 2008 http://www.niddk.nih.gov/welcome/release/8_8_01.htm.
- 2.Harris MI, Eastman RC, Cowie CC, Flegal KM, Eberhardt MS. Racial and ethnic differences in glycemic control of adults with type 2 diabetes. Diabetes Care. 1999;22(3):403–408. doi: 10.2337/diacare.22.3.403. [DOI] [PubMed] [Google Scholar]
- 3.Karter AJ, Ferrara A, Liu JY, Moffet HH, Ackerson LM, Selby JV. Ethnic Disparities in Diabetic Complications in an Insured Population. JAMA. 2002;287(19):2519–2527. doi: 10.1001/jama.287.19.2519. [DOI] [PubMed] [Google Scholar]
- 4.Saaddine JB, Cadwell B, Gregg EW, et al. Improvements in diabetes processes of care and intermediate outcomes: United States, 1988-2002. Ann Intern Med. 2006 Apr 4;144(7):465–474. doi: 10.7326/0003-4819-144-7-200604040-00005. [DOI] [PubMed] [Google Scholar]
- 5.Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA. 2004;291(3):335–342. doi: 10.1001/jama.291.3.335. [DOI] [PubMed] [Google Scholar]
- 6.Lasater LM, Davidson AJ, Steiner JF, Mehler PS. Glycemic control in English- vs Spanish-speaking Hispanic patients with type 2 diabetes mellitus. Arch Intern Med. 2001 Jan;Aug;161(1):77–82. doi: 10.1001/archinte.161.1.77. [DOI] [PubMed] [Google Scholar]
- 7.The CDC Diabetes Cost-effectiveness Group Cost-effectiveness of intensive glycemic control, intensified hypertension control, and serum cholesterol level reduction for type 2 diabetes. JAMA. 2002;287(19):2542–2551. doi: 10.1001/jama.287.19.2542. [DOI] [PubMed] [Google Scholar]
- 8.Heisler M, Faul JD, Hayward R, Langa K, Blaum CS, Weir D. Mechanisms for Racial and Ethnic Disparities in Glycemic Control in Middle-Aged and Older Americans in the Health and Retirement Study. Arch Intern Med. 2007;167(17):1–8. doi: 10.1001/archinte.167.17.1853. [DOI] [PubMed] [Google Scholar]
- 9.Hoerger TJ, Segel JE, Gregg EW, Saaddine JB. Is glycemic control improving in U.S. adults? Diabetes Care. 2008 Jan;31(1):81–86. doi: 10.2337/dc07-1572. [DOI] [PubMed] [Google Scholar]
- 10.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of Medicare coverage. Ann Intern Med. 2009 Apr 21;150(8):505–515. doi: 10.7326/0003-4819-150-8-200904210-00005. [DOI] [PubMed] [Google Scholar]
- 11.UKPDS Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):837–853. [PubMed] [Google Scholar]
- 12.Vijan S, Hofer TP, Hayward RA. Estimated benefits of glycemic control in microvascular complications in type 2 diabetes. Ann Intern Med. 1997;127(9):788–795. doi: 10.7326/0003-4819-127-9-199711010-00003. [DOI] [PubMed] [Google Scholar]
- 13.Zhang P, Engelgau MM, Norris SL, Gregg EW, Narayan KM. Application of economic analysis to diabetes and diabetes care. Ann Intern Med. 2004;140(11):972–977. doi: 10.7326/0003-4819-140-11-200406010-00039. [DOI] [PubMed] [Google Scholar]
- 14.Grant RW, Buse JB, Meigs JB. Quality of diabetes care in U.S. academic medical centers: low rates of medical regimen change. Diabetes Care. 2005;28(2):337–442. doi: 10.2337/diacare.28.2.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 16.Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135(9):825–834. doi: 10.7326/0003-4819-135-9-200111060-00012. [DOI] [PubMed] [Google Scholar]
- 17.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of Medication Adherence on Hospitalization Risk and Healthcare Cost. Medical Care. 2005;43(6):521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 18.Rubin RR. Adherence to pharmacologic therapy in patients with type 2 diabetes mellitus. Am J Med. 2005 May;118(Suppl 5A):27S–34S. doi: 10.1016/j.amjmed.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 19.Huang ES, Brown SE, Ewigman BG, Foley EC, Meltzer DO. Patient perceptions of quality of life with diabetes-related complications and treatments. Diabetes Care. 2007 Oct;30(10):2478–2483. doi: 10.2337/dc07-0499.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lopez L, Green AR, Tan-McGrory A, King R, Betancourt JR. Bridging the Digital Divide in Health Care: The Role of Health Information Technology in Addressing Racial and Ethnic Disparities. Jt Comm J Qual Patient Saf. 2011;37(10):437–445. doi: 10.1016/s1553-7250(11)37055-9. [DOI] [PubMed] [Google Scholar]
- 21.Fox S. The Social Life of Health Information. Pew Internet & American Life Project. 2011 Retrieved from http://www.pewinternet.org. [Google Scholar]
- 22.Israel BA, Eng E, Schulz AJ, Parker EA, Satcher D, editors. Introduction: Methods in community-based participatory research for health. Jossey-Bass; San Francisco, CA: 2005. pp. 3–26. [Google Scholar]
- 23.Parker EA, Israel BA, Williams M, Brakefield-Caldwell W, Lewis TC, Robins T, Ramirez E, Rowe Z, Keeler G. Community Action Against Asthma: Examining the Partnership Process of a Community-based Participatory Research Project. J Gen Intern Med. 2003;18:558–567. doi: 10.1046/j.1525-1497.2003.20322.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parker EA, Israel BA, Robins TG, Mentz G, Lin X, Brakefiled-Caldwell W, Ramirez E, Edgren KK, Salinas M, Lewis TC. Evaluation of Community Action Against Asthma: A Community Health Worker Intervention to Improve Children’s Asthma-Related Health by Reducing Household Environmental Triggers for Asthma. Health Educ Behav. 2008 Jun;35(3):376–395. doi: 10.1177/1090198106290622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harvey I, Schulz A, Israel B, Sand S, Myrie D, Lockett M, Weir S, Hill Y. The Healthy Connections Project: A community-based participatory research project involving women at risk for diabetes and hypertension. Prog Community Health Partnersh. 2009;3(4):287–300. doi: 10.1353/cpr.0.0088. [DOI] [PubMed] [Google Scholar]
- 26.Corkery E, Palmer C, Foley ME, Schechter CB, Frisher L, Roman SH. Effect of a bicultural community health worker on completion of diabetes education in a Hispanic population. Diabetes Care. 1997 Mar;20(3):254–7. doi: 10.2337/diacare.20.3.254. [DOI] [PubMed] [Google Scholar]
- 27.Spencer MS, Rosland AM, Kieffer EC, Sinco BR, Valerio M, Palmisano G, Anderson M, Guzman JR, Heisler M. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. Am J Public Health. 2011 Dec;101(12):2253–60. doi: 10.2105/AJPH.2010.300106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brownson CA, Heisler M. The role of peer support in diabetes care and self-management. Patient. 2009 Mar;2(1):5–17. doi: 10.2165/01312067-200902010-00002. [DOI] [PubMed] [Google Scholar]
- 29.Schleyer T, Thyvalikakath TP, Malatack P, Marotta M, Shah TA, Phanichphant P, Price G, Hong J. The feasibility of a three-dimensional charting interface for general dentistry. JADA. 2007;138(8):1072–82. doi: 10.14219/jada.archive.2007.0318. [DOI] [PubMed] [Google Scholar]
- 30.Blomkvist S. Towards a Model for Bridging Agile Development and User-Centered Design. In: Seffah A, editor. Human-Centered Software Engineering – Integrating Usability in the Development Process. Springer; Netherlands: 2005. pp. 219–244. [Google Scholar]
- 31.De Vito Dabbs A, Myers BA, McCurry KR, Dunbar-Jacob J, Hawkins RP, Begey A, Dew MA. User-Centered Design and Interactive Health Technologies for Patients. Comput Inform Nurs. 2009 May-Jun;27(3):175–83. doi: 10.1097/NCN.0b013e31819f7c7c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of Community-Based Research: Assessing Partnership Approaches to Improve Public Health. Annu. Rev. Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 33.Israel BA, Schulz AJ, Parker EA, Becker AB. Community-based Participatory Research: Policy Recommendations for Promoting a Partnership Approach in Health Research. Education for Health. 2001;14(2):182–197. doi: 10.1080/13576280110051055. [DOI] [PubMed] [Google Scholar]
- 34.Becker AB, Israel BA, Allen AJ. Strategies and Techniques for Effective Group Process in CBPR Partnerships. In: Israel BA, Eng E, Schulz AJ, Parker EA, editors. Methods in Community-Based Participatory Research for Health. Jossey-Bass; San Francisco: 2005. pp. 52–72. [Google Scholar]
- 35.Carlson BA, Neal D, Magwood G, Jenkins C, King MG, Hossler CL. A community-based participatory health information needs assessment to help eliminate diabetes information disparities. Health Promot Pract. 2006 Jul;7(3 Suppl):213S–22S. doi: 10.1177/1524839906288694. [DOI] [PubMed] [Google Scholar]
- 36.Wells KB, Staunton A, Norris KC, Bluthenthal R, Chung B, Gelberg L, Jones L, Kataoka S, Koegel P, Miranda J, Mangione CM, Patel K, Rodriguez M, Shapiro M, Wong M. Building an academic-community partnered network for clinical services research: the Community Health Improvement Collaborative (CHIC) Ethn Dis. 2006;16(1 Suppl 1):S3–17. Winter. [PubMed] [Google Scholar]
- 37.Ginossar T, Nelson S. Reducing the Health and Digital Divides: A Model for Using Community-Based Participatory Research Approach to E-Health Interventions in Low-Income Hispanic Communities. J Comput Mediat Commun. 2010;15:530–551. [Google Scholar]
- 38.Viswanathan M, Ammerman A, Eng E, Garlehner G, Lohr KN, Griffith D, Rhodes S, Samuel-Hodge C, Maty S, Lux L, Webb L, Sutton SF, Swinson T, Jackman A, Whitener L. Community-based participatory research: assessing the evidence. Evid Rep Technol Assess (Summ) 2004 Aug;(99):1–8. [PMC free article] [PubMed] [Google Scholar]
- 39.Minkler M. Community-based research partnerships: challenges and opportunities. J Urban Health. 2005 Jun;82(2 Suppl 2):ii3–12. doi: 10.1093/jurban/jti034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wallerstein N, Duran B, Minkler M, Foley K. Developing and Maintaining Partnerships with Communities. In: Israel BA, Eng E, Schulz AJ, Parker EA, editors. Methods in Community-Based Participatory Research for Health. Jossey-Bass; San Francisco: pp. 31–51. [Google Scholar]
- 41.Two Feathers J, Kieffer EC, Palmisano G, Anderson M, Sinco B, Janz N, Heisler M, Spencer M, Guzman R, Thompson J, Wisdom K, James SA. Racial and Ethnic Approaches to Community Health (REACH) Detroit partnership: improving diabetes-related outcomes among African American and Latino adults. Amer J Public Health. 2005;95(9):1552–1560. doi: 10.2105/AJPH.2005.066134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Miller WR, Rollnick S. Motivational Interviewing: Preparing people for change. 2nd ed Guilford Press; NewYork: [Google Scholar]
- 43.Rollnick S, Miller WR. What is Motivational Interviewing? Behav Cogn Psychother. 1995;23:325–334. doi: 10.1017/S1352465809005128. [DOI] [PubMed] [Google Scholar]
- 44.Resnicow K, McMaster F, Rollnick S. Action Reflections: A Client-Centered Technique to Bridge the WHY-HOW Transition in Motivational Interviewing. Behav Cogn Psychother. 2012 Mar;14:1–7. doi: 10.1017/S1352465812000124. [DOI] [PubMed] [Google Scholar]
- 45.Resnicow K, McMaster F. Motivational Interviewing: Moving from Why to How with Autonomy Support. Int J Behav Nutr Phys Act. 2012 Mar 2;9(1):19. doi: 10.1186/1479-5868-9-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Heisler M, Resnicow K. Helping patients make and sustain healthy changes: A brief introduction to motivational interviewing in clinical diabetes care. Clinical Diabetes. 2008;26(4):161–165. [Google Scholar]
- 47.Ahmad F, Shakya Y, Li J, Khoaja K, Norman CD, Lou W, Abuelaish I, Ahmadzi HM. A pilot with computer-assisted psychosocial risk-assessment for refugees. BMC Med Inform Decis Mak. 2012 Jul 16;:12–71. doi: 10.1186/1472-6947-12-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Levine J, Wolf RL, Chinn C, Edelstein BL, MySmileBuddy: An. iPad-Based Interactive Program to Assess Dietary Risk for Early Childhood Caries. J Acad Nutr Diet. 2012 Oct;112(10):1539–42. doi: 10.1016/j.jand.2012.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kagohara DM, van der Meer L, Ramdoss S, O’Reilly MF, Lancioni GE, Davis TN, Rispoli M, Lang R, Marschik PB, Sutherland D, Green VA, Sigafoos J. Using iPods(®) and iPads(®) in teaching programs for individuals with developmental disabilities: A systematic review. Res Dev Disabil. 2012;34(1):147–156. doi: 10.1016/j.ridd.2012.07.027. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 50.Jowett EL, Moore DW, Anderson A. Using an iPad-based video modelling package to teach numeracy skills to a child with an autism spectrum disorder. Dev Neurorehabil. 2012;15(4):304–12. doi: 10.3109/17518423.2012.682168. Epub 2012 Jun 12. [DOI] [PubMed] [Google Scholar]
- 51.Venkatesh S, Greenhill S, Phung D, Adams B, Duong T. Pervasive multimedia for autism intervention. Pervasive Mob Comput. 2012 [Google Scholar]
- 52.Tang TS, Funnell MM, Gillard M, Nwankwo R, Heisler M. The development of a pilot training program for peer leaders in diabetes: process and content. Diabetes Educ. 2011 Jan-Feb;37(1):67–77. doi: 10.1177/0145721710387308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Heisler M, Piette JD. “I help you, and you help me”: facilitated telephone peer support among patients with diabetes. Diabetes Educ. 2005 Nov-Dec;31(6):869–79. doi: 10.1177/0145721705283247. [DOI] [PubMed] [Google Scholar]
- 54.Tang TS, Funnell MM, Gillard M, Nwankwo R, Heisler M. Training peers to provide ongoing diabetes self-management support (DSMS): results from a pilot study. Patient Educ Couns. 2011 Nov;85(2):160–8. doi: 10.1016/j.pec.2010.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kreuter MW, Strecher VJ, Glassman B. One Size Does Not Fit All: The Case for Tailoring Print Materials. Ann Behav Med. 1999;21(4):276–283. doi: 10.1007/BF02895958. [DOI] [PubMed] [Google Scholar]
- 56.Vinson C, Bickmore T, Farrell D, Campbell M, An L, Saunders E, Nowak M, Fowler B, Shaikh A. Adapting research-tested computerized tailored interventions for broader dissemination and implementation. Transl Behav Med. 2011;1:193–202. doi: 10.1007/s13142-010-0008-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Breslin M, Mullan RJ, Montori VM. The design of a decision aid about diabetes medications for use during the consultation with patients with type 2 diabetes. Patient Educ Couns. 2008 Dec;73(3):465–472. doi: 10.1016/j.pec.2008.07.024. [DOI] [PubMed] [Google Scholar]
- 58.Mullan RJ, Montori VM, Shah ND, et al. The diabetes mellitus medication choice decision aid: a randomized trial. Arch Intern Med. 2009 Sep;169(17):1560–1568. doi: 10.1001/archinternmed.2009.293. [DOI] [PubMed] [Google Scholar]