Abstract
Background
Now more than ever, cancer patients want health information. Little has been published to characterize the information needs and preferred sources of that information for patients who have completed cancer treatment.
Methods
We used a nationally validated instrument to prospectively survey patients attending a cancer clinic for a post-treatment follow-up visit. All patients who came to the designated clinics between December 2011 and June 2012 were approached (N = 648), and information was collected only from those who agreed to proceed.
Results
The 411 patients who completed the instrument included individuals with a wide range of primary malignancies. Their doctor or health professional was overwhelmingly the most trusted source of cancer information, followed by the Internet, family, and friends. The least trusted sources of information included radio, newspaper, and television. Patients most preferred to receive personalized written information from their health care provider.
Conclusions
Cancer survivors are keenly interested in receiving information about cancer, despite having undergone or finished active therapy. The data indicate that, for patients, their health care provider is the most trusted source of cancer information. Cancer providers should ask patients about the information they want and should direct them to trusted sources.
Keywords: Information-seeking, information needs, follow-up care, survivorship
1. INTRODUCTION
Today, understanding is growing about the importance of involving cancer patients in decision-making about their care, with the literature identifying an association between participation in decision-making by patients and their families and improved patient satisfaction and quality of life1–4. With that understanding comes the need for additional information on diagnosis, prognosis, and treatment options to support patients and their families in making informed decisions.
In cancer care, much is known about the characteristics of newly diagnosed patients who do or do not seek information about their care, the topics about which they seek information, and the means they prefer for receiving that information5–8. In a recent population-based study, Nagler and colleagues9 reported that the rate of information-seeking varied by tumour type: patients with colorectal cancer reported consistently less information-seeking than did patients with breast or prostate cancer, and the differences were most pronounced in patients with early-stage disease. With regard to sources of cancer information, a survey of 800 patients and 200 care-givers reported that a high proportion of caregivers (48%), but a low proportion of patients (4.8%), accessed Internet resources directly for cancer information10. Another study followed 104 patients from their initial radiotherapy consultation through to their first follow-up visit and reported that, although the information needs of those patients declined over that period, they remained high11.
Although limited by small sample sizes and select population sampling, the literature suggests that the need for information related to rehabilitation, disease recurrence, health promotion, and available support services might also be high for patients during the follow-up phase of their cancer care12–15. Whether that need for information varies by cancer site is still largely unknown, but the growing literature suggests that provision of patient-tailored information can ensure that the appropriate type and amount of information is received16. Survivorship care plans might be an effective way to provide such information. A survey conducted by the livestrong Foundation reported that survivorship care plans—specifically, the treatment summaries contained therein—are associated with a greater probability of meeting patient information needs concerning possible late effects of treatment, care received during treatment, and care received after treatment17. Given that Canadians diagnosed with cancer today have a better chance than patients diagnosed a decade ago of surviving the first 5 years after their diagnosis18, there is a clear need to understand the diverse information needs of this growing population of long-term survivors.
To identify gaps in patient knowledge after cancer treatment, we surveyed patients attending appointments at follow-up cancer clinics in Calgary, Alberta. Our study aimed to identify the information needs of patients being seen in a follow-up clinic and to assess whether those information needs varied according to demographics, primary cancer site, or time since last treatment. The study also aimed to identify patient preferences for the means of receiving health information. Three specific research questions were addressed:
In what types of information are cancer patients in Alberta most interested during the post-treatment and surveillance period?
Do their information interests vary by primary cancer diagnosis, demographic factors, or socioeconomic factors?
By what means do post-treatment cancer patients in Alberta most prefer to receive information?
The intended outcome of this research is to inform knowledge management strategies to better meet the information needs of patients and their families after cancer treatment within a publicly funded, provincial, population-based cancer program.
2. METHODS
2.1. Study Participants
A convenience sample of adult patients with cancer who attended outpatient clinics at the Tom Baker Cancer Centre (Calgary, AB) and Holy Cross Centre (Calgary, AB) between December 2011 and June 2012 were invited to participate in this study. After patients were checked in by clinic staff, they were approached by a research assistant who explained the nature of the study and then pre-screened interested participants by verbally confirming that they were being seen for follow-up. Upon consent, eligible participants were provided with a written questionnaire that we estimated would take 10 minutes to complete. The questionnaire could be completed with the assistance of a family member or companion. Patients were informed that their responses would be kept confidential and would not negatively affect their care then or in the future. Each questionnaire was coded with a unique identification number to ensure confidentiality. Completed questionnaires were returned directly to the research assistant.
2.2. Questionnaire
The questionnaire was selected based on themes related to patient information needs identified in the peer-reviewed literature, validation of the questionnaire in cancer patients, question readability, and alignment of the survey content to our research questions. The Health Information National Trends Survey (hints) from the U.S. National Cancer Institute was found to most closely address each of those needs, and permission was obtained from the National Cancer Institute to use relevant questions from the 2003, 2005, and 2007 hints versions19. A draft of the survey was pilot-tested with 10 patients in the outpatient clinic at the Holy Cross Centre before recruitment began. Feedback derived from the pilot-testing phase was used to improve survey readability and ensure acceptable content and feasibility. The survey included items related to the importance of various cancer topics, usual and preferred sources for receiving cancer information and extent to which those sources of cancer information are trusted, preferred formats for receiving cancer information, and whether information found on the Internet was discussed with a health professional in the past year. Demographic items (age, sex, marital status, level of education, and income) and clinical information (for example, cancer type and date of diagnosis) were also requested.
2.3. Statistical Analysis
Descriptive statistics are used to summarize the characteristics of study participants and the sources and types of cancer information used. Comparative analyses are used to examine differences between patient groups defined according to disease site (that is, breast, prostate, non-prostate genitourinary, gynecologic, cutaneous, and gastrointestinal) with respect to discussing information found on the Internet within the past year with a health professional, extent to which various cancer information sources are trusted, preferred formats for receiving cancer information, and the importance of various cancer topics. The SPSS software application (version 19.0; IBM, Armonk, NY, U.S.A.) was used to perform all analyses.
Scientific and ethics approval for this study were obtained from the Alberta Cancer Research Ethics Committee and the Conjoint Health Research Ethics Board of the Faculties of Medicine, Nursing, and Kinesiology at the University of Calgary.
3. RESULTS
3.1. Patient Population
The 648 unique patients who came to the designated clinics between December 2011 and June 2012 were approached to participate, and of those, 411 (63.4%) agreed. No formal survey was conducted to determine reasons for nonparticipation, but disinterest and not feeling up to it were explanations commonly offered. Table i presents the sociodemographic and tumour characteristics of consenting respondents. Almost half the patients had been diagnosed with either breast cancer (23.4%) or prostate cancer (22.1%). Most respondents were 50 years of age or older (74.2%), and only a small proportion of patients (7.1%) had been treated 5 or more years earlier. Most respondents (89.8%) rated their general health status as excellent or good, and only a small proportion (fewer than 5.5%) indicated that they had experienced sadness, nervousness, restlessness, hopelessness, or worthlessness during the preceding 30 days (data not shown).
TABLE I.
Sociodemographic characteristics of survey respondents
| Characteristic | Value |
|---|---|
| Respondents (n) | 411 |
| Current age group [n (%)] | |
| ≤49 Years | 88 (21.4) |
| 50–59 Years | 86 (20.9) |
| 60–69 Years | 102 (24.8) |
| 70–79 Years | 68 (16.5) |
| ≥80 Years | 49 (11.9) |
| Not specified | 18 (4.4) |
| Sex [n (%)] | |
| Men | 174 (42.3) |
| Women | 219 (53.3) |
| Not specified | 18 (4.4) |
| Marital status [n (%)] | |
| Married | 269 (65.5) |
| Living as married | 21 (5.1) |
| Divorced | 45 (10.9) |
| Widowed | 31 (7.5) |
| Separated | 11 (2.7) |
| Single, never married | 20 (4.9) |
| Not specified | 14 (3.4) |
| Education level [n (%)] | |
| High school or less | 134 (32.6) |
| Post–high school | 87 (21.2) |
| College or university | 134 (32.6) |
| Postgraduate | 40 (9.7) |
| Not specified | 16 (3.9) |
| Race [n (%)] | |
| White | 343 (83.5) |
| Other | 51 (12.4) |
| Not specified | 17 (4.1) |
| Site of malignancy [n (%)] | |
| Breast | 96 (23.4) |
| Prostate | 91 (22.1) |
| Gynecologica | 58 (14.1) |
| Cutaneousb | 55 (13.4) |
| Gastrointestinalc | 25 (6.1) |
| Non-prostate genitourinaryd | 23 (5.6) |
| More than 1 sitee | 23 (5.6) |
| Not specified | 40 (9.7) |
| Time since treatment [n (%)] | |
| ≥5 Years | 29 (7.1) |
| 1–5 Years | 125 (30.4) |
| 6–12 Months | 62 (15.1) |
| ≤6 Months | 83 (20.2) |
| Still in treatment | 52 (12.7) |
| Never treated | 33 (8.0) |
| Not specified | 27 (6.6) |
Ovaries, uterus or endometrium, cervix, other.
Melanoma or non-melanoma skin cancer, or both
Stomach, pancreas, liver, colon, rectum, anus.
Kidney, bladder, testicles.
Two or more of breast, prostate, genitourinary, gynecologic, cutaneous, and gastrointestinal.
3.2. Information-Seeking Patterns
Table ii describes the sources and types of cancer information used by patients in their most recent search. The most frequently reported source of information was the Internet (57.4%); other commonly used sources of information included a health provider (32.6%), brochures or pamphlets (25.1%), and cancer organizations (24.3%). The least frequently reported cancer information sources included a 1–800 telephone number (0.2%), the library (4.4%), and complementary or alternative practitioners (4.9%). The most frequently reported types of information sought included information about a specific type of cancer (43.1%), treatment or cures for cancer (29.4%), prognosis or recovery from cancer (29.0%), and prevention of cancer (27.0%). The least frequently reported types of cancer information sought included where to get medical care (3.4%), paying for medical care or insurance (4.6%), and cancer organizations (5.4%).
TABLE II.
Sources and types of cancer information used in most recent search
| Variable | Value [n (%)] |
|---|---|
| Information source | |
| Internet | 236 (57.4) |
| Health provider | 134 (32.6) |
| Brochures or pamphlets | 103 (25.1) |
| Cancer organization | 100 (24.3) |
| Another person with cancer | 71 (17.3) |
| Books | 66 (16.1) |
| Family | 39 (9.5) |
| Newspaper | 36 (8.8) |
| Magazine | 32 (7.8) |
| Friend or co-worker | 27 (6.6) |
| Complementary or alternative practitioner | 20 (4.9) |
| Library | 18 (4.4) |
| 1–800 Telephone number | 1 (0.2) |
| Didn’t look for cancer information | 48 (11.7) |
| Missing response | 10 (2.4) |
| Type of information | |
| Specific type of cancer | 177 (43.1) |
| Treatment for cancer | 121 (29.4) |
| Prognosis for or recovery from cancer | 119 (29.0) |
| Prevention of cancer | 111 (27.0) |
| Causes of or risk factors for cancer | 103 (25.1) |
| Cancer in general | 103 (25.1) |
| Symptoms of cancer | 95 (23.1) |
| Coping with cancer | 88 (21.4) |
| Diagnosis of cancer | 54 (13.1) |
| Screening, testing, or early detection | 52 (12.7) |
| Complementary, alternative, or unconventional treatments | 43 (10.5) |
| Diagnostic tests | 42 (10.2) |
| Cancer organizations | 22 (5.4) |
| Paying for medical care or insurance | 19 (4.6) |
| Where to get medical care | 14 (3.4) |
| Didn’t look for cancer information | 17 (4.1) |
| Missing response | 16 (3.9) |
Table iii describes the frequency with which patients discussed information found on the Internet with their health professional during the preceding year. Data are presented for the group overall and by cancer site. Overall, more than 80% of respondents reported that they used the Internet, but only 30.4% of the patients reported having discussed the information they found there with their health professional. The rate of discussion with a health professional was highest among respondents with a breast cancer primary (37.5%); the rate of non-discussion was highest among respondents with a non-prostate genitourinary primary (65.2%). The patient’s cancer site and a discussion of information found on the Internet with a health professional were significantly associated (p < 0.0001), but we observed no significant association between sex and a discussion of information found on the Internet with a health professional (32.4% women vs. 28.7% men).
TABLE III.
Discussion, in the preceding year, with a health professional about information found on the Internet
| Cancer site |
Response [n (%)]
|
|||
|---|---|---|---|---|
| Yes | No | Internet non-user | Not specified | |
| Alla | 125 (30.4) | 188 (45.7) | 81 (19.7) | 17 (4.1) |
| Breast | 36 (37.5) | 45 (46.9) | 15 (15.6) | 0 (0) |
| Prostate | 28 (30.8) | 38 (41.8) | 24 (26.4) | 1 (1.1) |
| Gynecologicb | 17 (29.3) | 27 (46.6) | 12 (20.7) | 2 (3.4) |
| Non-prostate guc | 6 (26.1) | 15 (65.2) | 2 (8.7) | 0 (0) |
| Cutaneousd | 18 (32.7) | 29 (52.7) | 5 (9.1) | 3 (5.5) |
| Gastrointestinale | 7 (28.0) | 14 (56.0) | 4 (16.0) | 0 (0) |
| p = 0.000 | ||||
Includes patients who did not specify their cancer site (n = 40) and those who specified more than 1 cancer site (n = 23).
Ovaries, uterus or endometrium, cervix, other.
Kidney, bladder, testicles.
Melanoma or non-melanoma skin cancer, or both
Stomach, pancreas, liver, colon, rectum, anus.
gu = genitourinary.
3.3. Information-Seeking Preferences
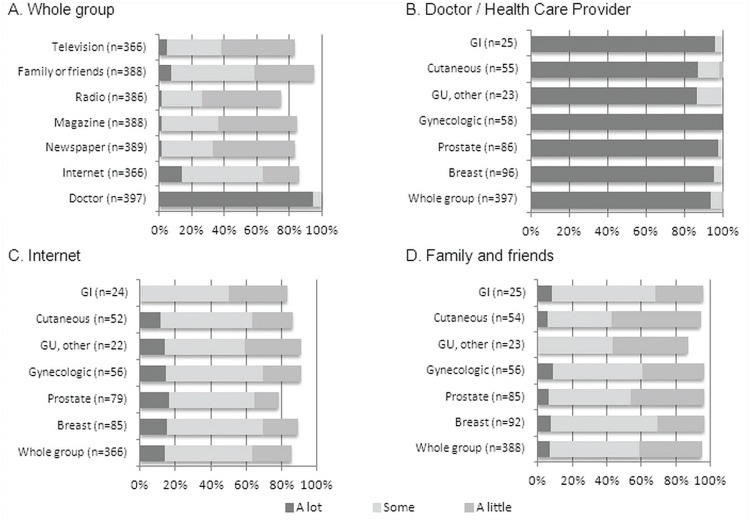
Figure 1 illustrates the level of trust—that is, “a lot” to “not at all”—that respondents reported having in various sources of cancer information. The doctor or health care provider was overwhelmingly the source of cancer information most trusted by the group overall, followed by Internet, and family and friends [Figure 1(A)]. The least trusted sources of information included radio, newspaper, and television. The level of trust in the doctor or health care provider was high across all cancer sites; however, it was highest for respondents with gynecologic primaries and lowest for respondents with non-prostate genitourinary primaries and cutaneous primaries. We observed a significant association between cancer site and level of trust in the doctor or health professional (p < 0.0001); no significant associations were observed between cancer site and level of trust in the Internet (p = 0.077) or in family and friends (p = 0.066).
Figure 1.
Level of trust in cancer information sources. (A) Whole-group rating of trust in cancer information sources. (B) Rating of trust in a health care provider, by cancer site. (C) Rating of trust in the Internet, by cancer site. (D) Rating of trust in family and friends, by cancer site.
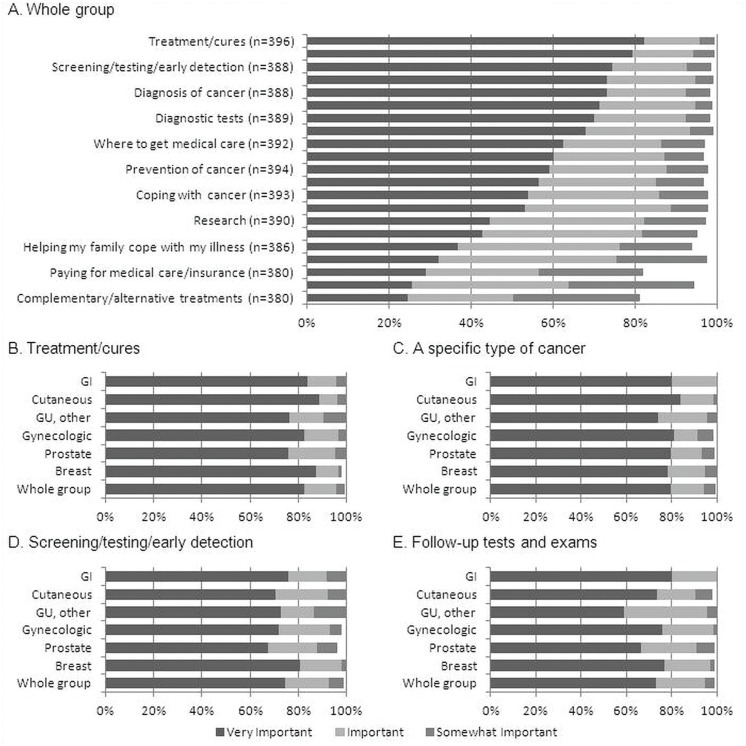
When asked to rate the importance—that is, “very important” to “not at all important”—of various cancer information topics, respondents rated information about treatment or cures; a specific type of cancer; screening, testing, or early detection; and follow-up tests and exams as the most important topics (Figure 2). We observed no significant associations between cancer site and the rated importance of information about treatment or cures (p = 0.270); about screening, testing, or early detection (p = 0.531); and about follow-up tests and exams (p = 0.068). However, information about a specific type of cancer varied significantly by cancer site (p = 0.020): it was highest among respondents with gastrointestinal and cutaneous primaries and lowest among respondents with non-prostate genitourinary primaries.
Figure 2.
Importance of cancer information topics. (A) Whole-group rating of importance of all cancer information topics. (B) Rating of importance of information about treatment or cures, by cancer site. (C) Rating of importance of information about a specific type of cancer, by cancer site. (D) Rating of importance of information about screening, testing, or early detection, by cancer site. (E) Rating of importance of information about follow-up tests and exams, by cancer site.
3.4. Preferred Sources of Information
Participants were asked to indicate whether they would prefer to receive information from these sources: an in-person meeting with a health care professional; reading materials personalized to their lifestyle or family history; e-mail or Internet; a telephone call from a health professional; a book, magazine, or other publication; an interactive cd-rom; a video or dvd; or an audio cd or mp3 file (Table iv). The source most commonly preferred was an in-person meeting with a health care professional (84.1%), followed by personalized reading materials (75.1%). We observed a significant association between cancer site and preference for an in-person meeting (p = 0.002); for personalized reading materials (p = 0.001); for a telephone call (p = 0.001); for a book, magazine, or other publication (p = 0.001); and for an interactive cd-rom (p = 0.008). An analysis by sex of the preferred media revealed that more women than men preferred an in-person meeting with a health professional (87.2% vs. 77.0%, p < 0.05); personalized reading materials (80.8% vs. 66.1%, p < 0.05); a telephone call from a health professional (72.1% vs. 54.0%, p < 0.05); and a book, magazine, or other publication (54.8% vs. 41.4%, p < 0.05).
TABLE IV.
Preferred ways of receiving information about cancer
| Response | Cancer site [n (%)] | p Value | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Alla | Breast | Prostate | Gynecologicb | Non-prostateguc | Cutaneousd | Gastro-intestinale | ||
| In-person meeting | 334 (84.1) | 83 (87.4) | 64 (73.6) | 54 (94.7) | 18 (78.3) | 44 (80.0) | 23 (95.8) | 0.002 |
| Personalized reading | 298 (75.1) | 78 (82.1) | 63 (72.4) | 46 (80.7) | 10 (43.5) | 39 (70.9) | 20 (83.3) | 0.001 |
| E-mail/Internet | 266 (67.0) | 61 (64.2) | 60 (69.0) | 40 (70.2) | 6 (26.1) | 39 (70.9) | 17 (70.8) | NS |
| Telephone call | 257 (64.7) | 68 (71.6) | 40 (46.0) | 45 (78.9) | 15 (65.2) | 36 (65.5) | 16 (66.7) | 0.001 |
| Publication | 198 (49.9) | 58 (61.1) | 34 (39.1) | 28 (49.1) | 7 (30.4) | 25 (45.5) | 15 (62.5) | 0.001 |
| Interactive cd-rom | 157 (39.5) | 42 (44.2) | 28 (32.2) | 25 (43.9) | 9 (39.1) | 20 (36.4) | 16 (66.7) | 0.008 |
| Video or dvd | 150 (37.8) | 36 (37.8) | 27 (31.0) | 23 (40.4) | 8 (34.8) | 24 (43.6) | 11 (45.8) | NS |
| Audio cd or mp3 | 68 (17.1) | 19 (20.0) | 12 (13.8) | 9 (15.8) | 4 (17.4) | 9 (16.4) | 7 (29.2) | NS |
Includes patients who did not specify their cancer site (n = 40) and those who specified more than 1 cancer site (n = 23).
Ovaries, uterus or endometrium, cervix, other.
Kidney, bladder, testicles.
Melanoma or non-melanoma skin cancer, or both
Stomach, pancreas, liver, colon, rectum, anus.
gu = genitourinary; ns = nonsignificant.
4. DISCUSSION
To date, only limited data have been published about the information-seeking preferences of patients undergoing follow-up cancer care. Our study suggests that, despite having completed active therapy, this population is very interested in receiving information about cancer. In fact, information about treatment and cures was rated highest in terms of importance. Not surprisingly, the topics of a specific type of cancer and of follow-up tests and exams were also among the highest-rated.
A recent study by Douma et al.11 looked at changes in the information needs of radiotherapy patients over time and found that those needs declined somewhat from initial consultation to follow-up, but nevertheless remained high; in fact, information needs increased or remained stable for 66% of the study respondents by the time of follow-up. A study analyzing calls received by a cancer information service provided by the National Cancer Institute found that, among 3696 patients undergoing post-treatment follow-up, specific treatment information was sought by 43%, general cancer site information by 27%, and prevention and risk factors information by 10%13. In general, information-seeking about those topics by patients during follow-up appears to be similar to that by patients in treatment11,13,20.
Most respondents in our study reported having used the Internet in past, and among all respondents, the Internet was the most frequently cited source of cancer information, followed by a health care provider, brochures or pamphlets, and cancer organizations. Mayer et al.15 also showed that, among cancer survivors who completed the 2003 version of the hints survey by telephone, the Internet was the most preferred non–health care provider source of information, followed by family and friends, cancer organizations, and the library. In contrast, another survey involving patients receiving treatment for thoracic malignancies (n = 139) showed that only 16% actually sought information from the Internet, despite 60% being interested in its use as an information source21. This latter study also found that, among respondents who reported using the Internet, the Internet-derived information was perceived to be of a quality similar to that of other nonphysician sources21, suggesting that trust in the Internet is equivalent to that in other sources. In contrast, our results suggest that the Internet is, in fact, trusted more than other sources such as television, radio, newspaper, and magazines. Approximately 64% of respondents in our study reported that they trust Internet-derived information “a lot” or “some.” The proportion of respondents in the hints (2007) telephone survey who reported trusting the Internet “a lot” or “some” was even higher at 73%22. But the most trusted source of information by far, in our study and others9,15,23, was a doctor or other health care provider. Complementary or alternative practitioners and services were not a frequently cited source of cancer information in our study. That finding makes sense in light of data from a 2009 study by Bennett and colleagues24, which showed that among survivors of adult cancers (n = 836) in New Zealand, the use of complementary and alternative medicine services ranged from <1% to 33% depending on the type of service and patient age.
Our study showed that, although use of the Internet is high, only a small proportion of patients (30% in the preceding year) discussed information found on the Internet with a health care provider; the rate of discussion was highest among respondents with a breast cancer primary (38%) and lowest among patients with a non-prostate genitourinary primary (26%). Further, there was no significant difference between the proportions of women and men who reported having a discussion with their health care provider. Those results accord with a survey of ambulatory patients (n = 191) and Canadian oncologists (n = 410) which found that, although 71% of patients reported having actively searched for cancer information, the rate of discussion with their oncologist was low: 52% of oncologists reported that fewer than a quarter of their patients wanted to discuss information that they had found, and just 19.6% reported that more than half their patients wanted to discuss information25.
Patients in our study indicated that the top three ways in which they most prefer to receive cancer information are from a health care professional in person (84%), from personalized reading materials (75%), and in e-mail or from the Internet (67%). Patients with a gastrointestinal malignancy had the highest preference for an in-person meeting with their health care professional (96%); patients with prostate cancer had the lowest preference (74%). Interestingly, only 44% of patients with non-prostate genitourinary malignancies preferred personalized reading materials. In our study, there were no significant differences between cancer sites in terms of preference for receiving information by e-mail or from the Internet—a finding that contrasts with results in the study by Mayer and colleagues15, which showed that cancer survivors most preferred to receive information from personalized reading materials (90%), print materials (82%), and a health care provider (80%). However, the latter data were not analyzed by cancer site.
Care plans might represent one of the best means for delivering information to patients undergoing follow-up cancer care. The U.S. Institute of Medicine called for patients completing their primary treatment for cancer—and for their primary care providers—to be provided with a treatment summary and comprehensive plan for follow-up, with the intent of providing guidance on follow-up care, prevention, and health maintenance26. A recent evaluation of the care plans of 36 breast cancer survivors and 21 head-and-neck cancer survivors in Alberta, including interviews with the physicians, nurses, and patients involved, suggested that care plans can enhance communication between survivors and care providers and that survivors appreciate individualized attention and comprehensiveness in a care plan27. The importance of providing cancer survivors with individualized information has been reported elsewhere28,29. The data gained from the present study could be used in part to inform the development survivorship care plans for several of the major types of cancer, including breast, prostate, gynecologic, and cutaneous malignancies.
5. CONCLUSIONS
Patients who have completed active therapy, but who are still undergoing follow-up care and cancer surveillance, are keenly interested to receive information about a range of cancer topics. Their information desires vary somewhat according to primary cancer site. The sources from which follow-up patients prefer to receive information also vary by cancer site. We conclude that initiatives to provide information to patients in this setting could be tailored to better meet patient needs according to their preferences. One strategy that might be useful is to develop survivorship care plans for patients and their family physicians. Those plans would include information about the specific type of malignancy; past, current, and ongoing treatment options; follow-up tests and exams; and other individualized information, as appropriate. Another strategy might be for physicians to provide patients with a list of trusted Web sites that contain appropriate information or to develop secure patient information portals with secure access that would contain information specific to the individual patient’s malignancy.
To our knowledge, the present study is the first to examine the information practices, interests, and preferences of patients undergoing follow-up for cancer and to investigate differences between the patients according to their primary cancer site. Further work will be required to evaluate the effectiveness of tailored care plans or the value of an “e-prescription” by physicians to their patients on completion of cancer treatment.
6. ACKNOWLEDGMENTS
This study was supported by a grant from Alberta Innovates Health Solutions (no. 201000221). The authors thank Linda Lutz and Angela Zwiers for assistance with instrument development, pre-testing, and interviewing.
7. CONFLICT OF INTEREST DISCLOSURES
The authors have no financial conflicts of interest to declare.
8. REFERENCES
- 1.Rutten LJ, Arora NK, Bakos AD, Aziz N, Rowland J. Information needs and sources of information among cancer patients: A systematic review of research (1980–2003) Patient Educ Couns. 2005;57:250–61. doi: 10.1016/j.pec.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 2.Lock KK, Willson B. Information needs of cancer patients receiving chemotherapy in an ambulatory-care setting. Can J Nurs Res. 2002;34:83–93. [PubMed] [Google Scholar]
- 3.Boudioni M, McPherson K, Moynihan C, et al. Do men with prostate or colorectal cancer seek different information and support from women with cancer? Br J Cancer. 2001;85:641–8. doi: 10.1054/bjoc.2001.1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mesters I, van den Borne B, De Boer M, Pruyn J. Measuring information needs among cancer patients. Patient Educ Couns. 2001;43:253–62. doi: 10.1016/S0738-3991(00)00166-X. [DOI] [PubMed] [Google Scholar]
- 5.Brody DS, Miller SM, Lerman CE, Smith DG, Caputo GC. Patient perception of involvement in medical care: relationship to illness attitudes and outcomes. J Gen Intern Med. 1989;4:506–11. doi: 10.1007/BF02599549. [DOI] [PubMed] [Google Scholar]
- 6.Jones RA, Steeves R, Ropka ME, Hollen P. Capturing treatment decision making among patients with solid tumors and their caregivers. Oncol Nurs Forum. 2013;40:E24–31. doi: 10.1188/13.ONF.E24-E31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berry DL, Wang Q, Halpenny B, Hong F. Decision preparation, satisfaction and regret in a multi-center sample of men with newly diagnosed localized prostate cancer. Patient Educ Couns. 2012;88:262–7. doi: 10.1016/j.pec.2012.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spittler CA, Pallikathayil L, Bott M. Exploration of how women make treatment decisions after a breast cancer diagnosis. Oncol Nurs Forum. 2012;39:E425–33. doi: 10.1188/12.ONF.E425-E433. [DOI] [PubMed] [Google Scholar]
- 9.Nagler RH, Gray SW, Romantan A, et al. Differences in information seeking among breast, prostate, and colorectal cancer patients: results from a population-based survey. Patient Educ Couns. 2010;81(suppl):S54–62. doi: 10.1016/j.pec.2010.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.James N, Daniels H, Rahman R, McConkey C, Derry J, Young A. A study of information seeking by cancer patients and their carers. Clin Oncol (R Coll Radiol) 2007;19:356–62. doi: 10.1016/j.clon.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 11.Douma KF, Koning CC, Zandbelt LC, de Haes HC, Smets EM. Do patients’ information needs decrease over the course of radiotherapy? Support Care Cancer. 2012;20:2167–76. doi: 10.1007/s00520-011-1328-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lewis RA, Neal RD, Hendry M, et al. Patients’ and healthcare professionals’ views of cancer follow-up: systematic review. Br J Gen Pract. 2009;59:e248–59. doi: 10.3399/bjgp09X453576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Squiers L, Finney Rutten LJ, Treiman K, Bright MA, Hesse B. Cancer patients’ information needs across the cancer care continuum: evidence from the cancer information service. J Health Commun. 2005;10(suppl 1):15–34. doi: 10.1080/10810730500263620. [DOI] [PubMed] [Google Scholar]
- 14.Beckjord EB, Arora NK, McLaughlin W, Oakley–Girvan I, Hamilton AS, Hesse BW. Health-related information needs in a large and diverse sample of adult cancer survivors: implications for cancer care. J Cancer Surviv. 2008;2:179–89. doi: 10.1007/s11764-008-0055-0. [DOI] [PubMed] [Google Scholar]
- 15.Mayer DK, Terrin NC, Kreps GL, et al. Cancer survivors information seeking behaviors: a comparison of survivors who do and do not seek information about cancer. Patient Educ Couns. 2007;65:342–50. doi: 10.1016/j.pec.2006.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nicolaije KA, Husson O, Ezendam NP, et al. Endometrial cancer survivors are unsatisfied with received information about diagnosis, treatment and follow-up: a study from the population-based profiles registry. Patient Educ Couns. 2012;88:427–35. doi: 10.1016/j.pec.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 17.Rechis R, Beckjord EB, Nutt S. Potential benefits of treatment summaries for survivors’ health and information needs: results from a livestrong survey. J Oncol Pract. 2014;10:75–8. doi: 10.1200/JOP.2013.000973. [DOI] [PubMed] [Google Scholar]
- 18.Canadian Cancer Society’s Advisory Committee on Cancer Statistics. Canadian Cancer Statistics 2013. Toronto, ON: Canadian Cancer Society; 2013. Special Topic: Liver Cancer. [Available online at: http://www.cancer.ca/∼/media/cancer.ca/CW/cancer%20information/%20cancer%20101/Canadian%20cancer%20statistics/canadian-cancer-statistics-2013-EN.pdf; cited July 23, 2013] [Google Scholar]
- 19.Koch–Weser S, Bradshaw YS, Gualtieri L, Gallagher SS. The Internet as a health information source: findings from the 2007 Health Information National Trends Survey and implications for health communication. J Health Commun. 2010;15(suppl 3):279–93. doi: 10.1080/10810730.2010.522700. [DOI] [PubMed] [Google Scholar]
- 20.Basch EM, Thaler HT, Shi W, Yakren S, Schrag D. Use of information resources by patients with cancer and their companions. Cancer. 2004;100:2476–83. doi: 10.1002/cncr.20261. [DOI] [PubMed] [Google Scholar]
- 21.Peterson MW, Fretz PC. Patient use of the Internet for information in a lung cancer clinic. Chest. 2003;123:452–7. doi: 10.1378/chest.123.2.452. [DOI] [PubMed] [Google Scholar]
- 22.Kowalczyk N, Draper LJ. Trends in patient information preferences and acquisition. Radiol Technol. 2012;83:316–24. [PubMed] [Google Scholar]
- 23.Cegala DJ, Bahnson RR, Clinton SK, et al. Information seeking and satisfaction with physician–patient communication among prostate cancer survivors. Health Commun. 2008;23:62–9. doi: 10.1080/10410230701806982. [DOI] [PubMed] [Google Scholar]
- 24.Bennett JA, Cameron LD, Whitehead LC, Porter D. Differences between older and younger cancer survivors in seeking cancer information and using complementary/alternative medicine. J Gen Intern Med. 2009;24:1089–94. doi: 10.1007/s11606-009-0979-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen X, Siu LL. Impact of the media and the Internet on oncology: survey of cancer patients and oncologists in Canada. J Clin Oncol. 2001;19:4291–7. doi: 10.1200/JCO.2001.19.23.4291. [DOI] [PubMed] [Google Scholar]
- 26.United States, National Academy of Sciences, Institute of Medicine. Implementing Cancer Survivorship Care Planning. Washington, DC: The National Academies Press; 2007. [Google Scholar]
- 27.Collie K, McCormick J, Waller A, et al. Qualitative evaluation of care plans for Canadian breast and head-and-neck cancer survivors. Curr Oncol. 2014;21:e18–28. doi: 10.3747/co.21.1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haq R, Heus L, Baker NA, et al. Designing a multifaceted survivorship care plan to meet the information and communication needs of breast cancer patients and their family physicians: results of a qualitative pilot study. BMC Med Inform Decis Mak. 2013;13:76. doi: 10.1186/1472-6947-13-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singh–Carlson S, Wong E, Martin L, Nguyen SK. Breast cancer survivorship and South Asian women: understanding about the follow-up care plan and perspectives and preferences for information post treatment. Curr Oncol. 2013;20:e63–79. doi: 10.3747/co.20.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]