Abstract
Background
Vascular injury is a devastating complication of acute knee dislocation. However, there are wide discrepancies in the reported frequency of vascular injury after knee dislocations, as well as important differences among approaches for diagnosis of this potentially limb-threatening problem.
Questions/purposes
We determined (1) the frequency of vascular and neurologic injury after knee dislocation and whether it varied by the type of knee dislocation, (2) the frequency with which surgical intervention was performed for vascular injury in this setting, and (3) the frequency with which each imaging modality was used to detect vascular injury.
Methods
We searched the MEDLINE® literature database for studies in English that examined the clinical sequelae and diagnostic evaluation after knee dislocation. Vascular and nerve injury incidence after knee dislocation, surgical repair rate within vascular injury, and amputation rate after vascular injury were used to perform a meta-analysis. Other measures such as diagnostic modality used and the vessel injured after knee dislocation were also evaluated.
Results
We identified 862 patients with knee dislocations, of whom 171 sustained vascular injury, yielding a weighted frequency of 18%. The frequency of nerve injuries after knee dislocation was 25% (75 of 272). We found that 80% (134 of 160) of vascular injuries underwent repair, and 12% (22 of 134) of vascular injuries resulted in amputation. The Schenck and Kennedy knee dislocation classifications with the highest vascular injury prevalence were observed in knees that involved the ACL, PCL, and medial collateral liagment (KDIIIL) (32%) and posterior dislocation (25%), respectively. Selective angiography was the most frequently used diagnostic modality (61%, 14 of 23), followed by nonselective angiography and duplex ultrasonography (22%, five of 23), ankle-brachial index (17%, four of 23), and MR angiography (9%, two of 23).
Conclusions
This review enhances our understanding of the frequency of vascular injury and repair, amputation, and nerve injuries after knee dislocation. It also illustrates the lack of consensus among practitioners regarding the diagnostic and treatment algorithm for vascular injury. After pooling existing data on this topic, no outcomes-driven conclusions could be drawn regarding the ideal diagnostic modality or indications for surgical repair. In light of these findings and the morbidity associated with a missed diagnosis, clinicians should err on the side of caution in ruling out arterial injury.
Introduction
Knee dislocations may cause vascular injuries, including injuries to the tunica intima, arterial occlusions, avulsion injuries, ruptures, or transections [5]. The popliteal artery’s anatomic location places it at particular risk for damage during knee dislocation. The popliteal artery originates at the position of the tendinous hiatus of the adductor magnus muscle; once distal to the popliteal fossa, it is anchored firmly by the tendinous arch of the soleus muscle before dividing into the anterior and posterior tibial arteries [21]. Thus, it is tethered firmly above and below the knee, making this artery extremely susceptible to injury.
Because vascular injury is potentially limb threatening, rapid identification and repair of vascular injury are critical. A delay in the diagnosis and repair of a vascular injury increases the time of warm ischemia and the risk for irreversible injury, resulting in the possible need for an above-knee amputation [3]. The reported frequency of vascular injury after knee dislocation is variable, with most estimates ranging from 22% to 32% [10, 41]. However, the majority of studies in this setting have relatively few patients, making them subject to sampling error, and/or they report little or no followup [16, 17, 24, 29, 38, 39].
Other potential complications seen in knee dislocations include compartment syndrome, deep vein thrombosis, and most commonly, neurologic injury. Neurologic damage involving the common peroneal nerve is estimated to occur in approximately 25% of knee dislocations [31]. The common peroneal nerve branches off the sciatic nerve and is located obliquely lateral to the popliteal fossa, bending around the fibular neck. While not a surgical emergency, injury to the peroneal nerve may compromise dorsiflexion of the foot leading to foot drop and gait impairment. Additionally, paresthesias and sensory loss to portions of the anterior lower lateral leg and the dorsal surface of the foot may also occur [43].
There is currently considerable debate in the literature regarding the optimal diagnostic method for detecting vascular injury. Conventional angiography was once the gold standard for diagnosis and was routinely ordered after knee dislocation. Some studies recommend routine angiography for all patients presenting with knee dislocation [6, 28], but many authors now advocate the use of selective angiography, suggesting only those patients with abnormal pulses or ankle-brachial indexes (ABIs) undergo angiography [13, 20, 28, 32]. Proponents of the former school of thought point out the grave clinical consequences of a missed vascular injury diagnosis, while those of the latter cite the accuracy of noninvasive screening examinations, as well as the costs and risks associated with angiography. Since each imaging technique inherently has its own advantages, agreement as to which method is the most readily available, is cost-effective, and has the most evidence-based support, along with the highest positive predictive value, cannot be found in the literature [28, 34]. This paper serves to provide data on these diagnostic methods in the current literature to serve as a source of information for further studies to be conducted.
In this systematic review, we surveyed the existing data to determine (1) the frequency of vascular and neurologic injury after knee dislocation and whether vascular injury varied by the type of knee dislocation, (2) the frequency with which surgical intervention was performed for vascular injury in this setting, and (3) the frequency with which each imaging modality was used to detect vascular injury.
Materials and Methods
Literature Search
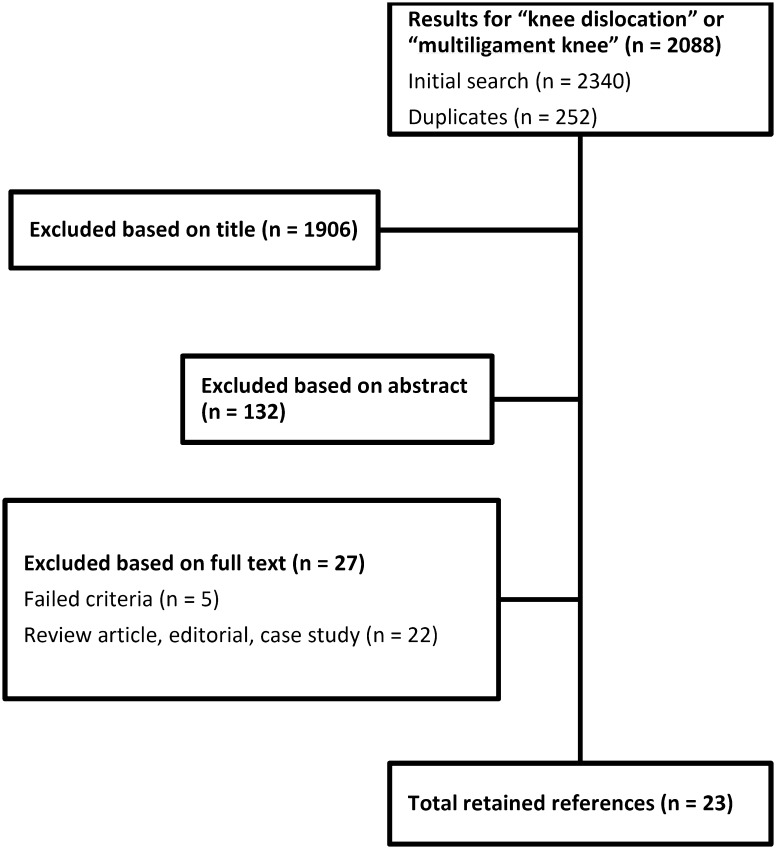
Three reviewers (OM, GAA, MGY) independently searched the MEDLINE® literature database for studies published in English, including randomized controlled trials, quasirandomized control trials, prospective and retrospective cohort studies, and case series that examined the clinical sequelae and diagnostic evaluation after knee dislocation (last search May 3, 2013). The search terms used were “knee dislocation” and “multiple ligament knee” and the search limits were English language and human subjects. The bibliographies of the retrieved articles were also reviewed to locate additional studies not found in the initial search (Fig. 1).
Fig. 1.
A flowchart shows the sequence of the literature review.
Study Selection and Data Extraction
The three reviewers evaluated the search results to identify those studies that were potentially relevant to this study. For the purposes of this study, knee dislocation was defined as gross knee instability with multiligamentous injury [27]. Papers that reported specifically on frequency of or diagnostic modalities for vascular injury were further evaluated. Exclusion criteria were case reports, review articles, and surgical technique articles. Retaining articles after full-text review required unanimous consensus among the three reviewers. Unanimous consensus was achieved in all cases. Twenty-three studies including 907 patients were evaluated [1, 2, 4, 6, 8, 11, 14, 17, 19, 20, 22, 27–29, 33–36, 38, 39, 41, 44, 45]. None of these studies were Level I, six studies were Level II, 15 studies were Level III, and two studies were Level IV. Fifteen studies totaling 756 patients reported the age of their patients with knee dislocation, yielding a mean age of 31.6 years (range, 12–78 years) [2, 4, 6, 8, 11, 20, 22, 27–29, 33–35, 38, 39].
Two reviewers (OM, GAA) independently extracted data. Disagreements between reviewers were resolved by consensus or consultation with a third reviewer (MGY). The information gathered included author and publication year, study type, total patient count, number of knee dislocations, number of vascular injuries, vessels injured, number of nerve injuries, number of injuries surgically repaired, amputation rate after vascular injury, diagnostic modality of vascular injury detection, and classification of knee dislocation associated with vascular injury. For the purposes of this review, vascular injury was defined as occlusion, thrombosis, transection, intimal flap, or intimal tear. Arterial spasm alone was not classified as vascular injury. Nerve injury was defined as any reported injury to the nerves. Anatomic classification of knee dislocation resulting in vascular injury was also evaluated. Dislocations were classified either by Schenck classification, with Wascher modification (Table 1) [40], or by direction of tibial displacement relative to the femur (Kennedy system [18]) [14, 34].
Table 1.
Anatomic classification of knee dislocations using Schenck system with Wascher modification [40]
| Type | Description |
|---|---|
| KDI | Multiligamentous injury with either cruciate intact |
| KDII | Bicruciate injury only |
| KDIII | Multiligamentous injury involving rupture of bicruciate and either collateral |
| KDIIIM | Multiligamentous injury involving bicruciate and MCL rupture |
| KDIIIL | Multiligamentous injury involving bicruciate and LCL rupture |
| KDIV | Panligament rupture |
| KDV | Fractural dislocation |
MCL = medial collateral ligament; LCL = lateral collateral ligament.
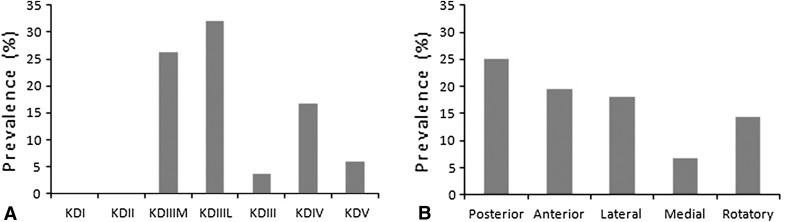
The Kennedy classification of knee dislocation uses tibial displacement relative to the femur and has five categories of dislocation: anterior, posterior, lateral, medial, and rotatory [18]. The Schenck classification is based on the number of ligaments ruptured and typically includes five classifications: KDI (both cruciate ligaments are intact), KDII (both cruciate ligaments only are ruptured), KDIII (one cruciate and one collateral ligament are ruptured), KDIV (panligament rupture), and KDV (fractural dislocation) [37]. With Wascher modification, the lateral ligament ruptured is specified, and two additional classifications are included: KDIIIM (one cruciate and medial collateral ligament ruptured) and KDIIIL (one cruciate and lateral collateral ligament ruptured) (Table 1) [40]. Thus, knee dislocations are reported as KDIII where studies used Schenck classification and reported as KDIIIM/KDIIIL where Schenck classification with Wascher modification was used. Seven studies totaling 584 knee dislocations reported on the classification of knee dislocation, with three studies using directional (Kennedy) classification, four studies using the Schenck classification system, and one study using both [2, 20, 27, 28, 33, 38, 39] (Table 2). According to the Schenck classification, 27 patients were identified with KDI knee dislocations, two with KDII dislocations, 19 with KDIIIM dislocations, 28 with KDIIIL dislocations, 55 with KDIII dislocations, 72 with KDIV dislocations, and 51 with KDV dislocations. No patients with KDI dislocations, no patients with KDII dislocations, five patients with KDIIIM dislocations, nine patients with KDIIIL dislocations, two patients with KDIII dislocations, 12 patients with KDIV dislocations, and three patients with KDV dislocations sustained vascular injury after knee dislocation. According to the Kennedy classification, 132 patients sustained posterior knee dislocations, 128 anterior dislocations, 50 lateral dislocations, 30 medial dislocations, and seven rotatory dislocations. Thirty-three posterior dislocations, 25 anterior dislocations, nine lateral dislocations, two medial dislocations, and one rotatory dislocation resulted in vascular injury.
Table 2.
Prevalence of vascular injury after knee dislocation by Schenck or directional (Kennedy) classification
| Study | Prevalence of vascular injury (%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Schenck classification | Kennedy classification | |||||||||||
| KDI | KDII | KDIIIM | KDIIIL | KDIII | KDIV | KDV | Posterior | Anterior | Lateral | Medial | Rotatory | |
| Azar et al. [2] (2011) | 0 | 0 | 43 | 33 | 60 | 100 | 38 | 0 | ||||
| Klineberg et al. [20] (2004) | 33 | 20 | 0 | |||||||||
| McDonough and Wojtys [27] (2009) | 0 | 0 | 17 | 32 | 14 | 0 | ||||||
| Mills et al. [28] (2004) | 33 | 42 | 0 | 0 | ||||||||
| Nicandri et al. [33] (2010) | 0 | 0 | 3 | 10 | 6 | |||||||
| Stannard et al. [38] (2004) | 0 | 0 | 2 | 16 | 3 | |||||||
| Treiman et al. [39] (1992) | 31 | 19 | 27 | 7 | 14 | |||||||
Using the collected data, we determined frequency of vascular injury after knee dislocation and which vessels were primarily injured. Twenty studies totaling 862 patients reported the frequency of vascular injury after knee dislocation [2, 4, 6, 8, 11, 14, 17, 19, 20, 22, 27–29, 33, 35, 36, 38, 39, 41, 44]. Three studies totaling 57 patients only reported data for patients with confirmed vascular injury and consequently could not be used to calculate a vascular injury frequency [1, 34, 45]. Twenty studies totaling 833 patients specified the vessels injured [1, 2, 4, 6, 11, 17, 19, 20, 22, 27–29, 33, 34, 36, 38, 39, 41, 44, 45]. We then stratified the frequency of vascular injury after knee dislocation based on knee dislocation classification. The frequency of nerve injury was also determined. Ten studies totaling 272 patients reported the frequency of nerve injury after knee dislocation [1, 2, 4, 6, 11, 19, 35, 36, 41, 44]. No assessment as to which classification of knee dislocation more commonly resulted in nerve injury was made. The frequency of surgical repair of the vascular injuries was determined, as well as the amputation rate, reasons for amputation, and frequency of each reason. Sixteen studies totaling 160 patients with vascular injury after knee dislocation reported the number of patients that underwent vascular repair [1, 2, 4, 6, 11, 14, 17, 19, 20, 28, 29, 33–36, 39], and 13 studies totaling 134 patients reported amputation information [2, 4, 8, 11, 14, 27–29, 33, 35, 38, 41, 44]. Finally, we evaluated the types of imaging modalities used to detect vascular injury and determined the frequency of each type. Twenty-one studies totaling 873 patients reported on the diagnostic modalities [1, 2, 4, 6, 11, 14, 17, 19, 20, 22, 27–29, 33–36, 38, 39, 41, 45].
The Newcastle-Ottawa Scale was used to evaluate the quality of the nonrandomized cohort studies used in this systematic review. This scale uses a star system to assess three study characteristics: (1) selection, (2) comparability, and (3) outcomes. An article of the worst possible quality would be awarded zero stars, while an article of the best possible quality would be awarded nine stars [42]. Six studies scored six stars, while 17 scored seven stars (Table 3).
Table 3.
Incidence of vascular and nerve injuries after knee dislocation
| Study | Number of knee dislocations* | Vascular injury (%) | Nerve injury (%) | Vessel injured (%) | Vascular injuries surgically repaired (%) | Amputation rate (%) | Study quality (number of quality stars)† |
|---|---|---|---|---|---|---|---|
| Alberty et al. [1] (1981) | 20 | 15 | PA (100) | 50 | 6 | ||
| Azar et al. [2] (2011) | 17 | 41 | 41 | PA (100) | 100 | 9 | 6 |
| Boisrenoult et al. [4] (2009) | 67 | 12 | 44 | PA (100) | 44 | 26 | 7 |
| Bui et al. [6] (2008) | 20 | 5 | 5 | PA (100) | 100 | 7 | |
| Frassica et al. [8] (1991) | 17 | 59 | 11 | 7 | |||
| Harner et al. [11] (2004) | 47 | 11 | 9 | PA (100) | 83 | 16 | 7 |
| Ibrahim et al. [14] (2008) | 36 | 14 | 100 | 22 | 6 | ||
| Kendall et al. [17] (1993) | 35 | 16 | PA (100) | 100 | 7 | ||
| King et al. [19] (2009) | 7 | 43 | 43 | PA (100) | 67 | 7 | |
| Klineberg et al. [20] (2004) | 55 | 22 | PA (92) SFA (8) |
50 | 7 | ||
| Levy et al. [22] (2010) | 9 | 22 | PA (100) | 7 | |||
| McDonough and Wojtys [27] (2009) | 72 (71) | 17 | PA (100) | 14 | 7 | ||
| Mills et al. [28] (2004) | 51 | 29 | PA (82) SFA (9) ATA (9) CFA (9) |
100 | 4 | 7 | |
| Miranda et al. [29] (2002) | 35 | 17 | PA (100) | 100 | 29 | 7 | |
| Nicandri et al. [33] (2010) | 31 | 19 | PA (100) | 67 | 40 | 7 | |
| Patterson et al. [34] (2007) | 18 | PA (94) ATA (6) |
100 | 6 | |||
| Potter et al. [35] (2002) | 21 | 10 | 48 | 100 | 17 | 7 | |
| Rios et al. [36] (2003) | 28 | 7 | 23 | PA (100) | 100 | 7 | |
| Stannard et al. [38] (2004) | 134 (126) | 7 | PA (100) | 16 | 7 | ||
| Treiman et al. [39] (1992) | 115 | 39 | PA (87) MGA (7) ATA (4) PTA (4) |
95 | 7 | ||
| Wascher et al. [41] (1997) | 47 (44) | 22 | 16 | PA (100) | 6 | 7 | |
| Wright et al. [44] (1995) | 18 | 26 | 37 | PA (100) | 17 | 6 | |
| Yahya et al. [45] (2005) | 19 | PA (100) | 89 | 6 |
* Studies with bilateral knee dislocations also give a patient count in parentheses; †the Newcastle-Ottawa Scale [42] was used to evaluate the quality of the studies used in this systematic review; an article of the worst possible quality would be awarded zero stars, while an article of the best possible quality would be awarded nine stars; PA = popliteal artery; SFA = superficial femoral artery; ATA = anterior tibial artery; CFA = common femoral artery; MGA = medial genticular artery; PTA = posterior tibial artery.
Statistics
A random-effects model was used to generate weighted averages and to assess the heterogeneity among studies for all quantitative measures, including frequency rates of vascular injury, nerve injury, surgical repair after vascular injury, and amputation after vascular injury [7, 30] (Table 3). Standard error for rates was presented as 95% CIs. Standard error was used because we wished to determine the degree to which each study’s reported injury frequency (sample mean) differed from the overall injury frequency (population mean), in contrast to the SD, which would only describe the degree to which individuals within each study differed from that study’s frequency. Cochrane I2 values were tabulated for quantitative measures and values of 25%, 50%, and 75% were classified as low, moderate, or high, respectively, according to the Cochrane Statistical Methods Group [12]. Heterogeneity is the existence of underlying differences between studies beyond chance alone. Cochrane I2 expresses, as a percentage, the total variation across studies due to heterogeneity. An I2 value of 0% indicates that all observed differences are due to chance (no heterogeneity), while a value of 100% indicates complete inconsistency between studies [30]. Heterogeneity among the studies for frequency rates ranged from low for vascular injury, nerve injury, and amputation rate to moderate for rate of surgical repair.
Results
The frequency of vascular injury after knee dislocation was 18% (171 of 862 patients; 95% CI, 12.8%–22.2%; I2 = 4.5%) (Fig. 2). The frequency of nerve injuries was 25% (75 of 272 patients; 95% CI, 13.9%–35.7%; I2 = 0.4%). We also found that the type of knee dislocation was associated with the likelihood of a vascular injury; the Schenck and Kennedy classifications with the highest vascular injury prevalence were KDIIIL (32%) (nine of 28) and posterior dislocation (25%) (33 of 132), respectively (Fig. 3). Of two KDII dislocations reported in this study, one was due to ultra-low-velocity dislocation in an obese patient and the other was unspecified. This is of importance because KDII dislocations are typically diagnosed in the chronic setting. As to the vessels injured, while the majority of studies reported injuries only to the popliteal artery (76%), other vessels included the medial genicular artery, anterior tibial artery, posterior tibial artery, superficial femoral artery, and common femoral artery (Table 3).
Fig. 2.
A Forest plot demonstrates the weighted combination of studies to calculate the vascular injury frequency (18%; 95% CI, 12.8%–22.2%).
Fig. 3A–B.
Prevalence of vascular injury after knee dislocation is shown, stratified by (A) Schenck classification and (B) Kennedy classification.
The large majority of patients in whom vascular injuries were diagnosed underwent surgical repair: 80% (134 of 160 patients; 95% CI, 72.8%–87.5%; I2 = 55.0%). Of these 134 patients, 22 underwent amputation, resulting in an amputation frequency of 12% (95% CI, 4.8%–19.3%; I2 = 0.0%) (Table 3). The majority (73%, 16 of 22) of amputations were performed due to infection or ischemia subsequent to failed vascular repair, while the remainder of amputations were performed at presentation due to prolonged ischemia or complete neurovascular disruption.
We found that, among diagnostic modalities, angiography was used most frequently (90% of studies), followed by duplex ultrasonography (24%), ABI (19%), and MR angiography (9.5%) (Table 4). Of 18 studies that reported on the use of selective versus routine angiography, only two studies recommended routine angiography on all patients presenting with knee dislocation [4, 27].
Table 4.
Diagnostic modalities used to detect vascular injury after knee dislocation
| Study | Ankle-brachial index | Angiography | Duplex | MR arthrography |
|---|---|---|---|---|
| Alberty et al. [1] (1981) | X | |||
| Azar et al. [2] (2011) | X | |||
| Boisrenoult et al. [4] (2009) | X | X | X | |
| Bui et al. [6] (2008) | X | |||
| Harner et al. [11] (2004) | X | |||
| Ibrahim et al. [14] (2008) | X | |||
| Kendall et al. [17] (1993) | X | |||
| King et al. [19] (2009) | X | |||
| Klineberg et al. [20] (2004) | X | |||
| Levy et al. [22] (2010) | X | X | ||
| McDonough and Wojtys [27] (2009) | X | |||
| Mills et al. [28] (2004) | X | X | X | |
| Miranda et al. [29] (2002) | X | |||
| Nicandri et al. [33] (2010) | X | X | ||
| Patterson et al. [34] (2007) | X | |||
| Potter et al. [35] (2002) | X | X | ||
| Rios et al. [36] (2003) | X | X | ||
| Stannard et al. [38] (2004) | X | |||
| Treiman et al. [39] (1992) | X | X | ||
| Wascher et al. [41] (1997) | X | |||
| Yahya et al. [45] (2005) | X | X |
Discussion
The morbidity associated with vascular injury after knee dislocation makes prompt diagnosis and treatment of these lesions critically important. The existing literature cites a wide range of frequency for these injuries and reveals a difference of opinion regarding the proper diagnostic evaluation. This review sought to determine the frequency of vascular and neurologic injury after knee dislocation, how often surgical intervention was performed for vascular injury in this setting, and the frequency with which each imaging modality was used for the detection of vascular injury.
This study is limited by the heterogeneity of the included studies. While heterogeneity tests (I2) were performed using a random-effects model, there are likely undetected differences that affect the reported results. For example, Azar et al. [2] included only obese patients with ultra-low-velocity knee dislocation, whereas the study of King et al. [19] consisted exclusively of open knee dislocations. This study is limited by the fact that results are split by the classifications used in the original study. In addition, our study is limited by a lack of outcome measures for diagnostic modalities or treatment options. A meta-analysis including outcome measures was attempted; however, outcome measures among different studies (ROM, IKDC score, Lysholm score) were too diverse to permit accurate combination and analysis. As with any systematic review, our data are limited by the quality of included studies.
The previously reported frequency of vascular injury is variable, with two large studies reporting a frequency of between 23% and 32% [10, 34]. In this review, studies with a majority of high-energy knee dislocations reported vascular injury frequencies between 7% and 43% [17, 19, 22, 27, 28, 33, 36, 38, 39, 41, 44], while those with a majority of low-energy dislocations (falls, sports injuries) reported frequencies of between 5% and 11% [6, 11]. One study of ultra-low-velocity knee dislocation in the obese had a vascular injury frequency of 41% [2]. The highest frequency was found in KDIIIL (32%) and posterior (25%) dislocations. KDIII injuries involve both cruciates and either collateral ligament. They usually represent higher-energy injuries, which can explain the higher frequency of vascular damage. Posterior dislocations are thought to produce shearing forces that result in intimal tearing and arterial transection, whereas anterior dislocations tend to cause arterial stretching injuries [39]. Nevertheless, because vascular injury can occur with any type of knee dislocation, it is imperative that every case be approached with the same diagnostic vigilance. In addition, predicting the risk of vascular injury based on directionality is made more difficult by the fact that many dislocations spontaneously reduce before presentation [9]. The popliteal artery is the most commonly injured vessel in the setting of knee dislocation because it is firmly anchored above and below the knee [34]. Of the 20 studies in our review reporting the vessels injured, all reported injury of the popliteal artery, either alone or in combination with other vessels.
We found that surgery was performed to treat vascular injuries in approximately 80% (134 of 160 patients), and the aggregate amputation frequency was 12% (22 of 134 patients). After surveying the data extracted from the literature, it is difficult to analyze what factors led to surgical repair because most studies did not mention specific indications for surgery in the setting of vascular injury. In addition, the circumstances surrounding cases of amputation were not explicitly stated. It has been shown that total ischemia time is directly correlated to rate of amputation [34]. The data in this review, however, did not consistently report time from injury to repair.
The best method for evaluating vascular injury in patients with knee dislocation is not so clear. The rationale behind the use of routine angiography, which was the historical approach but remains something that some authors advocate, is that physical examination findings can be misleading and that the consequences of a missed diagnosis can be catastrophic [25]. Patients with initially normal pulses or Doppler signals can eventually develop thromboses, leading to late vascular compromise [26]. Patterson et al. [34] and McCoy et al. [25] emphasized the association between normal peripheral pulses with intimal tears of the popliteal artery. Furthermore, McDonough and Wojtys [27] showed that physical examination alone failed to identify significant vascular injury. Angiography is not without its risks, however, which include hematoma, pseudoaneurysm, and arteriovenous fistula formation, as well as contrast-induced nephropathy [17, 24, 38]. Its use also adds to healthcare costs and increases the time for surgical treatment if performed in cases where there is hard evidence of vascular injury (distal ischemia, active hemorrhage, or expanding pulsatile hematoma) [38]. Some studies have also found false-positive results with the use of angiography ranging from 2.4% to 7%, leading to unnecessary surgical procedures and possible iatrogenic arterial or neurologic injury [23, 36, 38]. For these reasons, many authors now favor a number of selective angiography tests. Nicandri et al. [33] recommended pedal pulse examination and at least one imaging modality over an observation period of a minimum 24 hours. A less invasive study used in detecting popliteal artery injury when compared to arteriography is ABI. In addition to its safety, reproducibility, and economic considerations, it has been shown to be 95% to 100% sensitive and 80% to 100% specific in detecting vascular injuries requiring surgical repair [24]. Boisrenoult et al. [4] recommended immediate dislocation reduction if necessary, followed by ABI, and subsequent arteriogram or MR arthrography on all patients with knee dislocation, regardless of ABI findings. In addition, all patients who presented with abnormal ABI were evaluated with duplex ultrasound, another noninvasive imagining modality being explored in this setting, before arteriogram [4]. Levy et al. [22] used ABI both before and after reduction of dislocation, followed by arteriogram for patients with abnormal ABI or hard signs of vascular injury. Other studies surveyed included similar recommendations for reduction followed by pulse examination with ABI or duplex and arteriogram or immediate surgical exploration for those with abnormal findings [2, 11, 17, 28, 34, 35, 38, 39, 41, 45]. MR arthrography also shows potential in this setting through its convenience of including venous contrast while conducting a conventional MRI to evaluate ligamentous injury [15], though more studies are needed to determine its effectiveness in an acute setting.
Knee dislocations are relatively uncommon injuries and subsequent vascular injury occurs only in a subset of these; this relative rarity, combined with their potentially profound morbidity, means that clinicians must be especially vigilant in their diagnosis. Nonetheless, these potentially limb-threatening injuries continue to represent a diagnostic and treatment challenge to the clinician handling them. This study enhances our understanding of the frequency of vascular and nerve injuries after knee dislocation and of the diagnostic and treatment options available to physicians. The information shown here serves to illustrate the great difficulty clinicians face in determining the most effective method needed to determine vascular injury. In the current study, it was shown that posterior dislocations have a higher likelihood of concomitant vascular compromise. As such, the clinician should have an especially heightened clinical suspicion in this setting and should err on the side of caution in ruling out arterial injury. The best approach to evaluate vascular injury in this setting remains an incompletely answered question with the existing body of literature. Future studies should focus on prospective examination of different diagnostic and treatment modalities in the management of knee dislocation, with particular focus on outcomes after vascular injury. In addition, the role of MR arthrography versus angiography should be investigated, as the former can obviate the need for an additional invasive procedure.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
This work was performed at University of California–Los Angeles, Los Angeles, CA, USA.
References
- 1.Alberty RE, Goodfried G, Boyden AM. Popliteal artery injury with fractural dislocation of the knee. Am J Surg. 1981;142:36–40. doi: 10.1016/S0002-9610(81)80008-6. [DOI] [PubMed] [Google Scholar]
- 2.Azar FM, Brandt JC, Miller RH, 3rd, Phillips BB. Ultra-low-velocity knee dislocations. Am J Sports Med. 2011;39:2170–2174. doi: 10.1177/0363546511414855. [DOI] [PubMed] [Google Scholar]
- 3.Barnes CJ, Pietrobon R, Higgins LD. Does the pulse examination in patients with traumatic knee dislocation predict a surgical arterial injury? A meta-analysis. J Trauma. 2002;53:1109–1114. doi: 10.1097/00005373-200212000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Boisrenoult P, Lustig S, Bonneviale P, Leray E, Versier G, Neyret P, Rosset P, Saragaglia D. Vascular lesions associated with bicruciate and knee dislocation ligamentous injury. Orthop Traumatol Surg Res. 2009;95:621–626. doi: 10.1016/j.otsr.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 5.Brautigan B, Johnson DL. The epidemiology of knee dislocations. Clin Sports Med. 2000;19:387–397. doi: 10.1016/S0278-5919(05)70213-1. [DOI] [PubMed] [Google Scholar]
- 6.Bui KL, Ilaslan H, Parker RD, Sundaram M. Knee dislocations: a magnetic resonance imaging study correlated with clinical and operative findings. Skeletal Radiol. 2008;37:653–661. doi: 10.1007/s00256-008-0490-z. [DOI] [PubMed] [Google Scholar]
- 7.Egger M, Smith GD, Phillips AN. Meta-analysis: principles and procedures. BMJ. 1997;315:1533–1537. doi: 10.1136/bmj.315.7121.1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frassica FJ, Sim FH, Staeheli JW, Pairolero PC. Dislocation of the knee. Clin Orthop Relat Res. 1991;263:200–205. [PubMed] [Google Scholar]
- 9.Good L, Johnson R. The dislocated knee. J Am Acad Orthop Surg. 1995;3:284–292. doi: 10.5435/00124635-199509000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Green NE, Allen BL. Vascular injuries associated with dislocation of the knee. J Bone Joint Surg Am. 1977;59:236–239. [PubMed] [Google Scholar]
- 11.Harner CD, Waltrip RL, Bennett CH, Francis KA, Cole B, Irrgang JJ. Surgical management of knee dislocations. J Bone Joint Surg Am. 2004;86:262–273. doi: 10.2106/00004623-200402000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hollis JD, Daley BJ. 10-year review of knee dislocations: is arteriography always necessary? J Trauma. 2005;59:672–675; discussion 675–676. [PubMed]
- 14.Ibrahim SA, Ahmad FH, Salah M, Al Misfer AR, Ghaffer SA, Khirat S. Surgical management of traumatic knee dislocation. Arthroscopy. 2008;24:178–187. doi: 10.1016/j.arthro.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 15.Johnson ME, Foster L, DeLee JC. Neurologic and vascular injuries associated with knee ligament injuries. Am J Sports Med. 2008;36:2448–2462. doi: 10.1177/0363546508325669. [DOI] [PubMed] [Google Scholar]
- 16.Kaufman SL, Martin LG. Arterial injuries associated with complete dislocation of the knee. Radiology. 1992;184:153–155. doi: 10.1148/radiology.184.1.1609074. [DOI] [PubMed] [Google Scholar]
- 17.Kendall RW, Taylor DC, Salvian AJ, O’Brien PJ. The role of arteriography in assessing vascular injuries associated with dislocations of the knee. J Trauma. 1993;35:875–878. doi: 10.1097/00005373-199312000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Kennedy JC. Complete dislocation of the knee joint. J Bone Joint Surg Am. 1963;45:889–904. [PubMed] [Google Scholar]
- 19.King JJ, 3rd, Cerynik DL, Blair JA, Harding SP, Tom JA. Surgical outcomes after traumatic open knee dislocation. Knee Surg Sports Traumatol Arthrosc. 2009;17:1027–1032. doi: 10.1007/s00167-009-0721-4. [DOI] [PubMed] [Google Scholar]
- 20.Klineberg EO, Crites BM, Flinn WR, Archibald JD, Moorman CT., 3rd The role of arteriography in assessing popliteal artery injury in knee dislocations. J Trauma. 2004;56:786–790. doi: 10.1097/01.TA.0000075346.05460.D6. [DOI] [PubMed] [Google Scholar]
- 21.Kropman RH, Kiela G, Moll FL, de Vries JP. Variations in anatomy of the popliteal artery and its side branches. Vasc Endovascular Surg. 2011;45:536–540. doi: 10.1177/1538574411409065. [DOI] [PubMed] [Google Scholar]
- 22.Levy BA, Krych AJ, Shah JP, Morgan JA, Stuart MJ. Staged protocol for initial management of the dislocated knee. Knee Surg Sports Traumatol Arthrosc. 2010;18:1630–1637. doi: 10.1007/s00167-010-1209-y. [DOI] [PubMed] [Google Scholar]
- 23.Lohmann M, Lauridsen K, Vedel P. Arterial lesions in major knee trauma: pedal pulse a false sign of security? Arch Orthop Trauma Surg. 1990;109:238–239. doi: 10.1007/BF00453151. [DOI] [PubMed] [Google Scholar]
- 24.Martinez D, Sweatman K, Thompson EC. Popliteal artery injury associated with knee dislocations. Am Surg. 2001;67:165–167. [PubMed] [Google Scholar]
- 25.McCoy GF, Hannon DG, Barr RJ, Templeton J. Vascular injury associated with low-velocity dislocations of the knee. J Bone Joint Surg Br. 1987;69:285–287. doi: 10.1302/0301-620X.69B2.3818761. [DOI] [PubMed] [Google Scholar]
- 26.McCutchan JD, Gillham NR. Injury to the popliteal artery associated with dislocation of the knee: palpable distal pulses do not negate the requirement for arteriography. Injury. 1989;20:307–310. doi: 10.1016/0020-1383(89)90180-0. [DOI] [PubMed] [Google Scholar]
- 27.McDonough EB, Jr, Wojtys EM. Multiligamentous injuries of the knee and associated vascular injuries. Am J Sports Med. 2009;37:156–159. doi: 10.1177/0363546508324313. [DOI] [PubMed] [Google Scholar]
- 28.Mills WJ, Barei DP, McNair P. The value of the ankle-brachial index for diagnosing arterial injury after knee dislocation: a prospective study. J Trauma. 2004;56:1261–1265. doi: 10.1097/01.TA.0000068995.63201.0B. [DOI] [PubMed] [Google Scholar]
- 29.Miranda FE, Dennis JW, Veldenz HC, Dovgan PS, Frykberg ER. Confirmation of the safety and accuracy of physical examination in the evaluation of knee dislocation for injury of the popliteal artery: a prospective study. J Trauma. 2002;52:247–251; discussion 251–252. [DOI] [PubMed]
- 30.Neyeloff JL, Fuchs SC, Moreira LB. Meta-analyses and Forest plots using a Microsoft Excel spreadsheet: step-by-step guide focusing on descriptive data analysis. BMC Research Notes. 2012;5:52. doi: 10.1186/1756-0500-5-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Niall DM, Nutton RW, Keating JF. Palsy of the common peroneal nerve after traumatic dislocation of the knee. J Bone Joint Surg Br. 2005;87:664–667. doi: 10.1302/0301-620X.87B5.15607. [DOI] [PubMed] [Google Scholar]
- 32.Nicandri GT, Chamberlain AM, Wahl CJ. Practical management of knee dislocations: a selective angiography protocol to detect limb-threatening vascular injuries. Clin J Sport Med. 2009;19:125–129. doi: 10.1097/JSM.0b013e31819cd37a. [DOI] [PubMed] [Google Scholar]
- 33.Nicandri GT, Dunbar RP, Wahl CJ. Are evidence-based protocols which identify vascular injury associated with knee dislocation underutilized? Knee Surg Sports Traumatol Arthrosc. 2010;18:1005–1012. doi: 10.1007/s00167-009-0918-6. [DOI] [PubMed] [Google Scholar]
- 34.Patterson BM, Agel J, Swiontkowski MF, Mackenzie EJ, Bosse MJ. Knee dislocations with vascular injury: outcomes in the Lower Extremity Assessment Project (LEAP) Study. J Trauma. 2007;63:855–858. doi: 10.1097/TA.0b013e31806915a7. [DOI] [PubMed] [Google Scholar]
- 35.Potter HG, Weinstein M, Allen AA, Wickiewicz TL, Helfet DL. Magnetic resonance imaging of the multiple-ligament injured knee. J Orthop Trauma. 2002;16:330–339. doi: 10.1097/00005131-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 36.Ríos A, Villa A, Fahandezh H, de José C, Vaquero J. Results after treatment of traumatic knee dislocations: a report of 26 cases. J Trauma. 2003;55:489–494. doi: 10.1097/01.TA.0000043921.09208.76. [DOI] [PubMed] [Google Scholar]
- 37.Schenck RJ. Classification of knee dislocations. In: Fanelli GC, editor. The Multiple Ligament Injured Knee. New York, NY: Springer; 2004. pp. 37–49. [Google Scholar]
- 38.Stannard JP, Sheils TM, Lopez-Ben RR, McGwin G, Jr, Robinson JT, Volgas DA. Vascular injuries in knee dislocations: the role of physical examination in determining the need for arteriography. J Bone Joint Surg Am. 2004;86:910–915. [PubMed] [Google Scholar]
- 39.Treiman GS, Yellin AE, Weaver FA, Wang S, Ghalambor N, Barlow W, Snyder B, Pentecost MJ. Examination of the patient with a knee dislocation. The case for selective arteriography. Arch Surg. 1992;127:1056–1062; discussion 1062–1063. [DOI] [PubMed]
- 40.Wascher DC. High-velocity knee dislocation with vascular injury: treatment principles. Clin Sports Med. 2000;19:457–477. doi: 10.1016/S0278-5919(05)70218-0. [DOI] [PubMed] [Google Scholar]
- 41.Wascher DC, Dvirnak PC, DeCoster TA. Knee dislocation: initial assessment and implications for treatment. J Orthop Trauma. 1997;11:525–529. doi: 10.1097/00005131-199710000-00011. [DOI] [PubMed] [Google Scholar]
- 42.Wells GA, Shea B, O’Connell D, Petersen J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses.
- 43.Wood MB. Peroneal nerve repair: surgical results. Clin Orthop Relat Res. 1991;267:206–210. [PubMed] [Google Scholar]
- 44.Wright DG, Covey DC, Born CT, Sadasivan KK. Open dislocation of the knee. J Orthop Trauma. 1995;9:135–140. doi: 10.1097/00005131-199504000-00008. [DOI] [PubMed] [Google Scholar]
- 45.Yahya MM, Mwipatayi BP, Abbas M, Rao S, Sieunarine K. Popliteal artery injury: Royal Perth experience and literature review. ANZ J Surg. 2005;75:882–886. doi: 10.1111/j.1445-2197.2005.03550.x. [DOI] [PubMed] [Google Scholar]