Abstract
Background
Use of cementless hip replacements is increasing in many countries, but the best method for fixation for octogenarian patients remains unknown.
Questions/purposes
We studied how fixation method (cemented, cementless, hybrid) affects the survival of primary hip replacements and mortality in patients 80 years or older. Specifically, we asked if fixation method affects (1) the risk of revision; (2) the reasons for revision; and (3) the mortality after contemporary primary hip replacement in octogenarian patients.
Methods
A total of 4777 primary total hip replacements were performed in 4509 octogenarian patients with primary osteoarthritis in Finland between 1998 and 2009 and were registered in the Finnish Arthroplasty Register. Comorbidity data were collected from a nationwide quality register. Survival of hip replacements, using any revision as the end point, and mortality were analyzed using competing risks survival analysis and Cox regression analysis. The average followup was 4 years (range, 1–13 years).
Results
Cementless hip replacements were associated with a higher rate of early (within 1 year) revision compared with cemented hip replacements (hazard ratio, 2.9; 95% CI, 1.7–5.1), particularly in women. The difference was not explained by comorbidity or provider-related factors. Periprosthetic fracture was the leading mode of failure of cementless hip replacements. After 1 year, there were no differences in the survival rates although 10-year survival was slightly lower for cementless than cemented and hybrid hip replacements (93.9% [95% CI, 91.1%–96.7%] versus 97.4% [95% CI, 96.9%–98.0%] and 98.1% [95% CI, 96.9%–99.4%], respectively). Fixation method was not associated with mortality.
Conclusions
Cementless fixation was associated with an increased risk of revision and did not provide any benefit in terms of lower mortality in octogenarian patients.
Level of Evidence
Level II, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
Cemented THA is considered the gold standard in the management of late-stage osteoarthritis in older patients [20, 32, 33], with the 10- to 20-year survival rates exceeding 90% in patients 75 years and older [17, 21]. Cementless fixation, however, has gained popularity worldwide and also in the oldest patient groups [3, 20, 36], although its advantages over cemented fixation remain largely unproven [1, 5, 35].
The claimed advantages of cementless fixation, including faster surgery and potentially reducing cardiopulmonary stress and risk of embolization related to the use of cement, sound particularly appealing for older patients who often have several chronic diseases. However, some evidence suggests that the possible advantage of cementless over cemented hip replacements in implant survival is lost when patients are older than 75 years [17]. The reports of arthroplasty registers, recently reviewed by Troelsen et al. [36], report consistently higher rates of revision after cementless than cemented hip replacements in the oldest age groups. However, cemented fixation was associated with slightly higher mortality in a study based on the National Joint Registry of England and Wales data [18]. Nevertheless, it was considered the most cost-effective alternative in women 80 years and older [25]. However, comorbidities can act as confounding factors in these studies because they may affect the selection of the fixation method and mortality.
Because revision hip replacements are associated with greater surgical complexity and morbidity [4], longer recovery [4], and frequent need for subsequent reoperations [22], avoiding revisions is of utmost importance in octogenarians, who have reduced reserves to manage surgery-related stress [37]. Although the reported survival rates (Table 1) leave little room for improvement, some studies were performed in single orthopaedic units limiting the generalizability of their results. To our knowledge, only one register-based study compared different fixation methods [21]. In that study, the cementless hip replacements (used in 6.5% of operations) had poorer survival than hip replacements with hybrid fixation (95% versus 98% at 5 years), whereas cemented fixation did not differ from the two alternatives.
Table 1.
Reported survival of primary hip replacements in octogenarian patients
| Study | Number of hips/patients | Average age (years) | Prosthesis type | Average followup (range) | Survival rate (%) |
|---|---|---|---|---|---|
| Keisu et al. [15] | 123/114 (92/86 with complete followup) | 83 | Cementless acetabular component, cementless stem (collarless, tapered) | 5 years (2–11 years) | 100 |
| Kennedy et al. [16] | 510/510 (complete followup for 412/412) | 84 | Various cemented prostheses in 464 cases, cementless Bicontact® Plasmapore®* in 46 hips | 5.9 years | 98.6 (versus 96.2 in comparison group) |
| Ogino et al. [21] | 6989/6540 | 82.7 | Numerous different prostheses | Not reported | 5 years: 97 (95% CI, 96–97), 10 years: 94 (95% CI, 93–95) |
| Pieringer et al. [26] | 87/80 | 82.9 | Cementless stem + various cementless cups | 69.3 months (39–94 months) | 94.3 (95% CI, 73.9–99.4) |
| Stroh et al. [31] | 35/33 | 85 | Proximally coated tapered cementless implant | 48 months (24–90 months) | 97 (versus 94 in the comparison group) |
| Wurtz et al. [38] | 46/40 | 83 | Cemented stem, cementless cup | 48 months (1–128 months) | 100 (but 3 had liner exchange) |
* Bicontact® Plasmapore® (Aesculap Orthopaedics, B. Braun Melsungen AG, Melsungen Germany).
We therefore studied how fixation method (cemented, cementless, hybrid) affects the survival of primary hip replacements and mortality in patients 80 years and older. Specifically, we asked if fixation method affects (1) the risk of revision; (2) the reasons for revision; and (3) the mortality after contemporary primary hip replacement in octogenarian patients with osteoarthritis using records of a nationwide quality register with comprehensive comorbidity data.
Patients and Methods
We included primary THAs performed as a result of primary osteoarthritis in patients 80 years and older at the time of surgery in Finland between 1998 and 2009 in this observational arthroplasty register-based study. The data regarding these operations were collected from the nationwide PERFECT (PERFormance Effectiveness and Cost of Treatment episodes) database maintained by the Finnish Institute for Welfare and Health [19]. The database was created by combining data from several Finnish health registers, and its purpose is to provide nationwide up-to-date data regarding the outcomes of hip and knee replacements. The Finnish Arthroplasty Register is the main source for joint replacement-related data, but the database includes some hip and knee replacements identified from the records of the Hospital Discharge Register based on surgical procedure codes. In our study, revision joint replacements were identified from the Finnish Arthroplasty Register and were linked to a corresponding primary operation based on each citizen’s identification number and data regarding the surgically treated joint. Reporting to the Finnish Arthroplasty Register is mandatory for operating units and its coverage exceeds 95% (for primary operations).
In addition to surgery-related data, the database includes comprehensive comorbidity data collected from the Hospital Discharge Register and drug registers of the Social Insurance Institute of Finland [23]. Since 1987, the Hospital Discharge Register has kept records of hospitalizations in public and private hospitals. Comorbidities were identified based on diagnosis codes from these discharge records. The drug registers include data regarding prescriptions delivered from pharmacies since 1994 and allowances for reimbursement for medications for certain chronic diseases (like diabetes and coronary heart disease) since 1964. All registers have nationwide coverage, and in the Finnish publicly funded healthcare system, insurance status does not affect access to health care. Together these registers cover inpatient and outpatient care. Patients without any record indicating presence of a comorbid condition in these registers were considered free of that comorbidity. The PERFECT methodology and definitions for different comorbid conditions have been described and discussed [13, 23].
Of the 53,136 primary hip replacements recorded in the PERFECT database [19], 5400 were performed in octogenarian patients. After exclusion of THAs not recorded in the Finnish Arthroplasty Register [27] (and therefore lacking data regarding the side surgically treated, implanted prosthesis, and fixation method; n = 193), operations with missing data regarding implanted prostheses (n = 162), THAs with reverse hybrid fixation (n = 137), and hip replacements with resurfacing stem and/or cup (n = 131), 4777 primary THAs were included in our study, representing 6% (4777 of 79,880) of all primary hip replacements performed during the observation period (according to the Finnish Arthroplasty Register) and 9% of primary hip replacements included in the PERFECT database. No exclusions were made because of lack of comorbidity data. The percentage of octogenarian patients of all primary hip replacement recipients remained relatively constant during the observation period (varying between 5% and 7%), as did the annual incidence of hip replacements (185 per 100,000 in 1998 and 192 per 100,000 in 2009), except a peak at 236 per 100,000 in 2005 to 2006.
For the analyses, the data were divided into three groups according to the fixation of the hip replacement: (fully) cemented, (fully) cementless, and hybrid (cemented stem with cementless cup). In addition to this primary analysis, we repeated the analyses according to type (cemented, cementless) of fixation of femoral stems and acetabular cups.
There were no differences in baseline characteristics between the patient groups (Table 2). Cementless and hybrid fixation were used more frequently in central and other (including private) hospitals than in university hospitals.
Table 2.
Patient characteristics, medical history, and operation-related data according to fixation method
| Patient characteristics and operative data | Cemented (n = 3811), number (%) or median (range) | Cementless (n = 464), number (%) or median (range) | Hybrid (n = 502), number (%) or median (range) | p value |
|---|---|---|---|---|
| Average age (years) | 82 (80–102) | 82 (80–93) | 82 (80–95) | 0.464 |
| Sex | 0.135 | |||
| Male | 1064 (27.9) | 150 (32.3) | 145 (28.9) | |
| Female | 2747 (72.1) | 314 (67.7) | 357 (71.1) | |
| Comorbid diseases | ||||
| Hypertension | 2145 (56.3) | 263 (56.7) | 284 (56.6) | 0.981 |
| Cardiovascular disease | 1286 (33.7) | 174 (37.5) | 168 (33.5) | 0.260 |
| Diabetes | 327 (8.6) | 43 (9.3) | 43 (8.6) | 0.882 |
| Cancer | 343 (9.0) | 49 (10.6) | 48 (9.6) | 0.526 |
| Pulmonary disease | 383 (10.0) | 52 (11.2) | 61 (11.2) | 0.289 |
| Depression | 300 (7.9) | 27 (5.8) | 34 (6.8) | 0.224 |
| Psychotic disorder | 89 (2.3) | 10 (2.1) | 7 (1.4) | 0.403 |
| Dementia | 81 (2.1) | 13 (2.8) | 12 (2.4) | 0.623 |
| Any of the above | 2856 (74.9) | 357 (76.9) | 117 (76.7) | 0.482 |
| Previous joint replacements (contralateral hip and/or either knee) | 1336 (35.1) | 168 (36.2) | 170 (33.9) | 0.747 |
| Previous replacement of contralateral hip | 1025 (26.9) | 133 (28.7) | 123 (24.5) | 0.335 |
| Operating hospital | < 0.001 | |||
| University hospital | 1071 (28.1) | 82 (17.7) | 98 (19.5) | |
| Central hospital | 1304 (34.2) | 221 (47.6) | 240 (47.8) | |
| District hospital | 822 (21.6) | 32 (6.9) | 77 (15.3) | |
| Other (including private hospitals) | 614 (16.1) | 129 (27.8) | 87 (17.3) | |
| Same-day bilateral hip replacement | 16 (0.4) | 8 (1.7) | 1 (0.2) | 0.004 |
| Intravenous antibiotic prophylaxis (data missing for 56 operations) | 3695 (97.0) | 441 (95.0) | 485 (96.6) | 0.012 |
| Duration of perioperative hospitalization (days)* | 13 (0–4728) | 13 (0–2997) | 14 (0–2908) | 0.008 |
| Proportion of patients still hospitalized 90 days after surgery | 122 (3.2) | 19 (4.1) | 19 (3.8) | 0.509 |
* In 103 patients the length of perioperative hospitalization exceeded 1 year. Most of these patients probably are waiting for a place in a long-term care facility or are institutionalized at healthcare center wards.
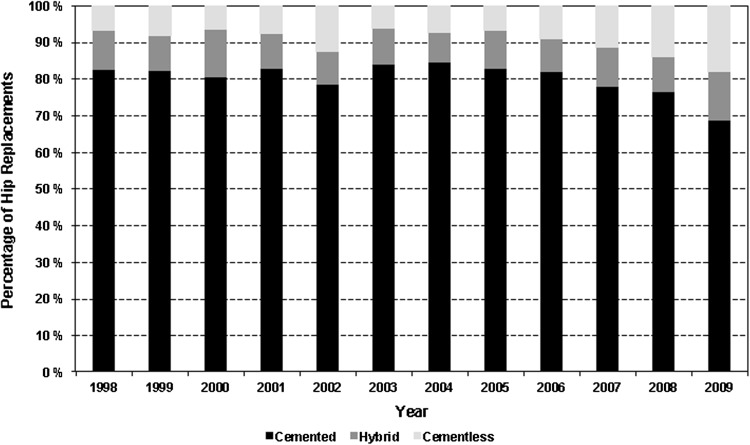
The use of cemented fixation decreased from 82% in 1998 to 69% in 2009 (p < 0.001) (Fig. 1). The trend was similar for femoral stems (from 93% to 82%; p < 0.001) and acetabular cups (from 82% to 69%; p < 0.001). There was considerable variation in the use of different fixation methods in octogenarian patients across the 20 hospital districts with the percentage of cementless hip replacements varying from 1% to 44%. In 1998, cementless fixation was not used in 12 hospital districts, but in 2009, it was being used in 18 of 20 hospital districts.
Fig. 1.
Changes in the use of cemented, hybrid, and cementless fixation in primary hip replacements performed in octogenarian patients with osteoarthritis from 1998 to 2009 are shown.
Exeter™ Universal (n = 1907; Stryker, Mahwah, NJ, USA), Spectron™ EF (n = 808; Smith & Nephew, Memphis, TN, USA), and Lubinus® SP II® (n = 760; Waldermar Link, Hamburg, Germany) were the most frequently used femoral stems in the cemented hip replacements. The most commonly used cementless stems were the Biomet® collarless (n = 103; Biomet, Warsaw, IN, USA), ABG™ II (n = 98; Stryker), and ABG™ HA (n = 49; Stryker). In the hybrid group, Exeter™ Universal accounted for 56% (n = 283) of femoral stems followed by Spectron™ EF (n = 84) and Lubinus® SP II® (n = 46). There were 11 specific stem-cup combinations that were used more than 48 times (ie, in more than 1% of all operations). These 11 combinations together accounted for 3670 cases (77%) of all operations included in our series (Table 3).
Table 3.
Stem-cup combinations used in more than 1% of the operations
| Femoral stem | Acetabular cup | Number (percent of all operations) |
|---|---|---|
| ABG™ II (Stryker, Mahwah, NJ, USA) | ABG™ II (Stryker, Mahwah, NJ, USA) | 56 (1.2) |
| Biomet® collarless (Biomet, Warsaw, IN, USA) | Biomet® Vision® (Biomet, Warsaw, IN, USA) | 56 (1.2) |
| Elite Plus™ Flanged (DePuy, Warsaw, IN, USA) | Elite Plus™ LPW (DePuy, Warsaw, IN, USA) | 55 (1.2) |
| Exeter™ Universal (Stryker, Mahwah, NJ, USA) | Contemporary (Stryker, Mahwah, NJ, USA) | 1308 (27.4) |
| Exeter™ All-polyethylene (Stryker, Mahwah, NJ, USA) | 564 (11.8) | |
| Omnifit™ Trident™ (Stryker, Mahwah, NJ, USA) | 91 (1.9) | |
| Lubinus® SP II® (Waldermar Link, Hamburg, Germany) | Link® FC (Waldermar Link, Hamburg, Germany) | 163 (3.4) |
| Link® IP (Waldermar Link, Hamburg, Germany) | 275 (5.8) | |
| Lubinus® Eccentric (Waldermar Link, Hamburg, Germany) | 280 (5.9) | |
| Spectron™ EF (Smith & Nephew, Memphis, TN, USA) | Reflection® All-polyethylene (Smith & Nephew, Memphis, TN, USA) | 771 (16.1) |
| Reflection® Interfit™ (Smith & Nephew, Memphis, TN, USA) | 51 (1.1) |
Outcomes
The primary endpoint was revision for any reason, defined as removal or exchange of any of the prosthesis components, as recorded in the Finnish Arthroplasty Register. Early failure rate (within 1 year after primary operation, as reasoned in the Statistics section) and the reasons for revision were reported separately. Mortality (90-day, 1-year, and overall) and the risk for revision resulting from aseptic loosening, infection, periprosthetic fracture, and dislocation were analyzed as secondary outcomes.
Statistics
The patients with joint replacements were followed up until December 31, 2010, resulting in a minimum followup of 1 year unless revision or death occurred before.
Baseline characteristics and prevalence of comorbid conditions were compared among patients with cemented, cementless, and hybrid hip replacements using the Kruskal-Wallis test for continuous variables and the chi-square test for categorical variables.
The survival without revision was calculated using cumulative incidence function (competing risks survival analysis). This technique was chosen because Kaplan-Meier analysis is known to overestimate survival rates where mortality (ie, competing risk) is high [28]. Cox regression analysis was used to compare the risk of revision, presented as hazard ratio (HR) with 95% CIs, among the different fixation methods. The same methods were used to analyze overall mortality. The chi-square test and Fisher’s exact test were used for comparison of mortality at 90 days and 1 year and reasons for revision across the groups.
Fulfillment of the proportional hazards assumption in the Cox models was investigated by inspecting log-minus-log curves and partial residual plots (against time). Because proportional hazards assumption was violated in the comparisons between cemented and cementless hip replacements and in the comparisons between cemented and cementless femoral stems and acetabular cups, the HRs in the comparisons of fixation methods were calculated splitting the followup into 0 to 1 year and greater than 1 year. Given the observed high early failure rate, this division was considered clinically reasonable. Proportional hazards assumption was met in all analyses concerning mortality.
The Cox analyses were first performed without adjustments. The analyses then were repeated with adjustment for age, gender, type of operating hospital (university, central, district, other), year of operation (to account for the effect of wider introduction of cementless fixation), a bivariate variable indicating whether the prosthesis was one of the most used models (Table 3), and presence of the eight comorbid conditions (hypertension, cardiovascular disease, chronic pulmonary disease, history of cancer, diabetes, depression, dementia, and psychotic disorders; each separately). This fully adjusted model was used as it gave similar results than a similar model lacking comorbidity data. The results based on this fully adjusted model are referred to as multivariate analysis.
As a sensitivity analysis, we repeated the regression analyses (1) with adjustment for age and sex; with inclusion of (2) only unilateral joint replacements where intravenous antibiotic prophylaxis was used; (3) only unilateral hip replacements that were the patient’s only hip replacements registered in the Finnish Arthroplasty Register between 1980 and 2010; (4) only stem-cup combinations used more than 48 times during the observation period; (5) only operations from hospital districts where cementless hip replacements were used in more than 10% of all cases (indicating routine use); and (6) only operations performed in hospital districts where cementless hip replacements were performed already in the beginning of the observation period (ie, in 1998, to minimize the effects of introduction of a new technique [24]). In addition, we conducted analyses concerning 1-year mortality with stratification by sex, presence of comorbid conditions (with, without), type of operating hospital, and year of operation (1998–2003, 2004–2009).
The creation and use of the PERFECT database [19] for research purposes was approved by the ethics committee of the National Institute for Health and Welfare. The research plan for our study was approved by the institutional review board of the same institution.
Results
Risk of Revision
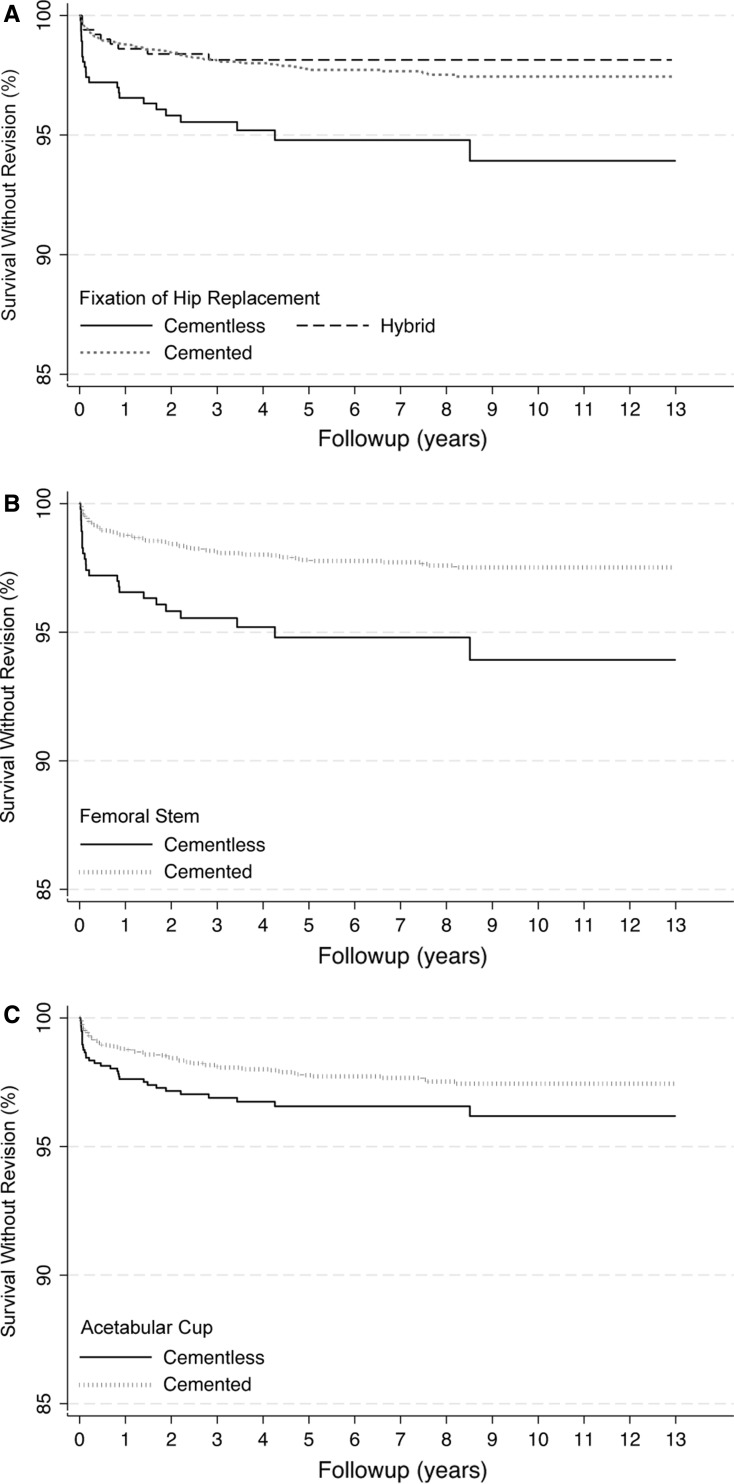
During the followup averaging 4 years (range, 0–13 years), 116 revisions were registered, 69 (59%) of which occurred during the first postoperative year. Cementless hip replacements had worse survival than cemented and hybrid hip replacements (Fig. 2A). Ten years postoperatively 6.1% of cementless THAs were revised compared with 2.6% and 1.9% of cemented and hybrid THAs (Table 4). Cementless hip replacements were especially associated with a high risk of early failure (HR, 2.9; 95% CI, 1.7–5.1; p < 0.001, compared with cemented hip replacements). The trend was similar in the comparison of cemented and cementless femoral stems and acetabular cups (Fig. 2B–C). Cementless femoral stems had a 1.7-fold risk (95% CI, 1.3–2.2; p < 0.001) and cementless acetabular cups had a 1.4-fold risk (95% CI, 1.1–1.8; p = 0.007) of early revision, compared with their cemented counterparts. After 1 year, no statistically significant differences were observed among different fixation methods (Table 4).
Fig. 2A–C.
The curves indicate survival without revision after (A) cemented, hybrid, and cementless hip replacement, and (B) in association with the use of cemented and cementless femoral stems and (C) acetabular cups.
Table 4.
Effect of fixation method on survival of hip replacements
| Fixation method | Survival without revision | Risk of revision | ||||
|---|---|---|---|---|---|---|
| 1 year (%) (95% CI) |
3 years (%) (95% CI) |
5 years (%) (95% CI) |
10 years (%) (95% CI) |
0–1 years HR (95% CI) |
More than 1 year HR (95% CI) |
|
| Type of hip replacement | ||||||
| Cemented | 98.8 (98.4–99.2) | 98.1 (97.7–98.6) | 97.8 (97.3–98.3) | 97.4 (96.9–98.0) | 1 | 1 |
| Cementless | 96.6 (94.9–98.3) | 95.5 (93.6–97.5) | 94.8 (92.6–97.0) | 93.9 (91.1–96.7) | 2.91 (1.65–5.13) | 1.83 (0.82–4.10) |
| Hybrid | 98.6 (97.6–99.7) | 98.1 (96.9–99.4) | 98.1 (96.9–99.4) | 98.1 (96.9–99.4) | 1.16 (0.52–2.56) | 0.41 (0.10–1.69) |
| Fixation of femoral stem | ||||||
| Cemented | 98.8 (98.4–99.1) | 98.1 (97.7–98.5) | 97.8 (97.3–98.3) | 97.2 (97.0–98.1) | 1 | 1 |
| Cementless | 96.6 (94.9–98.3) | 95.5 (93.6–97.5) | 94.8 (92.6–97.0) | 93.9 (91.1–96.7) | 1.69 (1.28–2.23) | 1.40 (0.94–2.09) |
| Fixation of acetabular cup | ||||||
| Cemented | 98.8 (98.4–99.2) | 98.1 (97.7–98.6) | 97.8 (97.3–98.3) | 97.4 (96.9–98.0) | 1 | 1 |
| Cementless | 97.6 (96.6–98.6) | 96.9 (95.8–98.0) | 96.6 (95.3–97.8) | 96.2 (94.7–97.6) | 1.41 (1.10–1.81) | 1.02 (0.71–1.46) |
HR = hazard ratio.
The differences in the risk of early revision between cementless and cemented hip replacements (multivariate HR, 2.8; 95% CI, 1.3–5.9; p = 0.007) and cementless and cemented femoral stems (multivariate HR, 1.6; 95% CI, 1.2–2.3; p = 0.005) remained statistically significant in the multivariate analysis. The trend was similar in the analysis of acetabular cups but the difference did not reach statistical significance (multivariate HR, 1.4; 95% CI, 0.99–2.0; p = 0.058).
Cementless fixation showed a twofold or greater risk of early revision compared with cemented hip replacements in the sensitivity analyses, although with a reduced number of cases included, statistical significance was not achieved in all analyses (Table 5). In a post hoc subgroup analysis, cementless fixation was strongly associated with the risk of early revision in women (multivariate HR, 3.5; 95% CI, 1.2–9.7; p = 0.018). In men, cementless fixation was not associated with early revision (multivariate HR, 2.1; 95% CI, 0.7–6.4; p = 0.202), but contradicting the original analysis, there was a trend suggesting an increase in the risk of late revision (multivariate HR, 3.8; 95% CI, 0.9–16.4; p = 0.078). The difference between sexes was not explained by patient characteristics or type of operating hospitals.
Table 5.
Results of the sensitivity analyses
| Sensitivity analysis | Number of hips | Risk of revision | ||||
|---|---|---|---|---|---|---|
| Cementless versus cemented | Hybrid versus cemented | |||||
| Total | Revised | HR for early revision (95% CI) | HR for late revision (95% CI) | HR for early revision (95% CI) | HR for late revision (95% CI) | |
| Inclusion of unilateral hip replacements with the use of intravenous antibiotic prophylaxis | 4597 | 112 | 3.07 (1.74–5.43) | 1.99 (0.88–4.47) | 1.01 (0.43–2.37) | 0.42 (0.10–1.76) |
| Inclusion of unilateral hip replacements that were the only hip replacements of the patients between 1980 and 2010 | 3097 | 71 | 4.44 (2.18–8.72) | 2.02 (0.78–5.27) | 0.62 (0.15–2.60) | 0.57 (0.13–2.39) |
| Inclusion of operations with the most commonly used stem-cup pairs | 3670 | 80 | 5.85 (2.61–13.11) | .08 (0.50–8.68) | 0.67 (0.09–4.93) | N/A |
| Inclusion of surgery performed in hospital districts where cementless fixation was used in more than 10% of cases | 1056 | 21 | 2.16 (0.44–10.70) | 1.81 (0.63–5.21) | 1.09 (0.11–10.52) | N/A |
| Inclusion of operations from hospital districts where cementless hip replacements were used already in the beginning of the observation period | 1501 | 34 | 2.44 (0.86–6.91) | 2.84 (0.98–8.18) | 0.83 (0.11–.640) | N/A |
The results are expressed as hazard ratios (HRs) (with 95% CIs); N/A = could not be calculated because of insufficient number of cases/endpoint.
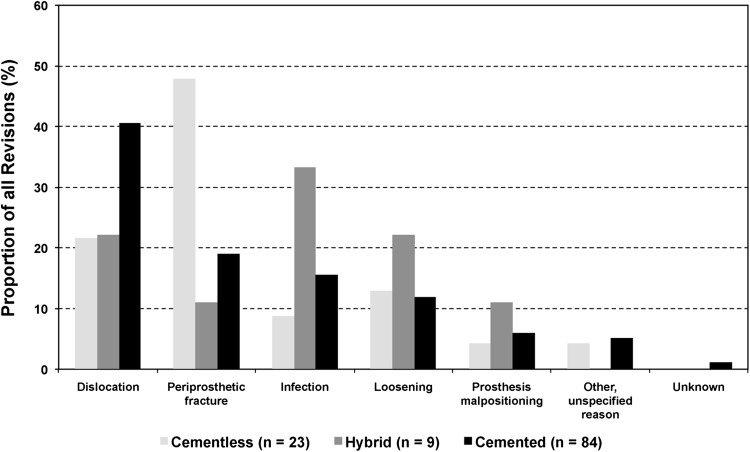
Reasons for Revision
The reasons for revision differed across the groups (p = 0.047): periprosthetic fracture was the leading mode of failure after cementless hip replacement and dislocation was the most common diagnosis leading to revision after cemented hip replacement (Fig. 3). The distribution of reasons for revision was similar in early revisions where periprosthetic fracture was the most common reason for early revision after cementless hip replacements (50% [eight of 16] versus 11% [five of 46] after cemented hip replacement; p = 0.024). In Cox analysis, fixation method did not affect the risk of early revision resulting from dislocation or infection (data not shown), but cementless hip replacements had a higher risk of early revision resulting from periprosthetic fracture (HR, 13.4; 95% CI, 4.4–40.8; p < 0.001) than cemented hip replacements. In women, significantly more revisions were the result of periprosthetic fracture after cementless than cemented or hybrid hip replacement (67% [eight of 12] versus 18% [10 of 57] and 0% [zero of five], respectively; p = 0.033). As such, sex was not associated with the risk of revision resulting from periprosthetic fracture, dislocation, or infection (data not shown).
Fig. 3.
The reasons for revision after primary hip replacement with cemented, cementless, and hybrid fixation are shown.
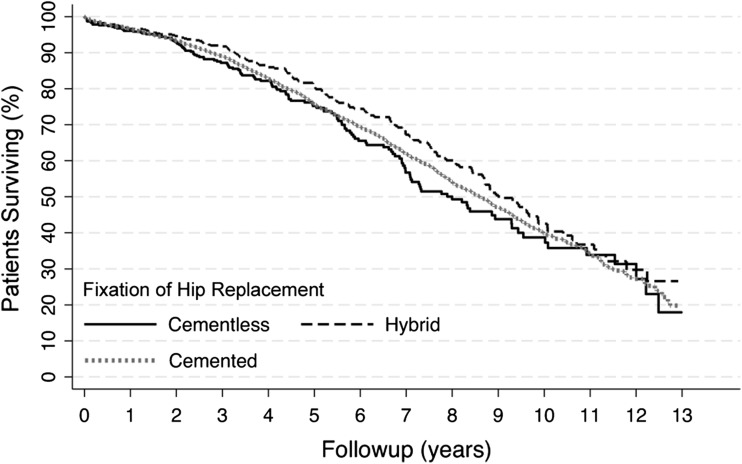
Mortality
There were no differences in mortality after cemented, cementless, and hybrid hip replacements at 90 days (1.2%, 1.5%, and 1.0%, respectively; p = 0.755) and 1 year (2.9%, 3.2%, and 2.6%; p = 0.837). No differences in long-term mortality were noted either (Fig. 4), the HRs for death being 1.1 (95% CI, 0.96–1.3; p = 0.151) and 0.89 (95% CI, 0.8–1.04; p = 0.131) for cementless and hybrid compared with cemented hip replacements, respectively. Cementless fixation was not found to have a protective effect in light of the 1-year mortality in any of the subgroup analyses (according to presence of comorbid conditions) (data not shown).
Fig. 4.
The graph shows mortality after cemented, hybrid, and cementless primary THA.
Discussion
Cementless hip replacements are being performed increasingly (Fig. 1) [3, 11, 20, 36], although the scientific rationale for advocating cementless over cemented fixation is questionable particularly in the oldest age groups [1, 5, 35, 36]. However, some of the oldest patients might benefit from avoiding the stress related to the cementing procedure, although this has not been proven. In this nationwide register-based study, we found a high early failure rate of cementless primary THAs in octogenarian patients with osteoarthritis. Women, in particular, were at high risk for early revision. Cementless fixation provided no benefit in terms of mortality or length of perioperative hospitalization. The available comorbidity data indicate that our results are not explained by differences in patient characteristics.
When interpreting our results, certain limitations should be kept in mind. First, we could not identify clinical failures that did not lead to revision. Not all older patients are suitable or willing to undergo surgery, which leads to overestimation of survival rates and leveling of the survival curves as followup increases (Fig. 2). As this effect becomes greater as followup increases, withholding from revision surgery is an unlikely explanation for observed differences in early revision rates. Second, we could not identify periprosthetic fractures already treated in the primary surgery group. Such fractures occur in at least 1% of primary operations with higher frequency in cementless than cemented hip replacements [7, 8, 20, 34] and are associated with considerable morbidity [30]. In addition, periprosthetic fractures that are treated with means other than revision hip replacement, eg, with osteosynthesis, could not be detected from the arthoplasty register data. Unregistered fractures lead to underestimation of the true failure rate and may level the differences between the studied fixation methods. Third, despite our nationwide data and followup of up to 13 years, the numbers of hip replacements and particularly revisions were relatively small, so especially in the sensitivity analyses there is risk of obtaining false-negative results. Although the multivariate analysis and the sensitivity analyses indicate that our results are robust against numerous confounding factors, we acknowledge that there are other, particularly patient-related, factors that may affect the durability of THAs but that cannot be taken into account using register-based data. Finally, it is possible that the high early failure rate of cementless THAs is partly related to increasing use of that technique and poorer outcomes on its introduction [24]. With lack of provider-related data and with the available case numbers, this issue could not be investigated in detail.
The 10-year survival rate exceeding 97% after cemented and hybrid hip replacements is in accordance with previous reports (Table 1) and suggests a slight improvement compared with an earlier study from the Finnish Arthroplasty Register where the overall 10-year survival after hip replacements performed from 1980 to 2004 was 94% [21]. Contradicting some earlier series from single orthopaedic units [15, 31], cementless hip replacements were associated with a high early failure rate in our nationwide series. Cementless hip replacements also performed the worst in the study by Ogino et al. [21], but in that series, the early failure rate did not appear particularly high. More recently, findings similar to ours have been reported from other arthroplasty registers for the oldest age groups (patients older than 65–75 years) [3, 36]. After 1 year, cementless fixation no longer was associated with increased risk of revision, but it also was not associated with improved survival, leading to poorer survival rates at 5 to 10 years than with cemented and hybrid fixation. Age has not been shown to hamper the long-term outcome [12, 17], although in the long-term followup of a randomized trial comparing cemented versus cementless primary THA, cementless stems had poorer survival than cemented ones in patients older than 65 years [6]. In addition, the radiographic followup of octogenarian patients with cementless hip replacements indicates that stable fixation with bone ingrowth can be achieved in the oldest patients [15, 26, 31].
Periprosthetic fracture was the most common reason for revision of a cementless hip replacement. This is not surprising because older age, female sex, and cementless (femoral) fixation have been identified as risk factors for early (within 90 days) periprosthetic fracture [30]. The result also is in line with a report from Hailer et al. using the Swedish Hip Arthroplasty Register and including patients of all ages [10]. The underlying mechanism may be intraoperative fracture that may have remained undetected during the operation or subsidence of the cementless component postoperatively. Because older women are at particular risk, osteoporosis also could play some role, but existing literature regarding the effect of osteoporosis or osteopenia on the primary fixation of cementless hip replacements, or an occurrence of periprosthetic fracture, is contradictory [2, 29]. Allowing only partial weightbearing to avoid stem subsidence and consequent periprosthetic fracture, which has been suggested by some authors [2, 31], may be difficult for frail older patients and delay their recovery to independent activity after surgery. Another explanation for the poor outcome after cementless fixation is the learning curve experienced when a new technique or hip replacement is introduced for use by a certain surgeon or hospital [9, 24]. Certain hip replacements have clearer learning curves than others [24], but unfortunately with the small case numbers and the high number of different components used, we precluded comparison of different cementless hip replacement designs.
Contradicting an earlier report [18], we did not observe increased mortality in association with cemented fixation. Cementless fixation did not show any benefit in terms of mortality in any patient subgroup. This is in accordance with a single-center study involving similar patient cohorts [14]. It is possible that other operation-related factors that could not be studied in our register-based study, like blood loss and duration of operation, confound our results. The effect on mortality of undergoing an early revision warrants additional study.
Our results, together with previously reported data from other arthroplasty registers [18, 36], including a cost-effective analysis [25], suggest that cementless hip replacements cannot be recommended for octogenarian patients. Larger, possibly multinational studies are needed to investigate if the observed high early failure rate is related to some specific prosthesis design. The remarkable variation in the use of different fixation techniques indicates there is need for guidelines to harmonize treatment practices and thus help in avoiding unnecessary revisions in octogenarian patients.
Footnotes
One of the authors (EJ) has received funding from the Competitive State Research Financing of the Expert Responsibility Area of Tampere University Hospital (Tampere, Finland) (grant 9P016).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution waived approval for this investigation, and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Coxa, Hospital for Joint Replacement, Tampere, Finland.
References
- 1.Abdulkarim A, Ellanti P, Motterlini N, Fahey T, O’Byrne JM. Cemented versus uncemented fixation in total hip replacement: a systematic review and meta-analysis of randomized controlled trials. Orthop Rev (Pavia). 2013;5:e8. doi: 10.4081/or.2013.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aro HT, Alm JJ, Moritz N, Mäkinen TJ, Lankinen P. Low BMD affects initial stability and delays stem osseointegration in cementless total hip arthroplasty in women: a 2-year RSA study of 39 patients. Acta Orthop. 2012;83:107–114. doi: 10.3109/17453674.2012.678798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Australian Orthopaedic Association. National Joint Replacement Registry. Hip and knee arthroplasty. Annual report 2012. Available at: https://aoanjrr.dmac.adelaide.edu.au/documents/10180/60142/Annual%20Report%202012?version=1.3&t=1361226543157. Accessed July 30, 2013.
- 4.Bozic KJ, Durbhakula S, Berry DJ, Naessens JM, Rappaport K, Cisternas M, Saleh KJ, Rubash HE. Differences in patient and procedure characteristics and hospital resource use in primary and revision total joint arthroplasty: a multicenter study. J Arthroplasty. 2005;20(7 suppl 3):17–25. doi: 10.1016/j.arth.2005.04.021. [DOI] [PubMed] [Google Scholar]
- 5.Clement ND, Biant LC, Breusch SJ. Total hip arthroplasty: to cement or not to cement the acetabular socket? A critical review of the literature. Arch Orthop Trauma Surg. 2012;132:411–427. doi: 10.1007/s00402-011-1422-2. [DOI] [PubMed] [Google Scholar]
- 6.Corten K, Bourne RB, Charron KD, Au K, Rorabeck CH. What works best, a cemented or cementless primary total hip arthroplasty?: minimum 17-year followup of a randomized controlled trial. Clin Orthop Relat Res. 2011;469:209–217. doi: 10.1007/s11999-010-1459-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davidson D, Pike J, Garbuz D, Duncan CP, Masri BA. Intraoperative periprosthetic fractures during total hip arthroplasty: evaluation and management. J Bone Joint Surg Am. 2008;90:2000–2012. doi: 10.2106/JBJS.H.00331. [DOI] [PubMed] [Google Scholar]
- 8.Fernandez-Fernandez R, García-Elias E, Gil-Garay E. Peroperative fractures in uncemented total hip arthroplasty: results with a single design of stem implant. Int Orthop. 2008;32:307–313. doi: 10.1007/s00264-006-0318-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flamme CH, Stukenborg-Colsman C, Wirth CJ. Evaluation of the learning curves associated with uncemented primary total hip arthroplasty depending on the experience of the surgeon. Hip Int. 2006;16:191–197. doi: 10.1177/112070000601600302. [DOI] [PubMed] [Google Scholar]
- 10.Hailer NP, Garellick G, Kärrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthop. 2010;81:34–41. doi: 10.3109/17453671003685400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Havelin LI, Fenstad AM, Salomonsson R, Mehnert F, Furnes O, Overgaard S, Pedersen AB, Herberts P, Kärrholm J, Garellick G. The Nordic Arthroplasty Register Association: a unique collaboration between 3 national hip arthroplasty registries with 280,201 THRs. Acta Orthop. 2009;80:393–401. doi: 10.3109/17453670903039544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jameson SS, Baker PN, Mason J, Rymaszewska M, Gregg PJ, Deehan DJ, Reed MR. Independent predictors of failure up to 7.5 years after 35 386 single-brand cementless total hip replacements: a retrospective cohort study using National Joint Registry data. Bone Joint J. 2013;95:747–757. doi: 10.1302/0301-620X.95B6.31378. [DOI] [PubMed] [Google Scholar]
- 13.Jämsen E, Peltola M, Eskelinen A, Lehto MU. Comorbid diseases as predictors of survival of primary total hip and knee replacements: a nationwide register-based study of 96 754 operations on patients with primary osteoarthritis. Ann Rheum Dis. 2013;72:1975–1982. doi: 10.1136/annrheumdis-2012-202064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jämsen E, Puolakka T, Eskelinen A, Jäntti P, Kalliovalkama J, Nieminen J, Valvanne J. Predictors of mortality following primary hip and knee replacement in the aged: a single-center analysis of 1,998 primary hip and knee replacements for primary osteoarthritis. Acta Orthop. 2013;84:44–53. doi: 10.3109/17453674.2012.752691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Keisu KS, Orozco F, Sharkey PF, Hozack WJ, Rothman RH, McGuigan FX. Primary cementless total hip arthroplasty in octogenarians: two to eleven-year follow-up. J Bone Joint Surg Am. 2001;83:359–363. doi: 10.1302/0301-620X.83B3.11006. [DOI] [PubMed] [Google Scholar]
- 16.Kennedy JW, Johnston L, Cochrane L, Boscainos PJ. Outcomes of total hip arthroplasty in the octogenarian population. Surgeon. 2013;11:199–204. doi: 10.1016/j.surge.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 17.Mäkelä KT, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. Total hip arthroplasty for primary osteoarthritis in patients fifty-five years of age or older: an analysis of the Finnish arthroplasty registry. J Bone Joint Surg Am. 2008;90:2160–2170. doi: 10.2106/JBJS.G.00870. [DOI] [PubMed] [Google Scholar]
- 18.McMinn DJ, Snell KI, Daniel J, Treacy RB, Pynsent PB, Riley RD. Mortality and implant revision rates of hip arthroplasty in patients with osteoarthritis: registry based cohort study. BMJ. 2012;344:e3319. doi: 10.1136/bmj.e3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Institute for Health and Welfare. PERFECT – PERFormance, Effectiveness and Cost of Treatment episodes. Available at: www.thl.fi/en_US/web/en/project?id=21963 Accessed October 3, 2013.
- 20.National Joint Registry for England and Wales. 9th annual report 2012. Available at: http://www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/9th_annual_report/NJR%209th%20Annual%20Report%202012.pdf. Accessed July 30, 2013.
- 21.Ogino D, Kawaji H, Konttinen L, Lehto M, Rantanen P, Malmivaara A, Konttinen YT, Salo J. Total hip replacement in patients eighty years of age and older. J Bone Joint Surg Am. 2008;90:1884–1890. doi: 10.2106/JBJS.G.00147. [DOI] [PubMed] [Google Scholar]
- 22.Parvizi J, Pour AE, Keshavarzi NR, D’Apuzzo M, Sharkey PF, Hozack WJ. Revision total hip arthroplasty in octogenarians: a case-control study. J Bone Joint Surg Am. 2007;89:2612–2618. doi: 10.2106/JBJS.F.00881. [DOI] [PubMed] [Google Scholar]
- 23.Peltola M, Juntunen M, Häkkinen U, Rosenqvist G, Seppälä TT, Sund R. A methodological approach for register-based evaluation of cost and outcomes in health care. Ann Med. 2011;43(suppl 1):S4–S13. doi: 10.3109/07853890.2011.586364. [DOI] [PubMed] [Google Scholar]
- 24.Peltola M, Malmivaara A, Paavola M. Hip prosthesis introduction and early revision risk: a nationwide population-based study covering 39,125 operations. Acta Orthop. 2013;84:25–31. doi: 10.3109/17453674.2013.771299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pennington M, Grieve R, Sekhon JS, Gregg P, Black N, van der Meulen JH. Cemented, cementless, and hybrid prostheses for total hip replacement: cost effectiveness analysis. BMJ. 2013;346:f1026. doi: 10.1136/bmj.f1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pieringer H, Labek G, Auersperg V, Bohler N. Cementless total hip arthroplasty in patients older than 80 years of age. J Bone Joint Surg Br. 2003;85:641–645. [PubMed] [Google Scholar]
- 27.Puolakka TJ, Pajamäki KJ, Halonen PJ, Pulkkinen PO, Paavolainen P, Nevalainen JK. The Finnish Arthroplasty Register: report of the hip register. Acta Orthop Scand. 2001;72:433–441. doi: 10.1080/000164701753532745. [DOI] [PubMed] [Google Scholar]
- 28.Ranstam J, Kärrholm J, Pulkkinen P, Mäkelä K, Espehaug B, Pedersen AB, Mehnert F, Furnes O, NARA study group Statistical analysis of arthroplasty data: II. Guidelines. Acta Orthop. 2011;82:258–267. doi: 10.3109/17453674.2011.588863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rhyu KH, Lee SM, Chun YS, Kim KI, Cho YJ, Yoo MC. Does osteoporosis increase early subsidence of cementless double-tapered femoral stem in hip arthroplasty? J Arthroplasty. 2012;27:1305–1309. doi: 10.1016/j.arth.2011.10.026. [DOI] [PubMed] [Google Scholar]
- 30.Sheth NP, Brown NM, Moric M, Berger RA, Della Valle CJ. Operative treatment of early peri-prosthetic femur fractures following primary total hip arthroplasty. J Arthroplasty. 2013;28:286–291. doi: 10.1016/j.arth.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 31.Stroh DA, Zywiel MG, Johnson AJ, Mont MA. Excellent survivorship with the use of proximally coated tapered cementless stems for total hip arthroplasty in octogenarians. Geriatr Orthop Surg Rehabil. 2011;2:100–104. doi: 10.1177/2151458511406267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Swedish Hip Arthroplasty Register. Annual report 2011. Available at: http://www.shpr.se/Libraries/Documents/%c3%85rsrapport_2011_eng_webb.sflb.ashx. Accessed July 30, 2013.
- 33.The Norwegian Arthroplasty Register. Report June 2010. Available at: http://nrlweb.ihelse.net/eng/Report_2010.pdf. Accessed July 30, 2013.
- 34.Thillemann TM, Pedersen AB, Johnsen SP, Søballe K. Inferior outcome after intraoperative femoral fracture in total hip arthroplasty: outcome in 519 patients from the Danish Hip Arthroplasty Registry. Acta Orthop. 2008;79:327–334. doi: 10.1080/17453670710015210. [DOI] [PubMed] [Google Scholar]
- 35.Toossi N, Adeli B, Timperley AJ, Haddad FS, Maltenfort M, Parvizi J. Acetabular components in total hip arthroplasty: is there evidence that cementless fixation is better? J Bone Joint Surg Am. 2013;95:168–174. doi: 10.2106/JBJS.K.01652. [DOI] [PubMed] [Google Scholar]
- 36.Troelsen A, Malchau E, Sillesen N, Malchau H. A review of current fixation use and registry outcomes in total hip arthroplasty: the uncemented paradox. Clin Orthop Relat Res. 2013;471:2052–2059. doi: 10.1007/s11999-013-2941-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.White PF, White LM, Monk T, Jakobsson J, Raeder J, Mulroy MF, Bertini L, Torri G, Solca M, Pittoni G, Bettelli G. Perioperative care for the older outpatient undergoing ambulatory surgery. Anesth Analg. 2012;114:1190–1215. doi: 10.1213/ANE.0b013e31824f19b8. [DOI] [PubMed] [Google Scholar]
- 38.Wurtz LD, Feinberg JR, Capello WN, Meldrum R, Kay PJ. Elective primary total hip arthroplasty in octogenarians. J Gerontol A Biol Sci Med Sci. 2003;58:M468–M471. doi: 10.1093/gerona/58.5.M468. [DOI] [PubMed] [Google Scholar]