Abstract
Background
Reconstruction of the multiligament-injured knee often involves extended surgical and tourniquet use times and often is performed in patients who have sustained concomitant fractures as well as vascular injuries, all of which would appear to predispose the patient to the potentially serious complications of deep vein thrombosis and perhaps pulmonary embolism, yet little is known about the frequency of venous thromboembolic (VTE) events after multiligamentous knee reconstruction.
Questions/purposes
The purposes of this study were to (1) determine the frequency of symptomatic VTE after multiligamentous knee reconstruction at a single institution; and (2) to determine associated risk factors for VTE in these patients.
Methods
The records of 134 (63% of the 213 consented individuals in our longitudinal database) patients who underwent primary (129 [96%]) or revision (five [4%]) multiligamentous knee reconstruction at a single institution between 1992 and 2013 were retrospectively reviewed. With two patients undergoing procedures bilaterally, this resulted in a total of 136 multiligamentous knee reconstructions. VTE for which clinical symptoms were evident and confirmed by imaging within 3 months after the reconstructive procedure was noted. Pre- and perioperative data were collected with respect to demographics, associated injuries, medical history, smoking status, and surgical data. Standard rehabilitation and thromboprophylaxis protocols were used in all patients.
Results
Three cases of symptomatic VTE (three deep vein thromboses) occurred after the 136 reconstructions (2%; 95% confidence interval, 0.53%–7.3%). Two of the three patients were obese and the remaining patient smoked and abused alcohol. However, as a result of a low frequency of VTE, no risk factors could be identified in this series.
Conclusions
Symptomatic VTE occurred in 2% of multiligamentous knee reconstructions at our institution while receiving thromboprophylaxis. This is similar to rates documented after anterior cruciate ligament reconstruction without thromboprophylaxis. Further multicenter research is required to identify the true frequency of and risk factors for developing VTE in patients undergoing multiligamentous knee reconstruction after knee dislocation.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Usually secondary to an acute knee dislocation, the multiligament-injured knee is a complex orthopaedic injury to the soft tissues, ligaments, and neurovascular structures [15, 19, 27, 37, 39, 50, 52]. Reconstruction of the multiligament-injured knee often combines arthroscopic and open techniques [13, 15, 26], involves extended surgical and tourniquet use times, and is often performed in patients who have sustained concomitant fractures as well as vascular and/or neurologic injuries from the initial trauma [14, 25, 30, 33, 49]. As such, these patients are at risk of developing venous thromboembolism (VTE). Numerous reports have documented the frequency of and risk factors for developing a VTE after hip and knee arthroplasty, knee arthroscopy, lower extremity trauma, and even hip arthroscopy [2, 3, 5, 7, 16, 17, 29, 35, 41, 43, 45, 47]. However, data with regard to VTE after multiligamentous knee reconstruction are scarce [9].
For patients who undergo routine knee arthroscopy, the incidence of VTE without thromboprophylaxis has ranged from 0% to 17.9% [3, 6, 17, 53]. Given the high energy of the injury and surgical complexity of the multiligamentous knee reconstruction, the risk in these patients may be greater. In published studies for multiligamentous knee reconstruction, only one, to our knowledge, has reported on the complication of VTE, suggesting a frequency similar to that reported after arthroscopic anterior cruciate ligament (ACL) reconstruction [9]. To our knowledge, no paper has assessed risk factors for developing VTE in this patient population.
Therefore, the purposes of our study were to (1) determine the frequency of clinically symptomatic VTE after multiligamentous knee reconstruction; and (2) evaluate the potential risk factors associated with these events.
Patients and Methods
The study was approved by the institutional review board at our institution. Patients were retrospectively identified from a prospective database at our institution, which includes patients who sustained a knee dislocation with multiligamentous knee injury. From this group, all patients who subsequently underwent a multiligamentous knee reconstruction, including revisions, and consented to be part of the database were included. In addition, all patients included required at least 90 days of followup. Patients were excluded if they were skeletally immature or if they did not have adequate injury, periprocedural, or followup data. Review of our knee dislocation database identified 213 potential subjects, which ultimately resulted in a series of 134 patients (63%) who underwent multiligamentous knee reconstruction with two undergoing bilateral reconstructions, totaling 136 multiligamentous knee reconstructions between February 3, 1992, and February 13, 2013. The 79 excluded patients did not undergo a multiligamentous knee reconstruction (42 of 213 [20%]), were skeletally immature (one of 213 [0.5%]), or simply did not possess enough periprocedural or followup data (36 of 213 [17%]) to be included in the series. Five of the patients (4%) underwent revision reconstructions.
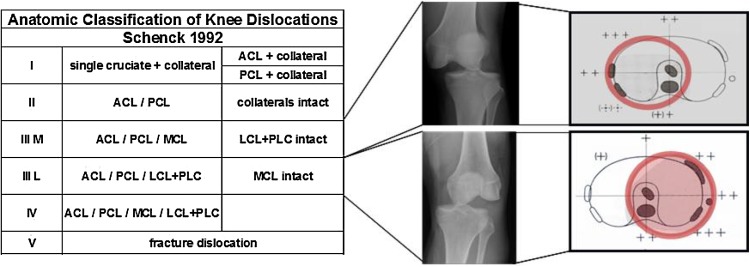
A multiligamentous knee injury was defined as one involving disruption of at least one of the cruciate ligaments and at least one of the collateral ligaments through the mechanism of a documented or presumed knee dislocation event based on imaging, history, and pattern. These injuries were then classified according to the system described by Wascher, which is a modification to the original KD (knee dislocation) classification system proposed by Schenck (Fig. 1) [36, 42, 51].
Fig. 1.
Anatomic classification of knee dislocations [36, 42, 51]. KD = knee dislocation; LCL = lateral collateral ligament; PLC = posterolateral corner. Reprinted from Peskun CJ, Levy BA, Fanelli GC, Stannard JP, Stuart MJ, MacDonald PB, Marx RG, Boyd JL, Whelan DB. Diagnosis and management of knee dislocations. Phys Sportsmed. 2010;38:101–111, with permission from JTE Multimedia.
All medical records were reviewed for the documentation of deep venous thrombosis (DVT) or pulmonary embolism (PE) after multiligamentous knee reconstruction. All patients presenting with clinically symptomatic signs of VTE underwent imaging (Doppler ultrasound) to positively confirm cases or further studies in scenarios where the diagnosis was still suspected despite a negative Doppler ultrasound. Occurrence of symptomatic VTE within 3 months of knee surgery was considered to be related to the surgery and was therefore included in our study [20, 22].
Before April 2007, all patients were prescribed 6 weeks of enteric-coated aspirin (ECA) for thromboprophylaxis after their reconstruction (35 reconstructions [26%]). Based on surgeon preference, from April 2007 on, thromboprophylaxis was in the form of 3 weeks of low-molecular-weight heparin (LMWH) followed by 3 weeks of ECA. For patients with a history of VTE before their injury or in those who developed a VTE from their initial knee dislocation event, they were referred to and assessed by the thrombophilia service to assist in determining the best regimen, which was either a similar protocol to the LMWH one mentioned or warfarin for 6 to 12 weeks based on their recommendations. All patients underwent a standardized postoperative rehabilitation protocol [8, 12].
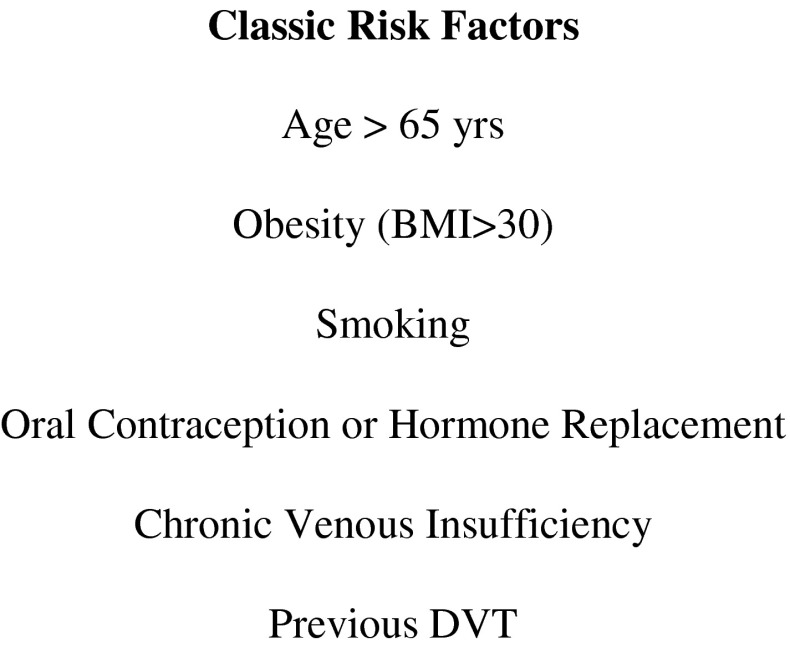
Data were collected by reviewing the medical record of each patient included in the study. Classic risk factors including age older than 65 years, obesity (body mass index [BMI] > 30 kg/m2), smoking, oral contraception or hormone replacement therapy, chronic venous insufficiency, and history of a previous DVT were all collected (Fig. 2) [6]. Furthermore, additional potential factors were documented such as sex and Deyo comorbidity score while taking into account any history of vascular, liver, oncologic, cardiac, cerebrovascular, or pulmonary disease. Most patients in the series were men (106 of 134 [79%]) and the mean age of all patients was 32 (range, 15–61 years; SD 11). The overall health of the patients in this series was rather good with only 11 (8%) of the patients possessing a Deyo comorbidity score of 1 or higher (Table 1). Injury and periprocedural parameters were also assessed including surgical and tourniquet use times and complications. Mechanisms of trauma for the entire population included 60 that involved motor vehicle/motorcycle/snowmobile accidents, 43 from sports-related injuries, seven from skiing/wakeboarding/rollerblading events, 16 fall/twisting injuries, and the remainder involving machinery, horses, and other miscellaneous causes. There were four patients with open injuries, 10 with vascular injuries and/or reconstructions, 19 who were placed in spanning external fixators, 10 patients who required fasciotomies, and 28 patients who sustained peroneal palsies (Table 2).
Fig. 2.
Classic risk factors as adapted from Delis et al. [6]. Adapted with permission from Delis KT, Hunt N, Strachan RK, Nicolaides AN. Incidence, natural history and risk factors of deep vein thrombosis in elective knee arthroscopy. Thromb Haemost. 2001;86:817–821.
Table 1.
Demographics
| Demographic | VTE group | No VTE group |
|---|---|---|
| Age (years) | 42 (median; range, 24–43) | 31 (mean; SD 11) |
| Mean of all: 32 (SD 11) | ||
| Sex (male:female) | 3:0 | 103:28 |
| BMI (kg/m2) | 35 (median; range, 28–42) | 30 (mean; SD 7) |
| Mean of all: 30 (SD 7) | ||
| Smoking | 33% (1/3) | 31% (40/131) |
| History of DVT | 0 | 5% (6/131) |
| Deyo comorbidity score ≥ 1 | 0 | 8% (11/131) |
All these risk factors were deemed nonsignificant; VTE = venous thromboembolism; BMI = body mass index; DVT = deep vein thrombosis.
Table 2.
Injury, periprocedural, and postoperative details
| Injury/surgical factors | VTE group | Non-VTE group* |
|---|---|---|
| (n = 3) | (n = 131) | |
| KD classification | ||
| I | 2 | 50 |
| II | – | 5 |
| III | 1 | 55 |
| IV | – | 14 |
| V | – | 12 |
| Time to MLKR (weeks) | 24 (median; range, 21–24) | 16 (median; range, 0–1374) |
| Open versus closed | 0 versus 3 | 4 versus 129 |
| Vascular injury | 0 | 10 |
| Peroneal palsy | 0 | 28 |
| Fasciotomies | 0 | 10 |
| External fixator | 0 | 19 |
| Acute versus delayed MLKR | 0 versus 3 | 18 versus 115 |
| Tourniquet time (minutes) | 78 (median; range, 63–93) | 102 (mean; SD 54) |
| Operative time (minutes) | 152 (median; range, 80–260) | 233 (mean; SD 76) |
| MUA | 0 | 10 |
All of these risk factors were deemed nonsignificant; * includes two patients who underwent bilateral reconstructions; VTE = venous thromboembolism; KD = knee dislocation; MLKR = multiligamentous knee reconstruction; MUA = manipulation under anesthesia.
The primary goal of this study was to estimate the frequency of symptomatic VTE after multiligamentous knee reconstruction. This was calculated as the number of patients diagnosed with a symptomatic VTE within 3 months of multiligamentous knee reconstruction divided by the total number of patients undergoing a multiligamentous knee reconstruction. This frequency is expressed as a percentage and is reported with a 95% confidence interval. Of additional interest was the comparison between those patients who had a VTE and those who did not with respect to potential risk factors including age, BMI, smoking status, medical history, open versus closed injury, placement of an external fixator, vascular and/or neurologic injury, and tourniquet and operative times. However, the small number of symptomatic VTE cases observed precluded formal statistical comparisons between the VTE and non-VTE groups. Therefore, differences between these groups are reported descriptively. All analyses were carried out using the JMP statistical software package (Version 8; SAS Institute Inc, Cary, NC, USA).
Results
After the multiligamentous knee reconstructions, three (2%; 95% confidence interval [CI], 0.53%–7.3%) patients with symptomatic VTE occurring within 3 months of surgery were identified. All were lower extremity DVTs on the operative side, and no patients developed a symptomatic PE. Median time to symptomatic VTE after reconstruction was 39 days (range, 7–80 days). Diagnosis was made by ultrasound in two of the patients with one of the patients requiring diagnosis through a venogram after ultrasound was reported as negative. All of the DVTs involved the posterior tibial and/or peroneal veins with only one involving the popliteal vein itself. Six patients in the non-VTE group had a history of DVT, all sequelae from their knee dislocation event, but none of these patients developed recurrence of their symptomatic DVT after reconstruction. Three of these patients were placed on LMWH, whereas the other three were placed on warfarin postoperatively for thromboprophylaxis.
Given the small number of symptomatic VTE events observed in this series, no risk factors could be identified, specifically with regard to age, sex, BMI, smoking status, history of DVT, or medical comorbidities (Table 1), because a robust analysis could not be performed given the lack of numbers. Similarly, analysis of potential injury and surgical factors such as time to reconstruction, open injuries, damage to neurovascular structures, performance of fasciotomies, application of an external fixator, or tourniquet or operative times could not identify any significant risk factors either (Table 2). All of the patients who developed VTE had sustained closed injuries, possessed no concomitant vascular or neurologic injuries accompanying their initial traumas, had tourniquet times of less than 120 minutes, and were primary reconstructions performed at least 3 weeks out from injury. They were all on the LMWH protocol after their surgery.
Discussion
VTE after lower extremity trauma and surgery is an unfortunate complication that can even result in death after simple knee arthroscopy [18, 34, 40]. The high-energy nature of a knee dislocation, required immobilization after injury, and subsequent surgical treatment rendered place each individual who sustains a multiligamentous knee injury at risk for developing a VTE [43]. However, few data exist regarding the frequency of VTE in patients who undergo multiligamentous knee reconstruction and less so with regard to potential risk factors that would make one more likely to develop a symptomatic VTE [9]. The frequency of symptomatic VTE in our series was 2% (95% CI, 0.53%–7.3%). Given the low frequency of the events in question, we could draw no inferences about the risk factors for symptomatic VTE in this population.
This study has a number of limitations. It reports on only clinically symptomatic VTE in patients undergoing multiligamentous knee reconstruction and thus it is likely we underestimated the frequency of VTE relative to what might have been discovered had a screening procedure such as ultrasound been used. For example, Ye et al. [55] found a rate of VTE in their patients undergoing arthroscopic ACL reconstruction of 14% diagnosed through screening venography; however, they did not comment on how many of these would have been diagnosed based on clinical symptoms only. As already mentioned, the low number of clinically symptomatic patients reported in our series made further statistical analysis impossible.
Our findings in terms of the frequency of VTE are consistent with the VTE frequency documented in the one other series of which we are aware of that studied patients who underwent multiligamentous knee reconstruction. Engebretsen et al. [9] reported on 85 patients who underwent surgical treatment of a KD II-V multiligamentous knee injury; of those, three (3.53%) developed a DVT. Numerous other cases series of patients who underwent multiligamentous knee reconstruction exist in the literature; however, many of them make no mention of the complication of VTE [15, 30, 37, 50]. The frequency of 2% in our series appears comparable to rates after arthroscopic ACL reconstruction [1, 3, 21, 48]. This may or may not be attributed to our approach of all patients receiving thromboprophylaxis after reconstruction. Camporese et al. [4] demonstrated a reduced rate of VTE in their patients who received LMWH, 1% versus 3% in those who received compression alone, after simple knee arthroscopy. Other published reports have revealed similar findings [31, 32, 54]. In a randomized trial evaluating the rate of VTE with the use of LMWH after ACL reconstruction, Marlovits et al. [28] had a reduced rate of VTE in the treatment group of 2.8% compared with 41.2% in the placebo group, but it is important to note that all their patients were screened for VTE. Despite the nature of the multiligamentous knee reconstruction being more complex and time-consuming than a standard arthroscopic ACL reconstruction, rates of symptomatic VTE appear similar between multiligamentous knee reconstruction with routine use of thromboprophylaxis and ACL reconstruction groups, which generally were managed without it.
In our series, of those patients who developed VTE, all possessed at least one classic risk factor for VTE as described by Delis et al. [6], with two being obese and the other possessing chronic tobacco use. However, given the severity of such trauma sustained and scope of surgery all patients in our series underwent, one could argue every one of our subjects possessed risk factors for development of a VTE. Additionally, in the group of patients who did not develop a symptomatic VTE, 45 (34%) had a BMI > 30 kg/m2, 40 (31%) of them smoked, and 71 (54%) had at least one classic risk factor. In a series of 85 patients who underwent knee arthroscopy, Williams et al. [53] found that 8.6% of the patients who possessed at least one classic risk factor were diagnosed with a clinically silent DVT compared with a rate of 1.6% in those who possessed no risk factors. Age has notably been documented as a risk factor for VTE after knee arthroscopy [16, 29]; however, with the younger age at which trauma such as knee dislocations usually occurs, it is difficult to assess how this affects the risk of VTE in the multiligamentous knee reconstruction population. To reiterate, given the lack of symptomatic VTE diagnosed in our series, further statistical analysis of the risk factors mentioned here was not possible. Despite our results not appearing to suggest a correlation with tourniquet use and symptomatic VTE, it is recommended to avoid the use of tourniquet compression in cases of multiligamentous knee reconstruction in which the patient underwent vascular repair with their initial trauma [7, 10, 38, 44, 46, 47].
We found that 2% (95% CI, 0.53%–7.3%) of patients who underwent multiligamentous knee reconstruction with routine thromboprophylaxis developed symptomatic VTE. Each patient with VTE had an identifiable risk factor, but large multicenter studies are needed to better assess the overall frequency and risk factors for development of symptomatic VTE after multiligamentous knee reconstruction. Based on our experience, we recommend that patients who sustain such trauma and undergo a multiligamentous knee reconstruction be placed on some form of thromboprophylaxis, with or without mechanical interventions, in accordance with American College of Chest Physicians guidelines regarding thromboprophylaxis after “major orthopaedic surgery” as a multiligamentous knee reconstruction would entail [11]. Given the rarity of such injuries [19, 23, 39], evolution of techniques and instrumentation over time [13, 26], and variation in application of functional and clinical outcome measures, conducting high-level research studies on multiligamentous knee injuries remains a challenge [23, 24].
Footnotes
One of the authors (BAL) is a consultant for Arthrex (Naples, FL, USA). One of the authors certifies that he or she (BAL, DLD, MJS) or a member of his or her immediate family, has or may receive payments or benefits, during the study period, an amount of less than USD 10,000 as part of the editorial board for CORR® (Deputy Editor), USD 10,000–100,000 from Arthrex, Inc, and USD 10,000–100,000 from Tenex Health (Lake Forest, CA, USA). One of the authors (BAL) receives research support from Stryker (Mahwah, NJ, USA), Biomet (Warsaw, IN, USA), and Arthrex; and is part of the editorial boards for Arthroscopy (Board of Trustees), Knee Surgery Sports Traumatology and Arthroscopy, and Journal of Knee Surgery. One of the authors (MJS) is a consultant for Arthrex and receives research support from Stryker and the USA Hockey Foundation.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Adala R, Anand A, Kodikal G. Deep vein thrombosis and thromboprophylaxis in arthroscopic anterior cruciate ligament reconstruction. Indian J Orthop. 2011;45:450–453. doi: 10.4103/0019-5413.82347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berry DJ. Surveillance for venous thromboembolic disease after total knee arthroplasty. Clin Orthop Relat Res. 2001;392:257–266. doi: 10.1097/00003086-200111000-00033. [DOI] [PubMed] [Google Scholar]
- 3.Bushnell BD, Anz AW, Bert JM. Venous thromboembolism in lower extremity arthroscopy. Arthroscopy. 2008;24:604–611. doi: 10.1016/j.arthro.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 4.Camporese G, Bernardi E, Prandoni P, Noventa F, Verlato F, Simioni P, Ntita K, Salmistraro G, Frangos C, Rossi F, Cordova R, Franz F, Zucchetta P, Kontothanassis D, Andreozzi GM. Low-molecular-weight heparin versus compression stockings for thromboprophylaxis after knee arthroscopy: a randomized trial. Ann Intern Med. 2008;149:73–82. doi: 10.7326/0003-4819-149-2-200807150-00003. [DOI] [PubMed] [Google Scholar]
- 5.Dahl OE, Gudmundsen TE, Haukeland L. Late occurring clinical deep vein thrombosis in joint-operated patients. Acta Orthop Scand. 2000;71:47–50. doi: 10.1080/00016470052943883. [DOI] [PubMed] [Google Scholar]
- 6.Delis KT, Hunt N, Strachan RK, Nicolaides AN. Incidence, natural history and risk factors of deep vein thrombosis in elective knee arthroscopy. Thromb Haemost. 2001;86:817–821. [PubMed] [Google Scholar]
- 7.Demers C, Marcoux S, Ginsberg JS, Laroche F, Cloutier R, Poulin J. Incidence of venographically proved deep vein thrombosis after knee arthroscopy. Arch Intern Med. 1998;158:47–50. doi: 10.1001/archinte.158.1.47. [DOI] [PubMed] [Google Scholar]
- 8.Edson CJ, Fanelli GC, Beck JD. Rehabilitation after multiple-ligament reconstruction of the knee. Sports Med Arthrosc. 2011;19:162–166. doi: 10.1097/JSA.0b013e31821918b2. [DOI] [PubMed] [Google Scholar]
- 9.Engebretsen L, Risberg MA, Robertson B, Ludvigsen TC, Johansen S. Outcome after knee dislocations: a 2–9 years follow-up of 85 consecutive patients. Knee Surg Sports Traumatol Arthrosc. 2009;17:1013–1026. doi: 10.1007/s00167-009-0869-y. [DOI] [PubMed] [Google Scholar]
- 10.Fahmy NR, Patel DG. Hemostatic changes and postoperative deep-vein thrombosis associated with use of a pneumatic tourniquet. J Bone Joint Surg Am. 1981;63:461–465. [PubMed] [Google Scholar]
- 11.Falck-Ytter Y, Francis CW, Johanson NA, Curley C, Dahl OE, Schulman S, Ortel TL, Pauker SG, Colwell CW., Jr Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e278S–e325S. doi: 10.1378/chest.11-2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fanelli GC. Posterior cruciate ligament rehabilitation: how slow should we go? Arthroscopy. 2008;24:234–235. doi: 10.1016/j.arthro.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 13.Fanelli GC, Stannard JP, Stuart MJ, MacDonald PB, Marx RG, Whelan DB, Boyd JL, Levy BA. Management of complex knee ligament injuries. J Bone Joint Surg Am. 2010;92:2235–2246. [PubMed] [Google Scholar]
- 14.Giuseffi SA, Bishop AT, Shin AY, Dahm DL, Stuart MJ, Levy BA. Surgical treatment of peroneal nerve palsy after knee dislocation. Knee Surg Sports Traumatol Arthrosc. 2010;18:1583–1586. doi: 10.1007/s00167-010-1261-7. [DOI] [PubMed] [Google Scholar]
- 15.Harner CD, Waltrip RL, Bennett CH, Francis KA, Cole B, Irrgang JJ. Surgical management of knee dislocations. J Bone Joint Surg Am. 2004;86:262–273. doi: 10.2106/00004623-200402000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Hetsroni I, Lyman S, Do H, Mann G, Marx RG. Symptomatic pulmonary embolism after outpatient arthroscopic procedures of the knee: the incidence and risk factors in 418,323 arthroscopies. J Bone Joint Surg Br. 2011;93:47–51. doi: 10.1302/0301-620X.93B1.25498. [DOI] [PubMed] [Google Scholar]
- 17.Hoppener MR, Ettema HB, Henny CP, Verheyen CC, Buller HB. Symptomatic deep vein thrombosis and immobilization after day-care arthroscopy of the knee. J Thromb Haemost. 2005;3:185–187. doi: 10.1111/j.1538-7836.2004.01091.x. [DOI] [PubMed] [Google Scholar]
- 18.Janssen RP, Sala HA. Fatal pulmonary embolism after anterior cruciate ligament reconstruction. Am J Sports Med. 2007;35:1000–1002. doi: 10.1177/0363546506298581. [DOI] [PubMed] [Google Scholar]
- 19.Jones RE, Smith EC, Bone GE. Vascular and orthopedic complications of knee dislocation. Surg Gynecol Obstet. 1979;149:554–558. [PubMed] [Google Scholar]
- 20.Kapoor A, Chew P, Silliman RA, Hylek EM, Katz JN, Cabral H, Berlowitz D. Venous thromboembolism after joint replacement in older male veterans with comorbidity. J Am Geriatr Soc. 2013;61:590–601. doi: 10.1111/jgs.12161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kieser C. A review of the complications of arthroscopic knee surgery. Arthroscopy. 1992;8:79–83. doi: 10.1016/0749-8063(92)90139-3. [DOI] [PubMed] [Google Scholar]
- 22.Lapidus LJ, Ponzer S, Pettersson H, de Bri E. Symptomatic venous thromboembolism and mortality in orthopaedic surgery–an observational study of 45 968 consecutive procedures. BMC Musculoskelet Disord. 2013;14:177. doi: 10.1186/1471-2474-14-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levy BA, Dajani KA, Whelan DB, Stannard JP, Fanelli GC, Stuart MJ, Boyd JL, MacDonald PA, Marx RG. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25:430–438. doi: 10.1016/j.arthro.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 24.Levy BA, Fanelli GC, Whelan DB, Stannard JP, MacDonald PA, Boyd JL, Marx RG, Stuart MJ. Controversies in the treatment of knee dislocations and multiligament reconstruction. J Am Acad Orthop Surg. 2009;17:197–206. doi: 10.5435/00124635-200904000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Levy BA, Krych AJ, Shah JP, Morgan JA, Stuart MJ. Staged protocol for initial management of the dislocated knee. Knee Surg Sports Traumatol Arthrosc. 2010;18:1630–1637. doi: 10.1007/s00167-010-1209-y. [DOI] [PubMed] [Google Scholar]
- 26.Levy BA, Stuart MJ. Treatment of PCL, ACL, and lateral-side knee injuries: acute and chronic. J Knee Surg. 2012;25:295–305. doi: 10.1055/s-0032-1324813. [DOI] [PubMed] [Google Scholar]
- 27.Levy BA, Zlowodzki MP, Graves M, Cole PA. Screening for extermity arterial injury with the arterial pressure index. Am J Emerg Med. 2005;23:689–695. doi: 10.1016/j.ajem.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 28.Marlovits S, Striessnig G, Schuster R, Stocker R, Luxl M, Trattnig S, Vecsei V. Extended-duration thromboprophylaxis with enoxaparin after arthroscopic surgery of the anterior cruciate ligament: a prospective, randomized, placebo-controlled study. Arthroscopy. 2007;23:696–702. doi: 10.1016/j.arthro.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 29.Mauck KF, Froehling DA, Daniels PR, Dahm DL, Ashrani AA, Crusan DJ, Petterson TM, Bailey KR, Heit JA. Incidence of venous thromboembolism after elective knee arthroscopic surgery: a historical cohort study. J Thromb Haemost. 2013;11:1279–1286. doi: 10.1111/jth.12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meyers MH, Moore TM, Harvey JP., Jr Traumatic dislocation of the knee joint. J Bone Joint Surg Am. 1975;57:430–433. [PubMed] [Google Scholar]
- 31.Michot M, Conen D, Holtz D, Erni D, Zumstein MD, Ruflin GB, Renner N. Prevention of deep-vein thrombosis in ambulatory arthroscopic knee surgery: a randomized trial of prophylaxis with low-molecular weight heparin. Arthroscopy. 2002;18:257–263. doi: 10.1053/jars.2002.30013. [DOI] [PubMed] [Google Scholar]
- 32.Montebugnoli M, Bugamelli S, Calo P, Zangheri E, Ferrari P. Prophylaxis of venous thromboembolism in minor orthopedic surgery with parnaparin. Clin Appl Thromb Hemost. 2007;13:249–258. doi: 10.1177/1076029607302667. [DOI] [PubMed] [Google Scholar]
- 33.Mook WR, Ligh CA, Moorman CT, 3rd, Leversedge FJ. Nerve injury complicating multiligament knee injury: current concepts and treatment algorithm. J Am Acad Orthop Surg. 2013;21:343–354. doi: 10.5435/JAAOS-21-06-343. [DOI] [PubMed] [Google Scholar]
- 34.Navarro-Sanz A, Fernandez-Ortega JF. Fatal pulmonary embolism after knee arthroscopy. Am J Sports Med. 2004;32:525–528. doi: 10.1177/0363546503258876. [DOI] [PubMed] [Google Scholar]
- 35.O’Reilly RF, Burgess IA, Zicat B. The prevalence of venous thromboembolism after hip and knee replacement surgery. Med J Aust. 2005;182:154–159. doi: 10.5694/j.1326-5377.2005.tb06643.x. [DOI] [PubMed] [Google Scholar]
- 36.Peskun CJ, Levy BA, Fanelli GC, Stannard JP, Stuart MJ, MacDonald PB, Marx RG, Boyd JL, Whelan DB. Diagnosis and management of knee dislocations. Phys Sportsmed. 2010;38:101–111. doi: 10.3810/psm.2010.12.1832. [DOI] [PubMed] [Google Scholar]
- 37.Plancher KD, Siliski J. Long-term functional results and complications in patients with knee dislocations. J Knee Surg. 2008;21:261–268. doi: 10.1055/s-0030-1247829. [DOI] [PubMed] [Google Scholar]
- 38.Price AJ. Hemostatic changes and postoperative deep-vein thrombosis associated with use of a pneumatic tourniquet. J Bone Joint Surg Am. 1982;64:1260. [PubMed] [Google Scholar]
- 39.Rihn JA, Groff YJ, Harner CD, Cha PS. The acutely dislocated knee: evaluation and management. J Am Acad Orthop Surg. 2004;12:334–346. doi: 10.5435/00124635-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 40.Rozencwaig R, Shilt JS, Ochsner JL., Jr Fatal pulmonary embolus after knee arthroscopy. Arthroscopy. 1996;12:240–241. doi: 10.1016/S0749-8063(96)90020-1. [DOI] [PubMed] [Google Scholar]
- 41.Salvo JP, Troxell CR, Duggan DP. Incidence of venous thromboembolic disease following hip arthroscopy. Orthopedics. 2010;33:664. doi: 10.3928/01477447-20100722-10. [DOI] [PubMed] [Google Scholar]
- 42.Schenk R. Classification of knee dislocations. Oper Tech Sports Med. 2003;11:193–198. doi: 10.1053/otsm.2003.35918. [DOI] [Google Scholar]
- 43.Sems SA, Levy BA, Dajani K, Herrera DA, Templeman DC. Incidence of deep venous thrombosis after temporary joint spanning external fixation for complex lower extremity injuries. J Trauma. 2009;66:1164–1166. doi: 10.1097/TA.0b013e318183801e. [DOI] [PubMed] [Google Scholar]
- 44.Sherman OH, Fox JM, Snyder SJ, Del Pizzo W, Friedman MJ, Ferkel RD, Lawley MJ. Arthroscopy–’no-problem surgery’. An analysis of complications in two thousand six hundred and forty cases. J Bone Joint Surg Am. 1986;68:256–265. [PubMed] [Google Scholar]
- 45.Small NC. Complications in arthroscopic surgery performed by experienced arthroscopists. Arthroscopy. 1988;4:215–221. doi: 10.1016/S0749-8063(88)80030-6. [DOI] [PubMed] [Google Scholar]
- 46.Smith TO, Hing CB. Is a tourniquet beneficial in total knee replacement surgery? A meta-analysis and systematic review. Knee. 2010;17:141–147. doi: 10.1016/j.knee.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 47.Stringer MD, Steadman CA, Hedges AR, Thomas EM, Morley TR, Kakkar VV. Deep vein thrombosis after elective knee surgery. An incidence study in 312 patients. J Bone Joint Surg Br. 1989;71:492–497. doi: 10.1302/0301-620X.71B3.2785998. [DOI] [PubMed] [Google Scholar]
- 48.Struijk-Mulder MC, Ettema HB, Verheyen CC, Buller HR. Deep vein thrombosis after arthroscopic anterior cruciate ligament reconstruction: a prospective cohort study of 100 patients. Arthroscopy. 2013;29:1211–1216. doi: 10.1016/j.arthro.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 49.Tay AK, MacDonald PB. Complications associated with treatment of multiple ligament injured (dislocated) knee. Sports Med Arthrosc. 2011;19:153–161. doi: 10.1097/JSA.0b013e31820e6e43. [DOI] [PubMed] [Google Scholar]
- 50.Wascher DC, Becker JR, Dexter JG, Blevins FT. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Results using fresh-frozen nonirradiated allografts. Am J Sports Med. 1999;27:189–196. doi: 10.1177/03635465990270021301. [DOI] [PubMed] [Google Scholar]
- 51.Wascher DC, Dvirnak PC, DeCoster TA. Knee dislocation: initial assessment and implication for treatment. J Orthop Trauma. 1997;11:525–529. doi: 10.1097/00005131-199710000-00011. [DOI] [PubMed] [Google Scholar]
- 52.Welling RE, Kakkasseril J, Cranley JJ. Complete dislocations of the knee with popliteal vascular injury. J Trauma. 1981;21:450–453. [PubMed] [Google Scholar]
- 53.Williams JS, Jr, Hulstyn MJ, Fadale PD, Lindy PB, Ehrlich MG, Cronan J, Dorfman G. Incidence of deep vein thrombosis after arthroscopic knee surgery: a prospective study. Arthroscopy. 1995;11:701–705. doi: 10.1016/0749-8063(95)90113-2. [DOI] [PubMed] [Google Scholar]
- 54.Wirth T, Schneider B, Misselwitz F, Lomb M, Tuylu H, Egbring R, Griss P. Prevention of venous thromboembolism after knee arthroscopy with low-molecular weight heparin (reviparin): results of a randomized controlled trial. Arthroscopy. 2001;17:393–399. doi: 10.1053/jars.2001.21247. [DOI] [PubMed] [Google Scholar]
- 55.Ye S, Dongyang C, Zhihong X, Dongquan S, Jin D, Jianghui Q, Jizhen Q, Pu Y, Huacheng H, Wei S, Qing J. The incidence of deep venous thrombosis after arthroscopically assisted anterior cruciate ligament reconstruction. Arthroscopy. 2013;29:742–747. doi: 10.1016/j.arthro.2013.01.017. [DOI] [PubMed] [Google Scholar]