Abstract
Background
When associated with a knee dislocation, management of the medial ligamentous injury is challenging, with little literature available to guide treatment.
Questions/purposes
We (1) compared MRI findings of medial ligament injuries between Schenck KDIIIM and KDIV injuries, (2) compared clinical outcomes and health-related quality of life as determined by Lysholm and Veterans Rand 36-Item Health Survey (VR-36) scores, respectively, of reconstructed KDIIIM and KDIV injured knees, and (3) determined reoperation rates of reconstructed KDIIIM and KDIV injured knees.
Methods
Over a 12-year period, we treated 65 patients with knee dislocations involving bicruciate ligament injury and concomitant medial ligament injuries, without or with posterolateral corner injuries (Schenck KDIIIM and KDIV, respectively); 57% were available for followup at a mean of 6.2 years (range, 1.1–11.6 years). These patients were contacted, and prospectively measured clinical outcomes scores (Lysholm and VR-36) were obtained and compared between subsets of patients. Preoperative MRIs (available for review on 49% of the patients) were rereviewed to characterize the medial ligament injuries.
Results
KDIIIM injuries more frequently had complete deep medial collateral ligament tears and posterior oblique ligament tears compared to KDIV injuries. KDIIIM knees had better Lysholm scores (88 versus 67, p = 0.027) and VR-36 scores (88 versus 70, p = 0.022) than KDIV knees. Female sex (Lysholm: 55 versus 85, p = 0.005; VR-36: 59 versus 85, p = 0.003) and an ultra-low-velocity mechanism (injury that occurs during activity of daily living in obese patients) (Lysholm: 55 versus 80–89, p = 0.002–0.013; VR-36: 60 versus 79–88, p = 0.001–0.017) were associated with worse outcomes. The overall reoperation rate was 28%, and the most common indication for reoperation was stiffness.
Conclusions
Medial ligament injury is common in knee dislocations. Females who sustain these injuries and patients who have an ultra-low-velocity mechanism should be counseled at the time of injury about the likelihood of inferior outcomes. As ROM deficits are the most commonly encountered complication, postoperative rehabilitation should focus on early ROM exercises as stability and wound healing allow. Future prospective studies are needed to definitively determine whether operative or nonoperative management is appropriate for particular medial ligamentous injury patterns.
Introduction
The medial collateral ligament (MCL) is frequently damaged in traumatic knee injuries [15]. While ligament injuries involving the medial side of the knee can frequently be successfully managed nonoperatively, the management of the medial ligamentous injury when associated with a knee dislocation is more challenging and a subject of controversy [27].
In contrast to the abundant biomechanical and clinical research into injuries to the posterolateral corner and associated lateral ligamentous structure injuries in knee dislocations [4, 5, 10, 17, 18, 29], the available literature and dedicated investigation to the medial-sided ligamentous injury in knee dislocations is sparse, particularly with regard to clinical outcomes [1–3, 12, 14, 15, 19, 24, 26–28]. Furthermore, the majority of available studies historically view the medial-sided injury as an MCL injury alone or in combination with an isolated ACL tear, failing to account for the multiple other structures that comprise the posteromedial corner and provide ligamentous support to the medial side of the knee that are frequently injured due to the rotational forces of a knee dislocation [6, 7, 11, 13]. Because of these issues, evidence-based treatment recommendations for the management of medial ligament injuries in knee dislocations are notably lacking.
Two of the deficits in the current literature that exist in regard to medial-sided injuries in knee dislocations are the characterization of the injury patterns to all medial supportive structures and clinical outcomes after reconstruction of the knee. As Hughston and Eilers [9] and later others alluded, in addition to the superficial and deep layers of the MCL, the posteromedial corner of the knee is described to consist of the semimembranosus and the posterior oblique ligament [16, 20–22]. Additional supportive structures that may have a functional role in medial knee stability, particularly in the setting of a bicruciate injury in knee dislocation, include the posterior horn of the medial meniscus, the meniscotibial ligaments, and the oblique popliteal ligament [2, 8, 16, 22]. Despite identification of these structures, it is unknown which are typically injured in a knee dislocation. Kovachevich et al. [15] published a systematic review of the operative management of MCL injuries in multiligament-injured knees. The authors noted “a paucity of objective data on the outcomes regarding surgical management of MCL tears in the combined ligament injured knee,” highlighting a need for further clinical investigation into outcomes after reconstruction.
We therefore further characterized the medial-sided injury in knee dislocations, specifically bicruciate ligament injuries including medial-sided involvement, without or with posterolateral corner injuries (Schenck KDIIIM and KDIV, respectively [23]), specifically by (1) comparing MRI findings of medial ligament injuries between KDIIIM and KDIV injured knees, (2) comparing Lysholm and Veteran’s Rand 36-Item Health Survey (VR-36) scores in patients whose KDIIIM and KDIV injured knees were reconstructed, and (3) evaluating complication and reoperation rates between patients whose KDIIIM and KDIV injured knees were reconstructed.
Patients and Methods
After institutional review board approval was obtained, we retrospectively reviewed all patients at our institution with multiligament knee injuries between September 2000 and September 2012 who underwent operative repair or reconstruction by the senior author (MDM) to identify a cohort of patients with knee dislocations and medial ligament injury. Inclusion criteria were patients with a bicruciate ligament injury and medial ligament injury identified by either MRI or stress radiography (KDIIIM or KDIV) and operative repair or reconstruction of at least one of the cruciate ligaments. Ligamentous injury patterns were defined by the senior author at the time of injury using MRI and stress radiography and confirmed with examination under anesthesia and arthroscopy at the time of reconstruction. All retrospective ligamentous injury pattern classifications were confirmed during the study using available MRI, MRI reports, stress radiography, and operative reports. All ligamentous injury patterns designated at the time of injury and/or reconstruction were confirmed to be correct. Exclusion criteria were significant additional trauma that would preclude accurate results (including tibial plateau fractures, distal femur fractures, and long-bone fractures), head trauma, or patient records not available for review.
Over the 12-year study period, 215 operatively managed medial ligament injuries were identified. In the entire cohort with medial ligament injuries, there were 165 male (76%) and 50 female patients (24%), with a mean ± SD age of 32 ± 13 years (range, 14–74 years) and a mean BMI of 34 ± 11 kg/m2 (range, 19–74 kg/m2). From this cohort, 65 knees had bicruciate injuries with associated medial-sided injury, including 32 KDIIIM knees and 33 KDIV knees.
A musculoskeletal radiologist (CMG) independently reviewed postinjury, preoperative MR images of the 32 patients (49%) with MR images available for review (14 KDIIIM patients and 18 KDIV patients). In addition to confirming the ACL and PCL injuries, the following structures were specifically assessed: superficial MCL, deep MCL, posterior oblique ligament, oblique popliteal ligament, semimembranosus, semitendinosus, medial meniscus body and posterior horn, meniscotibial ligaments, and meniscocapsular junction.
Of the 65 patients included in the retrospective portion of the study, three subsequently died from unrelated causes and one patient had a THA. Of the 61 remaining patients, 35 were able to be contacted for prospective followup data for a 57% followup rate. Of the 26 patients who were not available for clinical followup, 22 did not have appropriate contact information, two were incarcerated and unable to participate, and two were unwilling to participate. Followup was at a mean of 6.2 years (range, 1.1–11.6 years). There was no differential loss to followup between the KDIIIM and KDIV groups, with complete followup available on 47% (15 of 32) of the KDIIIM patients and 60% (20 of 33) of the KDIV patients (p = 0.267).
Of the 65 patients, 50 were male (77%) and 15 female (23.%); the mean age was 35 ± 15 years (range, 15–74 years) and the mean BMI was 37 ± 10 kg/m2 (range, 22–67 kg/m2). Peroneal nerve injury was present in six of 65 patients (9%), including none in the 32 KDIIIM injured knees and six (18%) in the 33 KDIV injured knees. Vascular injury was present in three of 65 patients (4.6%), including one (3.1%) in the 32 KDIIIM injured knees and two (6.1%) in the KDIV injured knees.
Operative intervention was pursued acutely or semiacutely, typically within the first 3 weeks after injury. All injured structures requiring reconstruction or repair were addressed in a single operation. Preoperative management typically consisted of a knee immobilizer or IROM® brace (DJO, LLC, Vista, CA, USA), with a focus on regaining full extension before surgery. All patients underwent operative reconstruction of at least one cruciate ligament (the ACL). Management of PCL tears was not randomized, and patients with significant laxity (defined as > 10-mm posterior translation) demonstrated on stress radiography were reconstructed. This resulted in PCL reconstructions in 63% (20 of 32) of KDIIIM knees and 70% (23 of 33) of KDIV knees, which was not different between groups (p = 0.540). Posterolateral corner injuries with varus laxity on stress radiography were reconstructed in KDIV knees. Management of the medial-sided injury was not randomized and consisted of nonoperative management in 16 of 65 knees (25%) (KDIIIM: 6%, KDIV: 42%), repair alone in 12 (18%) (KDIIIM: 25%; KDIV: 12%), and reconstruction in 37 (57%) (KDIIIM: 69%; KDIV: 46%).
The decision to observe, repair, or reconstruct the medial ligamentous injury was based on MRI findings, stress radiography, and intraoperative findings (Fig. 1). Patients were considered for nonoperative management (bracing) if the MCL injury was from the femoral side, if stress radiographs demonstrated less than 5 mm of side-to-side difference, and if no varus opening was noted in full extension. Patients with significant instability, tibial-sided injuries, an MCL trapped in the joint, or Stener lesions (when the superficial fibers of the MCL of the knee are torn without tearing of the deep fibers) typically underwent operative intervention for their medial injuries. When the MCL avulsed as a thick sleeve from its attachment, it was repaired primarily to a prepared bone bed with suture anchors or a screw and spiked washer (Fig. 2A–B). Midsubstance tears of the MCL, chronic tears, and tenuous repairs were typically supplemented with a reconstruction. Our preferred medial reconstruction was the modified Bosworth technique [12] in which the native semitendinosus was harvested but left attached to its distal insertion. The graft was looped around a screw, a spiked washer was placed at the medial epicondyle of the femur, and the graft was then secured about 6 cm distal to the joint near the posterior cortex of the tibia with another screw and washer (Figs. 2C–D, 3). When the native semitendinosus was unavailable or had been harvested for a concurrent or previous ACL reconstruction, an allograft was used to recreate the MCL Attempting to establish isometry of the graft is also important in MCL reconstruction. Fluoroscopy was used to confirm placement of a femoral guidewire in line with the posterior aspect of the femoral shaft on lateral imaging.
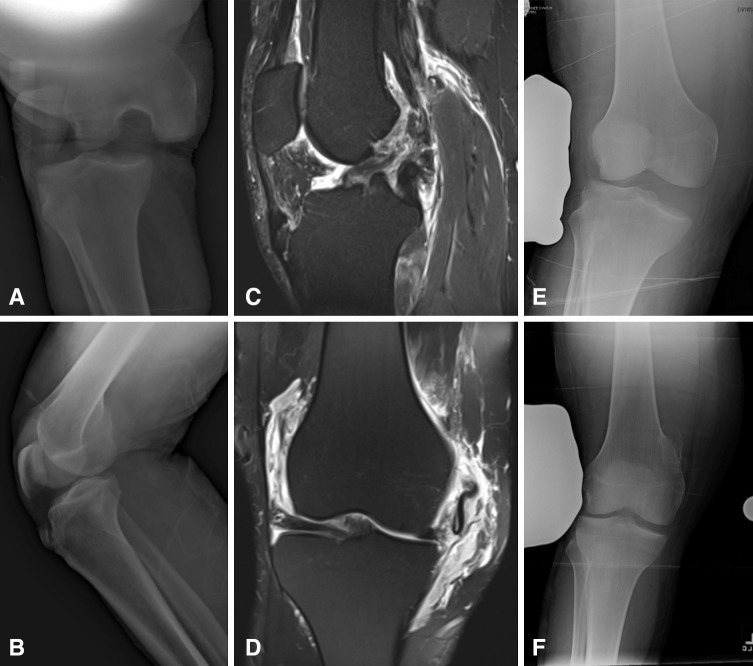
Fig. 1A–F.
Images illustrate the case of a 34-year-old dairy farmer who was kicked by a cow and sustained a KDIV knee dislocation. (A) AP and (B) lateral radiographs demonstrate the knee dislocation before reduction. (C) A sagittal short tau inversion recovery MR image and (D) a coronal fast spin echo T2-weighted MR image with fat saturation demonstrate complete ACL, PCL, lateral collateral ligament/posterolateral corner, and MCL injuries. He also had a significant posteromedial corner injury, which included medial meniscus and posterior oblique ligament tears. Valgus stress radiographs of the (E) injured and (F) uninjured knee demonstrate a greater than 10-mm side-to-side difference. (F) The uninjured knee valgus stress radiograph has been flipped horizontally to facilitate comparison with (E) the injured knee.
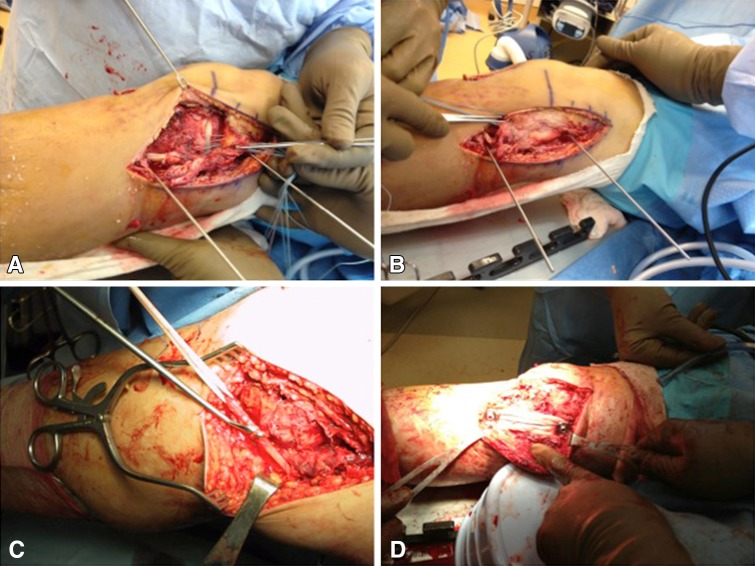
Fig. 2A–D.
Intraoperative photographs demonstrate (A, B) the typical medial ligament repair using suture anchors and (C, D) reconstruction using a modified Bosworth technique.
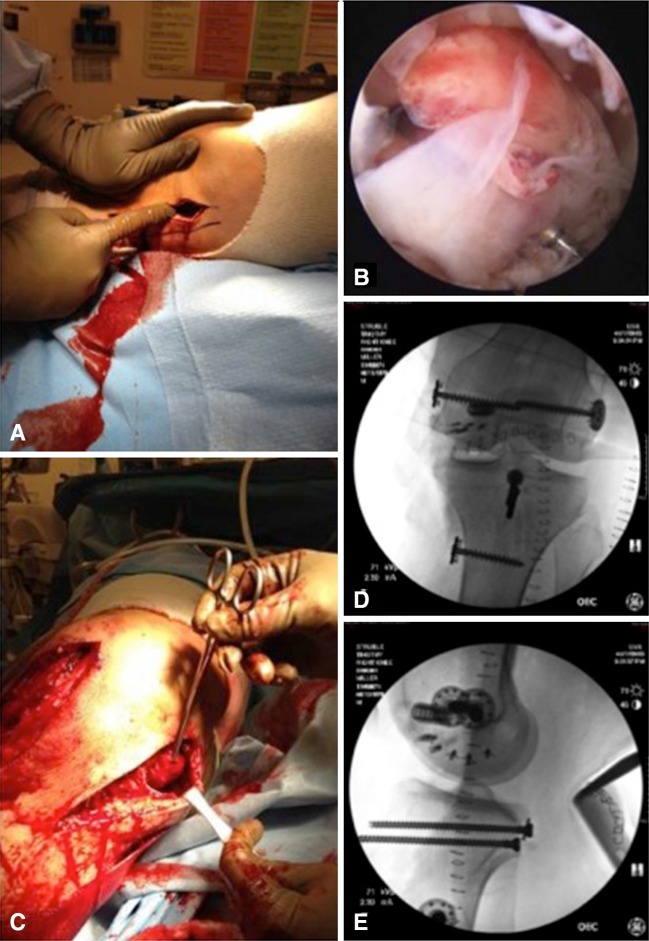
Fig. 3A–E.
Operative management of the KDIV injury in the patient depicted in Figure 1 is illustrated. (A) A medial egress incision is created. (B) Diagnostic arthroscopy confirmed a bicruciate injury. (C) Extraarticular reconstruction of the medial ligamentous injury is performed using a modified Bosworth technique. Postoperative (D) AP and (E) lateral imaging demonstrate typical hardware placement for the medial reconstruction, which is used intraoperatively to confirm an isometric location.
Postoperative management was standardized and the same for both the KDIIIM and KDIV injury patterns. Initial weightbearing was toe-touch only. Therapy for ROM in a hinged knee brace was started almost immediately, as stiffness is an unfortunately frequent complication of complex ligament reconstruction.
Chart review was utilized to ascertain epidemiologic information, injury characteristics, operative details, postoperative complications, and need for reoperation. Patients were then contacted to obtain clinical followup data, including Lysholm and VR-36 scores. No objective measurements of knee stability were made at final followup.
Patients were divided into several cohorts for comparison according to (1) ligamentous injury pattern, (2) sex, and (3) injury mechanism: high velocity (falls from height, motor vehicle collisions), low velocity (sports, falls from short height), and ultra-low velocity (falls during activities of daily living in obese patients).
We performed statistical analysis of all continuous variables and comparison of means using Student’s t-tests. Categorical values, including proportions of patients with followup, were calculated using chi-square tests. Multivariate analysis using ANOVA with least significant difference post hoc test was also performed to determine which variables were significant contributors to inferior outcomes scores. All obtained data were determined to be normally distributed by examining skewness and kurtosis values. For all statistical tests, p values of less than 0.05 were considered significant. Statistical analysis was performed using SPSS® Version 21 software (SPSS Inc, Chicago, IL, USA).
Results
All KDIIIM knees were noted to have involvement of the posterior oblique ligament, compared to 72% of KDIV knees (p = 0.032). The presence of deep MCL tears was similar between KDIIIM and KDIV knees, although complete deep MCL tears were more common in KDIIIM knees (43% versus 17%, p = 0.044) (Table 1). All KDIIIM and KDIV knees were noted to have complete ACL and PCL tears and at least high-grade partial MCL tears. No difference was noted between KDIIIM and KDIV knees regarding tears of the oblique popliteal ligament, semimembranosus, or semitendinosus tendons. Medial meniscal injury was common in both KDIIIM and KDIV knees, although no difference between injury patterns was noted with regard to meniscal tears, meniscocapsular separation, or injury to meniscotibial ligaments (Table 2).
Table 1.
MRI findings of medial ligament injury in knee dislocations
| Injury type | Superficial MCL (%) | Deep MCL (%) | Posterior oblique ligament (%) | Oblique popliteal ligament (%) | Semimembranosus (%) | Semitendinosus (%) |
|---|---|---|---|---|---|---|
| KDIIIM (n = 14) | ||||||
| None | 0 | 50 | 0.0 | 64 | 71 | 100 |
| Partial | 14 | 7 | 50 | 14 | 29 | 0 |
| Complete | 86 | 43 | 50 | 21 | 0 | 0 |
| KDIV (n = 18) | ||||||
| None | 0 | 61 | 28 | 67 | 56 | 100 |
| Partial | 50 | 22 | 44 | 22 | 39 | 0 |
| Complete | 50 | 17 | 28 | 11 | 6 | 0 |
MCL = medial collateral ligament.
Table 2.
MRI findings of medial meniscal injury in knee dislocations
| Injury type | Medial meniscus (%) | Medial meniscus body (%) | Medial meniscus posterior horn (%) | Meniscocapsular separation (%) | Meniscus tibial (%) |
|---|---|---|---|---|---|
| KDIIIM (n = 14) | |||||
| Tear | 43 | 36 | 43 | 21 | 29 |
| No tear | 57 | 64 | 57 | 79 | 71 |
| KDIV (n = 18) | |||||
| Tear | 44 | 33 | 39 | 22 | 28 |
| No tear | 56 | 67 | 61 | 78 | 72 |
KDIIIM knees had better Lysholm scores (88 versus 67, p = 0.027) and VR-36 scores (88 versus 70, p = 0.022) than KDIV knees (Table 3). Female patients had worse Lysholm scores (55 versus 85, p = 0.005) and VR-36 scores (59 versus 85, p = 0.003) compared to male patients (Table 4). There was no difference in injury pattern between male and female patients. An ultra-low-velocity mechanism was associated with worse Lysholm scores (55 versus 80–89, p = 0.002–0.013) and VR-36 scores (60 versus 79–88, p = 0.001–0.017) compared to high-velocity and low-velocity mechanisms (Table 5). There were no differences in outcomes between the high- and low-velocity cohorts.
Table 3.
Comparison of clinical outcomes based on injury pattern
| Injury type | Lysholm score (points) | VR-36 score (points) | Followup (years) |
|---|---|---|---|
| KDIIIM (n = 15) | |||
| Mean | 88 | 88 | 6.7 (range, 1.1–11.6) |
| SD | 4.6 | 1.9 | |
| KDIV (n = 20) | |||
| Mean | 67 | 70 | 5.6 (range, 1.2–11.6) |
| SD | 13.2 | 9.6 | |
| p value | 0.027 | 0.022 | |
VR-36 = Veterans Rand 36-Item Health Survey.
Table 4.
Comparison of clinical outcomes based on sex
| Sex | Lysholm score (points) | VR-36 score (points) | Followup (years) |
|---|---|---|---|
| Male (n = 26) | |||
| Mean | 85 | 85 | 6.1 (range, 1.1–11.6) |
| SD | 8.6 | 4.7 | |
| Female (n = 9) | |||
| Mean | 55 | 59 | 6.0 (range, 1.4–11.6) |
| SD | 11.1 | 9.3 | |
| p value | 0.005 | 0.003 | |
VR-36 = Veterans Rand 36-Item Health Survey.
Table 5.
Comparison of clinical outcomes based on injury mechanism
| Velocity of injury mechanism | Lysholm score (points) | VR-36 score (points) | Followup (years) |
|---|---|---|---|
| High (n = 10) | |||
| Mean | 80 | 79 | 6.1 (range, 1.4–7.9) |
| SD | 10.1 | 8.6 | |
| Low (n = 14) | |||
| Mean | 89 | 88 | 5.8 (range, 1.1–11.6) |
| SD | 5.1 | 2.0 | |
| Ultra-low (n = 11) | |||
| Mean | 55 | 60 | 6.7 (range, 1.2–11.6) |
| SD | 11.8 | 8.3 | |
| p value | |||
| High versus low | 0.626 | 0.465 | |
| High versus ultra-low | 0.013 | 0.017 | |
| Low versus ultra-low | 0.002 | 0.001 | |
VR-36 = Veterans Rand 36-Item Health Survey.
Multivariate analysis demonstrated that female sex and an ultra-low-velocity mechanism were associated with lower Lysholm scores, with p values ranging from 0.005 to 0.045. Female sex, ultra-low-velocity mechanism, and a KDIV injury pattern were found to be associated with lower VR-36 scores, with p values ranging from 0.0001 to 0.048.
With the numbers available, there were no differences in the proportion of patients who underwent reoperation between the KDIIIM and KDIV groups. The overall reoperation rate was 28% (18 of 65); 25% of KDIIIM knees (eight of 32) and 30% of KDIV knees (10 of 33) underwent reoperation. The most common reason for reoperation was stiffness requiring manipulation under anesthesia and lysis of adhesions (10 of 18). Painful hardware (three of 18), infection (three of 18), and graft failure (two of 18) were the remaining indications for reoperation.
Discussion
Knee dislocations frequently result in medial-sided ligamentous injury. While ligamentous injury involving the medial side of the knee can often be managed nonsurgically, when associated with a knee dislocation, the management of the medial ligamentous injury is more challenging and a subject of controversy. As previous authors have noted, there is a paucity of objective data on outcomes after surgical management of MCL tears in multiligament-injured knees [16]. We therefore (1) compared MRI findings of medial ligament injuries between KDIIIM and KDIV injured knees (defined as knee dislocations with bicruciate plus medial-sided injury, without or with posterolateral corner injuries, respectively), (2) compared clinical outcomes of various subsets of reconstructed KDIIIM and KDIV injured knees, and (3) evaluated complication and reoperation rates between various subsets of reconstructed KDIIIM and KDIV injured knees.
Our study has a number of limitations. First, owing to the retrospective nature of the study, patients were not randomized to a treatment group nor was there a standardized process for determining which patients received what type of management for their medial ligamentous injury. Additionally, as this study spanned 12 years of patients, 49% (32 of the original 65) of our patients did not have available MRI for review, and 43% (26 of the eligible 61) were not reachable for clinical followup. As a tertiary referral center, our referral area is vast and many patients are economically disadvantaged, making return for followup challenging. There was no differential loss to followup between the KDIIIM and KDIV groups. In general, though, it is fair to surmise that retrospective series with substantial loss to followup present a best-case picture in terms of clinical scores and reoperation rates; patients who are lost to followup generally are not doing as well clinically as those who attend followup. Although this study presents a relatively large number of patients for this uncommon injury, the small number of patients in the study does decrease the power of the study and subject the analysis to Type II errors. Additionally, many of these patients were referred to our tertiary care center from outside institutions. This selection bias may have resulted in a disproportionately higher number of complicated knee dislocations in our cohort.
We found that KDIIIM knee dislocations more frequently had complete deep MCL tears and tears of the posterior oblique ligament compared to KDIV knee dislocations, with similar injury patterns to the medial meniscus and its supporting structures. A recent MRI study by Chahal et al. [2] evaluated injuries to the posteromedial corner on MRI in 27 consecutive dislocated knees. While the authors included all injury patterns in their series, they noted that injury to at least one structure in the posteromedial corner occurred in 81% of patients, regardless of injury pattern. Of those knees with posteromedial corner injury, the posterior oblique ligament was injured in 64% of patients, the semimembranosus in 64% of patients, meniscotibial ligaments in 50% of patients, and the posterior horn of the medial meniscus in 41% of patients. We report similar findings in our series, with injury to the posterior oblique ligament in 84% of patients, semimembranosus in 38%, meniscotibial ligaments in 28%, and the posterior horn of the medial meniscus in 41%. Sims and Jacobson [25] also published an MRI study of medial-sided knee injury patterns, in which the authors noted a very high rate of injury to the posterior oblique ligament, in addition to high rates of semimembranosus and meniscocapsular injury, although very few of these also had concomitant injuries to the ACL and PCL (three patients). No studies, however, have previously examined the medial-sided injury pattern specifically in bicruciate-injured knees (KDIIIM and KDIV). The authors postulate that posterior oblique ligament involvement is more common in KDIIIM injuries compared to KDIV because the majority of the rotational and translational force must dissipate only through the medial side in KDIIIM knees, as the lateral side remains intact. In KDIV injuries, these forces can dissipate through both the lateral and medial sides, with both patterns demonstrating the same pattern of cruciate ligament injury.
Our patients with medial-sided injury in the setting of a knee dislocation overall reported reasonable clinical outcomes, with a mean Lysholm score of 75 ± 12 and a mean VR-36 score of 78 ± 9. We also found that, among patients with knee dislocations with medial ligament injury, KDIIIM injury patterns had better clinical outcomes than KDIV patterns, males had better outcomes than females, and an ultra-low-velocity mechanism led to inferior results. No previous studies have compared these effects on clinical outcomes in patients with medial ligamentous injury in knee dislocations. It is challenging to establish causality in a small retrospective series such as the present study, particularly with the potential for confounders, so the true reason for these relationships is not ascertainable. This is important information, however, to discuss with patients preoperatively and risk-stratify their chances of a satisfactory outcome with ligamentous reconstruction.
Our patients had an overall reoperation rate of 28%, with stiffness (15%) being the most common indication for surgical intervention. Two patients had reoperation for medial instability, representing a failure rate of 3%. Stannard et al. [27] reported arthrofibrosis in 18% of their cohort. The authors also reported an overall infection rate of 4%, similar to our overall infection rate of 4.6%. The authors also noted a 4% failure rate of their posteromedial corner reconstructions, which correlates well with our 3% failure rate.
In conclusion, medial ligament injury is common in knee dislocations. In addition to superficial and deep MCL injuries, the posterior oblique ligament, semimembranosus, and medial meniscus are frequently damaged. Females who sustain these injuries and patients who have an ultra-low-velocity mechanism should be counseled at the time of injury about the likelihood of inferior outcomes. As ROM deficits are the most commonly encountered complication, postoperative rehabilitation should focus on early ROM exercises as stability and wound healing allow. Future prospective studies are needed to definitively determine whether operative or nonoperative management is appropriate for particular medial ligamentous injury patterns.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial association (eg, consultancies, stock ownership, equity interest, patent/licensing agreements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Campbell JD. The evolution and current treatment trends with anterior cruciate, posterior cruciate, and medial collateral ligament injuries. Am J Knee Surg. 1998;11:128–135. [PubMed] [Google Scholar]
- 2.Chahal J, Al-Taki M, Pearce D, Leibenberg A, Whelan DB. Injury patterns to the posteromedial corner of the knee in high-grade multiligament knee injuries: a MRI study. Knee Surg Sports Traumatol Arthrosc. 2010;18:1098–1104. doi: 10.1007/s00167-009-1011-x. [DOI] [PubMed] [Google Scholar]
- 3.Fanelli GC, Edson CJ. Surgical treatment of combined PCL-ACL medial and lateral side injuries (global laxity): surgical technique and 2- to 18-year results. J Knee Surg. 2012;25:307–316. doi: 10.1055/s-0032-1326997. [DOI] [PubMed] [Google Scholar]
- 4.Gelber PE, Erquicia JI, Sosa G, Ferrer G, Abat F, Rodriguez-Baeza A, Segura-Cros C, Monllau JC. Femoral tunnel drilling angles for the posterolateral corner in multiligamentary knee reconstructions: computed tomography evaluation in a cadaveric model. Arthroscopy. 2013;29:257–265. doi: 10.1016/j.arthro.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 5.Gwathmey FW, Jr, Tompkins MA, Gaskin CM, Miller MD. Can stress radiography of the knee help characterize posterolateral corner injury? Clin Orthop Relat Res. 2012;470:768–773. doi: 10.1007/s11999-011-2008-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Halinen J, Lindahl J, Hirvensalo E, Santavirta S. Operative and nonoperative treatments of medial collateral ligament rupture with early anterior cruciate ligament reconstruction: a prospective randomized study. Am J Sports Med. 2006;34:1134–1140. doi: 10.1177/0363546505284889. [DOI] [PubMed] [Google Scholar]
- 7.Hastings DE. The non-operative management of collateral ligament injuries of the knee joint. Clin Orthop Relat Res. 1980;147:22–28. [PubMed] [Google Scholar]
- 8.House CV, Connell DA, Saifuddin A. Posteromedial corner injuries of the knee. Clin Radiol. 2007;62:539–546. doi: 10.1016/j.crad.2006.11.024. [DOI] [PubMed] [Google Scholar]
- 9.Hughston JC, Eilers AF. The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. J Bone Joint Surg Am. 1973;55:923–940. [PubMed] [Google Scholar]
- 10.Ibrahim SA, Ghafar S, Salah M, Abo Alnas M, Al Misfer A, Farouk H, Al Haran H, Khirait S. Surgical management of traumatic knee dislocation with posterolateral corner injury. Arthroscopy. 2013;29:733–741. doi: 10.1016/j.arthro.2012.11.021. [DOI] [PubMed] [Google Scholar]
- 11.Indelicato PA. Non-operative treatment of complete tears of the medial collateral ligament of the knee. J Bone Joint Surg Am. 1983;65:323–329. [PubMed] [Google Scholar]
- 12.Jacobson KE, Chi FS. Evaluation and treatment of medial collateral ligament and medial-sided injuries of the knee. Sports Med Arthrosc. 2006;14:58–66. doi: 10.1097/01.jsa.0000212305.47323.58. [DOI] [PubMed] [Google Scholar]
- 13.Kannus P. Long-term results of conservatively treated medial collateral ligament injuries of the knee joint. Clin Orthop Relat Res. 1988;226:103–112. [PubMed] [Google Scholar]
- 14.Klimkiewicz JJ, Petrie RS, Harner CD. Surgical treatment of combined injury to anterior cruciate ligament, posterior cruciate ligament, and medial structures. Clin Sports Med. 2000;19:479–92, vii. [DOI] [PubMed]
- 15.Kovachevich R, Shah JP, Arens AM, Stuart MJ, Dahm DL, Levy BA. Operative management of the medial collateral ligament in the multi-ligament injured knee: an evidence-based systematic review. Knee Surg Sports Traumatol Arthrosc. 2009;17:823–829. doi: 10.1007/s00167-009-0810-4. [DOI] [PubMed] [Google Scholar]
- 16.LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89:2000–2010. doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 17.Levy BA, Dajani KA, Morgan JA, Shah JP, Dahm DL, Stuart MJ. Repair versus reconstruction of the fibular collateral ligament and posterolateral corner in the multiligament-injured knee. Am J Sports Med. 2010;38:804–809. doi: 10.1177/0363546509352459. [DOI] [PubMed] [Google Scholar]
- 18.Levy BA, Fanelli GC, Whelan DB, Stannard JP, MacDonald PA, Boyd JL, Marx RG, Stuart MJ, Knee Dislocation Study Group Controversies in the treatment of knee dislocations and multiligament reconstruction. J Am Acad Orthop Surg. 2009;17:197–206. doi: 10.5435/00124635-200904000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Marx RG, Hetsroni I. Surgical technique: medial collateral ligament reconstruction using Achilles allograft for combined knee ligament injury. Clin Orthop Relat Res. 2012;470:798–805. doi: 10.1007/s11999-011-1941-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Petersen W, Loerch S, Schanz S, Raschke M, Zantop T. The role of the posterior oblique ligament in controlling posterior tibial translation in the posterior cruciate ligament-deficient knee. Am J Sports Med. 2008;36:495–501. doi: 10.1177/0363546507310077. [DOI] [PubMed] [Google Scholar]
- 21.Robinson JR, Bull AM, Thomas RR, Amis AA. The role of the medial collateral ligament and posteromedial capsule in controlling knee laxity. Am J Sports Med. 2006;34:1815–1823. doi: 10.1177/0363546506289433. [DOI] [PubMed] [Google Scholar]
- 22.Robinson JR, Sanchez-Ballester J, Bull AM, Thomas Rde W, Amis AA. The posteromedial corner revisited. an anatomical description of the passive restraining structures of the medial aspect of the human knee. J Bone Joint Surg Br. 2004;86:674–681. doi: 10.1302/0301-620X.86B5.14853. [DOI] [PubMed] [Google Scholar]
- 23.Schenck RC., Jr The dislocated knee. Instr Course Lect. 1994;43:127–136. [PubMed] [Google Scholar]
- 24.Shelbourne KD, Carr DR. Combined anterior and posterior cruciate and medial collateral ligament injury: nonsurgical and delayed surgical treatment. Instr Course Lect. 2003;52:413–418. [PubMed] [Google Scholar]
- 25.Sims WF, Jacobson KE. The posteromedial corner of the knee: medial-sided injury patterns revisited. Am J Sports Med. 2004;32:337–345. doi: 10.1177/0363546503261738. [DOI] [PubMed] [Google Scholar]
- 26.Stannard JP, Bauer KL. Current concepts in knee dislocations: PCL, ACL, and medial sided injuries. J Knee Surg. 2012;25:287–294. doi: 10.1055/s-0032-1326998. [DOI] [PubMed] [Google Scholar]
- 27.Stannard JP, Black BS, Azbell C, Volgas DA. Posteromedial corner injury in knee dislocations. J Knee Surg. 2012;25:429–434. doi: 10.1055/s-0032-1322605. [DOI] [PubMed] [Google Scholar]
- 28.Wijdicks CA, Griffith CJ, Johansen S, Engebretsen L, LaPrade RF. Injuries to the medial collateral ligament and associated medial structures of the knee. J Bone Joint Surg Am. 2010;92:1266–1280. doi: 10.2106/JBJS.I.01229. [DOI] [PubMed] [Google Scholar]
- 29.Yang BS, Bae WH, Ha JK, Lee DW, Jang HW, Kim JG. Posterolateral corner reconstruction using the single fibular sling method for posterolateral rotatory instability of the knee. Am J Sports Med. 2013;41:1605–1612. doi: 10.1177/0363546513488866. [DOI] [PubMed] [Google Scholar]