Abstract
Background
Knee dislocation may be associated with an injury to the common peroneal nerve with a subsequent foot drop. Previous studies have demonstrated good functional results after posterior tibial tendon transfer in patients with foot drop. No studies, to our knowledge, have focused exclusively on knee dislocation as the cause of common peroneal nerve injury leading to foot drop.
Questions/purposes
We determined the percentage of patients developing common peroneal nerve paresis after knee dislocation, the symptom improvement rate in these patients, and patient-reported outcomes (American Orthopaedic Foot and Ankle Society [AOFAS] ankle-hindfoot score), ankle dorsiflexion strength, and ROM in patients with no symptom improvement treated with posterior tibial tendon transfer.
Methods
Two hundred forty-seven patients with knee dislocation, defined as an injury to both the ACL and PCL with an additional injury to the lateral and/or medial ligaments (Schenck Classification II to IV), were registered in a single institution’s database between 1996 and 2011. The database was queried for the frequency of documented injuries to the common peroneal nerve and, among those, the frequency of spontaneous resolution after this injury. Patients demonstrating no active dorsiflexion 12 months after injury generally were offered posterior tibial tendon transfer. Postoperatively, patients were evaluated for AOFAS score, ankle dorsiflexion strength, and ROM.
Results
Forty-three patients (17%) had a common peroneal nerve paresis at admission. At 1-year followup, 15 of 43 patients (35%) had experienced symptom improvement. One patient experienced spontaneous improvement later than 1 year after injury. One patient was lost to followup. A below-knee amputation was performed in one patient due to the initial trauma. Seven patients were satisfied with their function using a brace or had medical contraindications to surgical treatment, while four patients refused the proposed operation with a tendon transfer, leaving 14 patients treated with posterior tibial tendon transfer. In the 12 patients available for evaluation, mean AOFAS score was 91 of 100. Mean (± SD) dorsiflexion strength was 118 (± 55) Nm on the operated side and 284 (± 94) Nm on the unaffected side (p < 0.001). Mean ROM was 67° (± 15°) on the operated side and 93° (± 14°) on the unaffected side (p < 0.001).
Conclusions
Based on these findings, we recommend posterior tibial tendon transfer for treatment of foot drop that persists at least 1 year after knee dislocation.
Level of Evidence
Level IV, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
Dislocation of the knee is a rare injury and accounts for 0.02% to 0.2% of orthopaedic injuries [12, 19, 20]. The cause of injury can be high- or low-energy trauma [3]. Almost 1/3 of the patients are polytraumatized [29], and the amputation rate after knee dislocation is approximately 10% [23]. Knee dislocation is often associated with additional injuries to the affected leg, such as injury to the popliteal artery (23%–32%) [6, 26], compartment syndrome, injury to the tibial nerve [13, 25, 30], and more often injury to the common peroneal nerve (14%–40%) [3, 14, 16, 21, 28].
Spontaneous healing potential after common peroneal nerve paresis is uncommon [9, 22, 31], but an incomplete nerve injury has a better prognosis [5]. Immediate surgical nerve suture, neurolysis, and nerve grafting have been reported to give poor results regarding return of motoric function [11, 31]. Some authors recommend repeated EMG and nerve conduction velocity testing to evaluate the status of the common peroneal nerve [9], and some recommend surgical intervention if no recovery of motor function is noted 3 months after the initial injury [5, 9]. Previous studies describe the results after posterior tibial tendon transfer for foot drop as fair to good [1, 7, 10, 18, 32], but the studies include patients with a wide range of reasons for foot drop. No previous studies, to our knowledge, have exclusively focused on patients with knee dislocation as the specific reason for the foot drop, and this may be important because patients with a more proximal lesion to the nerve (such as occurs with knee dislocations) may have some impairment to other muscle groups of the calf that can influence functional results when these lesions are treated surgically, and the severity of trauma associated with knee dislocations might itself influence the likelihood of motor recovery.
We therefore studied the percentage of patients developing common peroneal paresis after knee dislocation and the symptom improvement rate of these patients within 1 year after the injury. Additionally, the patient-reported outcomes using the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score, ankle dorsiflexion strength, and ROM in the subset of patients who underwent posterior tibial tendon transfer for foot drop after knee dislocations were studied.
Patients and Methods
Two hundred forty-seven patients with traumatic knee dislocations were treated at our hospital between May 1996 and January 2012 (Fig. 1). The inclusion criterion was a knee dislocation defined as an injury to both the ACL and PCL with an additional injury to the lateral and/or medial ligaments (Schenck Classification II to IV) [3]. Patients with severe intraarticular fracture of the knee (Schenck Classification V) or skeletal immaturity were not included. All 247 patients were entered into a prospective database and have been followed since the time of injury. In an early report from this database covering 85 patients [3], 51% were high-energy trauma, but unfortunately we do not have more detailed data on the larger cohort of all 247 at the time of this publication. This study was approved by the regional ethics committee (05.06.2012; reference: 2012/873), and informed consent was obtained before patient inclusion.
Fig. 1.
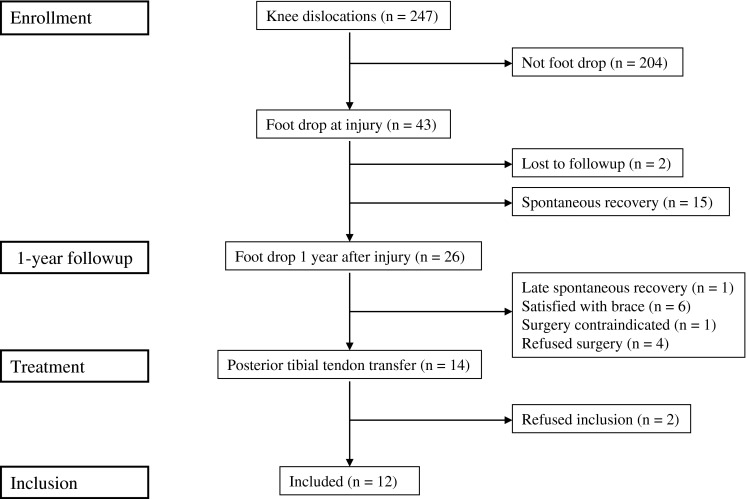
A flowchart shows the patient selection process.
At the time of admission, knee injuries, including injury to the common peroneal nerve and any additional injuries, were registered. The status of the common peroneal nerve was obtained from the patient’s chart in all 247 patients. Of the 247 patients, 43 suffered from a paresis of the common peroneal nerve at admission. The mechanism of injury was high-energy trauma in 22 of these patients and sports or low-energy trauma in 21 patients. These patients have not routinely been examined with EMG or nerve conduction velocity as our policy has not been reconstructive nerve surgery but later tendon transfers after awaiting spontaneous recovery at least 1 year. The nerve function was then again examined clinically at the followup 1 year after injury in 41 of these patients. One patient was not examined because he moved abroad and one patient had undergone amputation as a result of his original trauma.
A total of 26 patients had residual dorsiflexion weakness at 1 year, 13 from high-energy trauma and 13 from low-energy or sports injuries. One further patient experienced spontaneous improvement later than 1 year after injury. Seven patients were satisfied with their function using a brace or had medical contraindications to surgical treatment, while four patients refused the proposed operation with a tendon transfer. A total of 14 patients of the 26 with residual dorsiflexion weakness elected to have the procedure. Two patients refused to participate in the study, leaving 12 to be included in the study. There were 10 men and two women, with a mean age at time of injury of 28 years (range, 20–51 years) and a mean age at time of surgery of 30 years (range, 21–53 years) (Table 1). The patients completed questionnaires and were invited to a clinical followup including functional tests. The minimum followup after posterior tibial tendon transfer was 8 months (mean, 56 months; range, 8–204 months).
Table 1.
Characteristics and results in 12 patients undergoing posterior tibial tendon transfer
| Patient | Age (years) | Sex | ROM (°) | Ankle dorsiflexion strength (Nm) | AOFAS score (points) | 6-minute walking test distance (m)† | ||
|---|---|---|---|---|---|---|---|---|
| Operated ankle* | Nonoperated ankle | Operated ankle* | Nonoperated ankle | |||||
| 1 | 28 | Male | 55 (69%) | 80 | 97 (19%) | 509 | 97 | 459 (64%) |
| 2 | 42 | Male | 40 (67%) | 60 | 171 (46%) | 369 | 87 | 475 (74%) |
| 3 | 36 | Male | 55 (65%) | 85 | 157 (50%) | 315 | 97 | 681 (101%) |
| 4 | 56 | Female | 70 (74%) | 95 | 48 (21%) | 228 | 78 | 559 (103%) |
| 5 | 25 | Male | 80 (76%) | 105 | 157 (55%) | 286 | 83 | 506 (69%) |
| 6 | 26 | Male | 90 (82%) | 110 | 117 (55%) | 213 | 100 | 723 (100%) |
| 7 | 38 | Female | 70 (70%) | 100 | 17 (8%) | 202 | 75 | 459 (71%) |
| 8 | 27 | Male | 60 (60%) | 100 | 195 (65%) | 302 | 98 | 697 (97%) |
| 9 | 31 | Male | 85 (89%) | 95 | 166 (51%) | 326 | 95 | 663 (95%) |
| 10 | 57 | Male | 60 (57%) | 105 | 104 (38% | 277 | 88 | 639 (112%) |
| 11 | 31 | Male | 60 (67%) | 90 | 124 (53%) | 235 | 88 | 685 (98%) |
| 12 | 21 | Male | 80 (84%) | 95 | 62 (43%) | 144 | 100 | 764 (102%) |
| Mean ± SD | 67 ± 15 (72%) | 118 ± 55 (42%) | 91 ± 9 | 609 ± 111 (90%) | ||||
* Percentage of the nonoperated side in parentheses; †percentage of the normal distance adjusted for sex and age [15] in parentheses; AOFAS = American Orthopaedic Foot and Ankle Society ankle-hindfoot scale.
Before surgical treatment, the function of the tibialis posterior muscle and tendon was assessed. Full inversion strength was a prerequisite for the tendon transfer. No calcaneovalgus deformity was noted before surgery. In patients with no dorsiflexion above neutral position of the ankle (n = 5), a lengthening of the Achilles tendon was performed.
The surgical procedure was performed with the patients in the supine position, with the tourniquet control placed at the thigh. A four-incision technique was used. First, a longitudinal incision for harvesting the posterior tibial tendon was made over the insertion of the posterior tibial tendon to the naviculare bone, enabling the tendon to be detached from the bone. The second incision was made along the calf 7 to 8 cm above the tip of the medial malleolus, and the posterior tibial tendon was then pulled proximally. While avoiding the neurovascular structures, a forceps was introduced on the posterior side of the tibia, a 2- to 3-cm window in the interosseous membrane was made, and the forceps were brought anterior to the fibula where the third skin incision was made slightly distal to the second incision. The harvested tendon was passed close to the posterior surface of the tibia through the gap in the membrana interosseous. The tendon was then passed subcutaneously or under the extensor retinaculum to the dorsum of the foot. The fourth incision was made at the predetermined distal attachment site and 5-mm bone anchors (Twin-fix®; Smith & Nephew, Inc, Andover, MA, USA) were used for attachment of the tendon to the bone under tension. One anchor was used in two patients, two anchors in eight patients, and three anchors in one patient; in one patient, it was not possible to identify from the chart how many anchors were used. The tendon was fixed to the cuboid in five patients, it was fixed to the lateral cuneiform in six patients, and this was not described for one patient. In seven patients, the extensor hallucis longus and extensor digitorum longus were tenodized to the graft to achieve some active dorsiflexion of the toes or counteract hanging toes.
A lower leg splint was used for 3 weeks and replaced by a cast after suture removal for another 5 weeks in which toe-touch weightbearing was allowed. From 8 to 12 weeks, a walker was used during the day, allowing weightbearing as tolerated. A night splint was used until 12 weeks postoperatively. The rehabilitation protocol focused on ROM, strength, and proprioception, starting from 8 weeks postoperatively.
The AOFAS ankle-hindfoot scale was used to assess function. A test battery including dynamometric testing of ankle dorsiflexion strength, passive ROM, and a 6-minute walking test was used. All examinations were done by the same examiner (JH). The dorsiflexion force of the ankle was tested with the knee flexed 30° and the ankle plantarflexed 25° using a hand-held dynamometer (Hoggan microFET2 dynamometer; Hoggan Health Industries Inc, Salt Lake City, UT, USA). The force was tested both on the operated and nonoperated side through repetitive examinations. Ankle ROM was measured with standard goniometric techniques, using a hand-held goniometer (Biomet International Standard Goniometer; Biomet Orthopedics, Warsaw, Indiana, USA), and compared to the contralateral extremity through repetitive examinations.
A full medical history was obtained with focus on postoperative complications, foot and ankle alignment, whether the patients still were using the foot drop brace, and their activity level.
Statistical analyses were performed using SPSS® 18.0 for Windows® (SPSS Inc, Chicago, IL, USA). Normally distributed data are presented as group means and SDs. Differences were considered significant at p levels of 0.05 or less.
Results
We found that 17% of patients (43 of 247) had an injury of the common peroneal nerve with a subsequent partial or complete foot drop at hospital admission. All patients with a common peroneal nerve paresis had injuries to the posterolateral ligaments.
At 1-year followup, 35% of patients (15 of 43) experienced a spontaneous improvement of their foot drop and had no need for further treatment. One patient experienced spontaneous improvement later than 1 year after injury.
In the 12 patients available for evaluation after posterior tibial tendon transfer, the mean AOFAS ankle-hindfoot score was 91 ± 9 (Table 1). No patients used an ankle-foot orthosis for daily activities after posterior tibial tendon transfer. Two patients occasionally used their orthosis during sports activities. Four patients reported a high activity level; one patient is a high national-level athlete. One patient completed a marathon and two participate in downhill mountain biking. The others all participated in recreational sports, including bicycling, cross-country skiing, dancing, squash, football, and distance walking.
The mean ankle dorsiflexion strength was 118 ± 55 Nm, which represented 42% of the strength on the unaffected ankle (p < 0.001) (Table 1). The mean ROM was 67° ± 15°, which represented 72% of the ROM on the unaffected extremity (p < 0.001). The mean 6-minute walking test distance was 609 ± 111 m, which corresponds to 90% of the normal distance adjusted for sex and age [15].
One patient had a postoperative rupture of the tendon graft in the interosseus tunnel 7 months after posterior tibial tendon transfer. He was revised with a transfer of the flexor digitorum longus tendon to the dorsum of the foot. One patient developed an asymptomatic pes planovalgus. No other major foot malalignment was registered, and no other complications were reported.
Discussion
Knee dislocation with common peroneal nerve involvement may lead to a permanent disabling foot drop. Posterior tibial tendon transfer as treatment for foot drop has been reported with good to fair functional results [1, 7, 10, 18, 32], but the previous studies have included patients with a variety of causes for their foot drop. All of the patients included in our study had a knee dislocation as the specific injury causing the nerve damage. We surveyed the percentage of patients developing a common peroneal paresis and the symptom improvement rate of common peroneal nerve paresis after knee dislocation. We also examined the functional results after posterior tibial tendon transfer. We found, in the 247 patients with knee dislocations, 43 (17%) had an injury to the common peroneal nerve with a subsequent foot drop at hospital admission. Fifteen of these patients experienced improvement of symptoms within 1 year, and one patient even later than this; about ½ of the 26 remaining patients were content enough with an ankle-foot orthosis or did not want reconstructive foot surgery to address the dorsiflexion weakness that persisted, and about ½ opted for posterior tibial tendon transfer. Among the 12 who had the tendon transfer and agreed to participate in the study, a high AOFAS score was achieved, but persistent side-to-side differences in terms of ROM and dorsiflexion strength remained.
The main limitation of this study is the small number of patients. However, this is an uncommon complication of an uncommon injury, and no other patient series on the topic have comparable numbers [7, 10, 18, 27, 32]. One limitation in interpreting the results is that there is no consensus in outcome scores for this group. The AOFAS score is widely used in studies for ankle-foot conditions but has never been used for evaluating the results after posterior tibial tendon transfer. Also, the retrospective nature of the study is a limitation. However, it will be difficult to do a prospective study on this patient population, and all other studies are retrospective [7, 10, 18, 32]. Another limitation is that the technique of posterior tibial tendon transfer is complex, and the number of these procedures performed is low; one needs to consider surgeon experience in deciding to what degree the results here (which were obtained in a high-volume trauma setting) are generalizable to other settings.
Forty-three of the 247 patients (17%) in our study sustained a foot drop after the knee dislocation. This result is comparable to other studies showing a common peroneal nerve palsy incidence of 14% to 40% [3, 14, 16, 21, 28]. The differences among the studies might be the result of different patient populations. A high-energy trauma would be expected to produce more serious additional injuries. In this study, the group of knee dislocations (n = 247), the group of patients presenting with foot drop (n = 43), and the group with persistent foot drop (n = 26) included groups of patients about 50% of whom had experienced high-energy trauma. The definition of knee dislocation might also vary in different studies. Our inclusion criteria excluded patients with severe intraarticular fractures (Schenck Classification V) and less severe knee trauma (Schenck Classification I). Some studies also included patients with pure sensory dysfunction of the nerve [3, 16], whereas we focused on patients with severe motor dysfunction due to injury to the common peroneal nerve. We consider a sensory dysfunction as less disabling and chose to exclude these patients. Fifteen of 43 patients (35%) with a motor dysfunction of the common peroneal nerve in our study experienced a spontaneous improvement of symptoms within 1 year, and one patient experienced improvement even more than 1 year after the injury. Previous studies have demonstrated complete or partial recovery of nerve dysfunction in 40% to 50% of the patients [2, 9, 22, 31]. It is known that a partial nerve lesion has a far better prognosis [5]. The range in published results should be interpreted in light of these issues. Some other authors recommend waiting for spontaneous recovery for up to 3 months [5, 9]. Our results show that spontaneous recovery might occur later than this and even more than 1 year after the injury, though the latter is likely quite rare.
To our knowledge, the AOFAS ankle-hindfoot scale has not been used to evaluate posterior tibial tendon transfers. Other studies have instead focused on functional outcome or patient satisfaction as measured in other ways [7, 32], with 10 of 12 patients satisfied in one report [32] and 15 good and two improved in another [7]. Certainly the mean AOFAS score of 91 in this study would appear to hold up well against the results of others [7, 32]. The aim of the tendon transfer is to reduce or prevent pes equinus and improve gait so that the patient can discard the ankle-foot orthosis. The patients included in this study were mainly young with a high activity level, all participating in recreational sports activities and including one high national-level athlete. After posterior tibial tendon transfer, none of the 12 patients used their orthosis for daily activities, and only two patients used the orthosis occasionally for recreational or sports activities. Previous studies have also reported that most patients are able to discard their orthosis, leaving only a minority dependent on it for daily activities [32].
Previous studies also have shown patients achieve approximately 30% of their normal ankle dorsiflexion strength after posterior tibial tendon transfer [32]. In our study, the mean dorsiflexion strength was 42% of that of the unaffected ankle. Other studies have used the Cybex® for dynamometric evaluation [32]. We used a hand-held dynamometer under standardized conditions. All patients were examined by the same examiner and by repetitive examinations of both extremities. Hand-held dynamometers have been shown to have reliability and validity comparable to those of stationary devices such as the Cybex® and Biodex® [8, 24]. The favorable results could be due to the study population consisting of young and active persons, with a high rehabilitation potential. Additionally, the outcome after posterior tibial tendon transfer is reported to be better when the nerve injury is distally located, eg, in the knee region [32]. Our patients achieved an ROM of 72% when compared with the nonoperated ankle. Yeap et al. [32] reported an ROM on the operated side of 40% compared to the nonoperated side.
Our complication rate related to posterior tibial tendon transfer was low, as has also been previously reported [32]. One patient developed an asymptomatic pes planovalgus. This complication is rarely reported [4, 17, 32]. As the posterior tibial tendon is an important structure for arch support, its removal should be expected to produce a lower arch. In our series, there was no preoperative planovalgus deformity, which is an important disposing factor for dysfunction of the posterior tibial tendon. This finding, and the tendency to hindfoot rigidity in cases with foot drop, may protect the foot from sliding into valgus after posterior tibial tendon transfer.
In conclusion, the results after posterior tibial tendon transfer for foot drop are generally good. However, in this study, we present the results after posterior tibial tendon transfer performed exclusively in patients with common peroneal paresis after knee dislocation. This has not previously been studied. We found that our highly active and motivated patient group had a favorable outcome and was able to return to a high activity level after this procedure. We recommend this procedure in patients with a foot drop caused by traumatic injury to the common peroneal nerve that persists beyond 1 year, as spontaneous nerve improvement may occur within the first year.
Acknowledgments
The authors thank Tore Fjalestad MD, PhD for help with the statistical analysis.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial association (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Breukink SO, Spronk CA, Dijkstra PU, Heybroek E, Marck KW. [Transposition of the tendon of M. tibialis posterior an effective treatment of drop foot; retrospective study with follow-up in 12 patients] [in Dutch] Ned Tijdschr Geneeskd. 2000;144:604–608. [PubMed] [Google Scholar]
- 2.Cho D, Saetia K, Lee S, Kline DG, Kim DH. Peroneal nerve injury associated with sports-related knee injury. Neurosurg Focus. 2011;31:E11. doi: 10.3171/2011.9.FOCUS11187. [DOI] [PubMed] [Google Scholar]
- 3.Engebretsen L, Risberg MA, Robertson B, Ludvigsen TC, Johansen S. Outcome after knee dislocations: a 2–9 years follow-up of 85 consecutive patients. Knee Surg Sports Traumatol Arthrosc. 2009;17:1013–1026. doi: 10.1007/s00167-009-0869-y. [DOI] [PubMed] [Google Scholar]
- 4.Gasq D, Molinier F, Reina N, Dupui P, Chiron P, Marque P. Posterior tibial tendon transfer in the spastic brain-damaged adult does not lead to valgus flatfoot. Foot Ankle Surg. 2013;19:182–187. doi: 10.1016/j.fas.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 5.Goitz RJ, Tomaino MM. Management of peroneal nerve injuries associated with knee dislocations. Am J Orthop. 2003;32:14–16. [PubMed] [Google Scholar]
- 6.Green NE, Allen BL. Vascular injuries associated with dislocation of the knee. J Bone Joint Surg Am. 1977;59:236–239. [PubMed] [Google Scholar]
- 7.Hove LM, Nilsen PT. Posterior tibial tendon transfer for drop-foot. 20 cases followed for 1–5 years. Acta Orthop Scand. 1998;69:608–610. doi: 10.3109/17453679808999265. [DOI] [PubMed] [Google Scholar]
- 8.Janssen JC, Le-Ngoc L. Intratester reliability and validity of concentric measurements using a new hand-held dynamometer. Arch Phys Med Rehabil. 2009;90:1541–1547. doi: 10.1016/j.apmr.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 9.Johnson ME, Foster L, DeLee JC. Neurologic and vascular injuries associated with knee ligament injuries. Am Sports Med. 2008;36:2448–2462. doi: 10.1177/0363546508325669. [DOI] [PubMed] [Google Scholar]
- 10.Kilic A, Parmaksizoglu AS, Kabukcuoglu Y, Bilgili F, Sokucu S. [Extramembranous transfer of the tibialis posterior tendon for the correction of drop foot deformity] [in Turkish] Acta Orthop Traumatol Turc. 2008;42:310–315. doi: 10.3944/AOTT.2008.310. [DOI] [PubMed] [Google Scholar]
- 11.Kim DH, Murovic JA, Tiel RL, Kline DG. Management and outcomes in 318 operative common peroneal nerve lesions at the Louisiana State University Health Sciences Center. Neurosurgery. 2004;54:1421–1428; discussion 1428–1429. [DOI] [PubMed]
- 12.Klimkiewicz JJ, Petrie RS, Harner CD. Surgical treatment of combined injury to anterior cruciate ligament, posterior cruciate ligament, and medial structures. Clin Sports Med. 2000;19:479–492, vii. [DOI] [PubMed]
- 13.Malizos KN, Xenakis T, Mavrodontidis AN, Xanthis A, Korobilias AB, Soucacos PN. Knee dislocations and their management: a report of 16 cases. Acta Orthop Scand Suppl. 1997;275:80–83. doi: 10.1080/17453674.1997.11744752. [DOI] [PubMed] [Google Scholar]
- 14.Meyers MH, Harvey JP., Jr Traumatic dislocation of the knee joint: a study of eighteen cases. J Bone Joint Surg Am. 1971;53:16–29. [PubMed] [Google Scholar]
- 15.Motion-online. Available at: http://www.motion-online.dk. Accessed January 30, 2014.
- 16.Niall DM, Nutton RW, Keating JF. Palsy of the common peroneal nerve after traumatic dislocation of the knee. J Bone Joint Surg Br. 2005;87:664–667. doi: 10.1302/0301-620X.87B5.15607. [DOI] [PubMed] [Google Scholar]
- 17.Omid R, Thordarson DB, Charlton TP. Adult-acquired flatfoot deformity following posterior tibialis to dorsum transfer: a case report. Foot Ankle Int. 2008;29:351–353. doi: 10.3113/FAI.2008.0351. [DOI] [PubMed] [Google Scholar]
- 18.Ozkan T, Tuncer S, Ozturk K, Aydin A, Ozkan S. Tibialis posterior tendon transfer for persistent drop foot after peroneal nerve repair. J Reconstr Microsurg. 2009;25:157–164. doi: 10.1055/s-0028-1103502. [DOI] [PubMed] [Google Scholar]
- 19.Rihn JA, Groff YJ, Harner CD, Cha PS. The acutely dislocated knee: evaluation and management. J Am Acad Orthop Surg. 2004;12:334–346. doi: 10.5435/00124635-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Robertson A, Nutton RW, Keating JF. Dislocation of the knee. J Bone Joint Surg Br. 2006;88:706–711. doi: 10.1302/0301-620X.88B6.17448. [DOI] [PubMed] [Google Scholar]
- 21.Shields L, Mital M, Cave EF. Complete dislocation of the knee: experience at the Massachusetts General Hospital. J Trauma. 1969;9:192–215. doi: 10.1097/00005373-196903000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Sisto DJ, Warren RF. Complete knee dislocation: a follow-up study of operative treatment. Clin Orthop Relat Res. 1985;198:94–101. [PubMed] [Google Scholar]
- 23.Stayner LR, Coen MJ. Historic perspectives of treatment algorithms in knee dislocation. Clin Sports Med. 2000;19:399–413. doi: 10.1016/S0278-5919(05)70214-3. [DOI] [PubMed] [Google Scholar]
- 24.Sullivan SJ, Chesley A, Hebert G, McFaull S, Scullion D. The validity and reliability of hand-held dynamometry in assessing isometric external rotator performance. J Orthop Sports Phys Ther. 1988;10:213–217. doi: 10.2519/jospt.1988.10.6.213. [DOI] [PubMed] [Google Scholar]
- 25.Tomaino M, Day C, Papageorgiou C, Harner C, Fu FH. Peroneal nerve palsy following knee dislocation: pathoanatomy and implications for treatment. Knee Surg Sports Traumatol Arthrosc. 2000;8:163–165. doi: 10.1007/s001670050208. [DOI] [PubMed] [Google Scholar]
- 26.Treiman GS, Yellin AE, Weaver FA, Wang S, Ghalambor N, Barlow W, Snyder B, Pentecost MJ. Examination of the patient with a knee dislocation: the case for selective arteriography. Arch Surg. 1992;127:1056–1062; discussion 1062–1053. [DOI] [PubMed]
- 27.Vigasio A, Marcoccio I, Patelli A, Mattiuzzo V, Prestini G. New tendon transfer for correction of drop-foot in common peroneal nerve palsy. Clin Orthop Relat Res. 2008;466:1454–1466. doi: 10.1007/s11999-008-0249-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wascher DC. High-velocity knee dislocation with vascular injury: treatment principles. Clin Sports Med. 2000;19:457–477. doi: 10.1016/S0278-5919(05)70218-0. [DOI] [PubMed] [Google Scholar]
- 29.Wascher DC, Dvirnak PC, DeCoster TA. Knee dislocation: initial assessment and implications for treatment. J Orthop Trauma. 1997;11:525–529. doi: 10.1097/00005131-199710000-00011. [DOI] [PubMed] [Google Scholar]
- 30.Welling RE, Kakkasseril J, Cranley JJ. Complete dislocations of the knee with popliteal vascular injury. J Trauma. 1981;21:450–453. [PubMed] [Google Scholar]
- 31.Wood MB. Peroneal nerve repair: surgical results. Clin Orthop Relat Res. 1991;267:206–210. [PubMed] [Google Scholar]
- 32.Yeap JS, Birch R, Singh D. Long-term results of tibialis posterior tendon transfer for drop-foot. Int Orthop. 2001;25:114–118. doi: 10.1007/s002640100229. [DOI] [PMC free article] [PubMed] [Google Scholar]


