Abstract
Background
Nailing comminuted femur fractures may result in leg shortening, producing significant complications including pelvic tilt, narrowing of the hip joint space, mechanical and functional changes in gait, an increase in energy expenditures, and strains on spinal ligaments, leading to spinal deformities. The frequency of this complication in patients managed with an intramedullary (IM) nail for comminuted diaphyseal fractures is unknown.
Questions/purposes
We therefore determined (1) the frequency of LLDs, (2) whether a specific fracture pattern was associated with LLDs, (3) the frequency of reoperation, and (4) whether revision fixation ultimately corrected the LLD.
Methods
We studied 83 patients with 91 AO/OTA Type B or Type C fractures fixed with either an antegrade or retrograde IM nail from July 2002 through December 2005. There were 60 males and 23 females, with a mean age of 30 years (range, 15–79 years). All underwent a digitized CT scan in the immediate postoperative period. Measurements of both legs were performed. Any fixation producing a discrepancy and requiring a return to surgery was identified.
Results
An mean LLD of 0.58 cm was found in 98% of the patients, but only six (7%) patients had an LLD of greater than 1.25 cm. No fracture pattern or the presentation of bilateral injuries demonstrated a greater incidence of LLD. Of the patients with LLD, two patients refused further surgery while the remaining four patients, two Type B and two Type C fractures, ultimately underwent revision fixation. Repeat CT scans after revision surgery of all four patients demonstrated a residual LLD of only 0.2 cm.
Conclusions
Postoperative CT scans appear to be an efficient method to measure femoral length after IM nailing. Although residual LLDs may be common in comminuted femurs treated with IM nails, most LLDs do not appear to be functionally relevant. When an LLD of greater than 1.5 cm is identified, it should be discussed with the patient, who should be told that potential complications may occur with larger LLDs and that sometimes patients may benefit from repeat surgery.
Level of Evidence
Level IV, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
Intramedullary (IM) nailing of femoral shaft fractures demonstrates high rates of union, infrequent complications, and a reproducible surgical technique [2]. Using an antegrade or retrograde approach and either an indirect or a minimally invasive technique, IM nailing has become an accepted treatment for these injuries. Regardless of the approach, the goal is to preserve the fracture hematoma, minimize soft tissue disruption at the fracture site, and avoid separating small fragments away from the surrounding soft tissue [18].
Unlike open techniques, these methods do not rely on direct visualization of the fracture and an anatomic reduction of the femur. In fractures presenting with no comminution or comminution of less than 50% of the width of the bone, achieving the correct length is performed using fluoroscopy and verifying that cortical contact of the fracture has been achieved. With extensive shattering or segmental comminution, the ability to obtain cortical contact may be lost. Although traction techniques are used to avoid leg shortening, for a few of these unstable fractures, shortening may still occur. If shortening occurs, the leg length discrepancy (LLD) can produce a pelvic tilt [7], narrowing of the hip joint space [25], mechanical and functional changes in gait producing an increase in energy expenditures [9, 16, 27], and strains on spinal ligaments, leading to spinal deformities [5, 6, 32].
When patients present with an LLD, physical examination methods using either a tape measure, from the anterior superior iliac spine to the medial malleolus, or the block method, obtained with patients standing on blocks to level their pelvis [24], are indirect techniques that do not measure the specific length of bones and may be affected by conditions that produce a fixed pelvic tilt. Plain radiographic methods consisting of orthoroentgenograms, scanograms, or a teleoroentgenogram have been shown to be more accurate than clinical methods but may also miscalculate an LLD if flexion of the extremity occurred during the exposure [24]. Other methods to evaluate an LLD have included ultrasound [17] and MRI [20] but have shown less reliability than radiographic methods [24]. Currently, digitalized CT images, using an AP or lateral scout view of the bilateral femurs, appear to be the most cost-effective and reliable method to evaluate LLDs [1].
The problem is in identifying and efficiently correcting any LLD during the perioperative time of fixation. Some intraoperative methods used to prevent shortening have included the preoperative use of a metal ruler marked with lead-impregnated reference lines (Fig. 1), the use of intraoperative rulers [18], or the use of orthopaedic computer navigation systems [12]. Although techniques describing methods to prevent malalignment or malrotation have been reported [13, 18, 19, 21], the problem is that they do not assess length. Given the potential complications associated with LLDs, the question is whether equal lengths of the femur can be obtained at the time of the index surgery when significant comminution is identified on injury radiographs.
Fig. 1A–B.
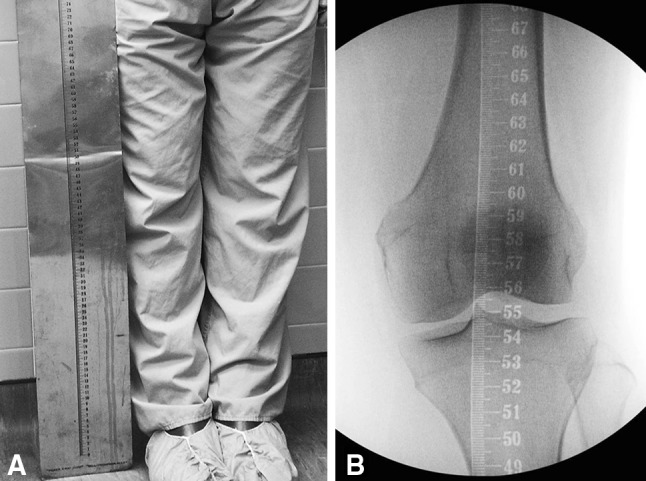
(A) A clinical photograph shows the length of the Bell-Thompson ruler. (B) A fluoroscopic image demonstrates the measurements of the Bell-Thompson ruler as it is projected onto the knee.
We therefore determined (1) the frequency of LLDs, (2) whether a specific fracture pattern was associated with a greater production of LLDs, (3) the frequency of reoperation, and (4) whether the revision fixation ultimately corrected the LLD.
Patients and Methods
After obtaining approval through the Institutional Review Board of the University of South Florida (Tampa, FL, USA), we prospectively evaluated all patients presenting with a diaphyseal femur fracture from July 2002 through December 2005 and treated with an IM device. During this time period, there were a total of 402 femur fractures of which 158 were diaphyseal injuries. These diaphyseal injuries were classified according to the AO/OTA classification system [22] into simple fractures (Type A), wedge fractures (Type B), or complex fractures (Type C). Inclusion criteria for this study consisted of all patients who presented with either a Type B or a Type C fracture pattern that underwent fixation with either an antegrade or retrograde IM nail. Ninety-five patients with 104 fractures were identified. Twelve patients did not undergo a CT scan. Six died and six were discharged before obtaining a scan, leaving 83 patients (60 male, 23 female; 91 fractures), with a mean age of 30 years (range, 15–79 years), available for evaluation. All patients underwent static nailings of their fractures. Patients were excluded if they presented with ipsilateral supracondylar or peritrochanteric femur fractures, open growth plates, or pathologic fractures or underwent definitive fixation using an external fixator, flexible nail, or a plating technique. All femurs were reamed 1 to 1.5 mm larger than the nail inserted.
Patient demographics and clinical data were recorded, including the mechanism of injury, age, sex, associated injuries, whether fractures were closed or open [10], surgical approach (antegrade versus retrograde), whether a fracture table, external fixator, or manual traction was utilized, and operative risk value according to the criteria of the American Society of Anesthesiologists [23].
Seventy-five (91%) patients had unilateral femur fractures and eight patients (9%) had bilateral femur fractures (Table 1). The five males and three females with bilateral injuries had a mean age of 28 years (range, 17–40 years). There were three Type A, seven Type B, and six Type C patterns. There were two open fractures, classified as one Grade I and one Grade IIIA injuries. Two patients presented only with femur fractures and all eight were treated using a retrograde technique. Forty-two patients (51%) sustained a unilateral Type B fracture (Table 1). These 30 males and 12 females had a mean age of 31 years (range, 15–79 years). Twenty-seven patients (64%) presented only with an isolated femur fracture. Seven patients (17%) presented with an open fracture. Six patients presented as with polytrauma and were classified as two Grade I, one Grade II, and three Grade IIIA open injuries. The remaining patient sustained an open Grade II injury. Thirty-one patients (74%), 21 with polytrauma, were managed using a retrograde technique. Thirty-three patients (40%) sustained a Type C fracture (Table 1). These 25 males and eight females had a mean age of 31 years (range, 17–56 years). Twenty-one patients (64%) presented with polytrauma. Ten patients (30%) had open fractures. In four who presented with polytrauma, their fractures were classified as one Grade I, one Grade II, and two Grade IIIA open injuries. The other six patients were classified as three Grade II, one Grade IIIA, and two Grade IIIB open injuries. Twenty-two patients (67%), 17 with polytrauma, were managed with a retrograde technique.
Table 1.
Patient demographics and clinical data
| Variable | Patients with Type B fractures | Patients with Type C fractures | Patients with bilateral fractures |
|---|---|---|---|
| Number of patients | 42 | 33 | 8 |
| Number of fractures | 42 | 33 | 16‡ |
| Age (years)* | 31 (15–79) | 32 (17–56) | 28 (17–40) |
| Number of males/females | 30/12 | 25/8 | 5 M/3 |
| Number of patients with isolated fractures (polytrauma) | 15 (27) | 12 (21) | 2 (6) |
| Type of nailing (number of fractures) | |||
| Antegrade nailing, fracture table (polytrauma) | 11 (6) | 11 (4) | 0 |
| Retrograde nailing, manual traction (polytrauma) | 29 (20) | 21 (16) | 8 (6) |
| Retrograde nailing, external fixator (polytrauma) | 2 (1) | 1 (1) | 0 |
| ASA score (points)* | 1.9 (1–4) | 1.9 (1–3) | 2.1 (1–4) |
| Mechanism of injury (number of patients) | |||
| Motor vehicle accident | 25 | 18 | 7 |
| Motorcycle accident | 5 | 6 | 1 |
| High-energy fall | 5 | 3 | 0 |
| Pedestrian | 3 | 1 | 0 |
| Assault | 2 | 0 | 0 |
| Sporting injury | 1 | 0 | 0 |
| Gunshot wound | 1 | 3 | 0 |
| Crush injury | 0 | 2 | 0 |
| Number of patients with open fractures (polytrauma) | 7 (6) | 10 (4) | 3 (2) |
| LLD (cm)* | 0.44 (0.1–3.8) | 0.78 (0.1–3.36) | 0.53 (0.1–2.0) |
| Number of patients with LLD | 41 (98%) | 33 (100%) | 8 (100%) |
| Number of patients returned to OR due to LLD (polytrauma, open) | 2 (1, 1) | 3 (0, 1)† | 0 |
* Values are expressed as mean, with range in parentheses; †one Type C fracture returned for malrotation; ‡ three Type A fractures seen in bilateral femur fractures; ASA = American Society of Anesthesiologists; LLD = leg length discrepancy; OR = operating room.
Unless medical problems precluded patients from being moved to the CT scanner, the protocol consisted of performing a digitized CT scan on all patients on the first or second postoperative day. Using an AP scout image, all scans were performed using a standard CT scanner (GE Medical Systems, Waukesha, WI, USA). All patients were scanned in a supine position with both hips and knees in complete extension. The measurements were performed superiorly from the central 1/3 of the femoral head at the hip to the central 1/3 of the medial femoral condyle inferiorly at the knee. Using the uninjured side or the noncomminuted fracture for comparison (Type A fracture pattern), measurements of both legs were taken and any fixation producing an LLD and requiring a return to surgery was identified. All measurements were performed by the senior author (DH), but no kappa coefficient was used to measure intraobserver reliability. The CT scan measurements did not assess rotational deformities.
During the study period, our indication for recommending surgery was an LLD measuring 1.25 cm or more. These revision surgeries were recommended to patients and were performed during the hospitalization for the index fracture surgery at a mean of 2 days (range, 1–3 days).
Results
Among the 83 patients treated for a comminuted diaphyseal femur fracture, only six (7%) demonstrated an LLD of 1.25 cm or more. Only one patient had equal leg lengths, and in the remaining 76 patients (92%), all demonstrated a small, measurable LLD (mean, 0.58 cm; range, 0.1–3.8 cm).
Evaluating the fractures demonstrated that neither the fracture pattern itself nor the presence of bilateral injuries contributed to an increase in LLDs. An overall mean LLD of 82 patients (98%) was 0.58 cm. Patients with bilateral injuries had a mean LLD of 0.53 cm (range, 0.1–2 cm). Only one of these patients had an LLD of 1.25 cm or more, measured at 2.0 cm. In the Type B fractures, the mean LLD was 0.44 cm (range, 0.1–3.8). Two patients had an LLD of 1.25 cm or more. The first measured 1.25 cm and the second 3.8 cm. The mean LLD in Type C fractures was 0.78 cm (range, 0.1–3.36 cm). Three patients had an LLD of 1.25 cm or more. The first measured 1.3 cm, the second 1.5 cm, and the third 3.36 cm.
Overall, seven patients (8%) underwent a second surgery as a result of their fracture. One patient was returned and corrected for a malrotation and two patients were revised after they developed a nonunion. Of the six patients identified with an LLD of 1.25 cm or more, two refused any further surgery. Only four patients (5%), two Type B and two Type C, returned to surgery to revise their LLDs (Fig. 2). After revision fixation, all seven patients healed.
Fig. 2A–C.

(A) A CT scan demonstrates a distraction of 1.5 cm after antergrade nailing of a Type C fracture performed on a fracture table. (B) An intraoperative fluoroscopic image shows the distracted femur fracture. (C) Using a back-slapping technique, a fluoroscopy image demonstrates that the distraction has been corrected.
After revision fixation on the four fractures with LLD, all underwent a second CT scan to assess length. Repeat scans demonstrated that all four femurs exhibited a residual LLD of 0.2 cm.
Discussion
IM nailing has become an accepted method of treating diaphyseal femur fractures. Current techniques have demonstrated high rates of union and little morbidity, along with reproducible results regardless of the approach used or whether the patient presented with polytrauma or an isolated injury [2]. For fractures with little or no comminution, obtaining the correct length can usually be verified using fluoroscopy. When the monitor has demonstrated that cortical contact has been achieved, the surgeon can be reasonably certain that the correct length has been restored. However, significant comminution of the femur will often lack bony landmarks to help judge the correct length of the bone, resulting in a longitudinal malalignment and complications associated with an LLD [5–7, 9, 16, 25, 27, 32]. Even using adjunctive methods of fixation such as manual traction, external fixators/femoral distracters, or a fracture table can still result in a LLD. We therefore used postoperative CT scans to determine (1) the frequency of LLDs, (2) whether or not a specific fracture pattern developed more LLDs, (3) the frequency of reoperation, and (4) whether the revision fixation ultimately corrected the LLD.
Our study has several limitations. First, there is no specific measurement or guidelines in the literature to help direct surgeons as to what LLD is unacceptable and should be revised. Empirically, we used 1.25 cm as a cutoff, but this distance may actually be a normal variant. Using the literature as a guide [3, 4, 28, 29, 33], 1.5 cm as a cutoff may be helpful, but again this number may just be an educated guess. Given that some plastic deformation occurs at the time of injury, along with some potential bone loss, we may have to accept that some LLD may be a normal, physiologic variant [28] and that the goal of fixation should therefore be to obtain an LLD that is not functionally relevant (perhaps < 1.0 cm). Secondly, the evaluation of the CT scans was performed by only one person. Although the scans were measured once or twice, there is no kappa coefficient value estimating intraobserver reliability. It is indeed possible that the measurements of these scans are not precise and that the use of others to measure the scans, followed by kappa values for interobserver reliability, may have produced different measurements. The reality however is that this may have only affected two or three patients and would not have affected those with an LLD of greater than 3 cm. Lastly is the concern that there were 12 patients who failed to obtain a scan after their fixation. Six of these patients presented with polytrauma, with significant associated injuries. Their medical conditions precluded them from obtaining a scan and they ultimately died. The remaining six patients were unfortunately discharged before anyone realized that they had not obtained their scans. It is possible that among these 12 patients there may have been some patients with a significant LLD necessitating a revision, but unfortunately this will never be answered.
The first finding of this study was that only six patients (7%) demonstrated an LLD of 1.25 cm or more after index procedure. In 76 patients (92%), an LLD was identified but did not appear to be functionally relevant and may actually have been a normal, physiologic variant. This may be demonstrated in the study by Strecker et al. [28]. In their series, they evaluated 178 healthy paired, atraumatic femurs using a CT scan. What they found was that the median difference between sides was 0.3 cm; at the 95th percentile it was 0.9 cm and at the 99th percentile it was 1.2 cm [28]. However, some caution should be used when interpreting these data. The authors noted that, because of the absence of normal statistical distribution, no mean values were available. Thus, all data were reported as medians and percentiles. Regardless, the small amount of measured LLD in 92% of our patients may actually be a normal variant.
Our second question asked whether a specific fracture pattern or the presence of bilateral femur fractures increased the risk of producing a LLD. Overall, we only had six patients (7%) with a significant LLD, defined in this study as 1.25 cm or more. One would intuitively have expected, because of the lack of visible cortical contact, at the completion of surgery, the Type C fracture pattern would create a greater risk for the development of a significant LLD. Indeed, some authors have reported that up to 44% of their cohorts had a significant LLD after surgery [8, 11, 15, 30]. However, this did not happen in our study. Techniques used as an attempt to avoid a significant LLD, especially in Type C fractures, included measuring both legs with the Bell-Thompson ruler preoperatively and recording that distance. Intraoperative techniques included using external fixators/femoral distracters, manual traction, and a fracture table for antegrade nailing to gain length and using an intraoperative ruler to measure the overall length before insertion of the interlocking screws. For Type B fractures, length was assessed by seeing cortical contact on the monitor. However, even with these approaches, some significant LLDs were identified. Given the associated lower-extremity trauma, the potential for bone loss, and an attempt to prevent future complications, the use of a postoperative CT scan, performed in polytraumatized patients with an open Type C fracture, may help ascertain that an LLD of less than 1.0 cm has been achieved [14].
Our third question concerned the frequency of reoperation as it related to how much shortening was acceptable. Using EMG, Vink and Huson [31] believed that complications do not occur with LLDs of less than 2 to 3 cm while Siffert [26] reported that LLDs of 1.0 to 2.5 cm were rarely symptomatic. However, Gurney et al. [9] demonstrated an LLD of 2 cm had significant effect on oxygen consumption and perceived exertion while authors in three other studies [4, 29, 33] reported that LLDs of 0.64 cm in an athlete or as little as 1.0 cm in the general population produced problems. Indeed, in patients with THA, Edeen et al. [3] found that 32% of patients were aware of a 0.97-cm LLD with up to 24% annoyed when it reached almost 1.48 cm. This sentiment was also echoed by Strecker et al. [28] who recommended correction of any posttraumatic LLD of greater than 1.5 cm. Comparing those recommendations to our study, two patients with an LLD of more 3.0 cm were accepted as necessitating a revision and an argument can be made for the patient with 1.5 cm of distraction. The fourth patient had an LLD of 1.25 cm, and by the time this fracture occurred, during the study period, postoperative CT scans routinely demonstrated an LLD of less than 1.0 cm. An empiric decision was made to return him to surgery to improve his LLD, with the followup CT scans for all four still demonstrating a residual LLD. Therefore, the question of how much LLD is acceptable has not been answered in this study, but a prospective, randomized multicenter trial may be required to answer this question.
Finally, we asked whether the revision fixation ultimately corrected the LLD. The answer would have to be no because, in the four patients who underwent revision for longitudinal malalignment, final scans demonstrated that all four had a residual LLD of 0.2 cm. Two approaches may improve the ability to achieve equal lengths. The first is to anatomically reduce every fragment, potentially stripping their blood supply and producing areas of avascular bone, resulting in more complications without actually achieving equal lengths. The second is the use of intraoperative CT scanning. Although this technology is currently available, it is unknown whether it can be used to provide measurements similar to a regular CT scan.
In conclusion, obtaining equal leg lengths in comminuted femur fractures can be difficult. Regardless of the approach used, the goal should be to obtain an LLD that is less than 1.0 cm because, at this distance, the LLD may actually be a normal variant. In significantly comminuted fractures, a CT scan during the immediate postoperative period can be used to determine whether the LLD is large enough to be of any concern. Care must be taken to ensure that both the hip and knee are in complete extension during the scan to avoid any false positives. Although no concrete guidelines exist for defining what constitutes a significant LLD, we recommend that patients should be informed of potential future complications and a possible return to surgery for any comminuted diaphyseal femur fracture fixed with an LLD of greater than 1.5 cm.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Tampa General Hospital, Tampa, FL, USA.
References
- 1.Aaron A, Weinstein D, Thickman D, Eilert R. Comparison of orthoroentgenography and computed tomography in the measurement of limb-length discrepancy. J Bone Joint Surg Am. 1992;74:897–902. [PubMed] [Google Scholar]
- 2.Canadian Orthopaedic Society Nonunion following intramedullary nailing of the femur with and without reaming: results of a multicenter randomized clinical trial. J Bone Joint Surg Am. 2003;85:2093–2096. [PubMed] [Google Scholar]
- 3.Edeen J, Sharkey PF, Alexander AH. Clinical significance of leg-length inequality after total hip arthroplasty. Am J Orthop. 1995;24:347–351. [PubMed] [Google Scholar]
- 4.Friberg O. Leg length asymmetry in stress fractures: a clinical and radiological study. J Sports Med Phys Fitness. 1982;22:485–488. [PubMed] [Google Scholar]
- 5.Friberg O. Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality. Spine (Phila Pa 1976). 1983;8:643–651. doi: 10.1097/00007632-198309000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Giles LG, Taylor JR. Low-back pain associated with leg length inequality. Spine (Phila Pa 1976). 1981;6:510–521. doi: 10.1097/00007632-198109000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Grill F, Chochole M, Schultz A. Pelvic tilt and leg length discrepancy] [in German. Orthopade. 1990;19:244–262. [PubMed] [Google Scholar]
- 8.Grützner P, Hochstein P, Simon R, Wentzensen A. Determination of torsion angle after shaft fractures of the lower extremity—clinical relevance and measurement techniques] [in German. Chirurg. 1999;70:276–284. doi: 10.1007/s001040050643. [DOI] [PubMed] [Google Scholar]
- 9.Gurney B, Mermier C, Robergs R, Gibson A, Rivero D. Effects of limb-length discrepancy on gait economy and lower-extremity muscle activity in older adults. J Bone Joint Surg Am. 2001;83:907–915. doi: 10.2106/00004623-200106000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Gustillo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24:742–746. doi: 10.1097/00005373-198408000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Harris I, Hatfield A, Walton J. Assessing leg length discrepancy after femoral fracture: clinical examination or computed tomography? ANZ J Surg. 2005;75:319–321. doi: 10.1111/j.1445-2197.2005.03349.x. [DOI] [PubMed] [Google Scholar]
- 12.Hüfner T, Kendoff D, Citak M, Geerling J, Krettek C. Precision in orthopedic computer navigation] [in German. Orthopade. 2006;35:1043–1055. doi: 10.1007/s00132-006-0995-x. [DOI] [PubMed] [Google Scholar]
- 13.Jaarsma RL, Verdonschot N, van der Venne R, van Kampen A. Avoiding rotational malalignment after fractures of the femur by using the profile of the lesser trochanter: an in vitro study. Arch Orthop Trauma Surg. 2005;125:184–187. doi: 10.1007/s00402-004-0790-2. [DOI] [PubMed] [Google Scholar]
- 14.Johnson EE. Acute lengthening of shortened lower extremities after malunion or non-union of a fracture. J Bone Joint Surg Am. 1994;76:379–389. doi: 10.2106/00004623-199403000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Karapinar L, Kaya A, Oztürk H, Altay T, Kayali C. Leg length discrepancies in adult femoral shaft fractures treated with intramedullary nailing. Ulus Travma Acil Cerrahi Derg. 2009;15:256–261. [PubMed] [Google Scholar]
- 16.Kaufman KR, Miller LS, Sutherland DH. Gait asymmetry in patients with limb-length inequality. J Pediat Orthop. 1996;16:144–150. doi: 10.1097/01241398-199603000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Konermann W, Gruber G. Ultrasound determination of leg length. Orthopade. 2002;31:300–305. doi: 10.1007/s00132-001-0298-1. [DOI] [PubMed] [Google Scholar]
- 18.Krettek C, Miclau T, Grün O, Schandelmaier P, Tscherne H. Intraoperative control of axes, rotation and leg length in femoral and tibial fractures: technical note. Injury. 1998;29(suppl 3):S-C29–S-C39. doi: 10.1016/S0020-1383(98)95006-9. [DOI] [PubMed] [Google Scholar]
- 19.Langer JS, Gardner MJ, Ricci WM. The cortical step sign as a tool for assessing and correcting rotational deformity in femoral shaft fractures. J Orthop Trauma. 2010;24:82–88. doi: 10.1097/BOT.0b013e3181b66f96. [DOI] [PubMed] [Google Scholar]
- 20.Leitzes AH, Potter HG, Amaral T, Marx RG, Lyman S, Widman RF. Reliability and accuracy of MRI scanogram in the evaluation of limb length discrepancy. J Pediatr Orthop. 2005;25:747–749. doi: 10.1097/01.bpo.0000173246.12184.a5. [DOI] [PubMed] [Google Scholar]
- 21.Liodakis E, Kenawey M, Liodaki E, Mommsen P, Krettek C, Hankemeier S. The axis-board: an alternative to the cable technique for intraoperative assess of lower limb alignment. Techol Health Care. 2010;18:165–171. doi: 10.3233/THC-2010-0579. [DOI] [PubMed] [Google Scholar]
- 22.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audigé L. Fracture and Dislocation Classification Compendium-2007. J Orthop Trauma. 2007;21(suppl 10):S35–S38. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 23.Owens WD, Felts JA. ASA physical status classification: a study of consistency ratings. Anesthesiology. 1978;49:239–243. doi: 10.1097/00000542-197810000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Sabharwal S, Kumar A. Methods for assessing leg length discrepancy. Clin Orthop Relat Res. 2008;466:2910–2922. doi: 10.1007/s11999-008-0524-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shih-Chieh H, Takahide K, Kozo N, Takashi M, Shiro R, Okazaki H. Narrowing of the joint space of the hip after traumatic shortening of the femur. J Bone Joint Surg Br. 1996;78:718–721. [PubMed] [Google Scholar]
- 26.Siffert RS. Lower limb-length discrepancy. J Bone Joint Surg Am. 1987;69:1100–1106. [PubMed] [Google Scholar]
- 27.Song KT, Halliday SE, Little DG. The effect of limb-length discrepancy on gait. J Bone Joint Surg Am. 1997;79:1690–1698. doi: 10.1302/0301-620X.79B5.7615. [DOI] [PubMed] [Google Scholar]
- 28.Strecker W, Keppler P, Gebhard F, Kinzl L. Length and torsion of the lower limb. J Bone Joint Surg Br. 1997;79:1019–1023. doi: 10.1302/0301-620X.79B6.7701. [DOI] [PubMed] [Google Scholar]
- 29.Subotnick SI. Limb length discrepancies of the lower extremity (the short leg syndrome) J Orthop Sports Phys Ther. 1981;3:11–15. doi: 10.2519/jospt.1981.3.1.11. [DOI] [PubMed] [Google Scholar]
- 30.Suger G, Liener U, Schmelz A, Kinzl L. Correction of post-traumatic diaphyseal malalignment of the lower extremity] [in German. Chirurg. 1998;69:1167–1177. doi: 10.1007/s001040050554. [DOI] [PubMed] [Google Scholar]
- 31.Vink P, Huson A. Lumbar back muscle activity during walking with a leg inequality. Acta Morphol Neerl Scand. 1987;25:261–271. [PubMed] [Google Scholar]
- 32.Vink P, Kamphuisen HA. Leg length inequality, pelvic tilt and lumbar back muscles activity during standing. Clin Biomech. 1989;4:115–117. doi: 10.1016/0268-0033(89)90049-1. [DOI] [PubMed] [Google Scholar]
- 33.White SC, Gilchrist LA, Wilk BE. Asymmetric limb loading with true or simulated leg-length differences. Clin Orthop Relat Res. 2004;421:287–292. doi: 10.1097/01.blo.0000119460.33630.6d. [DOI] [PubMed] [Google Scholar]


