Abstract
Background
The negative symptoms of schizophrenia are not effectively treated with antipsychotic medications. Repetitive transcranial magnetic stimulation (rTMS) is an alternative approach that may be more effective in treating negative symptoms, but there has been little research comparing the effectiveness of different rTMS stimulation protocols.
Objective
Compare the effect of four different rTMS protocols in the treatment of the negative symptoms of schizophrenia.
Methods
Ninety-six patients with schizophrenia who had prominent negative symptoms were randomly assigned to four treatment groups: 10 Hz, 20 Hz, theta burst stimulation (TBS), and mock rTMS (i.e., the control group). In the first three groups, the left dorsolateral prefrontal cortex was stimulated at 80% of the motor threshold five times per week for four weeks. Before and after the treatment, evaluators who were blind to the group assignment of patients administered the Positive and Negative Syndrome Scale (PANSS), the Scale for the Assessment of Negative Symptoms (SANS) and the Treatment Emergent Symptom Scale (TESS).
Results
Three of the 96 patients dropped out during the trial (two from the control group and one from the 20 Hz group). Compared to the control group, after 4 weeks of rTMS treatment all three treatment groups had lower scores on the PANSS negative symptom subscale, the PANSS general psychopathology subscale, and the SANS. The TBS group had significantly larger reductions in these scores than the 10 Hz group and the 20 Hz group, but there were no significant differences between the 10 Hz and 20 Hz groups. There were no pre- versus post-treatment differences in the PANSS positive symptom subscale scores between the four groups. No serious adverse events occurred and there were no statistically significant differences in the TESS scores across the four groups.
Conclusions
We find that rTMS, particularly the TBS stimulation protocol for rTMS, is a safe and effective treatment method for patients with schizophrenia who have prominent negative symptoms. Longitudinal studies with large samples are needed to optimize the rTMS treatment, to identify the stimulation protocol, duration, intensity and treatment interval that provides the best therapeutic result at the lowest risk to the patient.
Keywords: repetitive transcranial magnetic stimulation, schizophrenia, randomized controlled trial, treatment, China
Abstract
背景
抗精神病药物对精神分裂症阴性症状的疗效欠佳。重复经颅磁刺激(rTMS)或许是治疗阴性症状的另一种更有效的方法,但很少有关于不同模式rTMS治疗有效性比较的研究。
目标
比较四种不同模式rTMS对治疗精神分裂症阴性症状的效果。
方法
96例有明显阴性症状的精神分裂症患者随机分为四个治疗组:10赫兹,20赫兹,θ波脉冲刺激(TBS),和模拟rTMS治疗(即对照组)。在前三组,采用运行阈值的80%对左背外侧前额叶皮层进行刺激,每周五次,持续四周。治疗前后,由对患者分组单盲的评估者采用阳性和阴性症状量表(PANSS)、阴性症状评估量表(SANS)和不良反应量表(TESS)进行评估。
结果
96例患者中3名患者中途退出试验(两个来自对照组和一个来自20赫兹组)。与对照组相比,经rTMS治疗4周后,3个治疗组PANSS阴性症状分量表、PANSS一般精神病理分量表和SANS量表得分较低。TBS组这些量表的减分显著大于10赫兹组和20赫兹组,但10赫兹和20赫兹两组间无显著差异。四组之间PANSS阳性症状分量表评分治疗前后没有显著差异。未发生严重不良事件,并且4组TESS评分无统计学显著差异。
结论
我们发现rTMS治疗,特别是TBS刺激模式对于伴有明显阴性症状的精神分裂症患者是一种安全有效的治疗方法。我们需要进行大样本的纵向研究,以优化rTMS治疗,并确定刺激模式,持续时间,刺激强度以及治疗时间间隔,从而以最低的风险为患者提供最佳的治疗结果。
1. Introduction
Negative symptoms of schizophrenia—including blunt affect, avolition, lethargy, and social withdrawal– often lead to deteriorating cognitive functioning, reduced quality of life and heavy family burden.[1] These negative symptoms are also major causes of disability that severely impair patients’ interpersonal relationships and social functioning. Traditional antipsychotic medications have limited efficacy in treating these chronic, often refractory, symptoms.[1] At the time of the advent of atypical antipsychoticmedications there was renewed hope that these negative symptoms – that had proven resistant to traditional antipsychotic medications – would be effectively controlled, but time has shown that these hopes were unfounded.[2] Renewed effort is needed to identify effective strategies for ameliorating the negative symptoms of schizophrenia and, thus, improving the quality of life of individuals afflicted with this often life-long condition.
Repetitive transcranial magnetic stimulation (rTMS) is a neuro-electrophysiological technique developed from transcranial magnetic stimulation (TMS). It applies repetitive TMS to certain brain cortices to improve regional blood flow and, thus, brain metabolism. In targeted brain regions, rTMS influences the activity of various receptors and neurotransmitters (e.g., 5-HT); it can even induce changes in the expression of the genes that regulate neuronal activities.[3] This is the presumed underlying mechanism that leads to the reported positive effects of rTMS in the treatment of neuropsychological disorders.[4] rTMS is a noninvasive method which is safe and easy to administer so it is widely used in the research and treatment of schizophrenia, Parkinson’s disease, epilepsy, and depression.[4]
Neuroimaging studies suggest that the severity of negative symptoms in schizophrenia is inversely associated with the degree of activation of the left prefrontal cortex and other studies report that high frequency stimulation (>1 Hz) can increase cortical neuronal activities while low frequency stimulation (≤1 Hz) can reduce these activities. Based on these findings, the target region for administering rTMS to reduce negative symptoms is usually the left dorsolateral prefrontal cortex (DLPFC) and the most commonly used method of stimulation is high frequency stimulation (i.e., 10 Hz – 20 Hz). However, the results of studies using this method to treat the negative symptoms of schizophrenia have been inconsistent; some[5],[6] report good treatment effects while others[7],[8] find no effect. These inconsistencies may be due to the different stimulation modes for rTMS used in the different studies.[9] These routine stimulation protocols have limited influence on synaptic plasticity, their clinical effect is short-lived and the results can vary greatly between different individuals.[7],[10] To improve the effectiveness of rTMS in the treatment of schizophrenia and other conditions, new stimulation protocols are being developed and tested; one of the most promising new modes of rTMS istheta burst stimulation (TBS). The current study aims to examine the effectiveness of different rTMS stimulation protocols in the treatment of the negative symptoms of schizophrenia.
2. Methods
2.1. Participants
The recruitment and research procedures are shown in Figure 1. All participants were individuals with schizophrenia who sought treatment at the Guangzhou Brain Hospital from January 2011 to June 2013. The inclusion criteria were as follows: (a) meets the diagnostic criteria of schizophrenia specified in DSM-IV[11];(b) 20-55 years of age; (c) a score of ≥20 on the negative subscale of the Positive and Negative Syndrome Scale (PANSS) [12] with at least one of the seven negative symptom items scoring ≥4 points (moderately severe or greater);(d) has had negative symptoms for at least six weeks; (e) a score of <24 on the positive subscale of PANSS; (f) stable psychotic symptoms (i.e., a fluctuation < 10% in the total score of the PANSS negative subscale over the past two weeks); (g) has never been treated with modified electroconvulsive therapy; (h) has normal results in routine physiological examinations and laboratory examinations including ECG and EEG.
Figure 1. Flow chart of the study.
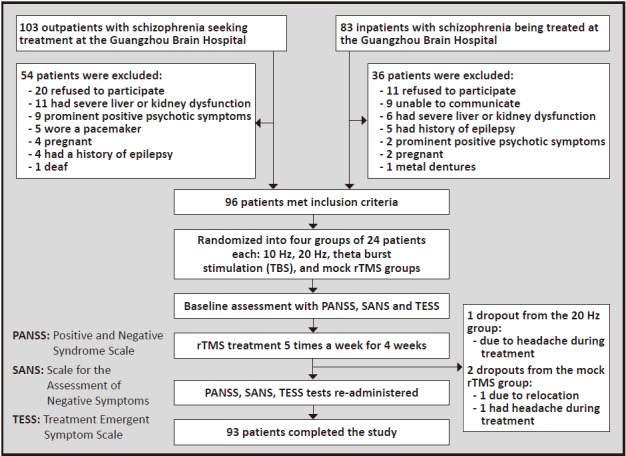
The exclusion criteria were: (a) wearing a pacemaker, cochlear implantor any other metal implant in the brain area near the rTMS stimulation site; (b) mental disorders induced by psychoactive substance; (c) a history of epilepsy, severe physiological illnesses, organic brain diseases or substance abuse; (d) current pregnancy; (e) being impulsive, violent, suicidal, or incapable of effective communication (as determined by a clinical interview).
A total of 96 patients participated in the study; 54 were males and 42 were females. The mean (sd) age was 47.2 (10.2), and the mean years of education was 12.5 (1.2) years. Patients were randomly assigned (using a random number table)to four treatment groups (24 participants in each group): 10 Hz, 20 Hz, TBS, and mock rTMS. As shown in Table 1, there were no significant differences across the four groups in terms of age, level of education, or gender ratio. Most patients used risperidone, quetiapine or olanzapine. The types and dosages of medications in the four groups were similar and did not change throughout the four weeks of rTMS trial.
Table 1.
Comparison of demographic characteristics of patients in the four treatment groups
| Treatment group | n | Age in years mean (sd) |
Female n (%) |
Years of education mean (sd) |
|---|---|---|---|---|
| mock rTMS | 22 | 46.7 (13.1) | 10 (45.5%) | 13.8 (0.1) |
| 10Hz stimulation | 24 | 48.0 (12.2) | 13 (55.2%) | 10.3 (0.3) |
| 20Hz stimulation | 23 | 49.1 (10.6) | 13 (56.5%) | 12.5 (0.3) |
| theta burst stimulation | 24 | 47.7 (11.8) | 11 (45.9%) | 12.9 (0.9) |
| statistic | F=0.89 | χ2=2.28 | F=0.63 | |
| p | 0.32 | 0.23 | 0.52 | |
This study was approved by the institutional review board of Guangzhou Brain Hospital. All the patients or their family members provided signed informed consent.
2.2. Types of treatment
The MagPro R100 rTMS machine (with an MF-125 round electromagnet) manufactured by the Danish company Dantec was used in this study. The stimulation site was the left DLPFC. The rTMS treatment was given five times per week for four weeks, resulting in a total of 20 sessions. The detailed setting and procedures of each group are described as follows. (a) For the 10 Hz group, the butterfly (figure-eight) coil was used. The motor threshold (MT) was determined first by stimulating the scalp once to induce movement of the right lateral interosseous muscle. When at least five movements (with amplitude greater than 0.05 mV in the motor-evoked potential recorded by the EMG) were induced out of ten stimulations, the output intensity of the rTMS was considered the MT. Thirty trains of 5-second and 10 Hz stimulations were performed, with 30-second breaks after each train. There were 1,500 stimulations in total which lasted for about 20 minutes. The initial intensity was 80% of the MT, and then it was gradually increased to 110% of the MT. (b) For the 20 Hz group, the settings were the same as the 10 Hz group except that the stimulation frequency was 20 Hz. (c) For the TBS group, the MF-125 round coil was used. The magnetic stimuli were applied over the same area as in the 10 Hz and 20 Hz groups. The basic train had a frequency of 5 Hz, and the stimulation was given every 200 ms. Three single pulses (50 Hz) were embedded within each 5 Hz pulse. The stimulation intensity was 80% of the MT, and each session had a total of 2,400 pulses which lasted for about 20 minutes. (d) For the mock rTMS group, the electromagnet was turned horizontally to form a 180° angle with the scalp. Other settings were the same with that of the 10 Hz group. Because the magnetic field induced by the stimulator sharply decreases as the distance increases, the magnetic field did not penetrate the skulls of the participants in the mock rTMS group.
2.3. Assessments
The Positive and Negative Syndrome Scale (PANSS)[13] (Cronbach’s alpha= 0.74-0.90), the Scale for the Assessment of Negative Symptoms (SANS),[14] and the Treatment Emergent Symptom Scale (TESS)[14] were used to assess treatment and adverse effects. The percent reduction of the negative scale score in PANSS and the total score of SANS were used to assess the treatment effect. Based on the percentage reductions in each of these scores, participants were grouped into the following four categories: clinically remitted (≥75% reduction), effectively treated (50-74% reduction), improved (25-49% reduction) and not improved (<25% reduction). To reduce bias and to enhance consistency, each patient was simultaneously assessed by two trained attending psychiatrists (who were blind to the patient group assignment) the day before the treatment started and the last day of the treatment. Their inter-rater reliability was good (Kappa=0.75-0.88). The mean value of the two evaluators scores was used in the analysis.
2.4. Statistical analysis
SPSS software version 11.5 (SPSS Inc., Chicago, IL, USA) was used for analysis. Means (sd) were used to describe test scores. Chi-squared tests were used to compare categorical variables including gender and the proportion of effectiveness. Paired t-tests were performed to compare the PANSS and SANS scores before and after treatment in each group. Repeated measures analysis of variance was used to estimate the overall treatment effects. Test scores follow normal distribution and the variance was homogeneous across the four groups. Thus, Fisher’s least significant difference (LSD) test was used for post-hoc comparisons between the four groups. When comparing the proportions of patients in the 4 groups that were effectively treated or improved we used a Tukey-type multiple comparison method based on an arcsin transformation of the original proportions.[15] The significance level was set at 0.05.
3. Results
During the study, one participant from the 20 Hz group dropped out due to severe headaches and two dropped out from the mock rTMS group – one due to moving away and one due to reported severe headaches. The remaining 93 participants completed the full course of the study.
3.1. Comparison of PANSS and SANS overall scores across groups
As shown in Table 2, before treatment, there were no cross-group differences in PANSS and SANS scores. After the four-week rTMS treatment, there were significant differences across groups and across time (F=8.96, p<0.001). Post-hoc comparisons found a significantly larger reduction in PANSS and SANS scores in all three treatment groups compared to the mock rTMS group. Moreover, the reduction was larger in the TBS group than that of the 10 Hz and 20 Hz groups. No significant differences in PANSS and SANS scores were found between the 10 Hz and the 20 Hz group.
Table 2.
Within-group and cross-group comparisons of the total scores of the Positive and Negative Syndrome Scale (PANSS) and the Scale for Assessment of Negative Symptoms (SANS) scores before and after treatment
| Scales | Mock rTMS mean (sd) [n=22] |
10 Hz stimulation mean (sd) [n=24] |
20 Hz stimulation mean (sd) [n=23] |
Theta burst stimulation mean (sd) [n=24] |
F | p |
|---|---|---|---|---|---|---|
| PANSS | ||||||
| before treatment | 78.3 (7.6) | 77.9 (9.2) | 79.2 (6.9) | 76.1 (8.6) | 2.30 | 0.288 |
| after treatment | 76.3 (8.8) | 63.3 (7.7) | 65.8 (7.5) | 58.8 (9.1) | 6.65 | 0.002 |
| F | 1.23 | 4.89 | 5.87 | 6.72 | ||
| p | 0.358 | 0.022 | 0.031 | 0.002 | ||
| SANS | ||||||
| before treatment | 62.8 (10.1) | 59.7 (9.6) | 63.4 (11.2) | 60.3 (10.9) | 1.56 | 0.301 |
| after treatment | 63.5 (9.5) | 49.6 (5.1) | 49.3 (8.1) | 41.3 (10.0) | 5.23 | 0.023 |
| F | 0.08 | 3.30 | 7.77 | 6.80 | ||
| p | 0.136 | 0.042 | 0.007 | 0.005 | ||
3.2. Comparison of PANSS subscales scores before and after treatment
As shown in Table 3, there were no cross-group differences in PANSS subscale scores before treatment. After four weeks of rTMS treatment, repeated measures analysis of variance revealed significant differences across groups and time (F=4.29, p<0.001). Post-hoc comparisons found larger reductions in the PANSS negative subscale score and the general psychopathology subscale score in all three treatment groups compared to the mock rTMS group, in which no reduction was found after four weeks. Moreover, the decrease in the PANSS negative subscale score was greater in the TBS and 20 Hz groups compared to the 10 Hz group. No pre- versus post-treatment differences or cross-group differences were found for the positive subscale scores.
Table 3.
Comparison of the three subscale scores of the Positive and Negative Syndrome Scale (PANSS) across the four treatment groups before and after treatment
| Subscale | Mock rTMS mean (sd) [n=22] |
10 Hz stimulation mean (sd) [n=24] |
20 Hz stimulation mean (sd) [n=23] |
Theta burst stimulation mean (sd) [n=24] |
F | p |
|---|---|---|---|---|---|---|
| negative symptom scale | ||||||
| before treatment | 38.6 (2.1) | 37.6 (5.1) | 36.2 (8.8) | 38.7 (7.4) | 1.37 | 0.123 |
| after treatment | 39.2 (3.3) | 31.0 (0.1) | 26.5 (5.1) | 23.5 (8.1) | 10.55 | 0.003 |
| F | 2.02 | 4.41 | 9.93 | 12.89 | ||
| p | 0.269 | 0.048 | 0.008 | <0.001 | ||
| positive symptom scale | ||||||
| before treatment | 15.1 (1.0) | 14.1 (2.5) | 17.8 (0.0) | 13.3 (3.5) | 1.77 | 0.630 |
| after treatment | 14.0 (0.1) | 13.2 (1.7) | 16.0 (0.4) | 16.0 (0.2) | 2.55 | 0.538 |
| F | 0.93 | 1.11 | 2.00 | 1.41 | ||
| p | 0.478 | 0.566 | 0.704 | 0.671 | ||
| general psychopathology scale | ||||||
| before treatment | 25.8 (3.3) | 26.0 (2.1) | 26.4 (3.5) | 25.4 (2.6) | 2.26 | 0.702 |
| after treatment | 24.1 (2.7) | 19.4 (3.3) | 24.1 (0.8) | 19.9 (1.1) | 8.83 | 0.043 |
| F | 2.80 | 5.42 | 2.64 | 3.03 | ||
| p | 0.170 | 0.037 | 0.169 | 0.033 | ||
3.3. Cross-group comparisons of treatment efficacy
Based on the reduction in PANSS negative subscale scores, 3 patients in the 10 Hz group were ‘effectively treated’ (50-74% reduction), 5 were ‘improved’ (25-49% reduction), and 16 showed no improvement (<25% reduction). In the 20 Hz group 4 were ‘effectively treated’, 5 were ‘improved’ and 14 showed no improvement. In the TBS group 7 were ‘effectively treated’, 7 were ‘improved’ and 10 showed no improvement. In the mock rTMS mock rTMS group no patients were ‘effectively treated’, 1 was ‘improved’ and 21 showed no improvement. Thus the proportions of patients in whom the treatment for negative symptoms was beneficial were 33.3%, 39.1%, 58.3%, and 4.5% for the 10 Hz, 20 Hz, TBS, and mock rTMS groups, respectively. These proportions are significantly different (χ2=15.02, df=3, p=0.002); multi-comparison testing (see methods) found that the proportions in the TBS group and Hz 20 group were significantly greater than the proportion in the mock rTMS group but none of the other pairwise comparisons were statistically significant.
Based on the SANS total scores, the numbers of patients who were effectively treated, improved, and showed no improvement were 2, 5, and 17 in the 10 Hz group; 4, 4, and 15 in the 20 Hz group; 6, 7, and 11 in the TBS group; and0, 2, and 20 in the mock rTMS group. The overall proportions of patients for whom the treatment was considered helpful were 29.2% (10Hz group), 34.8% (20 Hz group), 54.2% (TBS group), and 9.1% (mock rTMS group). These proportions are significantly different (χ2=10.85, df=3, p=0.013); multi-comparison testing found that the proportion who benefitted in the TBS group were significantly greater than the proportion in the mock rTMS group but none of the other pairwise comparisons were statistically significant.
3.4. Comparison of adverse reactions
During the rTMS treatment, two patients dropped out due to severe headache (one from the 20 Hz group and one from the mock rTMS group). Among the remaining 93 patients, five experienced insomnia (one from the 10 Hz group, two from the 20 Hz group, and two from the TBS group). After symptomatic treatment they were all able to complete the four-week rTMS treatment. No patients experienced epilepsy or epilepsy-like symptoms during the treatment. The mean (sd) TESS scores after four weeks of treatment for the 10 Hz, 20 Hz, TBS, and mock rTMS groups were 3.08 (0.93), 3.25 (0.55), 2.99 (0.70), and 2.88 (0.75), respectively. There was no significant difference across groups (F=2.93, p=0.475).
4. Discussion
4.1. Main findings
This double-blind randomized mock rTMS-controlled trial demonstrated that rTMS is an effective treatment method for the negative symptoms of schizophrenia in patients who have prominent negative symptoms. Using two different scales for assessing negative symptoms, all three active rTMS stimulations methods were more effective in reducing negative symptoms over a 4-week trial than mock rTMS and the theta burst stimulation method of rTMS proved more effective than the more routinely used high-frequency 10 Hz and 20 Hz stimulation methods. These dramatic improvements in negative symptoms occurred while the antipsychotic regimen remained constant and during which there was no appreciable change in the level of the positive symptoms of schizophrenia. The results were basically the same when analyzing the PANSS negative symptom subscale scores and SANS scores as continuous measures or when categorizing the percent change in the scores over the four weeks of treatment into three ranked levels of treatment effectiveness.
Overall, rTMS treatment was found to be a safe treatment method. Only one of the 72 participants in the three active rTMS groups had to discontinue treatment due to severe headaches. No seizures or other severe adverse effects were observed during the 4 weeks of treatment in these patients.
A previous study in China that assessed the treatment effect of rTMS using the TBS protocol on the negative symptoms of schizophrenia by Zhang and colleagues[9] also reported that TBS improved negative symptoms and did not change positive symptoms, but the study was small (n=15) and, unlike our study, did not include a comparison group of high-frequency rTMS. A different study by Zheng and colleagues[16] that was limited to male patients also found that TBS improved the negative symptoms of schizophrenia but,unlike our study, they reported that rTMS using the Hz 20 protocol did not improve negative symptoms. This difference from our study may have occurred because they only treated patients for 1 week (versus 4 weeks in our study) and, unlike our study, they enrolled un-selected patients with schizophrenia who did not necessarily have prominent negative symptoms.
4.2. Limitations
The current study has a relatively small sample size, which precluded stratified analysis by gender and age group. The current study only investigated one stimulation site, the DLPFC; the effectiveness of administering rTMS at other locations remains to be investigated. We only assessed the treatment outcome at the end of the rTMS treatment sessions, follow-up studies are needed to determine how long the treatment effect persists after termination of the rTMS intervention and, perhaps more importantly, to assess whether or not the persistence of the effect varies by the type of stimulation method employed.
4.3. Implications
Negative symptoms of schizophrenia are often resistant to pharmacological treatments. They are, nevertheless, frequently the main cause for the severe social disability experienced by individuals with schizophrenia. The evolution of a novel intervention that can effectively treat these symptoms, even if it is only effective for a small proportion of patients with schizophrenia, will be an important addition to the tools mental health professionals can employ to treat this profoundly disabling condition.
Our study confirms that rTMS holds promise as a treatment method for the negative symptoms of schizophrenia. We found that all methods of administering rTMS can substantially improve negative symptoms over a 4-week period. But many questions remain about the mechanism of action of rTMS and about the duration and stability of the clinical effect of this treatment. We also found that TBS – a new mode of rTMS that uses repeated bursts of theta waves – is more effective than traditional modes of rTMS which use high-frequency stimulation. This finding is in line with recent research[6],[7] that reports that by using shorter stimulation time and lower stimulation frequency TBS mode can more safely activate the brain cortex and enhance memory. These results highlight the fact that we are still at the start of the journey of understanding how rTMS works and, more importantly, of how we can get rTMS to work best. Longitudinal studies with large samples of patients will be needed to assess and compare different modes of rTMS used for different durations and repeated at different intervals to determine how to achieve the maximum therapeutic effect at the lowest risk to the patient and at the lowest cost to the community.
Biography

Suhua Zhao graduated with a bachelor’s degree in mental health sciences from the Hunan Medical University in 1994. She is currently a deputy-chief psychiatrist in the Psychiatry Department of the Guangzhou Psychiatric Hospital. She is also an adjunct associate professor and deputy director of the Department of Scientific Education and Information at Guangzhou Medical University. She is a member of the standing committee of the psychiatric section of the Guangzhou Medical Doctor’s Association. Her research interests focus on clinical research about schizophrenia andon the biochemistry of depression.
Funding Statement
This study was supported by the Guangzhou Medical Technology Project (2012A011070001).
Footnotes
Conflict of Interest: The authors declare no conflict of interest.
References
- 1.Wang RZ, Zhang JX, Yuan W, Tang JS, Liu JT, Li X, et al. [A study of insist and psychopathology vignettes in patients with schizophrenia] Shandong Jing Shen Yi Xue. 2001;14(4):237–240. Chinese. [Google Scholar]
- 2.Chen QS, Li YH, Qu LJ. [The research of risperidone combined with fluoxetine in the treatment of negative symptoms of schizophrenia] Jing Shen Yi Xue Za Zhi. 2007;20(5):299–230. Chinese. [Google Scholar]
- 3.Wang XM, Xie JP. [Advances in clinical application of repetitive transcranial magnetic stimulation] Guo Wai Yi Xue: Wu Li Yi Xue Yu Kang Fu Xue Fen Ce. 2004;24(1):43–45. Chinese. [Google Scholar]
- 4.Wang W. [The application of rTMS technology in psychiatry and neurology] Shen Jing Ji Bing Yu Jing Shen Wei Sheng. 2007;7(3):233–236. Chinese. [Google Scholar]
- 5.Prikryl B, Kasparek T, Skotakova S, Ustohal L, Kucerova H, Ceskova E. Treatment of negative symptoms of schizophrenia using repetitive transcranial magnetic stimulation in a double-blind randomized mock rTMSled study. Schizophr Res. 2007;95(1-3):151–157. doi: 10.1016/j.schres.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 6.Mogg A, Purvis R, Eranti S, Contell F, Taylor JP, Nicholson T, et al. Repetitive transcranial magnetic stimulation for negative symptoms of schizophrenia: a randomized mock rTMSled pilot study. Schizophr Res. 2007;93(1-3):221–228. doi: 10.4088/JCP.08r04808yel. [DOI] [PubMed] [Google Scholar]
- 7.Saba G, Verdun CM, Kaialou K, Rocamora JF, Dumortier G, Benadhira R, et al. Transcranial magnetic stimulation in the treatment of schizophrenia: a double blind sham mock rTMSled study. J Psychiatr Res. 2006;40(2):147–152. doi: 10.1016/j.jpsychires.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 8.Soekadar SR, Arfeller C, Rilk A, Plontke SK, Plewnia C. Theta burst stimulation in the treatment of incapacitating tinnitus accompanied by severe depression. CNS Spectr. 2009;14(4):208–211. doi: 10.1017/s1092852900020228. [DOI] [PubMed] [Google Scholar]
- 9.Zhang ZJ, Zhang XK, Li H, Zhong XL, Chen ZW, Liao LW, et al. [Double-blind randomized mock rTMSled trial of repetitive transcranial magnetic stimulation in the treatment of the negative symptoms of schizophrenia] Shanghai Jing Shen Yi Xue. 2010;22(5):262–265. Chinese. [Google Scholar]
- 10.Freitas C, Fregni F, Pascual-Leone A. Meta-analysis of the effects of repetitive transcranial magnetic stimulation (rTMS) on negative and positive symptoms in schizophrenia. Schizophr Res. 2009;108(1-3):11–24. doi: 10.1016/j.schres.2008.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington: American Psychiatric Association; 1994. [Google Scholar]
- 12.Goyal N, NizamieSH , Desarkar P. Efficacy of adjuvant high frequency repetitive transcranial magnetic stimulation on negative and positive symptoms of schizophrenia: preliminary results of a double blind sham-mock rTMSled study. J Neuropsychiatry Clin Neurosci. 2007;19(4):464–467. doi: 10.1176/jnp.2007.19.4.464. [DOI] [PubMed] [Google Scholar]
- 13.Si TM, Yang JZ, Shu L, Wang XL, Kong QM, Zhou Mo, et al. [The reliability, validity of PANSS and its implication] Zhongguo Xin Li Wei Sheng Za Zhi. 2004;18(1):45–47. doi: 10.3321/j.issn:1000-6729.2004.01.016. Chinese. [DOI] [Google Scholar]
- 14.Zhang MY. [Handbook of Psychiatric Rating Scales] Changsha: Hunan Science and Technology Press; 2003. pp. 81–201. Chinese. [Google Scholar]
- 15.Zar HG. Biostatistical Analysis (4th edition) Prentice Hall: New Jersey; 1999. pp. 563–565. [Google Scholar]
- 16.Zheng LN, Guo Q, LI H, LI CB, Wang JJ. [Effects of repetitive transcranial magnetic stimulation with different paradigms on the cognitive function and psychotic symptoms of schizophrenia patients] Beijing Da Xue Xue Bao (Yi Xue Ban) 2012;44(5):732–736. Chinese. [PubMed] [Google Scholar]


