Abstract
Background
Cardiovascular diseases are increasingly important in China, but the prevalence of risk factors for cardiovascular diseases in the indigent mentally ill are unknown.
Aim
Assess the prevalence of four key risk factors for cardiovascular disease -- hypertension, hyperglycemia, hyperlipidemia and smoking – among homeless patients with schizophrenia and identify factors associated with the presence of these risk factors.
Methods
We reviewed medical charts of 181 homeless and 181 non-homeless patients with schizophrenia or schizophreniform disorder admitted to the Shanghai Jiading Mental Health Center between May 2007 and April 2013. Demographic characteristics and risk factors of cardiovascular events were compared between the two groups. Logistic regression models identified the factors that were associated with the presence of one or more of the four risk factors.
Results
The prevalence of hypertension and hyperlipidemia were 19 to 20% in both males and females in the two groups; these rates are similar to those reported in the general population. The prevalence of hyperglycemia ranged from 11 to 15% among males and females in the two groups. Smoking was highly prevalent in male patients (82% in homeless males and 78% in non-homeless males) but, like in China generally, much less prevalent in female patients (7% in homeless females and 5% in non-homeless females). The logistic regression analysis found that male gender, older age, and urban (vs. rural) residence were independently associated with the presence of one or more of the four cardiovascular risk factors. Homelessness was not associated with the presence of cardiovascular risk factors.
Conclusion
This study is the first known report on cardiovascular risk factors among homeless mentally ill in China. The study did not assess several important factors (such as the type, dose and duration of use of antipsychotic medication) but it was, nevertheless, able to show that, unlike in high-income countries, homelessness is not related to elevated risk of cardiovascular disease in Chinese individuals with mental illnesses. Prospective studies with the growing number of homeless individuals in China will be needed to get a clearer picture of the best ways to provide them with the health care services they need.
Keywords: homeless, schizophrenia, cardiovascular risk factor, hyperlipidemia, hypertension, hyperglycemia, smoking, China
Abstract
背景
心血管疾病在中国日益增长,但是贫困精神病患者心血管疾病的危险因素患病率尚不明确。
目标
评估无家可归的精神分裂症患者中心血管疾病四个主要危险因素的患病率 - 高血压,高血糖,高血脂及吸烟 - 并确定与这些危险因素相关的因素。
方法
我们回顾了从2007年5月到2013年4月期间,在上海嘉定精神卫生中心住院的精神分裂症以及分裂样精神病患者病历,包括181名无家可归的患者和181非无家可归的患者。比较了两组间人口学特征和心血管事件的危险因素。使用逻辑回归模型确定了与四个风险因素中一种或多种存在关联的因素。
结果
两组患者的高血压和高血脂症的患病率范围为19%到20%(男性和女性的患病率范围相同);这些比率和一般人群报道的相似。两组患者的高血糖患病率介于11%和15%之间(男性和女性的患病率范围相同)。在男性患者中吸烟是非常普遍的(无家可归男性吸烟率82%,非无家可归男性吸烟率78%),但是在中国女性患者吸烟远没有那么普遍(无家可归女性吸烟率7%,非无家可归女性吸烟率5%)。 Logistic回归分析发现,男性,年龄,城市(与农村相比)与四大心血管危险因素中的一种或多种独立相关。无家可归与心血管危险因素的患病率不相关。
结论
本研究是对中国流浪精神病患者的心血管危险因素的第一个研究报告。这项研究有几个重要因素没有评估(如抗精神病药物的类型、剂量和使用时间),尽管如此,该研究还是能表明在中国,流浪与精神疾病患者心血管疾病风险增高无关,与高等收入国家不同。对于中国不断增多的流浪者而言,还需要进一步的前瞻性研究来探索他们所需的最佳医疗服务模式。
1. Introduction
Cardiovascular disease is a common non-communicable disease worldwide. According to the Chinese Cardiovascular Disease Report 2011,[1] 230 million Chinese citizens have cardiovascular diseases, accounting for 41% all deaths in the country. Studies in China confirm findings from other countries that identify hypertension, hyperlipidemia, diabetes, smoking and being over-weight as major risk factors for cardiovascular diseases.[2],[3]
Research studies from other countries report that cardiovascular diseases are prevalent among homeless individuals and a more common cause of death among homeless persons than among persons of the same age who are not homeless.[4] Poor diet, lack of exercise and limited health care probably contribute to the higher risk of heart disease among the homeless. In China schizophrenia is the most common mental disorder among homeless individuals.[5] Many of these individuals are treated with antipsychotic medications which can cause metabolic syndrome when used for prolonged periods,[6] substantially increasing their risk of cardiovascular diseases.
But there has been no research about the preva-lence of cardiovascular risk factors in the homeless mentally ill in China. The itinerant status of these individuals makes them a particularly difficult group to study. However, the new Shanghai Mental Health Act has provided targeted funds for treating homeless persons with mental disorders, so it is now feasible to identify relatively large numbers of these individuals. Between 2007 and 2013 more than 300 homeless people were admitted to the Shanghai Jiading Mental Health Center, the designated hospital to treat homeless people with mental disorders by the Shanghai’s Public Security Bureau and Civil Affairs Bureau. We used the opportunity afforded by this arrangement to assess the prevalence of cardiovascular risk factors in homeless individuals with schizophrenia in Shanghai. We conducted a retrospective chart review comparing the prevalence of four major cardiovascular risk factors – hypertension, dyslipidemia, diabetes, and smoking – in admitted individuals with schizophrenia or schizophreniform disorder who were and were not homeless.
2. Methods
2.1. Participants
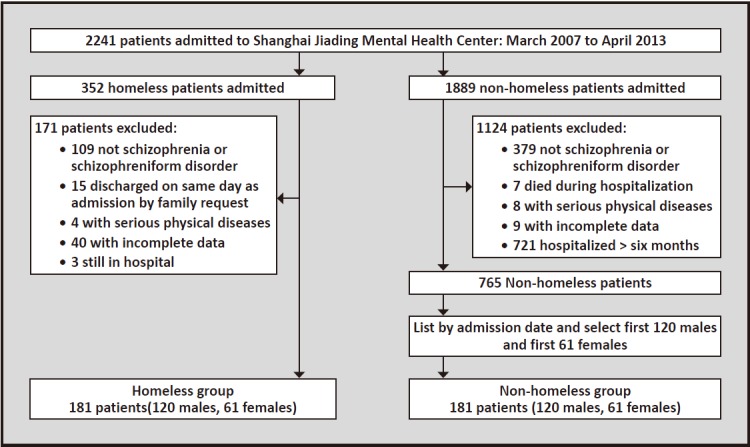
The enrollment of patients for this analysis is shown in Figure 1. There were a total of 2241 inpatients admitted to the Shanghai Jiading Mental Health Center between March 2007 and April 2013, among whom 352 were homeless and 1889 were not. In this study the operational definition of ‘homelessness’ is as follows: a mentally ill individual with no place to live who has no known guardian or for whom the guardian cannot be contacted who is transported to the hospital by police or by emergency services personnel. Among the homeless patients, 181 (120 males and 61 females) met the following inclusion and exclusion criteria: (a) admitting diagnosis of schizophrenia or schizophreniform disorder (it is often difficult to obtain prior histories on indigent individuals admitted with psychotic conditions, so the schizophreniform disorder diagnosis is given if there is no confirmation about the duration of the condition); (b) had no serious physical conditions; (c) duration of hospitalization was greater than one day but less than six months; (e) the individual had been discharged by the time the analysis was conducted in late 2013; and (e) the medical chart included information on all four cardiovascular risk factors being assessed in the study. Among the non-homeless patients admitted during this time, 765 met these inclusion and exclusion criteria; these individuals were sorted according to the date of discharge and then the medical charts of the first 120 male patients and the first 61 female patients were selected to constitute the non-homeless comparison group used in our analysis.
Figure 1. Flow chart of the study.
This study was approved by the Ethics Committee of the Shanghai Jiading Mental Health Center.
2.2. Assessment
In this study, all patients were assessed by two psychiatrists (one senior psychiatrist and one attending psychiatrist) who made the diagnosis based on the Chinese Classification of Mental Disorders, 3rd edition (CCMD-3).[7] The inter-rater reliability for this diagnosis was good between the two psychiatrists (kappa=0.82).
Sociodemographic factors, clinical characteristics, and cardiovascular risk factor data were abstracted from the patients’ hospital charts. Factors collected included gender, age, marital status, occupation, educational level, residency (urban or rural), personal monthly income, previous history of being a vagrant (defined as follows: stayed in a shelter or wandering away from home for more than 1 day) and history of smoking (both current and ex-smokers were considered smokers in this study). Information about risk factors for cardiovascular diseases collected on admission included blood pressure, total cholesterol (TC), high-density lipoprotein (HDL), low-density lipoprotein (LDL), triglycerides (TG) and fasting blood glucose. Routine admission assessments also included serum uric acid and an ultrasound of the liver.
Hypertension, hyperglycemia, hyperlipidemia and smoking were considered risk factors of cardiovascular diseases in this study. (Unfortunately, weights and heights were not obtained on all patients so we were not able to include body mass index as one of the risk factors considered in the study.) Hypertension was defined as a systolic blood pressure greater than 140 mmHg, diastolic blood pressure greater than 90 mmHg, or taking any antihypertensive medications.[8] The definition of hyperglycemia was based on criteria specified by The Chinese Guidelines for the Prevention of Type 2 Diabetes (version 2007)[9] published by the Chinese Medical Association Diabetes Society: patients with a fasting blood glucose greater than 6.0 mmol/L or who were taking anti-diabetic medications were deemed as having hyperglycemia. The definition of hyperlipidemia was based on The Chinese Guidelines for the Prevention of Adult Dyslipidemia.[10] Patients with serum TC greater than 5.72 mmol/L, serum TG greater than 1.7 mmol/L, or serum LDL-C greater than 3.6 mmol/L were deemed as having hyperlipidemia. The definition of hyperuricemia was a serum uric acid level greater than 420 µmol/L for males or greater than 367 µmol/L for females.[11] Fatty liver was diagnosed according to the results of the liver ultrasound.
2.3. Statistical analysis
SPSS version 17.0 was used for data entry and analy-sis. Normally distributed continuous variables were described using means and standard deviations; categorical data were presented as frequencies and proportions. When comparing the means of the two samples, a kurtosis-skewness test was first conducted to ensure the data were normally distributed; if not, a Mann-Whitney U test was used instead of the two-sample t-test. Chi-squared tests or Fisher Exact tests were used to compare proportions. The level of cardiovascular risk was assessed by computing the number of the four risk factors – hypertension, hyperlipidemia, hyperglycemia, and smoking – present in each individual. Logistic regression was used to identify the factors that were independently related to the presence of any (i.e., one or more) of the four cardiovascular risk factors. Independent variables considered included current homelessness, male gender, age (dichotomized as below 45 vs. 45 and above), marital status (currently married vs. other), educational status (less than high school vs. high school and above), personal monthly income (under 1000 Renminbi vs. 1000 Renmibi and above [1000 Renmibi=$170]), occupational status (currently employed vs. unemployed), residency (registered urban resident vs. rural resident), and prior history of vagrancy (yes vs no). The group membership was first entered into the regression model and then the remainder of the variables were entered by a backward stepwise procedure that identified variables that were independently associated with the presence of any cardiovascular risk factor. Separate logistic regression models were also generated for the homeless and non-homeless groups to determine if the pattern of associated factors for cardiovascular risk varied for these two groups. The statistical significance level was set at p<0.05 (two-sided) for all tests.
3. Results
3.1. Characteristics of the sample and comparison of cardiovascular risk factors between the two groups and between males and females within each group
The baseline characteristics of the two groups of inpatients are shown in Table 1. The gender of the two groups was balanced in the design of the study and the mean age of the two groups was not significantly different. Compared to non-homeless inpatients, the homeless group had significantly shorter index hospitalizations, were less educated, were less likely to be a registered urban resident, and were more likely to have hyperuricemia and a fatty liver. The four key risk factors for cardiovascular disease were quite common in both groups of patients but the prevalence of each risk factor and the number of risk factors present were not significantly different between the two groups. As shown in Table 2, in both groups there were no statistically significant differences in the prevalence of hypertension, hyperglycemia or hyperlipidemia between males and females, but male patients were much more likely to be smokers and, consequently, more likely to have multiple cardiovascular risk factors than female patients.
Table 1.
Basic characteristics of two groups
| Characteristics | Homeless group (n=181) |
Non-homeless group (n=181) |
statistic | p |
|---|---|---|---|---|
| Mean (sd) age in years | 33.8 (12.0) | 35.6 (11.7) | t=-1.41 | 0.159 |
| Mean (sd) days index hospitalization | 36.9 (44.9) | 61.9 (58.6) | z=-4.55 | <0.001 |
| Male [n (%)] | 120 (66.3%) | 120 (66.3%) | -- | -- |
| Previous history of vagrancy [n (%)] | 111 (61.3%) | 68 (37.6%) | χ2=0.43 | <0.001 |
| Currently married [n (%)] | 64 (35.4%) | 69 (38.1%) | χ2=0.30 | 0.586 |
| Employed [n (%)] | 22 (12.2%) | 20 (11.0%) | χ2=0.11 | 0.743 |
| Did not complete high school [n (%)] | 147 (81.2%) | 130 (71.8%) | χ2=4.44 | 0.035 |
| Urban household registration [n (%)] | 32 (17.7%) | 72 (39.8%) | χ2=21.59 | <0.001 |
| Monthly income below 1000 Renminbi [n (%)] | 155 (85.6%) | 161 (89.0%) | χ2=0.90 | 0.344 |
| Diagnosis of schizophrenia [n (%)] | 63 (34.8%) | 59 (32.6%) | χ2=0.20 | 0.656 |
| Hypertension [n (%)] | 35 (19.3%) | 35 (19.3%) | χ2=0.00 | >0.999 |
| Hyperglycemia [n (%)] | 25 (13.8%) | 21 (11.6%) | χ2=0.22 | 0.640 |
| Hyperlipidemia [n (%)] | 37 (20.4%) | 36 (19.9%) | χ2=0.02 | 0.896 |
| Smoker [n (%)] | 102 (56.4%) | 96 (53.0%) | χ2=0.40 | 0.526 |
| Number of cardiovascular risk factors [n (%)] | ||||
| None | 48 (26.5%) | 49 (27.1%) | ||
| One | 86 (47.5%) | 92 (50.8%) | ||
| Two | 39 (21.5%) | 31 (17.1%) | z=-4.23 | 0.672 |
| Three | 7 (3.9%) | 9 (5.0%) | ||
| Four | 1 (0.6%) | 0 (0.0%) | ||
| Taking anti-hypertensive medication [n (%)] | 3 (1.7%) | 15 (8.3%) | χ2=10.77 | <0.001 |
| Taking anti-diabetic medications [n (%)] | 1 (0.6%) | 8 (4.4%) | Fisher’s exact | 0.037 |
| Hyperuricemia [n (%)] | 6 (1.7%) | 15 (8.3%) | χ2=4.10 | 0.043 |
| Fatty liver on ultrasound [n (%)] | 8 (4.4%) | 18 (9.9%) | χ2=4.14 | 0.042 |
Table 2.
Cardiovascular risk factors between different genders in the two groups
| Risk factors | Homeless group | Non-homeless group | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Males (N=120) |
Females (N=61) |
statistic | p | Males (N=120) |
Females (N=61) |
statistic | p | ||
| Hypertension | 24 (20.0%) | 11 (18.0%) | χ2=0.10 | 0.751 | 23 (19.2%) | 12 (19.7%) | χ2=0.07 | 0.94 | |
| Hyperglycemia | 16 (13.3%) | 9 (14.8%) | χ2=0.07 | 0.793 | 13 (10.8%) | 8 (13.1%) | χ2=1.26 | 0.26 | |
| Hyperlipidemia | 25 (20.8%) | 12 (19.7%) | χ2=0.03 | 0.855 | 24 (20.0%) | 12 (19.7%) | χ2=0.00 | 0.96 | |
| Smoker | 98 (81.7%) | 4 (6.6%) | χ2=90.49 | <0.001 | 93 (77.5%) | 3 (4.9%) | χ2=73.71 | <0.001 | |
| Taking anti-hypertensive medication | 2 (1.7%) | 1 (1.6%) | Fisher’s exact | 1.000 | 9 (7.5%) | 6 (9.8%) | χ2=0.38 | 0.537 | |
| Taking anti-diabetic medications | 0 (0.0%) | 1 (1.6%) | Fisher’s exact | 0.543 | 5 (4.2%) | 3 (4.9%) | Fisher’s exact | 1.000 | |
| Number of cardiovascular risk factors | |||||||||
| None | 14 (11.7%) | 34 (55.7%) | 17 (14.2%) | 32 (52.5%) | |||||
| One | 66 (55.0%) | 20 (32.8%) | 67 (55.8%) | 25 (41.0%) | |||||
| Two | 32 (26.7%) | 7 (11.5%) | z=-3.57 | <0.001 | 27 (22.5%) | 4 (6.6%) | z=-3.59 | <0.001 | |
| Three | 8 (6.7%) | 0 (0.0%) | 9 (7.5%) | 0 (0.0%) | |||||
| Four | 1 (0.8%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |||||
3.2. Patient characteristics associated with presence of cardiovascular disease risk factors
Logistic regression was used to identify variables independently associated with cardiovascular risk in all patients and, separately, in the homeless and non-homeless groups. As shown in Table 3, male gender and being 45 years of age or older was associated with having one or more of the four cardiovascular risk factors in both the homeless and non-homeless groups. There were three additional factors independently associated with having cardiovascular risk factors in the homeless group that did not emerge in the non-homeless group: having a relatively high personal income, having an urban residence registration, and having a history of prior vagrancy. When combining both the homeless and non-homeless groups, membership in the homeless group (i.e., being admitted by police in the absence of available guardians) was not significantly associated with having cardiovascular risk factors, but being an urban resident was significantly associated with the presence of cardiovascular risk factors.
Table 3.
Logistic regression analyses of factors associated with cardiovascular risk in all subjects, homeless subjects and non-homeless subjectsa
| β | SE | Wald χ2 | p | OR | 95% CI of OR | |
|---|---|---|---|---|---|---|
| ALL SUBJECTS (N=362)b | ||||||
| Homeless (v. non-homeless) | -0.525 | 0.286 | 3.36 | 0.067 | 0.59 | 0.34-1.04 |
| Male | 2.546 | 0.300 | 71.93 | <0.001 | 12.76 | 7.08-22.98 |
| 45 years of age or older | -2.583 | 0.573 | 20.35 | <0.001 | 13.24 | 4.31-40.67 |
| Urban resident | 0.754 | 0.334 | 5.09 | 0.024 | 2.13 | 1.10-4.09 |
| HOMELESS SUBJECTS (n=181) | ||||||
| Male | 3.060 | 0.487 | 39.55 | <0.001 | 21.33 | 8.22-55.37 |
| 45 years of age or older | -1.991 | 0.747 | 7.11 | 0.008 | 7.32 | 1.69-31.65 |
| Income >1000 RMB/month | 0.802 | 0.398 | 4.06 | 0.044 | 2.23 | 1.02-4.86 |
| Urban residence permit | -2.507 | 0.744 | 11.36 | 0.001 | 12.27 | 2.85-52.71 |
| History of vagrancy | 1.010 | 0.442 | 5.23 | 0.022 | 2.75 | 1.15-6.53 |
| NON-HOMELESS SUBJECTS (n=181) | ||||||
| Male | 2.417 | 0.407 | 35.30 | <0.001 | 11.22 | 5.05-24.90 |
| 45 years of age or older | 3.418 | 1.068 | 10.25 | 0.001 | 30.51 | 3.76-247.33 |
OR, odds ratio; CI, confidence interval; RMB, Renmibi (1$US=6.15 RMB)
aBackwards stepwise regression with the following variables considered: gender, age, marital status, education level, personal income, employment status, residence status (urban v. rural) and prior history of vagrancy
bGroup membership variable (homeless v. non-homeless) is forced into model, other variables remain after backward stepwise methods used to remove non-significant variables
4. Discussion
4.1. Main findings
To the best of our knowledge, this is the first study that describes the prevalence of cardiovascular risk factors among homeless and non-homeless individuals with schizophrenia in China. The analysis was based on a retrospective chart review of homeless and non-homeless individuals from Shanghai, so it was only able to consider a limited number of variables. Nevertheless, it provides a very different picture of cardiovascular risk factors in Chinese individuals with mental illnesses than that reported in high-income countries. First, homelessness (defined in this study as individuals requiring a psychiatric hospitalization who do not have a place to live or an identified family member or guardian) is not associated with the prevalence of the main cardiovascular risk factors – hypertension, smoking, hyperlipidemia, or hyperglycemia. The main factors related to the prevalence of these risk factors in persons with schizophrenia or schizophreniform disorder are the same as those in the general popu-lation: male gender and increasing age. Urban (versus rural) residency is another factor associated with the presence of cardiovascular risk factors in individuals with schizophrenia or schizophreniform disorder who are admitted to hospital, presumably due to differences in the urban and rural lifestyles in China. And among homeless individuals admitted to a psychiatric hospital, having a higher income and a prior history of vagrancy is also associated with the presence of one or more cardiovascular risk factors.
We found a prevalence of hypertension of 19 to 20% in both males and females with schizophrenia or schizophreniform disorder admitted to a large psychiatric hospital in Shanghai. This prevalence is similar to the national prevalence figure from the fourth survey on hypertension conducted in 2002,[12] and slightly lower than the 23% prevalence (among individuals 15 years of age and older) estimated from a systematic review about the prevalence of hypertension in China during 2000-2010.[13] This finding is quite different from that of previous studies in high-income countries that report a much higher prevalence of hypertension in the homeless population.[3],[4] One possible explanation is that in China both homeless and non-homeless individuals with schizophrenia live in relative poverty, limiting the availability of the dietary and lifestyle factors associated with hypertension.
Our findings showed that smoking is highly preva-lent among male patients with schizophrenia (82% in homeless males and 78% in non-homeless males) which is similar to reports from high-income countries.[3],[4] In contrast, smoking in Chinese females with schizophrenia (7% in homeless females and 5% in non-homeless females) was much lower than the 57% prevalence reported in studies from high-income countries.[4] We consider this a reflection of the differences in the smoking culture between China – where smoking is uncommon in females – and that in high-income countries. Nonetheless, this finding highlights the need for tobacco control initiatives among male patients with schizophrenia in China.[14]
Our study also found that non-homeless patients with schizophrenia or schizophreniform disorder were more likely to have hyperuricemia and fatty liver compared to the homeless patients. These two conditions were not considered primary risk factors for cardiovascular disease in this study but they have, nevertheless been linked to cardiovascular conditions.[15],[16],[17],[18] Though less prevalent than hypertension or other cardiovascular risk factors, they represent serious health problems that would benefit from early recognition and management; further research is needed to confirm this observation and to identify the possible reasons.
4.2. Limitations
This study only included patients with schizophrenia (and schizophreniform disorder) who were admitted to a single hospital in Shanghai, so the relevance of the findings for community-dwellers with schizophrenia or to those with other types of mental illnesses is unknown. The analysis is based on a retrospective chart review of discharged psychiatric inpatients, so the range of cardiovascular risk factors considered was, necessarily, narrow. Many factors of potential relevance to cardiovascular risk were not obtained: body mass index; family history of heart disease; alcohol and other substance use history; and exercise status. We were, for example, not able to differentiate ex-smokers from current smokers. And, given the indigent nature of the subjects, the past psychiatric history was often incomplete, particularly as regards the type, dosage and duration of use of antipsychotic medications.
4.3. Implications
The rapid economic growth of China had been associated with both an increase in the prevalence of lifestyle risk factors for cardiovascular diseases and a rise in the number of homeless individuals with mental disorders in metropolitan areas. Developing effective methods for providing basic health care and psychological support to this growing subgroup of mentally ill individuals is a challenge that Chinese cities are only now just starting to recognize and address, partly due to the renewed emphasis on mental health issues stimulated by China’s new national mental health law. This is the first study to consider the relevance of chronic medical illnesses in the indigent mentally ill in China. It describes the distribution of potentially modifiable cardiovascular risk factors among homeless patients with schizophrenia, a vulnerable population with low socioeconomic status and very limited resources. The coverage of prevention and intervention strategies for chronic physical illnesses in China should be expanded to include this difficult-to-reach population. Prospective studies with the growing number of homeless individuals will be needed to get a clearer picture of the best ways to provide them with the health care services they need.
Biography

Qing Chen obtained her Master’s degree from Hubei Medical College (now Wuhan University School of Medicine) in 1993. She is an attending psychiatrist at Jiading Mental Health Center where she has been working since 2007. She has been the head of the Department of Psychiatry since 2008. Her main research interest is clinical psychiatry and psychotherapy.
Footnotes
Conflict of Interest: The authors declare no conflict of interest.
References
- 1.National Cardiovascular Center. [China Cardiovascular Report 2011] 2012. Chinese. [Google Scholar]
- 2.Lee TC, Hanlon JG, Ben-David J, Booth GL, Cantor WJ, Connelly PW, et al. Risk factors for cardiovascular disease in homeless adults. Circulation. 2005;111(20):2629–2635. doi: 10.1161/CIRCULATIONAHA.104.510826. [DOI] [PubMed] [Google Scholar]
- 3.Hu DY. [Chinese expert consensus about the Integrated management of multiple cardiovascular risk factors in patients with diabetes] Xin Nao Xue Guan Bing Fang Zhi. 2012;4(12):261–266. doi: 10.3969/j.issn.1009-816X.2012.04.001. Chinese. [DOI] [Google Scholar]
- 4.Szerlip MI, Szerlip HM. Identification of Cardiovascular Risk Factors in Homeless Adults. Am J Med Sci. 2002;324:242–246. doi: 10.1097/00000441-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Ding WT, Guo H, Hu LR. [Case-control study of risk factors for homeless mental disorders] Zhongguo Yu Fang Yi Xue Za Zhi. 2009;3:179–182. Chinese. [Google Scholar]
- 6.Liu JB, Wu JH. [Effects of chlorpromazine, clozapine, risperidone on glucose metabolism in patients with first-episode schizophrenia, lipids and body weight] Zhongguo Shen Jing Jing Shen Ji Bing Za Zhi. 2004;30(4):294–295. doi: 10.3969/j.issn.1002-0152.2004.04.019. Chinese. [DOI] [Google Scholar]
- 7.Psychiatry Branch of Chinese Medical Association. Chinese Classification and Diagnostic Criteria of Mental Disorder, 3th ed. Jinan: Shandong Science and Technology Press; 2001. Chinese. [Google Scholar]
- 8.Chen ZY, Zhong NS. [Internal Medicine] People’s Health Publishing House; 2008. Chinese. [Google Scholar]
- 9.Chinese Medical Association Diabetes Society. [2007 version The Guideline of the Chinese Type 2 Diabetes Prevention, version 2007] Zhong Hua Nei Fen Mi Dai Xie Za Zhi. 2008;18 Chinese. [Google Scholar]
- 10.The joint committee of the guideline development of China adult dyslipidemia prevention. [The guideline of China adult dyslipidemia prevention] Zhong Hua Xin Xue Guan Bing Za Zhi. 2007;35(5):390–413. Chinese. [PubMed] [Google Scholar]
- 11.Chinese expert consensus panel of diagnosis and treatment of cardiovascular disease combined with asymptomatic hyperuricemia. [The diagnosis and treatment proposal of cardiovascular disease combined with asymptomatic hyperuricemia (2nd Edition)] Zhongguo Xin Xue Guan Bing Yan Jiu. 2012;10:2241–2249. [Google Scholar]
- 12.Luo H. [“three to five years away from poverty, but a disease back to the past”, China is facing a “prevention” crisis of hypertension - interview Professor Liu Lisheng, chairman of China Hypertension League] Zhongguo Yi Yao Zhi Nan. 2006;5:38–49. Chinese. [Google Scholar]
- 13.Bai J, Tang ZL, Li L, Gu LN, Xue D. [A systematic review: prevalence rate of hypertension in China] Shanghai Yu Fang Yi Xue. 2012;24(11):604–608. Chinese. [Google Scholar]
- 14.Zhang LJ, Hu DY, Yang JG, Xu YY, Li TC, Wang GH, et al. [Incidence and risk factors of hyperuricemia in the population with cardiovascular disease] Shou Du Yi Ke Da Xue Xue Bao. 2005;26(2):124–127. doi: 10.3969/j.issn.1006-7795.2005.02.007. Chinese. [DOI] [Google Scholar]
- 15.Zhang LJ, Hu DY, Yang JG, Xu YY, Li TC, Wang GH, et al. [Prevalence of hyperuricemia in patients with cardiovascular risk facotrs] Shou Du Yi Ke Da Xue Xue Bao. 2005;26(2):124–127. doi: 10.3969/j.issn.1006-7795.2005.02.007. Chinese. [DOI] [Google Scholar]
- 16.Jiang GR, Zheng H, Shao SW. [Research progress in hyperuricemia] Yi Xue Zong Shu. 2008;14(11):1673–1675. doi: 10.3969/j.issn.1006-2084.2008.11.027. Chinese. [DOI] [Google Scholar]
- 17.Yan HM, Gao X, Liu M, Gu Q, Zhang B, Li X. [Studies of the relationship between non-alcoholic fatty liver and metabolic syndrome] Zhongguo Tang Niao Bing Za Zhi. 2006;14(5):326–328. doi: 10.3321/j.issn:1006-6187.2006.05.003. Chinese. [DOI] [Google Scholar]
- 18.Ober K, Carlson L, Anderson Cardiovascular risk factors in homeless adults. J Cardiovasc Nurs. 1997;11(4):50–59. doi: 10.1097/00005082-199707000-00006. [DOI] [PubMed] [Google Scholar]


