Abstract
The incidence of difficult direct intubation in the intensive care unit (ICU) is estimated to be as high as 20%. Recent advances in video-technology have led to the development of video laryngoscopes as new intubation devices to assist in difficult airway management. Clinical studies indicate superiority of video laryngoscopes relative to conventional direct laryngoscopy in selected patients. They are therefore an important addition to the armamentarium of any clinician performing endotracheal intubation. We present a practical review of commonly available video laryngoscopes with respect to design, clinical efficacy, and safety aspects relevant to their use in the ICU.
Keywords: Difficult airway, intensive care unit, video laryngoscopes
Introduction
According to the American Society of Anesthesiologists, the incidence of difficult and failed intubation in the operating room is 1.2-3.8% and 0.13-0.30%, respectively[1,2] with estimates as high as 20% in the intensive care unit (ICU) or emergency department setting.[3,4,5,6,7] Video laryngoscopes are now increasingly available to assist with difficult airway management. It is important that the critical care clinician has a clear understanding of the specifications, user interfaces and geometry of individual video laryngoscopes and the efficacy and safety aspects of each of these devices. This review will concentrate on the commonly available video laryngoscopes focusing on design, efficacy, and safe use in the ICU setting.
Evaluation of Video Laryngoscopes
Studies of the efficacy of video laryngoscopes commonly describe the following outcomes: Glottic visualization (using the Cormack and Lehane classification), intubation success rate, number of attempts at intubation, need for intubation adjuncts and time to intubation. In this regard one major caution exists in extrapolating the Cormack and Lehane classification to the use of video laryngoscopes.[8] This classification is based on the premise that failed direct intubation most commonly results from failure to directly view the laryngeal inlet. However, while glottic visualization is still relevant to the use of video laryngoscopes, this may not always equate to successful intubation, as the insertion and advancement of the endotracheal tube (ETT) may fail despite clear video-assisted glottic visualization. The British Difficult Airway Society has provided advice about the assessment of and minimum level of evidence required to make decisions about the purchase of new video laryngoscopes. They recommend that any new device must have at least Level 3b evidence (at least one case control or historical control study) before it is considered for purchase and clinical use.[9,10]
Classification of Video Laryngoscopes
Video laryngoscopes can be broadly categorized as follows: (1) Standard blade style, (2) angulated blade style, and (3) anatomically shaped, channeled design.[11]
Standard blade style video laryngoscopes
These devices are based on a conventional standard MacIntosh or a Miller direct laryngoscope design with the addition of a camera that provides an image of the upper airway on a video-display. The advantage of the design is that these video laryngoscopes are inserted using the familiar technique. Although video laryngoscopy with Macintosh style blade is similar to standard laryngoscopy there is an important difference. The video blade can be inserted without sweeping the tongue that is, in the midline. This may be kinesthetically easier for learners as they do not have to control the tongue laterally. These devices also allow the operator the option of using them as direct laryngoscopes by simply ignoring the video-display. The video-display can also assist with teaching of direct laryngoscopy.[12]
Storz CMAC (Karl Storz GmbH and Co. KG, Tuttlingen, Germany)
Introduced to clinical practice in 2009, the Storz CMAC has three MacIntosh style blade options (sizes 2-4) and more recently a Miller style blade, that attach to either a large 7-inch stand mounted video-display or to a video screen mounted on the laryngoscope handle [Figures 1 and 2]. The reusable blades are only 14 mm thick and useful for patients with limited mouth opening. The aperture angle of 80° allows a wide field of view, which is enhanced by an integrated white balance and antifogging system. There is also the ability to record static images or 60-min of video onto a secure digital card, beneficial for quality assurance and teaching [Table 1].
Figure 1.

The Storz CMAC blade
Figure 2.
Storz CMAC video laryngoscope system: The video-display is mounted on a separate stand connected via a cable to the reusable laryngoscope componen
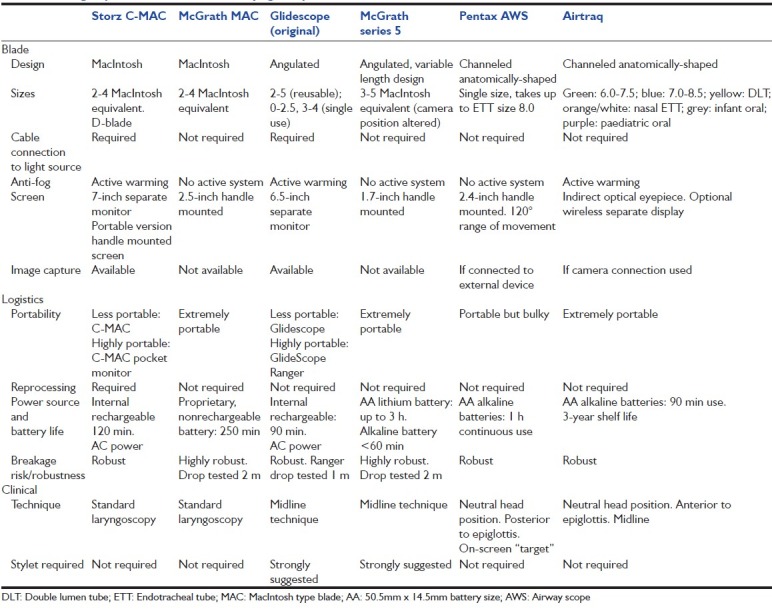
Table 1.
Design specifications of video laryngoscopes

Technique
The CMAC MacIntosh style blade is inserted into the mouth similar to a conventional laryngoscope. The epiglottis is visualized and the blade tip is inserted into the vallecula. With the laryngeal inlet ideally placed in the middle of the video-display, the handle can be lifted if required to improve the view. The MacIntosh blade design enables passage of the ETT without the routine need for stylets or a preformed ETT.
Troubleshooting
The large handle can result in difficult blade insertion in patients who are pregnant, obese, or have hyper-expanded chests. To overcome this, the blade should be inserted diagonally into the mouth with subsequent conventional positioning of the blade thereafter.[13] Inability to pass the ETT despite adequate view of the laryngeal inlet is uncommon (1 in 20 cases) compared to other video laryngoscope systems.[14] This can be overcome by the use of a bougie or a preformed stylet.
Efficacy
Compared with Pentax airway scope and the Glidescope®, the CMAC provided the easiest blade insertion and highest clarity of laryngeal view in patients without predictors of difficult intubation, however intubation may take longer and require more external laryngeal pressure.[15] For patients with predicted difficult airways, when compared with direct laryngoscopy, the CMAC was associated with a significant improvement of Cormack and Lehane grade 1 or 2 views, higher first attempt success rate, and reduced requirement for bougie assisted intubation.[16] Similar findings were reported in the ICU setting.[17]
McGrath MAC (Aircraft Medical, Edinburgh, UK)
Introduced to clinical practice in 2010, The McGrath MAC video laryngoscope has a fixed length metal alloy camera stick used with a plastic disposable blade that slides over it [Figure 3]. The MacIntosh style blades comes in three sizes (2, 3, and 4), with a maximum height of 11.9 mm, minimizing crowding of the mouth during use. The blade design incorporates “vertically aligned optics” that the manufacturers claim reduces the “blind spot” described later in this review. It has a 2.5-inch handle mounted screen, which articulates in one plane placing the display in line with the operator. The McGrath MAC is very portable and can be taken outside the ICU. There is no anti-fog system, but the device employs a hydrophilic optical surface coating to minimize condensation on the light source [Table 1].
Figure 3.

From left to right, The Original Glidescope® with its angulated blade to 60°, a Macintosh blade size 4, and the McGrath MAC video laryngoscope with a similar profile to the standard MacIntosh blade
Technique
The McGrath MAC is inserted into the mouth in the same way as a MacIntosh laryngoscope. When the tip of the blade is in the vallecula the image of the larynx should be positioned in the middle upper third of the video-display [Figure 4].
Figure 4.

McGrath MAC in use. The McGrath MAC is inserted into the mouth under direct vision in a manner similar to conventional direct laryngoscopy. The blade tip is placed in the vallecula with the laryngeal inlet lying centrally in the upper third of the display
Troubleshooting
If there is difficulty successfully directing the tube through the vocal cords, a bougie or external laryngeal manipulation may be helpful.
Efficacy
The McGrath MAC is relatively new has not been well-studied in the literature to date and there are currently no controlled data on its performance in difficult airways. Reports of efficacy have been restricted to successful case reports.[18]
Glidescope Direct
The Glidecope Direct has been developed and studied as an intubation trainer to facilitate instruction of direct laryngoscopy with a MacIntosh blade.[19,20] Key design features include a reusable MacIntosh blade design, built-in anti-fog mechanism, digital video technology, and real-time recording. This allows an instructor to observe and record the procedure on the video-display, confirm successful intubation and review direct laryngoscopy technique.
Video laryngoscopes with angulated blades
The key feature of these video laryngoscopes is that the blade is designed with a marked anterior curve in the sagittal plane - the “angulated blade”. This permits laryngeal visualization and intubation without the need for alignment of the oral-pharyngeal and laryngeal axes. Airway structures are only viewed “indirectly” through the video-display. This angulated design is advantageous in patients with an anterior larynx and makes these video laryngoscopes truly “difficult airway” devices. However, because of the sharp angulation, the ETT must be introduced “around the corner” requiring it to be preshaped using a variety of stylets.
Glidescope®(Verathon, Bothell, WA, USA)
First introduced into clinical use in 2001, the device has undergone numerous design modifications. There are three different monitor types in the Glidescope range - the original Glidescope® [Figure 3], the Glidescope Cobalt®, and the Glidescope Ranger®. These can be coupled with two blade shapes, the angulated blade and the recently released MacIntosh style Glidescope Direct®.
The angulated blade design incorporates a 60° anterior curvature in the midline, one-third of the distance from the blade tip. Reusable blades for use with the original Glidescope® are available in sizes 2, 3, 4, and 5, with a maximum height of 14.5 mm. The newer Glidescope Cobalt® comprises a video baton (available in two sizes) with disposable blades called “stats”. These “stats” range in size from 0 to 4 and are bulkier than the reusable blades with a maximum height of 16 mm at the mouth, comparing favorably to the height of a MacIntosh laryngoscope, which is approximately 25 mm thick. The “stats” are quick and easy to apply and as the video baton only requires low-level disinfection after patient use allowing rapid turnaround of the device. The Glidescope® camera is positioned approximately halfway along the length of the blade and incorporates an integrated anti-fog system. This proximal camera position allows a wide field of view but contributes to the “blind spot”. The Original Glidescope® and the Glidescope Cobalt® have a 6.5 inch stand mounted video-display somewhat limiting portability and ergonomics. The Glidescope Ranger® is a self-contained unit with increased portability and robustness suitable for use in the field. It incorporates a 3.4-inch antireflective screen, designed for outdoor use in daylight conditions. Similar to the Storz CMAC, the device has storage capacity of 60-min of video [Table 1].
Technique
The ETT should be performed to 60° using a stylet so that it resembles the shape of the blade [Figure 5]. The Gliderite® rigid steel stylet may be used for a size 6 or larger ETT or a standard malleable stylet is an appropriate alternative. Following a “look-up, look-down” sequence described later in this review, the Glidescope® blade is inserted in the midline over the tongue (without sweeping the tongue to the side) into the vallecula. An optimized view places the laryngeal inlet in the midline of the upper third of the screen [Figure 6]. It is important to avoid excessive depth of insertion of the blade as this result in a narrow field of view and increases the angle that the ETT must follow for successful intubation.
Figure 5.

The Glidescope with a preformed endotracheal tube using a stylet. Note that the ETT is preformed to match the angulated profile of the Glidescope blade®
Figure 6.

The Glidescope in use. The Glidescope blade has been inserted into the mouth in the midline under direct vision. The blade tip is placed in the vallecula and an optimized view places the laryngeal inlet lying centrally in the upper third of the display
Troubleshooting
Tube delivery to the glottis is the most difficult part of Glidescope® use due to the acute angle of the path of the ETT to the glottis. This can be overcome by correctly preforming the ETT with a stylet, and passing the tube close to the blade when inserted. Improved intubation success rate may be possible with increased tube angulation to 90°, preformed 8 cm proximal to the tube tip.[21] If the tube still passes posterior to the glottis then laryngeal manipulation, gum elastic bougie, or unidirectional stylet (Flexit stylet) may be helpful. If a Gliderite stylet® is being used the stylet can be partially withdrawn, which directs the tube tip anteriorly. “Reverse loading” when using a stylet may be helpful if the tube contacts the tracheal rings at an angle, which restricts tube passage. This involves loading the ETT with “reverse camber.” This is where the tube is rotated 180° from its usual orientation on the stylet. When this is done the radio-opaque stripe is on the concave side of the tube rather than the convex side where it usually resides. Loading the tube with reverse camber allows it to pass into the larynx more easily.[22] In patients with small mouths, ETT passage may be assisted by inserting the Glidescope® to the left of the midline or by inserting the ETT into the mouth before the Glidescope®.[23,24,25] This must be performed under direct vision to avoid inadvertent injury to oropharyngeal structures.[26]
Efficacy
In a review of over 6600 patients, Mihai et al. they found that there was no consistent advantage of the Glidescope® with regard to first attempt success at intubation when used in unselected patients.[27] However, in a subset of over 1000 patients with predicted difficult airways, first attempt intubation success was better. A recent meta-analysis comparing Glidescope® video laryngoscopy to direct laryngoscopy found that the Glidescope® was associated with an improved glottic view, particularly amongst patients with predicted or simulated difficult airways.[28] However, only in inexperienced operators was first attempt success at intubation and reduced time to intubation significantly improved. The authors suggested the Glidescope® was useful in patients with clinical features of difficult direct laryngoscopy, as a rescue method after failed direct intubation, and for use by non-expert providers. In contrast, in a study by Cooper et al.,[29] the Glidescope® resulted in satisfactory views in 99% of patients. Failed intubation occurred in 3.7% of patients, half of which occurred despite adequate view of the glottis. This cautions the interpretation of studies that use improved laryngeal view as major indicators to validate the technique.
In the ICU setting no difference was observed in either the number of attempts at intubation or complications of intubation after the introduction of the Glidescope®.[30] In contrast, Kory et al. performed a single center study of the Glidescope® versus a historical cohort of conventional intubations in ICU. The use of the Glidescope® was associated with increased first attempt success and less esophageal intubation.[31]
There is a definite learning curve using the Glidescope® for both experienced and novice clinicians. In operators with no experience at intubation, intubation success with the Glidescope® progressively improved to over 80% with just three uses, compared with a peak success rate of 33% for direct laryngoscopy.[32] When performed by experienced anesthetists in a simulated difficult airway scenario there was also a reduced time to successful intubation. Anesthetists with no previous Glidescope® experience took on average 85 s for successful intubation, while those with >10 previous uses of the Glidescope® took 31 s.[33]
McGrath Series 5 (Aircraft Medical, Edinburgh, UK)
Introduced to clinical practice in 2008, the McGrath series 5 consists of three basic components: Handle, camera stick, and single use angulated blade [Figure 7].[34] Blades are available in sizes equivalent to McIntosh sizes 3, 4, and 5. The length of the camera stick and docked blade can be further adjusted by disarticulating the camera and inserting it inside the blade to three different positions. The maximum height of the blade is 13 mm. The 1.7-inch video-display is handle mounted and can be rotated through 90° in both the horizontal and vertical planes, allowing the operator to simultaneously focus on the video-display and the patient. There is no anti-fog system, and the manufacturer recommends separate application of anti-fog solution prior to use, which may be disadvantageous when used in an emergency situation. The device lacks the ability to record or store images [Table 1].
Figure 7.

The McGrath series 5 video laryngoscope with its handle mounted display and angulated blade design. The position of the disposable blade can be placed on the camera stick in three different positions (photo courtesy of Aircraft Medical Limited)
Technique
The ETT is prepared as for the Glidescope® with a stylet angled to 60° to match the curvature of the blade. The device should be inserted in the midline over the tongue and the blade placed in the vallecula. In the event of the epiglottis obstructing the view, the blade tip can be passed posterior to the epiglottis.
Troubleshooting
Due to the angulated blade design of the McGrath series 5 and the Glidescope® similar problems are encountered. The approach to these is previously described for the Glidescope® above.
Efficacy
There are no reports of clinical studies of the McGrath in ICU patients. In operating room, the device has been shown to provide superior laryngeal views compared with direct laryngoscopy in unselected patients, patients with predicted difficult airways and in failed direct intubation.[35,36] The McGrath is an easily learned technique with novice users demonstrating proficiency after six uses in a manikin study.[37]
Storz CMAC D-Blade
Recently a D-blade has been developed for use with the Storz CMAC system described above. This blade has an angulated design similar to the Glidescope® and can be used as an indirect laryngoscope only. Similar to the use of other angulated blades, a stylet is recommended.
Video laryngoscopes with a tube channel
This style of video laryngoscope is anatomically shaped and has a tube guide channel to direct the ETT to the glottis. The main advantage of incorporating a tube channel is control of ETT advancement, which may reduce intubation time with respect to unchanneled devices.[15,38]
Pentax airway scope 100 (Pentax AWS 100, Pentax Corporation, Tokyo, Japan)
The Pentax video laryngoscope incorporates an anatomically shaped, transparent, disposable, polycarbonate blade (called a P-blade) that slips easily over a flexible fiberoptic cable [Figure 8]. The P-blade comes in only one size, which accommodates ETT's up to size 8. The P-blade consists of three parallel channels. The left channel houses the fiberoptic cable that transmits the camera picture from 3 cm proximal to the tip of the blade. The right channel is for the tube and the third midline channel can be used for oxygen insufflation or application of suction. The handle mounted 2.4-inch liquid-crystal display screen can be angled to suit the operator and incorporates a “cross hair” to indicate the predicted trajectory of the ETT. The Pentax AWS is slightly bulkier than other video laryngoscopes being 18 mm at its maximum height, necessitating adequate patient mouth opening for this device to be useful. There is no anti-fog mechanism; however, to reduce the risk of fogging the blade can be placed in warm water before use[39] [Table 1].
Figure 8.
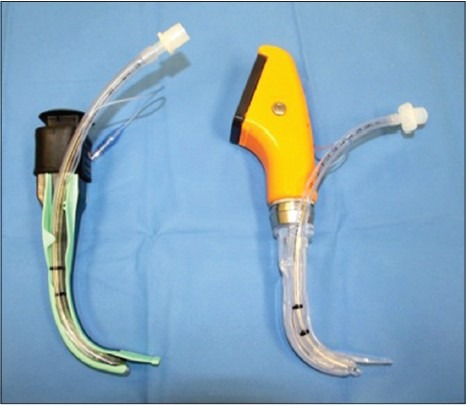
Airtraq optical laryngoscope on the left and the Pentax airway scope on the right with their channeled design. The endotracheal tube is loaded into a tube guide in a position in which the tip will not obstruct the optical view
Technique
To prepare the Pentax, the P-blade is attached and the ETT lubricated and loaded into the tube channel on the side of the blade. The tube should be positioned so its tip lies out of view of the camera. The blade is inserted into the mouth in the midline and advanced over the tongue and along the palatal wall until the epiglottis is visualized. The blade is then passed posterior to the epiglottis directly elevating it out of the way (the Miller or “straight blade” approach) to visualize the glottis. The target symbol on the video-display should be aligned with the glottis and the tube advanced through the vocal cords before being detached from the blade laterally [Figure 9].
Figure 9.
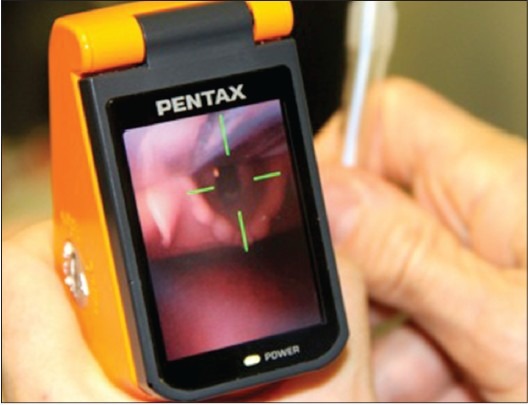
Pentax airway scope in use. The blade has been inserted in the midline in the oral cavity and the blade tip positioned posterior to the epiglottis (so-called straight blade approach). An optimized view shows the “cross hair” placed on the laryngeal inlet to facilitate accurate endotracheal tube placement
Troubleshooting
Due to the bulky dimensions, there may be some difficulty inserting the Pentax into the mouth due to close proximity of the chest. In this situation, the blade can be inserted into the mouth first and then subsequently attached to the handle. Alternatively, the device can be inserted like a Guedel airway upside down and then rotated 180° in the mouth.[40] Inability to successfully pass the ETT may also occur despite view of the glottis and a bougie may first be passed through the loaded ETT into the larynx before railroading the tube. This is particularly useful if the blade length is not sufficient to pass posterior to the epiglottis, which can obstruct the path of the tube.[39] If the target symbol cannot be successfully aligned, laryngeal manipulation may be effective. Alternatively, the tube could be deployed into the hypopharynx before partially inflating the cuff to move it anteriorly to the glottic opening. The cuff is then deflated and the tube advanced into the trachea with reinflation of the cuff once the tube is in a satisfactory position.[41]
Efficacy
The Pentax has not been subjected to clinical studies in ICU patients however in the operating room has consistently shown to improve the laryngeal views and successful intubation in simulated and difficult airways situations.[42,43,44] Time to intubation is comparable to direct laryngoscopy if operators are familiar with the device.[36,39] There is also evidence that the pressor response to intubation is reduced with the Pentax compared to when using a conventional laryngoscope.[45] The Pentax can also be used with the head in a neutral position. In patients requiring cervical spine immobilization, use of the Pentax AWS has been consistently shown to improve laryngeal view, time to intubation, and improve intubation success rate.[46,47] Radiological studies in patients without manual in-line stabilization indicate that there is less movement of the cervical spine to obtain optimal laryngeal view with the Pentax relative to direct laryngoscopy.[48] Until date, there have been no studies with regard to learning curve or rate of improvement of operator skill with this device.
Airtraq Optical laryngoscope (Prodol Meditec S.A., Vizcaya, Spain)
Airtraq is a single use, disposable indirect optical laryngoscope [Figure 8]. The blade has two parallel channels. The optical channel comprises a series of lenses, prisms, and mirrors, which produces a magnified image of the airway to the eyepiece. In addition, this can be connected to an external video-display. The image is derived from close to the tip of the blade. The other channel allows preloading of the ETT. The device contains a low temperature battery powered light source with an inbuilt anti-fog system.[49,50]
The Airtraq is available in seven different color coded variations including two adult sizes for oral intubation. A green “small adult” size accommodates a size 6.0-7.5 ETT and requires 16 mm of mouth opening. A blue “regular-adult” size Airtraq accommodates sizes 7.0-8.5 mm ETT and requires 18 mm of mouth opening. The yellow Airtraq is for use with a size 35-41 Fr double lumen tube and therefore has a wider tube channel. In addition, two Airtraqs color coded orange and white are designed specifically for nasotracheal intubation and lack a tube guide.[51] The more recent Airtraq Avant comprises an optical baton that can be reused up to 50 times with a disposable blade and eyepiece. The blades come in only two sizes, a small and a regular, allowing 6.0-7.5 mm and 7.0-8.5 mm ETTs, respectively [Table 1].
Technique
When turned on it takes 30-60 s for the anti-fog system to become effective; the light stops flashing once this has occurred. The anterior blade and ETT should be lubricated before loading the tube in the tube channel. Care should be taken not to position the tube tip too distally on the blade as this may obstruct the view. Maintaining the patients head in a neutral position can facilitate insertion. The blade is inserted into the mouth in the midline over the tongue. The blade is then advanced over the contour of the tongue. Once the device has passed over the base of the tongue the operator should view the tip through the eyepiece. The manufacturers recommend the tip of the Airtraq should be placed in the vallecula (MacIntosh technique). However, a technique whereby the blade is passed posterior to the epiglottis has also been described.[51] To optimize the view the device should be lifted vertically and the laryngeal inlet should be centered with a side-to-side rotation of the device.[52] To achieve successful passage of the tube, it is important that the lower border of the glottis lies below the midline of the view due to the expected initial downward trajectory of the tube when it exits the tube guide. The tube is then advanced, the cuff inflated and test ventilation should be undertaken with the Airtraq in situ. To complete the process the Airtraq is disengaged from the ETT with a lateral movement.
Troubleshooting
As described for the Pentax, the Airtraq can also be inserted into the mouth similar to a Guedel airway before rotating it through 180°.[53] Inability to obtain any laryngeal view may be due to the device being inserted too far, which can be rectified by gentle withdrawal. The “triple maneuver (downward, back and up)” aims to optimize laryngeal position.[54] If tube passage is difficult despite an adequate view, a bougie can be passed through the preloaded tube as described for the Pentax AWS.[44] A similar technique involving a fiberoptic scope via the preloaded ETT has also been described.[54]
Efficacy
There is no evidence of superiority of the Airtraq over direct laryngoscopy in unselected patients when performed by experienced operators.[55] However, in patients with predicted or known difficult airways, the device has been shown to improve success rate and shorten time to intubation.[56,57] Studies have also demonstrated the efficacy of the Airtraq in patients requiring cervical spine immobilization, improving both laryngeal views and time to intubation.[58,59] Case reports have also described its use in awake intubations.[60] The learning curve for the device for airway novices has also been shown to be short when compared with direct laryngoscopy.[61,62]
Safety Aspects Relevant to Use of All Video Laryngoscopes
There have been numerous case reports of injuries to the upper airway associated with use of video laryngoscopes. This largely results from the operator looking solely at the video screen and blindly advancing the ETT through soft tissues of the mouth. Use of a stylet may contribute. Injuries and perforations of the soft palate, palatopharyngeal folds and tonsillars pillars have been reported.[51,63,64,65,66] The risk of trauma has also been attributed to a video laryngoscope “blind spot”. This refers to the inability to see the tip of the ETT in the hypopharynx after direct vision is lost and before the tip can be viewed indirectly through the video-display.[42,65]
Trauma can largely be avoided by following a sequential “look-up, look-down” approach. The video laryngoscope should be is inserted into the mouth under direct vision (look-down). Next, the larynx is visualized by looking up at the video-display. When the ETT is inserted into the mouth, this is again done under direct vision by looking down, before the operator's attention is finally drawn to the video-display to direct the ETT through the vocal cords. By directly observing the video laryngoscope and the ETT entering into the mouth, there is a potentially reduced risk of airway trauma.
Role of Video Laryngoscopes in Intensive Care Unit
The clinical role of video laryngoscopes in the ICU is still being defined. Benefits in unselected patients for routine airway management are unproven. For uncomplicated airways, video laryngoscopes are not superior to direct laryngoscopy. Furthermore, intubation using a video laryngoscope tends to be slower, possibly attributed to lack of experience, difficulty with tube advancement, and the division of the operator's attention between two domains.[67,68,69] This is of particular significance in ICU patients with marginal respiratory physiology and where intubation is particularly time critical. The most recent recommendations from the American Society of Anesthesiologists strongly endorse the use of video laryngoscopy in the event of intubation difficulty.[70] However, these devices are not considered in the older British Difficult Airway Society guidelines.[71] Importantly, video laryngoscopy should not be considered as an alternative substitute to the gold standard of an awake fiberoptic intubation in patients with known or predicted difficult airways. Video laryngoscopes may be used to facilitate the awake intubation itself and have been used for this purpose.[72,73,74]
The use of video laryngoscopes for ICU patients requiring tube exchange has recently been described.[75] Video laryngoscope were used in conjunction with an airway exchange catheter if “no view” of the glottis was evident with conventional direct laryngoscopy.[75] Use of the video laryngoscope in this situation improved glottic visualization in the majority of cases. This study may suggest an increased margin of safety for high-risk patients undergoing tube exchange.[75] Finally, video laryngoscopes have been used to aid the insertion of percutaneous tracheostomies in the ICU.[73] The main advantage appears to be in maintaining video imaging of the withdrawn ETT at the juxta-glottic position, minimizing the risk of tube dislodgment and avoiding inadvertent cuff perforation. Use of the Glidescope for this purpose is reported to interfere with the procedure less than a standard laryngoscope, due to the handle design not impinging on the tracheostomy field.[76]
Conclusion
Video laryngoscopes provide an alternative method to direct endotracheal intubation. There is no current evidence of superiority of these devices in unselected patients or proven benefit in ICU patients. However, video laryngoscopes have an important role in the ICU as an aid to teaching endotracheal intubation to trainees. The video-display allows demonstration and real-time supervision of the procedure. Given the increasing evidence of efficacy in difficult airway management in the operating room, they are an important addition to the armamentarium of critical care clinicians involved in advanced airway management.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Crosby ET, Cooper RM, Douglas MJ, Doyle DJ, Hung OR, Labrecque P, et al. The unanticipated difficult airway with recommendations for management. Can J Anaesth. 1998;45:757–76. doi: 10.1007/BF03012147. [DOI] [PubMed] [Google Scholar]
- 2.Benumof JL. Management of the difficult adult airway. With special emphasis on awake tracheal intubation. Anesthesiology. 1991;75:1087–110. doi: 10.1097/00000542-199112000-00021. [DOI] [PubMed] [Google Scholar]
- 3.Tayal VS, Riggs RW, Marx JA, Tomaszewski CA, Schneider RE. Rapid-sequence intubation at an emergency medicine residency: Success rate and adverse events during a two-year period. Acad Emerg Med. 1999;6:31–7. doi: 10.1111/j.1553-2712.1999.tb00091.x. [DOI] [PubMed] [Google Scholar]
- 4.Sakles JC, Laurin EG, Rantapaa AA, Panacek EA. Airway management in the emergency department: A one-year study of 610 tracheal intubations. Ann Emerg Med. 1998;31:325–32. doi: 10.1016/s0196-0644(98)70342-7. [DOI] [PubMed] [Google Scholar]
- 5.Heuer JF, Barwing TA, Barwing J, Russo SG, Bleckmann E, Quintel M, et al. Incidence of difficult intubation in intensive care patients: Analysis of contributing factors. Anaesth Intensive Care. 2012;40:120–7. doi: 10.1177/0310057X1204000113. [DOI] [PubMed] [Google Scholar]
- 6.Jaber S, Amraoui J, Lefrant JY, Arich C, Cohendy R, Landreau L, et al. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: A prospective, multiple-center study. Crit Care Med. 2006;34:2355–61. doi: 10.1097/01.CCM.0000233879.58720.87. [DOI] [PubMed] [Google Scholar]
- 7.Griesdale DE, Bosma TL, Kurth T, Isac G, Chittock DR. Complications of endotracheal intubation in the critically ill. Intensive Care Med. 2008;34:1835–42. doi: 10.1007/s00134-008-1205-6. [DOI] [PubMed] [Google Scholar]
- 8.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–11. [PubMed] [Google Scholar]
- 9.Pandit JJ, Popat MT, Cook TM, Wilkes AR, Groom P, Cooke H, et al. The Difficult Airway Society ‘ADEPT’ guidance on selecting airway devices: The basis of a strategy for equipment evaluation. Anaesthesia. 2011;66:726–37. doi: 10.1111/j.1365-2044.2011.06787.x. [DOI] [PubMed] [Google Scholar]
- 10.Laffey JG. Strengthening the evidence base for airway equipment: Time to be more ‘ADEPT’. Anaesthesia. 2011;66:656–8. doi: 10.1111/j.1365-2044.2011.06824.x. [DOI] [PubMed] [Google Scholar]
- 11.Behringer EC, Kristensen MS. Evidence for benefit vs novelty in new intubation equipment. Anaesthesia. 2011;66(Suppl 2):57–64. doi: 10.1111/j.1365-2044.2011.06935.x. [DOI] [PubMed] [Google Scholar]
- 12.Howard-Quijano KJ, Huang YM, Matevosian R, Kaplan MB, Steadman RH. Video-assisted instruction improves the success rate for tracheal intubation by novices. Br J Anaesth. 2008;101:568–72. doi: 10.1093/bja/aen211. [DOI] [PubMed] [Google Scholar]
- 13.Kaplan MB, Hagberg CA, Ward DS, Brambrink A, Chhibber AK, Heidegger T, et al. Comparison of direct and video-assisted views of the larynx during routine intubation. J Clin Anesth. 2006;18:357–62. doi: 10.1016/j.jclinane.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 14.van Zundert A, Maassen R, Lee R, Willems R, Timmerman M, Siemonsma M, et al. A Macintosh laryngoscope blade for videolaryngoscopy reduces stylet use in patients with normal airways. Anesth Analg. 2009;109:825–31. doi: 10.1213/ane.0b013e3181ae39db. [DOI] [PubMed] [Google Scholar]
- 15.Teoh WH, Saxena S, Shah MK, Sia AT. Comparison of three videolaryngoscopes: Pentax Airway Scope, C-MAC, Glidescope vs the Macintosh laryngoscope for tracheal intubation. Anaesthesia. 2010;65:1126–32. doi: 10.1111/j.1365-2044.2010.06513.x. [DOI] [PubMed] [Google Scholar]
- 16.Aziz MF, Dillman D, Fu R, Brambrink AM. Comparative effectiveness of the C-MAC video laryngoscope versus direct laryngoscopy in the setting of the predicted difficult airway. Anesthesiology. 2012;116:629–36. doi: 10.1097/ALN.0b013e318246ea34. [DOI] [PubMed] [Google Scholar]
- 17.Noppens RR, Geimer S, Eisel N, David M, Piepho T. Endotracheal intubation using the C-MAC ® video laryngoscope or the Macintosh laryngoscope: A prospective, comparative study in the ICU. Crit Care. 2012;16:R103. doi: 10.1186/cc11384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hyuga S, Sekiguchi T, Ishida T, Yamamoto K, Sugiyama Y, Kawamata M. Successful tracheal intubation with the McGrath(®) MAC video laryngoscope after failure with the Pentax-AWS™ in a patient with cervical spine immobilization. Can J Anaesth. 2012;59:1154–5. doi: 10.1007/s12630-012-9790-9. [DOI] [PubMed] [Google Scholar]
- 19.Healy DW. The GlideScope Direct: Its use as a videolaryngoscopic intubation trainer. J Clin Anesth. 2012;24:433. doi: 10.1016/j.jclinane.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 20.Viernes D, Goldman AJ, Galgon RE, Joffe AM. Evaluation of the GlideScope direct: A new video laryngoscope for teaching direct laryngoscopy. Anesthesiol Res Pract. 2012;2012:820961. doi: 10.1155/2012/820961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dupanović M, Isaacson SA, Borovcanin Z, Jain S, Korten S, Karan S, et al. Clinical comparison of two stylet angles for orotracheal intubation with the GlideScope video laryngoscope. J Clin Anesth. 2010;22:352–9. doi: 10.1016/j.jclinane.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 22.Dow WA, Parsons DG. ‘Reverse loading’ to facilitate Glidescope intubation. Can J Anaesth. 2007;54:161–2. doi: 10.1007/BF03022022. [DOI] [PubMed] [Google Scholar]
- 23.Doyle DJ, Zura A, Ramachandran M. Videolaryngoscopy in the management of the difficult airway. Can J Anaesth. 2004;51:95. [PubMed] [Google Scholar]
- 24.Cooper RM. Videolaryngoscopes in the management of the difficult airway: Reply. Can J Anaesth. 2004;51:95–6. [Google Scholar]
- 25.Jones PM, Turkstra TP, Armstrong KP, Armstrong PM, Cherry RA, Hoogstra J, et al. Effect of stylet angulation and endotracheal tube camber on time to intubation with the GlideScope. Can J Anaesth. 2007;54:21–7. doi: 10.1007/BF03021895. [DOI] [PubMed] [Google Scholar]
- 26.Cooper RM. Complications associated with the use of the GlideScope videolaryngoscope. Can J Anaesth. 2007;54:54–7. doi: 10.1007/BF03021900. [DOI] [PubMed] [Google Scholar]
- 27.Mihai R, Blair E, Kay H, Cook TM. A quantitative review and meta-analysis of performance of non-standard laryngoscopes and rigid fibreoptic intubation aids. Anaesthesia. 2008;63:745–60. doi: 10.1111/j.1365-2044.2008.05489.x. [DOI] [PubMed] [Google Scholar]
- 28.Griesdale DE, Liu D, McKinney J, Choi PT. Glidescope ® video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: A systematic review and meta-analysis. Can J Anaesth. 2012;59:41–52. doi: 10.1007/s12630-011-9620-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cooper RM, Pacey JA, Bishop MJ, McCluskey SA. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. 2005;52:191–8. doi: 10.1007/BF03027728. [DOI] [PubMed] [Google Scholar]
- 30.Ural K, Subaiya C, Taylor C, Ramadhyani U, Scuderi-Porter H, Nossaman BD. Analysis of orotracheal intubation techniques in the intensive care unit. Crit Care Resusc. 2011;13:89–96. [PubMed] [Google Scholar]
- 31.Kory P, Guevarra K, Mathew JP, Hegde A, Mayo PH. The impact of video laryngoscopy use during urgent endotracheal intubation in the critically ill. Anesth Analg. 2013;117:144–9. doi: 10.1213/ANE.0b013e3182917f2a. [DOI] [PubMed] [Google Scholar]
- 32.Ayoub CM, Kanazi GE, Al Alami A, Rameh C, El-Khatib MF. Tracheal intubation following training with the GlideScope compared to direct laryngoscopy. Anaesthesia. 2010;65:674–8. doi: 10.1111/j.1365-2044.2010.06335.x. [DOI] [PubMed] [Google Scholar]
- 33.Lim Y, Yeo SW. A comparison of the GlideScope with the Macintosh laryngoscope for tracheal intubation in patients with simulated difficult airway. Anaesth Intensive Care. 2005;33:243–7. doi: 10.1177/0310057X0503300215. [DOI] [PubMed] [Google Scholar]
- 34.Shippey B, Ray D, McKeown D. Case series: The McGrath videolaryngoscope - an initial clinical evaluation. Can J Anaesth. 2007;54:307–13. doi: 10.1007/BF03022777. [DOI] [PubMed] [Google Scholar]
- 35.Shippey B, Ray D, McKeown D. Use of the McGrath videolaryngoscope in the management of difficult and failed tracheal intubation. Br J Anaesth. 2008;100:116–9. doi: 10.1093/bja/aem303. [DOI] [PubMed] [Google Scholar]
- 36.O'Leary AM, Sandison MR, Myneni N, Cirilla DJ, Roberts KW, Deane GD. Preliminary evaluation of a novel videolaryngoscope, the McGrath series 5, in the management of difficult and challenging endotracheal intubation. J Clin Anesth. 2008;20:320–1. doi: 10.1016/j.jclinane.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 37.Ray DC, Billington C, Kearns PK, Kirkbride R, Mackintosh K, Reeve CS, et al. A comparison of McGrath and Macintosh laryngoscopes in novice users: A manikin study. Anaesthesia. 2009;64:1207–10. doi: 10.1111/j.1365-2044.2009.06061.x. [DOI] [PubMed] [Google Scholar]
- 38.Liu EH, Goy RW, Tan BH, Asai T. Tracheal intubation with videolaryngoscopes in patients with cervical spine immobilization: A randomized trial of the Airway Scope and the GlideScope. Br J Anaesth. 2009;103:446–51. doi: 10.1093/bja/aep164. [DOI] [PubMed] [Google Scholar]
- 39.Asai T, Liu EH, Matsumoto S, Hirabayashi Y, Seo N, Suzuki A, et al. Use of the Pentax-AWS in 293 patients with difficult airways. Anesthesiology. 2009;110:898–904. doi: 10.1097/ALN.0b013e31819c45e5. [DOI] [PubMed] [Google Scholar]
- 40.Suzuki A, Terao M, Fujita S, Henderson JJ. Tips for intubation with the Pentax-AWS rigid indirect laryngoscope in morbidly obese patients. Anaesthesia. 2008;63:442–4. doi: 10.1111/j.1365-2044.2008.05509.x. [DOI] [PubMed] [Google Scholar]
- 41.Xue FS, Liu JH, Liao X, Yuan YJ. Use of cuff inflation to facilitate nasotracheal intubation with the Airway Scope. Anaesthesia. 2011;66:754. doi: 10.1111/j.1365-2044.2011.06807.x. [DOI] [PubMed] [Google Scholar]
- 42.Malik MA, Subramaniam R, Maharaj CH, Harte BH, Laffey JG. Randomized controlled trial of the Pentax AWS, Glidescope, and Macintosh laryngoscopes in predicted difficult intubation. Br J Anaesth. 2009;103:761–8. doi: 10.1093/bja/aep266. [DOI] [PubMed] [Google Scholar]
- 43.Tan BH, Liu EH, Lim RT, Liow LM, Goy RW. Ease of intubation with the GlideScope or Airway Scope by novice operators in simulated easy and difficult airways - a manikin study. Anaesthesia. 2009;64:187–90. doi: 10.1111/j.1365-2044.2008.05753.x. [DOI] [PubMed] [Google Scholar]
- 44.Suzuki A, Toyama Y, Katsumi N, Kunisawa T, Sasaki R, Hirota K, et al. The Pentax-AWS((R)) rigid indirect video laryngoscope: Clinical assessment of performance in 320 cases. Anaesthesia. 2008;63:641–7. doi: 10.1111/j.1365-2044.2008.05452.x. [DOI] [PubMed] [Google Scholar]
- 45.Nishikawa K, Matsuoka H, Saito S. Tracheal intubation with the PENTAX-AWS (airway scope) reduces changes of hemodynamic responses and bispectral index scores compared with the Macintosh laryngoscope. J Neurosurg Anesthesiol. 2009;21:292–6. doi: 10.1097/ANA.0b013e3181a9c6dc. [DOI] [PubMed] [Google Scholar]
- 46.Hirabayashi Y, Fujita A, Seo N, Sugimoto H. Cervical spine movement during laryngoscopy using the Airway Scope compared with the Macintosh laryngoscope. Anaesthesia. 2007;62:1050–5. doi: 10.1111/j.1365-2044.2007.05188.x. [DOI] [PubMed] [Google Scholar]
- 47.Maruyama K, Yamada T, Kawakami R, Kamata T, Yokochi M, Hara K. Upper cervical spine movement during intubation: Fluoroscopic comparison of the AirWay Scope, McCoy laryngoscope, and Macintosh laryngoscope. Br J Anaesth. 2008;100:120–4. doi: 10.1093/bja/aem313. [DOI] [PubMed] [Google Scholar]
- 48.Maruyama K, Yamada T, Kawakami R, Hara K. Randomized cross-over comparison of cervical-spine motion with the AirWay Scope or Macintosh laryngoscope with in-line stabilization: A video-fluoroscopic study. Br J Anaesth. 2008;101:563–7. doi: 10.1093/bja/aen207. [DOI] [PubMed] [Google Scholar]
- 49.Maharaj CH, Higgins BD, Harte BH, Laffey JG. Evaluation of intubation using the Airtraq or Macintosh laryngoscope by anaesthetists in easy and simulated difficult laryngoscopy - A manikin study. Anaesthesia. 2006;61:469–77. doi: 10.1111/j.1365-2044.2006.04547.x. [DOI] [PubMed] [Google Scholar]
- 50.Ford PN, Hamer C, Medakkar S. Use of the Airtraq in the difficult airway. Eur J Anaesthesiol. 2007;24:730–1. doi: 10.1017/s0265021507000233. [DOI] [PubMed] [Google Scholar]
- 51.Cooper RM, Law JA. Management of the Difficult and Failed Airway. 2nd ed. New York: McGraw Hill; 2012. Rigid and semirigid fibreoptic and videolaryngoscopy and intubation. [Google Scholar]
- 52.Dhonneur G, Abdi W, Amathieu R, Ndoko S, Tual L. Optimising tracheal intubation success rate using the Airtraq laryngoscope. Anaesthesia. 2009;64:315–9. doi: 10.1111/j.1365-2044.2008.05757.x. [DOI] [PubMed] [Google Scholar]
- 53.Dhonneur G, Ndoko SK, Amathieu R, Attias A, Housseini LE, Polliand C, et al. A comparison of two techniques for inserting the Airtraq laryngoscope in morbidly obese patients. Anaesthesia. 2007;62:774–7. doi: 10.1111/j.1365-2044.2007.05128.x. [DOI] [PubMed] [Google Scholar]
- 54.Malin E, Montblanc Jd, Ynineb Y, Marret E, Bonnet F. Performance of the Airtraq laryngoscope after failed conventional tracheal intubation: A case series. Acta Anaesthesiol Scand. 2009;53:858–63. doi: 10.1111/j.1399-6576.2009.02011.x. [DOI] [PubMed] [Google Scholar]
- 55.Maharaj CH, O’Croinin D, Curley G, Harte BH, Laffey JG. A comparison of tracheal intubation using the Airtraq or the Macintosh laryngoscope in routine airway management: A randomised, controlled clinical trial. Anaesthesia. 2006;61:1093–9. doi: 10.1111/j.1365-2044.2006.04819.x. [DOI] [PubMed] [Google Scholar]
- 56.Healy DW, Maties O, Hovord D, Kheterpal S. A systematic review of the role of videolaryngoscopy in successful orotracheal intubation. BMC Anesthesiol. 2012;12:32. doi: 10.1186/1471-2253-12-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ndoko SK, Amathieu R, Tual L, Polliand C, Kamoun W, El Housseini L, et al. Tracheal intubation of morbidly obese patients: A randomized trial comparing performance of Macintosh and Airtraq laryngoscopes. Br J Anaesth. 2008;100:263–8. doi: 10.1093/bja/aem346. [DOI] [PubMed] [Google Scholar]
- 58.Maharaj CH, Buckley E, Harte BH, Laffey JG. Endotracheal intubation in patients with cervical spine immobilization: A comparison of macintosh and airtraq laryngoscopes. Anesthesiology. 2007;107:53–9. doi: 10.1097/01.anes.0000267529.71756.f0. [DOI] [PubMed] [Google Scholar]
- 59.Durga P, Kaur J, Ahmed SY, Kaniti G, Ramachandran G. Comparison of tracheal intubation using the Airtraq(®) and Mc Coy laryngoscope in the presence of rigid cervical collar simulating cervical immobilisation for traumatic cervical spine injury. Indian J Anaesth. 2012;56:529–34. doi: 10.4103/0019-5049.104568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dimitriou VK, Zogogiannis ID, Liotiri DG. Awake tracheal intubation using the Airtraq laryngoscope: A case series. Acta Anaesthesiol Scand. 2009;53:964–7. doi: 10.1111/j.1399-6576.2009.02012.x. [DOI] [PubMed] [Google Scholar]
- 61.Di Marco P, Scattoni L, Spinoglio A, Luzi M, Canneti A, Pietropaoli P, et al. Learning curves of the Airtraq and the Macintosh laryngoscopes for tracheal intubation by novice laryngoscopists: A clinical study. Anesth Analg. 2011;112:122–5. doi: 10.1213/ANE.0b013e3182005ef0. [DOI] [PubMed] [Google Scholar]
- 62.Hirabayashi Y, Seo N. Airtraq optical laryngoscope: Tracheal intubation by novice laryngoscopists. Emerg Med J. 2009;26:112–3. doi: 10.1136/emj.2008.059659. [DOI] [PubMed] [Google Scholar]
- 63.Hsu WT, Hsu SC, Lee YL, Huang JS, Chen CL. Penetrating injury of the soft palate during GlideScope intubation. Anesth Analg. 2007;104:1609–10. doi: 10.1213/01.ane.0000265490.26332.48. [DOI] [PubMed] [Google Scholar]
- 64.Vincent RD, Jr, Wimberly MP, Brockwell RC, Magnuson JS. Soft palate perforation during orotracheal intubation facilitated by the GlideScope videolaryngoscope. J Clin Anesth. 2007;19:619–21. doi: 10.1016/j.jclinane.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 65.Leong WL, Lim Y, Sia AT. Palatopharyngeal wall perforation during Glidescope intubation. Anaesth Intensive Care. 2008;36:870–4. doi: 10.1177/0310057X0803600620. [DOI] [PubMed] [Google Scholar]
- 66.Malik AM, Frogel JK. Anterior tonsillar pillar perforation during GlideScope video laryngoscopy. Anesth Analg. 2007;104:1610–1. doi: 10.1213/01.ane.0000264321.04403.06. [DOI] [PubMed] [Google Scholar]
- 67.Malik MA, Maharaj CH, Harte BH, Laffey JG. Comparison of Macintosh, Truview EVO2, Glidescope, and Airwayscope laryngoscope use in patients with cervical spine immobilization. Br J Anaesth. 2008;101:723–30. doi: 10.1093/bja/aen231. [DOI] [PubMed] [Google Scholar]
- 68.Sun DA, Warriner CB, Parsons DG, Klein R, Umedaly HS, Moult M. The GlideScope Video Laryngoscope: Randomized clinical trial in 200 patients. Br J Anaesth. 2005;94:381–4. doi: 10.1093/bja/aei041. [DOI] [PubMed] [Google Scholar]
- 69.Enomoto Y, Asai T, Arai T, Kamishima K, Okuda Y. Pentax-AWS, a new videolaryngoscope, is more effective than the Macintosh laryngoscope for tracheal intubation in patients with restricted neck movements: A randomized comparative study. Br J Anaesth. 2008;100:544–8. doi: 10.1093/bja/aen002. [DOI] [PubMed] [Google Scholar]
- 70.Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118:251–70. doi: 10.1097/ALN.0b013e31827773b2. [DOI] [PubMed] [Google Scholar]
- 71.Henderson JJ, Popat MT, Latto IP, Pearce AC. Difficult Airway Society. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia. 2004;59:675–94. doi: 10.1111/j.1365-2044.2004.03831.x. [DOI] [PubMed] [Google Scholar]
- 72.Moore AR, Schricker T, Court O. Awake videolaryngoscopy-assisted tracheal intubation of the morbidly obese. Anaesthesia. 2012;67:232–5. doi: 10.1111/j.1365-2044.2011.06979.x. [DOI] [PubMed] [Google Scholar]
- 73.Jeyadoss J, Nanjappa N, Nemeth D. Awake intubation using Pentax AWS videolaryngoscope after failed fibreoptic intubation in a morbidly obese patient with a massive thyroid tumour and tracheal compression. Anaesth Intensive Care. 2011;39:311–2. [PubMed] [Google Scholar]
- 74.Uslu B, Damgaard Nielsen R, Kristensen BB. McGrath videolaryngoscope for awake tracheal intubation in a patient with severe ankylosing spondylitis. Br J Anaesth. 2010;104:118–9. doi: 10.1093/bja/aep352. [DOI] [PubMed] [Google Scholar]
- 75.Mort TC. Tracheal tube exchange: feasibility of continuous glottic viewing with advanced laryngoscopy assistance. Anesth Analg. 2009;108:1228–31. doi: 10.1213/ane.0b013e3181990a82. [DOI] [PubMed] [Google Scholar]
- 76.Gillies M, Smith J, Langrish C. Positioning the tracheal tube during percutaneous tracheostomy: Another use for videolaryngoscopy. Br J Anaesth. 2008;101:129. doi: 10.1093/bja/aen158. [DOI] [PubMed] [Google Scholar]


