Abstract
Objectives:
The study was conducted to assess knowledge, attitude, and practice regarding insulin use among diabetic patients in tertiary care hospitals.
Materials and Methods:
Type 1 and 2 diabetic patients, aged 18 years and above, attending the Medicine/Endocrinology out-patient department or admitted as in-patients in three hospitals in and around Kolkata were enrolled. A pretested structured questionnaire comprising of 51 items was administered through face-to-face interview. Responses from 385 subjects were analyzed.
Results:
Both higher educational and higher economic standards were associated with better understanding of insulin use. Longer duration of diabetes and its treatment (oral anti-diabetic drugs and insulin) were associated with better knowledge of some parameters. Female subjects were less aware of HbA1c as a monitoring tool. Among current insulin users, 70% had never used a glucometer; only 27.33% carried simple carbohydrates for use in hypoglycemic attacks; and 32% failed to rotate sites for insulin injection.
Conclusion:
Knowledge and attitude were satisfactory on the whole but deficiencies in practice were pronounced, which can potentially be removed through appropriate counseling.
KEY WORDS: Attitude, diabetes mellitus, knowledge, mellitus, practice
Introduction
India is rapidly emerging as the diabetes capital of the world. Currently, there are approximately 63 million diabetics in India,[1] second only to China, and this figure is likely to increase substantially by 2025.[2] Insulin is mandatory for type 1 diabetes and is frequently required in type 2 diabetes as the disease progresses. Statistics from developed countries show that more than 30% of all diabetics use insulin either singly or in combination with oral anti-diabetic drugs (OADs),[3] though this figure may be lower for India.[4] Inadequate knowledge regarding insulin is likely to influence its acceptance and adherence. Being an injectable drug, its use is more likely to be influenced by misconceptions than OADs. There are several Indian studies with emphasis on diabetes epidemiology[5,6,7,8] but ones related to knowledge-attitude-practice (KAP) survey in diabetics are limited.[9,10,11] A large proportion of type 2 diabetics also eventually require insulin for blood sugar control and the assessment of their knowledge and attitude towards insulin, even if not using this drug, was considered important to evaluate the gaps that need to be addressed.
Therefore we undertook this KAP study with two objectives – to assess the extent of insulin literacy in all adult diabetics irrespective of whether they are using insulin and to assess, in actual insulin users, the extent to which they follow accepted practice.
Materials and Methods
A multicentric, cross-sectional, KAP survey was carried out between September 2012 and February 2013 among patients attending the Medicine and Endocrinology out-patient departments (OPD) or admitted to Medicine wards at three institutions – two based in urban areas (one a teaching hospital) and the third based in a small town also serving the adjoining rural population. The study subjects comprised of adult (>18 years) diabetic patients who were willing to respond to the study questionnaire. Written informed consent was obtained prior to interview and the study was cleared by the Institutional Ethics Committee.
The questionnaire used for the survey was designed by the authors and underwent content and construct validation by a peer group comprising one senior pharmacologist and two endocrinologists. It was pre-tested on a group of 30 ambulatory diabetic patients currently using insulin and educated at least up to the primary level (10 at each center) to remove any ambiguity in interpretation of the responses. All subjective terms were defined or categorized, and an individual question was reworded or reframed if three or more respondents at any of the centers faced difficulty with the question. The revised questionnaire was re-administered to the same 30 subjects after a gap of 7-10 days to ensure that no ambiguities persisted. The finalized questionnaire had 51 items of which the first 27 pertained to knowledge and attitude. The remainder focused on practice and this section was administered only to current insulin users. Data captured during the pilot survey was not reused for the actual survey. On each day of survey, the first five consecutive adult patients reporting to the relevant OPD were selected, explained about the survey and if willing, interviewed in a separate room. OPD surveys were carried out once a week at each center. Indoor patients were surveyed once every two weeks at each of the hospitals in the medicine wards (up to 10 subjects per day in the numerical sequence of the beds), excluding those who were critically ill, unwilling to participate, or already surveyed.
The calculated sample size was 385, assuming a response distribution of 50:50 on the question of whether a subject was actually using insulin, with 5% margin of error and 95% confidence level. Data have been summarized by routine descriptive statistics, and key proportions expressed with their 95% confidence interval (CI). Subgroup comparison of numerical variables was done by Student's independent samples t-test if normally distributed or by Mann-Whitney U test if otherwise. Fisher's exact test or Pearson's Chi-square test was employed for intergroup comparison of categorical variables. Chi-square test for trend analysis was used where applicable. All analyses were two-tailed. GraphPad Prism version 5 and IBM SPSS Statistics version 20 software were used for analysis.
Results
Data of all 385 surveyed subjects (216 (56.1%) indoor patients) were included in the analysis. Mean age of the study subjects was 52.1 ± 13 years (range, 25-89 years) with 95% CI being 50.8-53.4 years; with a mean duration of diabetes of 9.4 ± 7.6 years (95% CI: 8.6-10.1 years). Majority (72.20%) were under 60 years of age with 40-49 years age group being the major contributor (29.35%). More than half of the subjects were males (212; 55.06%). Almost all subjects had completed at least their primary education (96.6%) and majority were Hindus (83.9%). Around 70% had an average monthly family income of less than Rs. 25,000. All subjects were being treated with drugs, and 303 subjects (78.7%) had consulted a specialist (endocrinologist) for their diabetes at least once prior to their hospital visit. The mean duration of oral anti-diabetic drug (OAD) use was 8.3 ± 7.12 years (95% CI: 7.6-9.1 years) and among current insulin users, the mean duration of insulin use was 4.3 ± 4.57 years (95% CI: 3.59-5.06 years). There were 150 (38.96%) current insulin users while 164 (42.6%) had never been advised insulin, 47 (12.2%) advised insulin but not using it and 24 (6.23%) advised insulin temporarily in the past.
Knowledge and attitude analysis revealed interesting findings [Table 1]. Forty-seven subjects (12.21%) were not using insulin despite medical advice, of whom 9 (19.15%) were illiterate, 38 (80.85%) had a general dislike for injections, 19 (40.43%) cited financial constraints, and 25 (53.19%) were non-adherent to medical advice because they believed insulin was habit forming. Greater reluctance regarding insulin use was found among followers of Islamic faith (P < 0.001) compared to other religions.
Table 1.
Response distribution to questions pertaining to knowledge and attitude regarding insulin use (n=385)
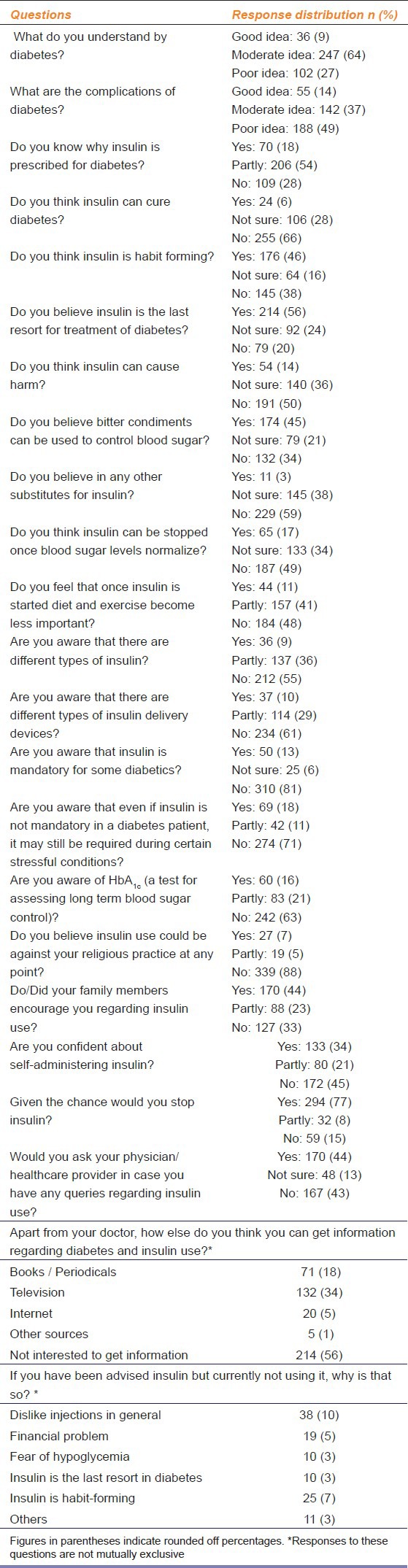
Both higher education and economic standards were associated with significantly higher (P < 0.001) understanding of diabetic complications, the benefits of insulin use, awareness that insulin is not habit forming, need for continuity, and the confidence for self-administration of insulin. Longer duration of diabetes (>10 years) was associated with awareness of continuing insulin use (P = 0.031) and that insulin is not habit forming (P = 0.039). Longer duration of OAD use (≥ 3 years) was associated with better knowledge about diabetic complications (P = 0.013), benefits of insulin use (P < 0.001), awareness that insulin is not habit forming in nature (P = 0.001), need for continuity in insulin use (P = 0.002), and the confidence for self-administration of insulin (P = 0.042). Longer duration of insulin use (>3 years) was also associated with better understanding (P < 0.05) of the benefits of insulin and the confidence for self-administration of the injection. Of all subjects, 276 (71.7%) had a modest understanding of the role of insulin and only 24 (6.2%) believed that insulin could cure diabetes.
A substantial proportion (45.2%) believed that bitter condiments (like bitter gourd or neem) could be used to control blood sugar, although only 11 (2.86%) believed that insulin could be “substituted” in any way. Among 54 (14%) subjects who felt insulin was harmful, hypoglycemia was the most common fear. Only 170 (44.2%) had discussed with their healthcare provider regarding insulin, and 214 (55.6%) were currently not interested to gather information about insulin from physicians or other sources. Overall, 294 (76.4%) subjects opined that, given the chance, they would stop insulin; the proportion was 87.80% among those who were never advised insulin but dropped to 54.67% among current insulin users-a statistically significant difference (P < 0.001). A significantly higher proportion of women opined that they were likely to discontinue insulin (P < 0.001).
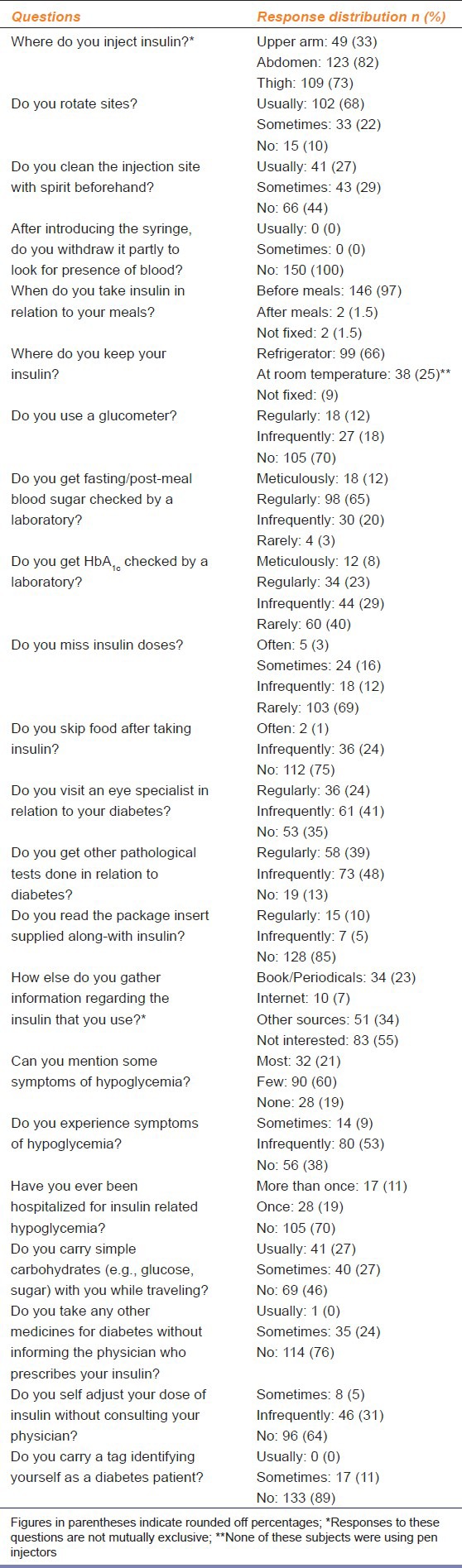
There were 150 current insulin users (38.96% of the sample), of whom 117 (78%) used vials, 18 (12%) pen injectors and 15 (10%) resorted to both; 109 (72.7%) administered insulin themselves; 36 (24%) subjects also took indigenous medications along with insulin; and alarmingly, 54 (36%) had at some point self-adjusted their doses without medical advice. Of the insulin users, 116 (77.3%) did get their blood glucose checked periodically and 121 (80.7%) had rarely, if at all, missed insulin doses. However, 105 (70%) had never used a glucometer and only 18 (12%) used a glucometer regularly for home blood glucose monitoring. It is of concern to note that 38 (25.3%) subjects reported a significant number of meals skipped following insulin injection. While 122 (81.3%) patients could enumerate the essential symptoms of hypoglycemia, only 41 (27.3%) patients made it a practice to carry simple carbohydrates (e.g. glucose sachets, sugar cubes) for use during such attacks. There was no association with education status in this regard. Table 2 lists the findings related to practice of insulin use in the study subjects.
Table 2.
Response distribution to questions pertaining to practice of insulin use (n=150)
Discussion
Aided by increasing urbanization, rural to urban migration, adoption of sedentary lifestyle, and unhealthy food habits, the diabetes pandemic continues to snowball worldwide. These adverse factors interact with the already heightened genetic predisposition for diabetes among Indians, leading to onset of diabetes at a younger age.[12] In addition to modification of diet and lifestyle and institution of insulin or other anti-diabetic drugs, the management of this complex metabolic disease needs continuous educational and counseling efforts. The need is all the more acute among diabetics on insulin to ensure its effective and safe use. Our KAP study was conceived in this context to capture data regarding insulin use and its perceived advantages and disadvantages.
As far as knowledge and attitude are considered, the study population showed satisfactory trends comparable to earlier KAP studies conducted in other parts of India.[9,10,11,12] However, there are some points of difference in our study. Approximately 51% of our subjects had a satisfactory idea about diabetes and its signs and symptoms, while 60-77% subjects had good idea in a study done with Bhilai steel plant workers who were mostly educated at least up to graduation level. Only a minority of our subjects (even if well-educated) reported carrying simple sugars while traveling as precaution against serious hypoglycemia-this figure is 67.1% in a hospital-based KAP study in Bijapur.[10] Overall, in our study, awareness regarding insulin as a therapeutic option was satisfactory and the belief that insulin could cure diabetes or that it could be substituted was minimal. On the negative side, even some well-educated subjects were not using insulin in spite of medical advice. Paucity of knowledge regarding the necessity for continuity of insulin administration and pronounced inhibition to discuss insulin treatment with the physician were other notable findings.
Some aspects of practice were satisfactory. Neither skipping insulin doses nor meals after taking insulin emerged as lacunae, and majority were getting their blood glucose checked regularly. However, the scenario regarding some “modern” practices was dismal. Only a handful used glucometer regularly, majority had never used one. This is particularly significant, as guidelines from western countries clearly recommend self-monitoring of blood glucose in insulin users.[13] Despite knowledge of hypoglycemia symptoms, only a quarter of insulin users carried simple carbohydrates with them while traveling, and a miniscule number had ever carried a tag for identification as a diabetic on insulin. Considering the potentially life-saving impact of these two simple interventions, this aspect merits further evaluation and emphasis in diabetes clinics. The practice aspect needs improvement through careful initial counseling and reiteration at each follow-up visit. The use of counseling checklists may be considered.
Despite care to spread out our data collection over time and space, our study has its share of limitations. The sampling was purposive rather than random. A relatively younger age group (40-49 years) comprised the major proportion of our sample, and both literacy rate and economic standards were higher than the averages for Indian population.
Despite these limitations, this study provides a “situation analysis” regarding insulin in diabetic patients visiting hospitals. This can be utilized as baseline to identify educational needs and plan more effective diabetes care services. Studies from the Indian subcontinent have shown that substantial expenditure is incurred by people with diabetes; resources could be saved by earlier detection, effective management, and effective reduction in diabetes co-morbidities and complications through insulin-based improved diabetes care.[14] Some monitoring and practice aspects need urgent attention. Diabetes clinics in tertiary care hospitals are probably in the best position to launch interventional and educational programs with the help of local physicians, healthcare workers, community leaders, and mass media.
Acknowledgments
The authors are grateful to Mrs. Bandana Das Choudhury for preparation of the informed consent documents in vernacular (Hindi and Bengali) language.
Footnotes
Source of Support: Nill
Conflict of Interest: No
References
- 1.International Diabetes Federation. IDF diabetes atlas. 5th ed. 2012. [Last accessed on 2013 Nov 15, Last cited on 2013 Nov 20]. Available from: http://www.idf.org/sites/default/files/5E_IDFAtlasPoster_2012_EN.pdf .
- 2.Mohan V, Sandeep S, Deepa R, Shah B, Varghese C. Epidemiology of type 2 diabetes: Indian scenario. Indian J Med Res. 2007;125:217–30. [PubMed] [Google Scholar]
- 3.United States Centers for Disease Control and Prevention. Diabetes data and trends: Age-adjusted percentage of adults with diabetes using diabetes medication, by type of medication, United States, 1997-2011 [document on the internet] 2013. [Last accessed on 2013 Nov 20]. Available from: http://www.cdc.gov/diabetes/statistics/meduse/fig2.htm .
- 4.Kapur A, Shishoo S, Ahuja MM, Sen V, Mankame K. Diabetes care in India-patient's perceptions, attitudes and practices. Int J Diabetes Dev Ctries. 1997;17:5–14. [Google Scholar]
- 5.Ramachandran A, Jali MV, Mohan V, Snehlata C, Vishwanathan M. High prevalence of diabetes in an urban population of southern India. BMJ. 1988;297:587–90. doi: 10.1136/bmj.297.6648.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mishra A, Pandey RM, Devi JR, Sharma R, Vikram NK, Khanna N. High prevalence of diabetes, obesity and dyslipidemia in urban slum population in northern India. Int J Obes Relat Metab Disord. 2001;25:1722–9. doi: 10.1038/sj.ijo.0801748. [DOI] [PubMed] [Google Scholar]
- 7.Madhu SV, Rao PV. Epidemiology of diabetes mellitus in India. In: Tripathi BB, Chandalia HB, editors. RSSDI Textbook of Diabetes Mellitus. 2nd ed. Hyderabad: Research Society for study of diabetes in India; 2008. pp. 209–26. [Google Scholar]
- 8.Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK, et al. Diabetes Epidemiology Study Group in India (DESI) High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia. 2001;44:1094–101. doi: 10.1007/s001250100627. [DOI] [PubMed] [Google Scholar]
- 9.Shah VN, Kamdar PK, Shah N. Assessing the knowledge, attitudes and practice of type 2 diabetes among patients of Saurashtra region, Gujarat. Int J Diabetes Dev Ctries. 2009;29:118–22. doi: 10.4103/0973-3930.54288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Priyanka Raj CK, Angadi MM. Hospital-based KAP study on diabetes in Bijapur, Karnataka. Indian J Med Spec. 2010;1:80–3. [Google Scholar]
- 11.Malathy R, Narmadha M, Ramesh S, Alvin JM, Dinesh BN. Effect of a diabetes counseling programme on knowledge, attitude and practice among diabetic patients in Erode district of South India. J Young Pharm. 2011;3:65–72. doi: 10.4103/0975-1483.76422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Behera SK, Behera RR, Thakur H. A study of knowledge and practices in prevention of type 2 diabetes mellitus among Bhilai steel plant employees. Indian J Med Specialities. 2012;3:143–8. [Google Scholar]
- 13.American Diabetes Association. Standards of medical care in diabetes-2012. Diabetes Care. 2012;35(Suppl 1):S11–63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khowaja AL, Khuwaja AK, Cosgrove P. Cost of diabetes care I out-patient clinics of Karachi, Pakistan. BMC Health Serv Res. 2007;7:189. doi: 10.1186/1472-6963-7-189. [DOI] [PMC free article] [PubMed] [Google Scholar]


