Abstract
Aim
Perforation of the anterior cortex during femoral intramedullary nailing can be a major complication. We aim to determine the influence of entry point and radius of curvature on intramedullary nail position in the distal femur using a synthetic bone model.
Methods
Using synthetic femora, the greater trochanter was measured and entry points marked in two planes. A standard recommended technique was used to insert two different Stryker Gamma 3 intramedullary nails of different radius of curvature. The synthetic femora were sectioned and the centre of nail to anterior cortex distance (CAD) was measured. Statistical interpretation of the results was performed using linear regression analyses.
Results
We found that the more posterior entry points led to a more anterior placement in the distal femur in both nails of differing radius of curvature (11 mm and 13.5 mm CAD). The smaller radius of curvature led to a more central placement of the nail tip in the distal femur.
Conclusion
Anterior penetration of the distal femur can be minimized by a more anterior entry point and with the use of a femoral intramedullary nail with a smaller radius of curvature.
Keywords: Entry point, Femoral nail, Radius of curvature
1. Introduction
Anterior penetration of the distal femur during the insertion of a femoral intramedullary nail is a major complication with implications on post-operative rehabilitation and function (Fig. 1). With the increase in metabolic bone disease, osteoporosis and bisphosphonate use, there is a cohort of patients with deformities in their femoral bow. Stress fractures managed with intramedullary nailing can be difficult when the anterior bow does not correspond with the available radii of curvature of common femoral nails. There are concerns of supracondylar femoral fractures as a result of nail penetration.1
Fig. 1.

(a) Radiograph intra-operatively of the lateral distal femur showing penetration of the distal nail through the anterior cortex. (b) Sagittal computed tomography (CT) reconstruction of the distal femur. (c) Axial CT reconstruction of the distal femur in the same patient.
Factors contributing to nail penetration include abnormal femoral anatomy, variable trochanteric entry point and the trajectory of trochanteric guide wire and reamer. Other factors include the mismatch between the anatomical femoral bow and femoral nail radius of curvature,2 a property that is not readily available or emphasized in many manufacturers' product information guides. Nail length and diameter may also play a role in combination with the radius of curvature. That is, penetration of the anterior cortex may be prevented if a shorter length nail is chosen even if its radius of curvature is relatively large.3 Fracture pattern and position are also important. A mismatch can occur in an intertrochanteric fracture with a distal bow, compared to that of a mid-shaft fracture with a distal bow.
Our paper demonstrates that the radius of curvature of a femoral nail as well as the position and trajectory of the trochanteric guide wire and entry reamer, influences positioning of the nail in the distal femur. To our knowledge, no previous study has demonstrated this.
2. Materials and methods
Synthetic femora supplied by Stryker™ (Stryker Howmedica, Ritherford, NJ) were used for this study. The greater trochanter was measured as 39 mm in the sagittal plane at the point corresponding to the proximal tip on an antero-posterior fluoroscopic image. The greater trochanter was subsequently divided into anterior, middle and posterior thirds, each measuring 13 mm in length. Points ‘a’, ‘c’, and ‘e’ were defined as points in the centre of each third.
A standard Stryker 3.2 mm entry K-wire was directed towards the centre of femoral shaft in the coronal and sagittal plane. A point in the sagittal plane 150 mm inferior to the tip of the greater trochanter in the centre of the shaft was chosen as the end point for this wire. A line was drawn from the entry point of the K-wire to the point on the lateral shaft to give the trajectory in the sagittal plane.
A 15.5 mm trochanteric entry reamer was used to open each trochanter. The synthetic saw bones were manufactured to be pre-reamed to 14 mm along the canal of the femora. This simulated our routine technique of sequential cannulated reaming to 1.5 mm greater than the proposed diameter of intramedullary nail. In this study we used two different types of Stryker™ Gamma 3 trochanteric intramedullary nails. One with a diameter of 10 mm and radius of curvature of 150 cm, and the other with a diameter of 11 mm and radius of curvature of 200 cm (Fig. 2). The neck angle and length were kept constant.
Fig. 2.
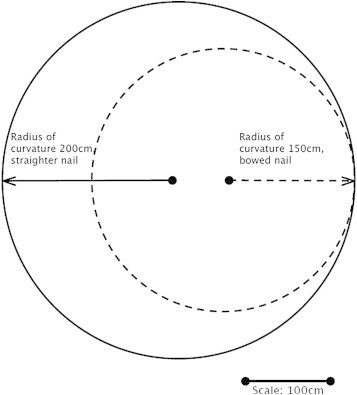
Schematic diagram demonstrating effect of radius of curvature.
A total of ten synthetic femora were used, two for each entry point (a to e) using each type of nail (200 and 150 radii of curvature). The femora were sectioned distal to the tip of each nail. The centre of the nail to the anterior cortex distance (CAD) was measured, perpendicular to the epicondylar axis. This step was performed by an independent observer blinded to the entry point and the type of nail used. The nail anteversion was kept in line with the femoral neck to ensure that any differences in the CAD were not due to rotation of the nail in the intramedullary canal.
To determine the influence of entry point and radius of curvature on intramedullary nail position we conducted linear regression analyses. Univariate analyses were conducted followed by multivariate analysis. The outcome in all analyses was the measurement from the centre of the nail to the anterior cortex distance (CAD), measured in millimetres. P values less than 0.05 were considered significant. Statistical analyses were carried out using STATA software (Stata11, StataCorp LP, Texas, USA).
3. Results
There was a significant association between femoral nail entry point and CAD score after allowing for radius of curvature (t8 = −2.31, P < 0.05), and also between radius of curvature and CAD score after allowing for entry point (t8 = 3.32, P < 0.02). On multiple regression, both entry point and radius of curvature were both significantly associated with CAD score, P < 0.0001. Using the 10 mm diameter nail with a 150 cm radius of curvature as opposed to a 11 mm diameter nail with a 200 cm radius of curvature, after controlling for nail entry point, resulted in an average 3.4 mm increase in CAD score (95% confidence interval 2.8 mm to 4.0 mm) (Table 1, Fig. 3). The more anterior the entry point, after controlling for nail diameter and radius of curvature, the higher the CAD score, with the model predicting a 1 mm difference for each point on average (95% confidence interval 0.8 mm to 1.2 mm).
Fig. 3.
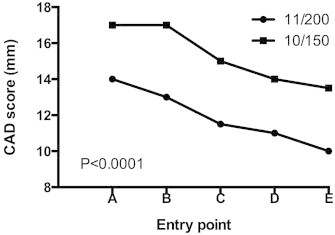
Graph demonstrating CAD scores with varying entry points for each nail (150 cm and 200 cm radius of curvature).
In summary, the more anterior the entry point and the smaller the radius of curvature of an intramedullary femoral nail, the greater the CAD score, and the less likelihood of anterior penetration of the femoral nail in the distal femur.
4. Discussion
Anterior penetration of the distal femur during femoral intramedullary nailing is a complication that has a significant bearing on a patient's post-operative course. It can change their outcome and function. There is a paucity of evidence looking at risk factors for anterior femoral cortex penetration during intramedullary nailing. This preventable complication can be addressed with careful surgical technique and attention to specific factors. To our knowledge this is the first synthetic bone model study on this topic.
Roberts et al retrospectively reviewed 150 patients treated with intramedullary fixation of proximal femur fractures and found that 25% of patients had anterior ‘cortical impingement’.3 They sought to determine preoperative factors that would place patients at a higher risk of cortical impingement. Factors identified as contributing to this included increasing femoral angle of incidence (increasing femoral anterior bow), shorter patients (less than 160 cm in height) and an entry point in the posterior one-third of the greater trochanter. These findings are consistent with our study, where an anterior one-third entry point increased the CAD. We found that the more posterior entry points in our study showed an increased angle of trajectory for the nail, which increased the relative bow of the femur. These findings stress the importance of preoperative planning and knowledge of specific dimensions of the proposed nail to be implanted.
There have been two series reporting early and late supracondylar fractures secondary to anterior penetration of the nail in the distal femur.1,2 Two percent of patients (5 of 302) in one series fractured at the distal nail tip in the early postoperatively period, with two of these patients noted to have marked anterior bowing of the femur. Egol et al highlighted design deficiencies in most current femoral intramedullary implants, with the mismatch between their range of radius of curvature (186 cm to 300 cm) and the mean femoral radius of curvature (120 cm).4
Currently manufactured femoral nails have differing radii of curvature depending on the manufacturer, the specific type of nail and even the nail length. For example, the Stryker™ Gamma 3 trochanteric intramedullary nail has the option of a 200 cm or 150 cm radius of curvature. However, this fact is not readily available in the product surgical technique guide. The Synthes™ (Paoli, PA) A2FN has an increasing radius of curvature as the nail length increases to accommodate the likely variations in anatomy with differing patient stature. This information is not readily available in the product surgical technique guide. Furthermore, because of the high rate of anterior impingement and lack of occurrence of posterior nail tip position, the development and availability of more implants with smaller radius of curvature should be considered.3
There are limitations to our study. Synthetic bones are useful for practicing surgical techniques and refining skills, however their internal characteristics and modulus of elasticity are markedly different to human femora. The advantages of using synthetic bones in our study include that each bone is identical in shape and length as well as medullary canal diameter, width and position. We felt that it would not be practical nor ethical to perform a similar prospective study on patients with femoral fractures due to the changes of fracture reduction and fixation caused by differing entry points and nail type. Cadaveric models could be used; however, this would be resource intensive in Australia where cadaveric specimens are at a premium. It would also require the use of the image intensifier which could introduce error in image projection and interpretation. The individual results would also be difficult to interpret due to the variations of cadaveric femoral anatomy.
Manufacturers of synthetic femora report their quality to resemble young bone as opposed to older, more osteoporotic bone. The cortical diameter of a synthetic bone is uniform throughout, which is certainly not true of cadaveric or live femora. None of the nail tips in our study came close to ‘impinging’ or penetrating the anterior cortex of the distal femur because of the dense quality of synthetic cancellous and cortical bone in the models. It would be reasonable to assume that the results in our study would be more dramatic, with lower CAD's and higher rates of penetration, if performed on cadaveric or live femora due to the osteoporotic quality of bones with the greater amount of thinning occurring in the anterior femoral cortex.1,5 It has been shown in anatomical studies that the medullary canal of the distal femur does not lie centrally within the femur, but is positioned slightly anterior.4,6
We have shown that the anterior penetration of the distal femur can be minimized by a more anterior entry point and with the use of a femoral intramedullary nail with a smaller radius of curvature. Further research looking at the effects of differing entry points and radius of curvature in cadaveric specimens would be beneficial.
Conflicts of interest
All authors have none to declare.
References
- 1.Ostrum R.F., Levy M.S. Penetration of the distal femoral anterior cortex during intramedullary nailing for subtrochanteric fractures: a report of three cases. J Orthop Trauma. 2005;19:656–660. doi: 10.1097/01.bot.0000154481.46693.69. [DOI] [PubMed] [Google Scholar]
- 2.Robinson C.M., Houshian S., Khan L.A.K. Trochanteric-entry long cephalomedullary nailing of subtrochanteric fractures caused by low-energy trauma. J Bone Joint Surg Am. 2005;87:2217–2226. doi: 10.2106/JBJS.D.02898. [DOI] [PubMed] [Google Scholar]
- 3.Roberts J.W., Libet L.A., Wolinsky P.R. Who is in danger? Impingement and penetration of the anterior cortex of the distal femur during intramedullary nailing of proximal femur fractures. J Trauma Acute Care Surg. 2012;73:249–254. doi: 10.1097/TA.0b013e318256a0b6. [DOI] [PubMed] [Google Scholar]
- 4.Egol K.A., Chang E.Y., Cvitkovic J., Kummer F.J., Koval K.J. Mismatch of current intramedullary nails with the anterior bow of the femur. J Orthop Trauma. 2004;18:410–415. doi: 10.1097/00005131-200408000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Feik S.A., Thomas C.D., Bruns R., Clement J.G. Regional variations in cortical modeling in the femoral mid-shaft: sex and age differences. Am J Phys Anthropol. 2000;112:191–205. doi: 10.1002/(SICI)1096-8644(2000)112:2<191::AID-AJPA6>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 6.Walensky N.A. A study of anterior femoral curvature in man. Anat Rec. 1965;2001:221–228. doi: 10.1002/ar.1091510406. [DOI] [PubMed] [Google Scholar]


