Abstract
In recent years, a growing number of potential autoimmune disorders affecting neurons in the central nervous system have been identified, including narcolepsy. Narcolepsy is a lifelong sleep disorder characterized by excessive daytime sleepiness with irresistible sleep attacks, cataplexy (sudden bilateral loss of muscle tone), hypnagogic hallucinations, and abnormalities of Rapid Eye Movement sleep. Narcolepsy is generally a sporadic disorder and is caused by the loss of hypocretin (orexin)-producing neurons in the hypothalamus region of the brain. Studies have established that more than 90% of patients have a genetic association with HLA DQB1*06:02. Genome-wide association analysis shows a strong association between narcolepsy and polymorphisms in the TCRα locus and weaker associations within TNFSF4 (also called OX40L), Cathepsin H and the P2RY11-DNMT1 (purinergic receptor subtype P2Y11 to DNMT1, a DNA methytransferase) loci, suggesting an autoimmune basis. Mutations in DNMT1 have also been reported to cause narcolepsy in association with a complex neurological syndrome, suggesting the importance of DNA methylation in the pathology. More recently, narcolepsy was identified in association with seasonal streptococcus, H1N1 infections and following AS03-adjuvanted pH1N1 influenza vaccination in Northern Europe. Potential immunological pathways responsible for the loss of hypocretin producing neurons in these cases may be molecular mimicry or bystander activation. Specific autoantibodies or T cells cross-reactive with hypocretin neurons have not yet been identified, however, thus narcolepsy does not meet Witebsky’s criteria for an autoimmune disease. As the brain is not an easily accessible organ, mechanisms of disease initiation and progression remain a challenge to researchers.
Keywords: Narcolepsy, Hypocretin, H1N1 infection, HLA association, Autoimmune
1. Introduction
Narcolepsy is a chronic debilitating sleep disorder that was first described in the late 19th century and can be characterized by excessive daytime sleepiness, disrupted nocturnal sleep, rapid eye movement (REM) sleep occurring at the onset of sleep, and cataplexy (a sudden progressive loss of skeletal muscle tone in response to strong emotional stimuli) [1-3]. The presence of cataplexy is distinctively characteristic for narcolepsy and is defined by sudden and transient episodes of bilateral loss of muscle tone of brief duration (less than 2 min), often triggered by emotions – most reliably laughing or joking – with preserved consciousness [4,5]. Sleep paralysis (an inability to move, most commonly upon awakening) and hypnagogic hallucinations (dream-like events occurring at sleep onset) are also frequently associated with the disease, though these symptoms are more variable [1,6]. The pathophysiology of narcolepsy is closely related to abnormalities of REM sleep that are the electrophysiologic signature of the syndrome [7,8]. Treatment of narcolepsy is usually symptomatic and uses stimulants such as amphetamine and Modafinil, antidepressants such as Venlafaxine and Clomipramine, and sodium oxybate, a strong sedative for overnight sleep [9-13].
Over the last two decades, the understanding of the pathophysiology of narcolepsy has increased greatly. Mainly based on the tight association of narcolepsy with a specific HLA subtype (DQB1*06:02), many authors have postulated that the disorder may be autoimmune in nature. In continuation of these HLA associations, recent data on disease onset in children and its association with H1N1-infection and vaccination indicate that mechanisms such as molecular mimicry or bystander activation could be essential contributors in the development of narcolepsy. In this review, we will discuss data supporting an autoimmune basis of narcolepsy.
1.1. Loss of hypocretin producing neurons
Hypocretin (orexin) neurons play a critical role in the regulation of sleep and wakefulness, and disturbances of the hypocretin system have been directly linked to narcolepsy in animals and humans [14-16]. Hypocretin is an excitatory neuropeptide hormone produced in the hypothalamus region of the brain, functioning to promote wakefulness, food intake, and energy expenditure [17-19]. Hypocretins 1 and 2, also called orexins A and B, are two dorso-lateral hypothalamic neuropeptides that function by regulating sleepe –wake cycles, food intake, and pleasure-seeking behavior [18]. Amongst the areas of the brain that the neurons producing hypocretins project to are the locus coeruleus, tuberomammillary nucleus, raphe nucleus, and ventral tegmental areas [20]. These areas contain norepinephrine, histamine, serotonin, and dopamine containing neurons, respectively. Deficiency of hypocretin likely leads to the malfunctioning of these systems and is manifested in the form of abnormal REM sleep and excessive daytime sleepiness [21]. Hypocretin neurons also project to other areas of the hypothalamus, olfactory bulb, cerebral cortex, thalamus, brainstem and even spinal cord [20,22]. The participation of these other projections to the phenotype of narcolepsy is less studied but also likely.
In 1979, studies in Doberman Pinschers demonstrated that narcolepsy was inherited in a single autosomal recessive pattern [23]. Genetic studies in canines later linked this phenotype to a mutation in the hypocretin receptor 2 gene [24]. In 2000, Nishino and coworkers presented some of the earliest reports of hypocretin deficiency in narcoleptic patients with cataplexy. Their study showed that seven of nine patients having narcolepsy with cataplexy had no detectable hypocretin in their CSF, however all of the controls had detectable hypocretin neuropeptides in their CSF [25]. After these initial findings, a multitude of additional studies have supported a connection between the loss of hypocretin neuropeptides and narcolepsy with cataplexy [26,27]. Interestingly, it was later found out that, unlike in canines, hypocretin deficiency in humans diagnosed with narcolepsy with cataplexy was not due to mutations in hypocretin system genes but rather a secondary loss of hypocretin neurons in the dorso-lateral hypothalamus [26,27]. A study from Peyron et al. found that only one HLA negative early onset narcoleptic patient had a hypocretin mutation among 74 other patients (including many with early onset or atypical features) screened for similar mutations [27]. Their group also reported the loss of hypocretin neurons in the brains of six deceased patients with narcolepsy with cataplexy. Thannickal et al. later reported that hypocretin neurons are reduced by 85%–95% in association with evidence of gliosis [26]. Another interesting observation is that the nearby melanin-concentrating hormone neurons are found intact in narcolepsy with cataplexy brain tissues [28]. The very specific loss of hypocretin producing neurons that result in the development of narcolepsy with cataplexy indicates a potential autoimmune driven process.
1.2. Strong HLA association with narcolepsy
The MHC, also known in humans as the human leukocyte antigen (HLA) region, is one of the most gene dense region of the human genome, encoding 252 expressed loci including several key immune response genes [29]. The extent of linkage disequilibrium within the region has proved to be challenging when trying to extract the exact location of etiological variants [30,31]. Components of the HLA class II encoded HLA-DRB1-DQA1-DQB1 haplotype have been associated with several autoimmune diseases, including rheumatoid arthritis, type 1 diabetes and Graves’ disease [32-36]. Antigen presentation and T cell activation are important for triggering autoimmune responses, and the findings above have prompted investigators to study many genes within HLA pathways for a potential association with narcolepsy.
Narcolepsy is genetically characterized by a strong linkage to specific HLA alleles. A genetic association of narcolepsy with HLA-DR2 and HLA-DQ1 in the major histocompatibility (MHC) region was described more than 25 years ago [37]. Mignot et al. discovered that HLA DQA1*01:02 and DQB1*06:02 are the primary candidate susceptibility genes for narcolepsy in the HLA class II region and reported that complex HLA-DR and -DQ interactions contribute to the genetic predisposition to human narcolepsy [38,39]. Additional studies established that more than 85% of patients diagnosed with narcolepsy with cataplexy have HLA DQB1*06:02, often in combination with HLA DR2 (DRB1*1501), while only half of patients displaying atypical, mild, or narcolepsy without cataplexy have HLA DQB1*06:02 [40]. Other HLA alleles affect the predisposition to narcolepsy with cataplexy [41,42]. Interestingly, the occurrence of the HLA DQB*06:02 allele is not limited to narcolepsy with cataplexy, and is found in 12%–38% of the general population [43,44].
1.3. Non-HLA genes associated with narcolepsy
Although the majority of patients with the sporadic form of narcolepsy are HLA DQB1*06:02 positive, there have been consistent reports of patients with defined narcolepsy-cataplexy, without the HLA DQB1*06:02 allele [41,45]. During studies of multiplex families, it was found that more than one third of patients are negative for HLA DQB1*06:02. These findings indicate that genetic predisposition to narcolepsy cannot not be fully explained by HLA allele association, and that additional non-HLA gene components contribute to the development of the disease in at least some cases [46-48].
More recently, through the use of genome-wide association (GWA) analysis in three ethnic groups, researchers have found a strong association between narcolepsy (mostly sporadic cases with DQB1*06:02) and polymorphisms in the TCRα (T-cell receptor alpha) locus [49]. The TCR is a molecule expressed on the surface of T cells that plays an important role in the recognition of antigens bound to HLA molecules [50]. These findings together with the strong association with HLA DQA1*01:02 and DQB1*06:02, strongly suggest an autoimmune basis in the development of narcolepsy may be through CD4+ T cells since those are recognizing HLA-DQ.
Other loci are also involved. Kornum et al. reported GWA analyzes for narcolepsy in three ethnic groups and identified an additional SNP in the 3′ untranslated region of P2RY11, the purinergic receptor subtype P2Y11 gene [51]. In addition, analysis revealed that the P2RY11 receptor is highly expressed in cytotoxic CD8+ T lymphocytes, further complicating the etiology of the cell types involved in the development of narcolepsy. Complementing this observation, Winkelmann et al. observed that a dominant clinical phenotype that includes narcolepsy with cataplexy, deafness, cerebellar ataxia, and dementia (ADCA-DN) that was due to highly penetrant DNMT1 gene mutations [52]. As DNMT1 is located in extremely close proximity to P2RY11 (within 30 kb), it is possible that the genetic association in sporadic cases and the rare autosomal dominant ADCA-NC disease could be linked somehow. DNMT1 is a DNA methytransferase that is highly expressed in immune system cells, and hypomethylation has been shown to be involved in other autoimmune diseases such as lupus. DNMT1 also plays an important role in differentiation of CD4+ T cells into T regulatory cells by relieving repression of Foxp3 expression following TCR stimulation [53]. A possibility would be that an absence of T regulatory cells with specificity toward hypocretin neurons could result in autoimmunity. Complicating this picture however, DNMT1 and DNA methylation is also important for neuronal survival and neurodegeneration, so these loci could have effects on narcolepsy at multiple levels.
In a recently published study, Faraco et al. [54] used the Immunochip, an SNP chip designed to further fine map various autoimmune disease loci, and found that variants in two additional loci, Cathepsin H and Tumor necrosis factor super family member 4 (TNFSF4, also called OX40L), attained genome-wide significance [54]. As these genes are important for antigen processing and downstream T cell stimulatory effects, these findings further implicate the process of antigen presentation by HLA Class II+ APCs to T cells in the pathophysiology of narcolepsy.
1.4. Humoral immunity and role of autoantibody in narcolepsy
The occurrence of autoantibody is an important feature of autoimmune diseases and one of important factor for Witebsky’s defining criteria for an autoimmune disease [55]. Autoantibodies have been found in autoimmune diseases primarily affecting neurons in central nervous system [56]. Investigators have long searched for autoantibodies that would cross the blood brain barrier and lead to the destruction of hypocretin-secreting neurons and the subsequent development of narcolepsy. A report from Aran et al. showed elevated levels of anti-Streptococcal antibodies in patients’ serum with recent onset of narcolepsy [57]. A study in Japan of narcoleptic and idiopathic hypersomnia patients revealed altered levels of IgG subclasses, indicating humoral immune alteration in narcolepsy and idiopathic hypersomnia [58]. More recently, studies have been published that describe the detection of autoantibodies against tribbles homologue 2 (TRIB2) in narcoleptic individuals. Cvetkovics – Lopes et al. reported that a portion of narcolepsy subjects with recent disease onset carried anti-TRIB2 autoantibodies [59]. Recently, while conducting quality receiver operating characteristic curve (QROC) analysis, the Mignot group further determined that a cutoff point of 2.3 years following cataplexy onset was a strong predictor for the presence of the anti-TRIB2 autoantibodies [60]. However, TRIB2 is expressed in many other cell components both in CNS and periphery including immune cells [61-63]. So it is more likely that TRIB2 autoantibodies are not the causative factor for hypocretin-cell destruction but a downstream effect of cell loss. Finally, recent studies, notably in post H1N1 2009 cases, have not found TRIB2 autoantibodies, suggest possible heterogeneity in triggering factors [64].
Many recent studies have also focused on the prepro-hypocretin, hypocretin or the hypocretin system as direct targets of autoantibodies. Black et al. found no evidence for IgG reactivity to prepro-hypocretin or its cleavage products in CSF of DQB1*06:02-positive narcoleptic patients [65,66]. These results suggest that the generation of autoantibodies directed against prepro-hypocretin or its peptide cleavage products are unlikely to mediate the development of narcolepsy. Similar results were generated by Tanaka et al. who developed a sensitive radio-ligand assay to screen for antibodies directed against hypocretin-1 and -2, and its two known hypocretin receptors [67]. Using a different approach, Smith et al. transferred immunoglobulins from narcoleptic patients into mice and then tested for contractile responses to the muscarinic agonist carbachol in the bladder. They reported that the mice treated with patient IgG showed a significantly increased response to carbachol. However, this effect was indirect, as direct application of purified IgG on the bladder preparation did not yield the same results. Furthermore, the authors reported behavioral changes in the mice treated with patient immunoglobulins [68]. The mechanism through which a putative antibody affecting peripheral cholinergic transmission could lead to narcolepsy is unclear. Moreover, attempts to replicate these findings using different mice strains and longer-term administration of narcolepsy sera or immunoglobulins have been negative so far (unpublished data). Overall, we believe that extensive studies have not provided conclusive evidence for a humoral-based immune response against the hypocretin system in the development of narcolepsy.
1.5. H1N1 infection/vaccination and recent onset of narcolepsy
In recent years, research has focused on the potential role of 2009 pandemic H1N1 (pH1N1) infections and vaccination in the onset of narcolepsy. Finnish investigators first suggested the possibility that narcolepsy/hypocretin deficiency could be triggered by H1N1 vaccination. They reported that Pandemrix, an adjuvanted AS03 pandemic H1N1 vaccine used in Europe likely contributed to the onset of narcolepsy among those 4–19 years old during the influenza pandemic of 2009–2010 [69]. Finnish reports also found a 12.7-fold risk of narcolepsy in 4–19 year-old individuals within approximately 8 months after Pandemrix vaccination as compared to unvaccinated individuals in the same age group [69]. Similar reports come from Sweden where around 200 cases of post-Pandemrix narcolepsy have been reported to the Swedish Authority. More recently, the European Center for Disease Control and Prevention (ECDC) and Vaccine Adverse Event Surveillance and Communication Consortium (VAESCO) reviewed epidemiological data that suggested an increase in narcoleptic diagnoses starting in 2008 [70]. The VAESCO report revealed that in Sweden and Finland, caseecontrol studies showed association between AS03-adjuvanted vaccine and an increased risk of narcolepsy in population aged 5–19 years [71]. Although no increase in incidence of narcolepsy has been observed in Italy, the Netherlands, and the United Kingdom, vaccine coverage was low in these countries (ECDC report 2012) [71].
Also implicating a connection between pH1N1 and the development of narcolepsy is a study from China showing that narcoleptic onset in children is highly correlated with seasonal and annual patterns of upper airway infections, including a large peak following the 2009–2010H1N1 influenza pandemic [72]. It was also observed that the peak of diagnosed narcoleptic individuals was 6 months following winter pH1N1 infections in 2009–2010, and that the correlation was independent of H1N1 vaccination in the majority of individuals [72]. Another recent study from Korea however found no increase in the number of narcolepsy incident cases or incidence rates during the influenza A (H1N1)pdm09 vaccination period in South Korea, although few cases were found [73]. Although not fully conclusive, these findings strongly suggest an association between H1N1, Pandemrix and the development of narcolepsy-cataplexy.
1.6. Possible mechanism underlying the association of H1N1 with narcolepsy
Narcolepsy, like other autoimmune diseases, is multifactorial. In addition to HLA and other genetic associations, other factors including environmental ones must be involved. In some earlier studies, T cells subsets (helper/cytotoxic) have been examined in narcolepsy patients, and no major changes were found [74,75]. A possible mechanism that could be involved is molecular mimicry involving cross-reactivity of H1N1-specific T cells and hypocretin-producing neurons. Cross-reactive CD4+ T cells that recognize both a foreign H1N1 epitope and an epitope present on hypocretin-producing cells and presented by HLA-DQB1*06:02 by antigen presenting cells could however be involved with a major overall alteration of T cell subsets (Fig. 1). The generation of a strong immune response mediated by the ASO3 adjuvant or additional cofactors such as streptococcus superantigens in the presence of H1N1 infections could also be important; AS03 is known to induce strong immune responses [76], while streptococcus superantigens generate polyclonal T cell responses. The generation and activation of these cross-reactive T cells could result in additional responses such as the local release of cytokines and chemokines that in turn recruits and activates other immune cells mediating hypocretin neuron damage and loss (for example cytotoxic CD8+cells or microglial cells). Antibody mediated dysregulation of hypocretin cells could also be involved, although as mentioned above autoantibodies have never been clearly identified beside TRIB2 in a small subset of cases. It is also possible that hypocretin cells may be unusually sensitive to some specific form of immune mediated cell killing.
Fig. 1.
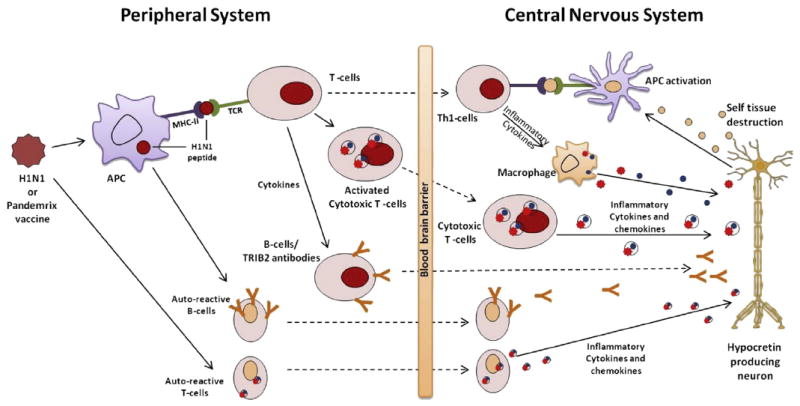
Possible pathway for a role of H1N1 seasonal infection and Pandemrix vaccination in onset of narcolepsy: the seasonal H1N1 influenza infection or the Pandemrix vaccine could stimulate auto-reactive T-cells or B-cells targeting towards hypocretin producing neurons via several different mechanisms. (i) Molecular mimicry of T-cells, it describes the activation of cross-reactive T-cells that recognize the H1N1 epitope and then the same T-cell (or a clone) migrates to the CNS, where it recognizes a antigen specific to hypocretin producing neurons (cross-reactivity). Activation of cross-reactive T cells results in release of cytokines and chemokines that recruits and activates macrophages, which mediates self-tissue damage. The subsequent release of hypocretin self antigen and their uptake by APCs perpetuate the autoimmune disease narcolepsy. (ii) H1N1 antigens or Pandemrix vaccine may cross-link the MHC and TCR molecules independent of antigen specificity and activates the cytotoxic T cells which are auto reactive and specific towards hypocretin producing neurons. (iii) Molecular mimicry involving B-cells and antibody mediated disease could also be involved, possibly targeting TRIB2 as a cross-reactive antigen. This process requires signals from activated T-cells (T-cell help). Bystander activation of resting auto-reactive B cells (iv) and T cells (v) as a result of general immune activation independent of specific antigens. Current results in narcolepsy research point towards a T-cell mechanism. APC: Antigen presenting cell; CNS: Central nervous system; H1N1: H1N1 influenza A virus or epitopes from adjuvant vaccines; MHC: Major histocompatibility complex; TCR: T-cell receptor; TRIB2: tribbles homologue 2.
1.7. Narcolepsy incidence in children
With some notable exceptions, such as celiac disease in infants and older children, autoimmune diseases affect children more rarely. In recent years, however, the number of children diagnosed with autoimmune disorders has been steadily climbing. It has also been established that children below the age of 10 and the elderly above 65 age groups have higher susceptibility to complications following seasonal infection, and a lower response to vaccination. Currently there is a great interest in understanding the connection between the 2009–2010 H1N1 pandemic seasons and the sharp increase in narcoleptic cases, especially in children. In China, the increased numbers of narcolepsy onset following the H1N1 influenza pandemic was reported in children [72]. The Scandinavian data also revealed that children who received Pandemrix that were born between January 1991 and December 2005 had narcolepsy rates of nine per 100,000, compared with 0.7 per 100,000 for unvaccinated children which is nearly 13 times higher [69]. No such increase was observed in adults, suggesting that children were more susceptible to developing narcolepsy following H1N1 exposure. To complicate matters further however, narcolepsy manifests differently in children versus adults, and the disease may be diagnosed later in older individuals whereas in children, the diagnosis is often easy with the onset of disease being clear.
What could explain these differences is unclear. In children, the immune system has the ability to respond to seasonal infections with a larger pool of naïve CD4+ and CD8+ T cells relative to adult that have a more mature and less plastic T-cell repertoire [77]. In addition, children have been shown to react differently to H1N1 infections both quantitatively and qualitatively. The fact cases following pH1N1 are mostly children suggests that the naive T cell pool and response in children is critical. The contribution of seasonal H1N1 or streptococcus infections along with genetic susceptibility might establish a population of T cells that are capable of recognizing self proteins which might be hypocretin related protein in the case of children developing narcolepsy.
2. Conclusions
In recent years, a growing number of autoimmune disorders affecting neurons in the central nervous system have been identified, although most are antibody mediated [78-80]. In addition to the specific targeting of the neurons, links between pathogenic inflammation and neuronal injury/cell death in models of CNS diseases such as Alzheimer’s disease, Parkinson’s disease and multiple sclerosis is providing additional information. Regarding narcolepsy, the disease does not meet Witebsky’s criteria but autoimmunity is extremely likely based on circumstantial evidence. First, narcolepsy has a strong genetic association with HLA DQB1*06:02 and a potential target for the autoimmune process, hypocretin cells. Second, Genome-wide association analysis also shows association with TCRα, P2RY11-DNMT1, CTSH and TNFSF4, consistent with an autoimmune basis. Finally, narcolepsy seemed triggered by upper airway infections, consistent with the suspected role of infections as a trigger of other autoimmune disorders. To understand narcolepsy, it will be important to understand how the immune targets neurons such as hypocretin producing cells, a process that we believe more likely to be T-cell mediated. However, the complex nature of central nervous system and the immune system presents unique challenges in finding a mechanism for the cause of narcolepsy.
References
- 1.Taheri S, Zeitzer JM, Mignot E. The role of hypocretins (orexins) in sleep regulation and narcolepsy. Annual Review of Neuroscience. 2002;25:283–313. doi: 10.1146/annurev.neuro.25.112701.142826. [DOI] [PubMed] [Google Scholar]
- 2.Okun ML, Lin L, Pelin Z, Hong S, Mignot E. Clinical aspects of narcolepsy-cataplexy across ethnic groups. Sleep. 2002;25:27–35. doi: 10.1093/sleep/25.1.27. [DOI] [PubMed] [Google Scholar]
- 3.Mohsenin V. Narcolepsy–master of disguise: evidence-based recommendations for management. Postgraduate Medicine. 2009;121:99–104. doi: 10.3810/pgm.2009.05.2008. [DOI] [PubMed] [Google Scholar]
- 4.Overeem S, Mignot E, van Dijk JG, Lammers GJ. Narcolepsy: clinical features, new pathophysiologic insights, and future perspectives. Journal of Clinical Neurophysiology: Official Publication of the American Electroencephalographic Society. 2001;18:78–105. doi: 10.1097/00004691-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Anic-Labat S, Guilleminault C, Kraemer HC, Meehan J, Arrigoni J, Mignot E. Validation of a cataplexy questionnaire in 983 sleep-disorders patients. Sleep. 1999;22:77–87. [PubMed] [Google Scholar]
- 6.Dauvilliers Y, Arnulf I, Mignot E. Narcolepsy with cataplexy. Lancet. 2007;369:499–511. doi: 10.1016/S0140-6736(07)60237-2. [DOI] [PubMed] [Google Scholar]
- 7.Aldrich MS. The neurobiology of narcolepsy-cataplexy syndrome. International Journal of Neurology. 1991:25–26. 29–40. [PubMed] [Google Scholar]
- 8.Nishino S, Kanbayashi T. Symptomatic narcolepsy, cataplexy and hypersomnia, and their implications in the hypothalamic hypocretin/orexin system. Sleep Medicine Reviews. 2005;9:269–310. doi: 10.1016/j.smrv.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 9.Mignot EJ. A practical guide to the therapy of narcolepsy and hypersomnia syndromes. Neurotherapeutics: The Journal of the American Society for Experimental NeuroTherapeutics. 2012;9:739–52. doi: 10.1007/s13311-012-0150-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Black J, Houghton WC. Sodium oxybate improves excessive daytime sleepiness in narcolepsy. Sleep. 2006;29:939–46. doi: 10.1093/sleep/29.7.939. [DOI] [PubMed] [Google Scholar]
- 11.Hogl B, Saletu M, Brandauer E, Glatzl S, Frauscher B, Seppi K, et al. Modafinil for the treatment of daytime sleepiness in Parkinson’s disease: a double-blind, randomized, crossover, placebo-controlled polygraphic trial. Sleep. 2002;25:905–9. [PubMed] [Google Scholar]
- 12.Mignot E, Nishino S. Emerging therapies in narcolepsy-cataplexy. Sleep. 2005;28:754–63. doi: 10.1093/sleep/28.6.754. [DOI] [PubMed] [Google Scholar]
- 13.Nishino S, Okuro M. Emerging treatments for narcolepsy and its related disorders. Expert Opinion on Emerging Drugs. 2010;15:139–58. doi: 10.1517/14728210903559852. [DOI] [PubMed] [Google Scholar]
- 14.Aldrich MS. The neurobiology of narcolepsy-cataplexy. Progress in Neurobiology. 1993;41:533–41. doi: 10.1016/0301-0082(93)90042-q. [DOI] [PubMed] [Google Scholar]
- 15.Aldrich MS. Diagnostic aspects of narcolepsy. Neurology. 1998;50:S2–7. doi: 10.1212/wnl.50.2_suppl_1.s2. [DOI] [PubMed] [Google Scholar]
- 16.Nishino S, Mignot E. Pharmacological aspects of human and canine narcolepsy. Progress in Neurobiology. 1997;52:27–78. doi: 10.1016/s0301-0082(96)00070-6. [DOI] [PubMed] [Google Scholar]
- 17.Hagan JJ, Leslie RA, Patel S, Evans ML, Wattam TA, Holmes S, et al. Orexin A activates locus coeruleus cell firing and increases arousal in the rat. Proceedings of the National Academy of Sciences of the United States of America. 1999;96:10911–6. doi: 10.1073/pnas.96.19.10911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sutcliffe JG, de Lecea L. The hypocretins: excitatory neuromodulatory peptides for multiple homeostatic systems, including sleep and feeding. Journal of Neuroscience Research. 2000;62:161–8. doi: 10.1002/1097-4547(20001015)62:2<161::AID-JNR1>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 19.Brown RE, Sergeeva O, Eriksson KS, Haas HL. Orexin A excites serotonergic neurons in the dorsal raphe nucleus of the rat. Neuropharmacology. 2001;40:457–9. doi: 10.1016/s0028-3908(00)00178-7. [DOI] [PubMed] [Google Scholar]
- 20.Shibata M, Mondal MS, Date Y, Nakazato M, Suzuki H, Ueta Y. Distribution of orexins-containing fibers and contents of orexins in the rat olfactory bulb. Neuroscience Research. 2008;61:99–105. doi: 10.1016/j.neures.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 21.Thorpy M. Therapeutic advances in narcolepsy. Sleep Medicine. 2007;8:427–40. doi: 10.1016/j.sleep.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 22.Jones BE. Modulation of cortical activation and behavioral arousal by cholinergic and orexinergic systems. Annals of the New York Academy of Sciences. 2008;1129:26–34. doi: 10.1196/annals.1417.026. [DOI] [PubMed] [Google Scholar]
- 23.Foutz AS, Mitler MM, Cavalli-Sforza LL, Dement WC. Genetic factors in canine narcolepsy. Sleep. 1979;1:413–21. doi: 10.1093/sleep/1.4.413. [DOI] [PubMed] [Google Scholar]
- 24.Lin L, Faraco J, Li R, Kadotani H, Rogers W, Lin X, et al. The sleep disorder canine narcolepsy is caused by a mutation in the hypocretin (orexin) receptor 2 gene. Cell. 1999;98:365–76. doi: 10.1016/s0092-8674(00)81965-0. [DOI] [PubMed] [Google Scholar]
- 25.Nishino S, Ripley B, Overeem S, Lammers GJ, Mignot E. Hypocretin (orexin) deficiency in human narcolepsy. Lancet. 2000;355:39–40. doi: 10.1016/S0140-6736(99)05582-8. [DOI] [PubMed] [Google Scholar]
- 26.Thannickal TC, Moore RY, Nienhuis R, Ramanathan L, Gulyani S, Aldrich M, et al. Reduced number of hypocretin neurons in human narcolepsy. Neuron. 2000;27:469–74. doi: 10.1016/s0896-6273(00)00058-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peyron C, Faraco J, Rogers W, Ripley B, Overeem S, Charnay Y, et al. A mutation in a case of early onset narcolepsy and a generalized absence of hypocretin peptides in human narcoleptic brains. Nature Medicine. 2000;6:991–7. doi: 10.1038/79690. [DOI] [PubMed] [Google Scholar]
- 28.Thannickal TC, Nienhuis R, Siegel JM. Localized loss of hypocretin (orexin) cells in narcolepsy without cataplexy. Sleep. 2009;32:993–8. doi: 10.1093/sleep/32.8.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Horton R, Wilming L, Rand V, Lovering RC, Bruford EA, Khodiyar VK, et al. Gene map of the extended human MHC. Nature Reviews Genetics. 2004;5:889–99. doi: 10.1038/nrg1489. [DOI] [PubMed] [Google Scholar]
- 30.Shiina T, Inoko H, Kulski JK. An update of the HLA genomic region, locus information and disease associations: 2004. Tissue Antigens. 2004;64:631–49. doi: 10.1111/j.1399-0039.2004.00327.x. [DOI] [PubMed] [Google Scholar]
- 31.Gabriel SB, Schaffner SF, Nguyen H, Moore JM, Roy J, Blumenstiel B, et al. The structure of haplotype blocks in the human genome. Science. 2002;296:2225–9. doi: 10.1126/science.1069424. [DOI] [PubMed] [Google Scholar]
- 32.Singal DP, Blajchman MA. Histocompatibility (HL-A) antigens, lymphocyto-toxic antibodies and tissue antibodies in patients with diabetes mellitus. Diabetes. 1973;22:429–32. doi: 10.2337/diab.22.6.429. [DOI] [PubMed] [Google Scholar]
- 33.Dorman JS, Bunker CH. HLA-DQ locus of the human leukocyte antigen complex and type 1 diabetes mellitus: a HuGE review. Epidemiologic Reviews. 2000;22:218–27. doi: 10.1093/oxfordjournals.epirev.a018034. [DOI] [PubMed] [Google Scholar]
- 34.van der Horst-Bruinsma IE, Visser H, Hazes JM, Breedveld FC, Verduyn W, Schreuder GM, et al. HLA-DQ-associated predisposition to and dominant HLA-DR-associated protection against rheumatoid arthritis. Human Immunology. 1999;60:152–8. doi: 10.1016/s0198-8859(98)00101-3. [DOI] [PubMed] [Google Scholar]
- 35.Newton JL, Harney SM, Wordsworth BP, Brown MA. A review of the MHC genetics of rheumatoid arthritis. Genes and Immunity. 2004;5:151–7. doi: 10.1038/sj.gene.6364045. [DOI] [PubMed] [Google Scholar]
- 36.Simmonds MJ, Howson JM, Heward JM, Carr-Smith J, Franklyn JA, Todd JA, et al. A novel and major association of HLA-C in Graves’ disease that eclipses the classical HLA-DRB1 effect. Human Molecular Genetics. 2007;16:2149–53. doi: 10.1093/hmg/ddm165. [DOI] [PubMed] [Google Scholar]
- 37.Langdon N, Shindler J, Parkes JD, Bandak S. Fluoxetine in the treatment of cataplexy. Sleep. 1986;9:371–3. doi: 10.1093/sleep/9.2.371. [DOI] [PubMed] [Google Scholar]
- 38.Mignot E. Genetics of narcolepsy and other sleep disorders. American Journal of Human Genetics. 1997;60:1289–302. doi: 10.1086/515487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mignot E, Lin X, Arrigoni J, Macaubas C, Olive F, Hallmayer J, et al. DQB1*0602 and DQA1*0102 (DQ1) are better markers than DR2 for narcolepsy in Caucasian and black Americans. Sleep. 1994;17:S60–7. doi: 10.1093/sleep/17.suppl_8.s60. [DOI] [PubMed] [Google Scholar]
- 40.Rogers AE, Meehan J, Guilleminault C, Grumet FC, Mignot E. HLA DR15 (DR2) and DQB1*0602 typing studies in 188 narcoleptic patients with cataplexy. Neurology. 1997;48:1550–6. doi: 10.1212/wnl.48.6.1550. [DOI] [PubMed] [Google Scholar]
- 41.Mignot E, Lin L, Rogers W, Honda Y, Qiu X, Lin X, et al. Complex HLA-DR and -DQ interactions confer risk of narcolepsy-cataplexy in three ethnic groups. American Journal of Human Genetics. 2001;68:686–99. doi: 10.1086/318799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hor H, Kutalik Z, Dauvilliers Y, Valsesia A, Lammers GJ, Donjacour CE, et al. Genome-wide association study identifies new HLA class II haplotypes strongly protective against narcolepsy. Nature Genetics. 2010;42:786–9. doi: 10.1038/ng.647. [DOI] [PubMed] [Google Scholar]
- 43.Mignot E. Genetic and familial aspects of narcolepsy. Neurology. 1998;50:S16–22. doi: 10.1212/wnl.50.2_suppl_1.s16. [DOI] [PubMed] [Google Scholar]
- 44.Hong SC, Lin L, Jeong JH, Shin YK, Han JH, Lee JH, et al. A study of the diagnostic utility of HLA typing, CSF hypocretin-1 measurements, and MSLT testing for the diagnosis of narcolepsy in 163 Korean patients with unexplained excessive daytime sleepiness. Sleep. 2006;29:1429–38. doi: 10.1093/sleep/29.11.1429. [DOI] [PubMed] [Google Scholar]
- 45.Lin L, Hungs M, Mignot E. Narcolepsy and the HLA region. Journal of Neuroimmunology. 2001;117:9–20. doi: 10.1016/s0165-5728(01)00333-2. [DOI] [PubMed] [Google Scholar]
- 46.Tafti M, Maret S, Dauvilliers Y. Genes for normal sleep and sleep disorders. Annals of Medicine. 2005;37:580–9. doi: 10.1080/07853890500372047. [DOI] [PubMed] [Google Scholar]
- 47.Dauvilliers Y, Maret S, Tafti M. Genetics of normal and pathological sleep in humans. Sleep Medicine Reviews. 2005;9:91–100. doi: 10.1016/j.smrv.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 48.Singh SM, George CF, Kryger MH, Jung JH. Genetic heterogeneity in narcolepsy. Lancet. 1990;335:726–7. doi: 10.1016/0140-6736(90)90842-s. [DOI] [PubMed] [Google Scholar]
- 49.Hallmayer J, Faraco J, Lin L, Hesselson S, Winkelmann J, Kawashima M, et al. Narcolepsy is strongly associated with the T-cell receptor alpha locus. Nature Genetics. 2009;41:708–11. doi: 10.1038/ng.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Petrie HT, Livak F, Burtrum D, Mazel S. T cell receptor gene recombination patterns and mechanisms: cell death, rescue, and T cell production. The Journal of Experimental Medicine. 1995;182:121–7. doi: 10.1084/jem.182.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kornum BR, Kawashima M, Faraco J, Lin L, Rico TJ, Hesselson S, et al. Common variants in P2RY11 are associated with narcolepsy. Nature Genetics. 2011;43:66–71. doi: 10.1038/ng.734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Winkelmann J, Lin L, Schormair B, Kornum BR, Faraco J, Plazzi G, et al. Mutations in DNMT1 cause autosomal dominant cerebellar ataxia, deafness and narcolepsy. Human Molecular Genetics. 2012;21:2205–10. doi: 10.1093/hmg/dds035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Josefowicz SZ, Wilson CB, Rudensky AY. Cutting edge: TCR stimulation is sufficient for induction of Foxp3 expression in the absence of DNA methyl-transferase 1. Journal of Immunology. 2009;182:6648–52. doi: 10.4049/jimmunol.0803320. [DOI] [PubMed] [Google Scholar]
- 54.Faraco JLL, Kornum BR, Kenny EE, Trynka G, Einen M, et al. ImmunoChip study implicates antigen presentation to T cells in narcolepsy. PLOS Genetics. doi: 10.1371/journal.pgen.1003270. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rose NR, Bona C. Defining criteria for autoimmune diseases (Witebsky’s postulates revisited) Immunology Today. 1993;14:426–30. doi: 10.1016/0167-5699(93)90244-F. [DOI] [PubMed] [Google Scholar]
- 56.Graus F, Saiz A, Dalmau J. Antibodies and neuronal autoimmune disorders of the CNS. Journal of Neurology. 2010;257:509–17. doi: 10.1007/s00415-009-5431-9. [DOI] [PubMed] [Google Scholar]
- 57.Aran A, Lin L, Nevsimalova S, Plazzi G, Hong SC, Weiner K, et al. Elevated anti-streptococcal antibodies in patients with recent narcolepsy onset. Sleep. 2009;32:979–83. doi: 10.1093/sleep/32.8.979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tanaka S, Honda M. IgG abnormality in narcolepsy and idiopathic hypersomnia. PloS One. 2010;5:e9555. doi: 10.1371/journal.pone.0009555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cvetkovic-Lopes V, Bayer L, Dorsaz S, Maret S, Pradervand S, Dauvilliers Y, et al. Elevated tribbles homolog 2-specific antibody levels in narcolepsy patients. The Journal of Clinical Investigation. 2010;120:713–9. doi: 10.1172/JCI41366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kawashima M, Lin L, Tanaka S, Jennum P, Knudsen S, Nevsimalova S, et al. Anti-tribbles homolog 2 (TRIB2) autoantibodies in narcolepsy are associated with recent onset of cataplexy. Sleep. 2010;33:869–74. doi: 10.1093/sleep/33.7.869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sung HY, Francis SE, Crossman DC, Kiss-Toth E. Regulation of expression and signalling modulator function of mammalian tribbles is cell-type specific. Immunology Letters. 2006;104:171–7. doi: 10.1016/j.imlet.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 62.Eder K, Guan H, Sung HY, Ward J, Angyal A, Janas M, et al. Tribbles-2 is a novel regulator of inflammatory activation of monocytes. International Immunology. 2008;20:1543–50. doi: 10.1093/intimm/dxn116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dalal J, Roh JH, Maloney SE, Akuffo A, Shah S, Yuan H, et al. Translational profiling of hypocretin neurons identifies candidate molecules for sleep regulation. Genes and Development. 2013 doi: 10.1101/gad.207654.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dauvilliers Y, Montplaisir J, Cochen V, Desautels A, Einen M, Lin L, et al. Post-H1N1 narcolepsy-cataplexy. Sleep. 2010;33:1428–30. doi: 10.1093/sleep/33.11.1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Black JL, 3rd, Silber MH, Krahn LE, Avula RK, Walker DL, Pankratz VS, et al. Studies of humoral immunity to preprohypocretin in human leukocyte antigen DQB1*0602-positive narcoleptic subjects with cataplexy. Biological Psychiatry. 2005;58:504–9. doi: 10.1016/j.biopsych.2005.04.026. [DOI] [PubMed] [Google Scholar]
- 66.Black JL, 3rd, Silber MH, Krahn LE, Fredrickson PA, Pankratz VS, Avula R, et al. Analysis of hypocretin (orexin) antibodies in patients with narcolepsy. Sleep. 2005;28:427–31. doi: 10.1093/sleep/28.4.427. [DOI] [PubMed] [Google Scholar]
- 67.Tanaka S, Honda Y, Inoue Y, Honda M. Detection of autoantibodies against hypocretin, hcrtrl, and hcrtr2 in narcolepsy: anti-Hcrt system antibody in narcolepsy. Sleep. 2006;29:633–8. doi: 10.1093/sleep/29.5.633. [DOI] [PubMed] [Google Scholar]
- 68.Smith AJ, Jackson MW, Neufing P, McEvoy RD, Gordon TP. A functional autoantibody in narcolepsy. Lancet. 2004;364:2122–4. doi: 10.1016/S0140-6736(04)17553-3. [DOI] [PubMed] [Google Scholar]
- 69.Nohynek H, Jokinen J, Partinen M, Vaarala O, Kirjavainen T, Sundman J, et al. AS03 adjuvanted AH1N1 vaccine associated with an abrupt increase in the incidence of childhood narcolepsy in Finland. PloS One. 2012;7:e33536. doi: 10.1371/journal.pone.0033536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kwok R. Vaccines: the real issues in vaccine safety. Nature. 2011;473:436–8. doi: 10.1038/473436a. [DOI] [PubMed] [Google Scholar]
- 71.European Centre for Disease Prevention and Control (ECDC) VAESCO investigation into narcolepsy. 2012 Mar; http://wwwecdceuropaeu/en/activities/sciadvice/Lists/ECDC%20Reviews/ECDC_DispFormaspx?List¼512ff74f-77d4-4ad8-b6d6-bf0f23083f30&ID=14;1017.
- 72.Han F, Lin L, Warby SC, Faraco J, Li J, Dong SX, et al. Narcolepsy onset is seasonal and increased following the 2009 H1N1 pandemic in China. Annals of Neurology. 2011;70:410–7. doi: 10.1002/ana.22587. [DOI] [PubMed] [Google Scholar]
- 73.Choe YJ, Bae GR, Lee DH. No association between influenza A(H1N1)pdm09 vaccination and narcolepsy in South Korea: an ecological study. Vaccine. 2012 doi: 10.1016/j.vaccine.2012.10.030. [DOI] [PubMed] [Google Scholar]
- 74.Matsuki K, Honda Y, Naohara T, Satake M, Someya T, Harada S, et al. Lymphocyte subsets in HLA-DR2-positive narcoleptic patients. Folia Psychiatrica et Neurologica Japonica. 1985;39:499–505. doi: 10.1111/j.1440-1819.1985.tb00803.x. [DOI] [PubMed] [Google Scholar]
- 75.Hinze-Selch D, Wetter TC, Zhang Y, Lu HC, Albert ED, Mullington J, et al. In vivo and in vitro immune variables in patients with narcolepsy and HLA-DR2 matched controls. Neurology. 1998;50:1149–52. doi: 10.1212/wnl.50.4.1149. [DOI] [PubMed] [Google Scholar]
- 76.Morel S, Didierlaurent A, Bourguignon P, Delhaye S, Baras B, Jacob V, et al. Adjuvant system AS03 containing alpha-tocopherol modulates innate immune response and leads to improved adaptive immunity. Vaccine. 2011;29:2461–73. doi: 10.1016/j.vaccine.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 77.Unutmaz D, Pileri P, Abrignani S. Antigen-independent activation of naive and memory resting T cells by a cytokine combination. The Journal of Experimental Medicine. 1994;180:1159–64. doi: 10.1084/jem.180.3.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Posner JB, Dalmau JO. Paraneoplastic syndromes affecting the central nervous system. Annual Review of Medicine. 1997;48:157–66. doi: 10.1146/annurev.med.48.1.157. [DOI] [PubMed] [Google Scholar]
- 79.Bataller L, Dalmau JO. Paraneoplastic disorders of the central nervous system: update on diagnostic criteria and treatment. Seminars in Neurology. 2004;24:461–71. doi: 10.1055/s-2004-861540. [DOI] [PubMed] [Google Scholar]
- 80.Posner JB, Dalmau JO. Yet another paraneoplastic antibody. Annals of Neurology. 2001;49:141–2. doi: 10.1002/1531-8249(20010201)49:2<141::aid-ana31>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]


