Abstract
Along with upper airway cough syndrome (formerly, postnasal drip syndrome) and eosinophilic airway inflammation (asthma, non-asthmatic eosinophilic bronchitis), gastroesophageal reflux disease (GERD) is generally considered among the most common etiologies of chronic cough. Indeed, cough management guidelines published by numerous respiratory societies worldwide recommend evaluation and treatment of GERD as an integral component of the diagnostic/therapeutic algorithm for the management of chronic cough. However, a significant number of patients with chronic cough presumed due to GERD do not report improvement despite aggressive acid-suppressive therapy. Some of these refractory cases may be due to the recently appreciated entity of non-acid or weakly acidic reflux. Further contributing to the controversy are recent studies demonstrating that patients with chronic cough do not have excessive reflux events relative to healthy volunteers. Although a temporal relationship between cough and reflux events has been suggested by studies utilizing impedance-pH monitoring of reflux events and objective cough recording, consensus is lacking in terms of whether this temporal relationship proves a causal link between reflux and cough. The 4th American Cough Conference, held in New York in June, 2013, provided an ideal forum for the debate of this issue between two internationally recognized experts in the field of reflux and chronic cough.
Keywords: gastroesophageal reflux disease, cough, pH monitoring, impedance-pH monitoring, proton pump inhibitors, reflux testing, esophagus
Introduction
Multiple prospective studies have demonstrated that gastroesophageal reflux disease (GERD) is among the most common etiologies of chronic cough [1,2]. However, despite the availability of effective acid-suppressing agents, a significant percentage of patients with chronic cough presumed due to GERD prove refractory to seemingly appropriate therapy. Indeed, multiple studies and meta-analyses have failed to document a therapeutic effect of proton-pump inhibitors (PPIs) and histamine-2 receptor antagonists for chronic cough associated with GERD [3–5]. The ability of anti-reflux surgery [6] and prokinetic agents such as metaclopramide [7] to ameliorate cough that had not improved despite acid suppression raised awareness that some cases of chronic cough are due to non-acid or weakly acidic refluxate. These and other observations have thus called into question the importance of acid reflux and GERD in general as an etiologic factor in chronic cough.
The 4th American Cough Conference, which took place in New York City, June 7–8, 2013, provided an ideal venue for discussion and debate on this topic. Professor Peter Kahrilas of the Northwestern University Feinberg School of Medicine argued in favor of a causal relationship between GERD and chronic cough, whereas Dr. Jaclyn Smith of the University of Manchester, UK, defended the opposing view. The following is a summary of the debate that occurred in front of an audience of clinicians and investigators who all share an interest in the field of cough.
Peter J. Kahrilas for the Motion
The Montreal definition defines gastroesophageal reflux disease (GERD) as inclusive of all conditions in which the reflux of stomach contents causes troublesome symptoms and/or complications; reflux-cough syndrome is one such condition [8]. Large population-based surveys have demonstrated an increased risk of several ENT and pulmonary symptoms among patients with either esophagitis or reflux symptoms [9–11]. The reported odds ratios for having laryngeal or pulmonary conditions among GERD patients in these studies range from 1.2 to 3.0, with nocturnal cough having the strongest association. However, for a number of reasons it is far from straightforward to establish the causality of gastroesophageal reflux (GER) as the cause of refractory chronic cough in a clinical scenario. Hence, estimates of the proportion of chronic cough cases with GER as the underlying pathogenesis vary widely (0–40%) among specialty centers [2]. Part of the explanation for that is in not fully appreciating that cough can have multiple etiologies in an individual patient, with GER being but one of them.
Establishing causality is more difficult than establishing association, which simply explores the co-occurrence of phenomena. Within the framework of evidence-based-medicine [12] the criteria for causation for reflux causing cough would be: 1) that reflux precede the onset of cough; 2) the demonstration of a dose-response relationship between reflux and cough; 3) demonstration that the association between reflux and cough makes biological sense; 4) demonstration of a consistent association between reflux and cough among studies; and 5) supportive evidence from GERD treatment trials aimed at relieving cough. Although item #1 makes sense, it is difficult to apply in the case of reflux-cough. Reflux can be a normal physiological event, can be caused by cough, and it is generally difficult to establish the threshold at which it becomes a ‘disease’ as opposed to an episodic occurrence. As for item #2, this ignores the phenomenon of hypersensitivity. Somewhat paradoxically, in many instances, the worse the reflux disease, the less sensitive the individual to episodes of reflux. Patients with severe reflux, manifest as Barrett’s esophagus and peptic stricture often report only modest heartburn. On the other hand, patients with nonerosive reflux disease generally report experiencing more severe heartburn than patients with esophagitis. This leaves items #3, #4, and #5; that the reflux cough association make biological sense, that the association between reflux and cough be consistent among trials, and that there be supportive evidence of the association from GERD treatment trials aimed at relieving cough. Each of these criteria will be explored in turn.
Physiology of the reflux cough association
Alternative hypotheses for the mechanism wherein reflux might cause cough are by stimulation of a vagal esophageal-bronchial reflex or by regurgitation, with or without aspiration. In the first case this would be a manifestation of hypersensitivity while in the second, cough might be one of a number of reflux laryngitis symptoms or a consequence of ‘microaspiration’. Evidence can be found supporting each of these mechanisms.
Physiological studies have examined the effect of intra-esophageal acid infusion in suspected reflux-cough patients with varied results. Ing et al. found that cough frequency was acutely increased by 15 minutes of acid infusion in 22 suspected reflux-cough patients, but not in 12 control subjects [13]. Interestingly, saline infusion also significantly increased the cough frequency in about half of the patients but to a much lesser degree than did acid. In a similar experiment with 12 reflux-cough patients, Irwin had contradictory findings, instead showing no acute change in cough frequency when alternating between acid and saline infusion [14]. However, cough frequency was probably not the optimal outcome measure for these proof-of-principle experiments and more recent investigations have instead focused on the concept of cough sensitivity, determined by tussigenic challenges with agent such as capsaicin or citric acid. The irritative substances are delivered by nebulizer, sequentially doubling the concentration until the individual coughs at least two (C2) or five times (C5) in the 15 seconds after inhalation of a test concentration [15]. Applying such methodology, Javorka et al [16] was able to show that intra-esophageal acid infusion significantly sensitized the cough reflex in patients with chronic cough and asthma. However, acid infusion only increased cough reflex sensitivity in patients with objective evidence of GERD (endoscopic or pH-metry) and airway disease, not if reflux patients without airway disease or healthy controls suggesting that both pathologies were prerequisite.
The alternative physiological mechanism for reflux-cough causation is regurgitation or ‘microaspiration’. However, for all that has been written about it, evidence in support of these as causal mechanisms is less robust that that supporting a reflexive mechanism. Refluxate containing acid and pepsin reaching the larynx and pharynx is often referred to as laryngopharyngeal reflux (LPR) and is frequently invoked as a cause of chronic laryngitis with a spectrum of symptoms, including cough. LPR is usually diagnosed on the basis of laryngoscopic findings, but these signs show poor specificity for reflux when tested in a blinded fashion [17] and may even be the result of the trauma of chronic coughing [18]. An alternative diagnostic approach is to monitor reflux reaching the larynx or pharynx with either pH-metry or combined pH-impedance metry. However, this too is unlikely to have much diagnostic utility given that even though refluxate occasionally reaches the pharynx in chronic cough patients (mean, 2 per 24 hours) [19], it does so no more frequently than what is observed in healthy controls [20]. As for ‘microaspiration’, the concept is that minute amounts of gastric acid, enzymes, and/or bile aspirated into the airway are the root cause of chronic irritation leading to cough. Implicit in this model, is that even trace amounts of these substance in the airway represent an abnormality. However, this proves not to be the case. Controlled observations have found that airway pepsin concentrations in bronchoalveolar lavage samples taken from chronic cough patients are no different from those in healthy volunteers [21]. On the other hand, sputum pepsin concentrations were weakly correlated with the number of proximal reflux events (r = 0.33, P = .045) and inversely related to cough frequency (r = −0.52, P = .04), suggesting that coughing appears to be a protective mechanism, clearing pepsin from large airways of chronic cough patients. Also supportive of this construct, a recent prospective study of 51 otherwise healthy adult patients undergoing elective orthopedic surgery quantified lower airway pepsin concentrations in samples obtained immediately following endotracheal intubation and found enzymatically active pepsin C (but not pepsin A) in 22% of them [22]. Pepsin C can be expressed by pneumocytes whereas pepsin A is exclusive to the stomach; most publications on the subject do not distinguish between these isoforms.
Temporal association between reflux and cough
Both reflux and cough are discreet events and if reflux were causing cough, one would anticipate some degree of temporal association between the two. Hence the diagnostic approach of prolonged (24 hr or more) reflux and cough monitoring and examining the co-occurrence of events. It sounds simple, but of course it is quite complex. Early studies seeking to establish reflux-cough correlation required that patients press an event marker each time they coughed, as is done when associating symptoms such as heartburn or chest pain with reflux events. However, in contrast to heartburn or chest pain, several hundred coughs may occur over a 24-h period in patients with chronic cough, making this task inherently difficult and inaccurate. The high frequency of coughing also increases the probability of chance association with reflux events making it absolutely mandatory to establish statistically significant reflux-cough association with an index such as the symptom association probability (SAP) as opposed to the symptom index (SI) that might suffice for an infrequent symptom [23]. Hence it is easy to find fault in these early studies [14, 24–26] on methodological grounds.
Two technological enhancements have vastly improved our ability to correlate cough with reflux during physiological testing: use of impedance-pH monitoring to detect all reflux events irrespective of pH and the use of a physiological signal (manometry or microphone) to detect and time the occurrence of coughs. Together with use of the SAP, these technologies greatly improve the objectivity of the analysis. All recent studies utilizing one or another variation of these enhancements have consistently demonstrated that in a substantial proportion of chronic cough patients (20–48%) cough follows reflux more frequently than expected by chance [27–31]. Furthermore, the pH of the reflux events preceding cough does not matter; reflux events of pH> 4 are equally important as those with pH italic>4 [30–31]. The most sophisticated and convincing of these studies (ironically published by my antagonist in this debate) enrolled chronic cough patients irrespective of concomitant diagnoses that might also explain cough and utilized acoustic monitoring coupled with computer analysis to detect coughs [30]. These investigators found the strongest reflux-cough association of all of the studies (48%) and were also able to show the reverse correlation, that cough prompted reflux. When cough did prompt reflux, it did so outside of the 10-second window that might be attributable to the abdominal strain associated with coughing. Hence, the developing hypothesis is that reflux-cough patients exhibit hypersensitivity of both the airway, demonstrable by tussive challenges and the esophagus, manifest by sensitivity to weakly acidic reflux and likely the triggering of transient lower esophageal sphincter relaxations.
GERD treatment trials aimed at relieving cough
Evident from the discussion up to this point, the relationship between gastroesophageal reflux and chronic cough is particularly complex with the influences of other disease processes, issues of cause and effect, and hypersensitivity all coming into play. Consequently, relevant treatment trials aimed at relieving cough with GERD treatment have been a heterogeneous lot, employing a wide variety of patient selection criteria and outcome measures. The only thing held relatively constant among the trials was the treatment; high dose proton pump inhibitors (PPIs). Hence, it is not entirely surprising that a recent Cochrane review and a meta-analysis found insufficient evidence to conclude that PPI treatment is beneficial in treating nonspecific chronic cough [32–33]. The irony of this is the substantial uncontrolled data, well summarized in the American College of Chest Physicians 2006 Practice Guidelines [1], suggesting efficacy of diet, antacids, histamine-2 receptor antagonists, prokinetics, PPIs, and antireflux surgery in improving or curing reflux cough syndrome.
Seeking to reconcile the contradiction between clinical wisdom and controlled trials, a recent systematic review re-explored GERD-cough treatment trials with a focus on relating study outcomes to whether or not the patients studied had objective evidence of GERD [34]. Although this may seem rather obvious, it was, in fact, one of the most variable of inclusion criteria among studies. The analysis found that of the nine placebo controlled, randomized clinical trials identified, only two reported a statistically significant reduction in cough frequency and/or severity after pharmacologic acid suppressive therapy. However, in six [5,25, 35–37] of the seven datasets in which the therapeutic gain of PPI vs placebo could be calculated, the PPI treatment effect was greater. Furthermore, the only dataset demonstrating no therapeutic gain was from a study that intentionally enrolled patients with normal esophageal pH-metry [38]. When the therapeutic gain data from these trials were segregated according to the pH-metry characteristics of the patients included, response was greater in patient subsets with pathologic esophageal acid exposure (range, 12.5%–35.8%) than in those without (range, 0.0%–8.6%) (Figure 1).
Figure 1.
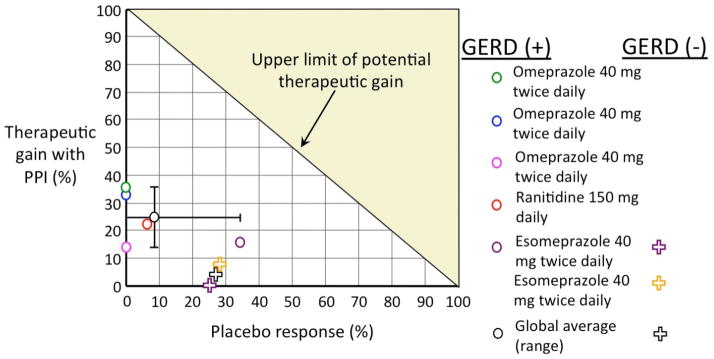
Calculated therapeutic gain (acid suppressive therapy minus placebo response) in improving chronic cough for datasets derived from patients with pathologic esophageal acid exposure (GERD +) defined by 24 hour pH-metry and populations including patients with normal esophageal acid exposure (GERD −). From Kahrilas PJ, et al. Chest 2013;143:605–12, with permission (ref. 34).
Accepting that PPI therapy does benefit patients with chronic cough, one must concede that the therapeutic gain is modest at best. Again, hypersensitivity and the cough-evoking potential of reflux irrespective of pH are likely explanations for this. The apparent success of antireflux surgery in treating patients with chronic cough refractory to PPI therapy, albeit in uncontrolled trials, also supports these concepts. Antireflux surgery is potentially more effective than PPI therapy in chronic cough patients, as both acid and weakly acidic reflux are reduced. A recent retrospective analysis concluded that this was particularly true in patients with concomitant heartburn or >12% esophageal acid exposure on pH-metry [39]. However, among the many studies reporting benefit in reduced chronic cough after antireflux surgery [40–46] none were placebo controlled, which is essential for a condition that tends to resolve spontaneously over time.
Conclusions: putting it all together
The relationship between reflux and chronic cough is far from straightforward because data do not exist to meet all evidence-based-medicine criteria for causation: that exposure precede the onset of cough (no); demonstration of a dose-response relationship (no); demonstration that the association makes biological sense (yes); demonstration of a consistent association among studies (yes, when the studies are well done); supportive evidence from treatment trials (yes, but not robust). Most relevant to the clinical scenario are treatment data and having a reliable test or algorithm for detection of affected patients. Neither is robust in the case of reflux-cough. Evidence of the efficacy of using proton pump inhibitors for treating cough is scant, but there is a hint of efficacy if one examines those data for patients with objective evidence of GERD (endoscopy of physiological monitoring). Uncontrolled data also support the efficacy of antireflux surgery in treating chronic cough. Furthermore, evidence of hypersensitivity is ever-expanding; both with respect to the esophagus and to the cough reflex itself. When the influence of hypersensitivity is accounted for, studies suggest that 40% of chronic cough patients have a relevant reflux-cough association. Hence, in all likelihood, GER is a cause of chronic cough, but there are a number of important caveats: 1) the likely mechanism is a vagal reflex rather than ‘microaspiration’; 2) hypersensitivity is an important mechanism; 3) many affected patients have few esophageal GER symptoms; and 5) PPI trials are an insensitive method of establishing GER causality.
Jaclyn A. Smith against the Motion
An association between gastroesophageal reflux disease and chronic cough has long been recognized, however such an association may just reflect that these conditions tend to affect a similar population and does not necessarily imply causality. Current evidence suggests that patients with chronic cough do not have excessive intra- or extra- esophageal reflux. Whilst studies have found reflux events tend to be linked in time to cough in up to 50% of patients, such temporal associations do not provide strong evidence of causality. Well-designed controlled trials demonstrating that reducing reflux events, through either medical or surgical intervention, reduces coughing are currently lacking, hence a causal relationship has not yet been established.
Potential Mechanisms Linking Reflux to Cough
Reflux events potentially trigger coughing through three main mechanisms:
Microaspiration of refluxate into the airways
Extension of reflux into the larynx and pharynx (laryngo-pharyngeal reflux)
An ‘esophageal bronchial reflex’
There are technical challenges in accurately measuring pepsin and bile acids in airway samples [47]. To date, three studies have investigated biochemical markers of refluxate in samples from patients with chronic cough and compared them to healthy controls [21,48,49]. Irrespective of whether these studies collected broncho-alveolar lavage fluid or induced sputum, measured levels of pepsin or bile acids, none have suggested significant differences between patients with chronic cough and controls. This would suggest micro-aspiration of refluxate is unlikely to play an important role in chronic cough.
The accurate measurement of refluxate in the larynx and pharynx is extremely difficult and therefore there is little convincing evidence that excessive laryngopharyngeal reflux is important in chronic cough. Standard pH electrodes tend to dry out in the larynx/pharynx and therefore do not function. Impedance measurements demonstrate a highly variable baseline, causing very poor agreement in reporting of pharyngeal reflux events, even amongst expert reviewers [50]. Studies investigating pharyngeal reflux in patients with chronic cough are therefore likely to be unreliable [19,51]. Recently, a new type of pH electrode has been developed, designed specifically to function in the pharynx and to detect aerosolised and liquid acid reflux events. Some initial evaluations comparing this system with simultaneous esophageal impedance monitoring have been disappointing however, suggesting a significant proportion of pharyngeal events detected (up to 35%) represent swallowing [52] and that there is poor agreement between acid reflux events within the esophagus and pH changes in the pharynx [53].
So, currently there is little evidence to suggest extra-esophageal reflux is an important factor in chronic cough. The most compelling evidence that reflux may cause coughing comes from studies investigating intra-esophageal reflux events, which can be accurately assessed.
Intra-esophageal Reflux and Cough
Several investigators have quantified the nature of gastro-esophageal reflux events using esophageal pH/impedance monitoring in patients presenting with chronic cough. Such studies seem to agree that the number and acidity of reflux events measured by esophageal impedance is comparable to that in healthy controls, irrespective of whether unselected subjects are studied [21] or those in whom other causes of cough have been excluded [27,28]. Therefore as a group, chronic cough patients seem to exhibit physiological amounts of reflux.
However when the precise timing of cough and reflux events has been interrogated, up to 48% of patients with chronic cough display significant temporal associations (positive symptom association probability), with reflux events preceding cough more frequently than would be expected by chance alone [27–31]. These associations have been described for reflux events in the distal esophagus and therefore support the notion that a neuronal mechanism might explain the link between reflux and cough events. However, there are unanswered methodological questions with these studies, for example, what the optimal time window should be to classify events as associated and whether the statistical analyses used are the most appropriate. Moreover, an association in time does not confirm causality. Greater confidence that reflux events can trigger coughing will only be achieved when it has been shown that blocking reflux events directly impacts upon the number of cough events.
Evidence from Interventions for Reflux in Chronic Cough Patients
Proton Pump Inhibitors
Given the observation that chronic cough patients on average do not exhibit excessive acid reflux, it is perhaps unsurprising that randomized controlled trials of proton pump inhibitors have been largely disappointing [3]. One retrospective analysis of previous studies has suggested that there could be a sub-group of responders amongst patients with higher levels of esophageal acid exposure [34]. Few of these studies used validated measures of cough however, and so there is a concern that such a finding may be confounded by an improvement in more typical symptoms associated with excessive esophageal acid such as heartburn. Adequately powered and appropriately designed prospective studies with validated measures of cough are needed in order to establish whether such responders truly exist.
Laparoscopic Fundoplication
Data from studies of patients with typical reflux symptoms demonstrate that laparoscopic fundoplication is highly effective in reducing the numbers of reflux events detected by pH/impedance [54] and produces symptomatic improvement comparable to PPI treatment [55]. Responses are poorer in patients with atypical symptoms, normal acid exposure and symptoms refractory to PPI treatment [56]. Unfortunately the quality of data describing the effect of fundoplication in patients with chronic cough is low, with most reports describing series of patients with no control group or comparator therapy, patients selected for surgery using a variety of different criteria and then the effect not assessed with validated tools for the assessment of cough [6,40,43,45,57–60]. Nonetheless if these data are accurate, approximately 60% may respond to surgery, however it remains unclear which groups of patients are most likely to respond. Better designed studies are needed to establish whether fundoplication is truly effective in a subgroup of patients with chronic cough and if so, what features define this group.
Reflux is just another Cough ‘Trigger’
A final important consideration in the debate about a causal link between gastro-esophageal reflux disease and cough is the question, if reflux does trigger coughing in a subgroup of patients, is this their only cough trigger? Patients with chronic cough frequently report coughing to a wide variety of triggers. These include otherwise innocuous exposures to airway irritants such as smoke or perfumes, changes in temperature, and use of the larynx such as talking excessively, laughing or singing. All these stimuli have the potential to activate vagal afferents, so perhaps such patients are also hypersensitive to internal vagal stimuli such as esophageal reflux events. Of note, in our study, patients with positive reflux-cough associations with also had heightened cough responses to inhaled citric acid. This supports the idea that central sensitization might explain neuronal crosstalk between esophagus and cough reflex, but also suggests these same patients are sensitized to airway as well as esophageal stimuli. If this is the case, targeting treatments to reduce reflux events may not be a successful strategy and indeed the term gastro-esophageal reflux disease may not be the most appropriate classification phenomenon of reflux triggering cough. Newer terms such as cough hypersensitivity syndrome are being suggested to describe the sensitivity of patients to environmental cough stimuli but may also ultimately encompass cough responses to reflux.
Conclusions
In conclusion, whilst there is a significant body of circumstantial evidence associating chronic cough with gastro-esophageal reflux disease, definitive studies establishing a causal effect are still lacking. Furthermore, it remains to be determined whether reflux-cough associations are simply a reflection of vagal neuronal hypersensitivity and accompanied by cough responses to many other innocuous stimuli, rather than a discrete form of gastro-esophageal reflux disease.
Footnotes
Conflict of interest: Dr. Kahrilas is supported by R01 DK56033 and R01 DK092217 from the Public Health Service; Dr. Smith…; Dr. Dicpinigaitis reports no conflicts relevant to the content of this manuscript.
References
- 1.Irwin RS. Chronic cough due to gastroesophageal reflux disease: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl 1):80S–94S. doi: 10.1378/chest.129.1_suppl.80S. [DOI] [PubMed] [Google Scholar]
- 2.Morice AH, Fontana GA, Sovijarvi ARA, Pistolesi M, Chung KF, Widdicombe J, et al. The diagnosis and management of chronic cough. Eur Respir J. 2004;24:481–492. doi: 10.1183/09031936.04.00027804. [DOI] [PubMed] [Google Scholar]
- 3.Chang AB, Lasserson TJ, Gaffney J, Connor FL, Garske LA. Gastro-oesophageal reflux treatment for prolonged nonspecific cough in children and adults. Cochrane Database Syst Rev. 2011;(1):CD004823. doi: 10.1002/14651858.CD004823.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Faruqi S, Molyneux ID, Fathi H, Wright C, Thompson R, Morice AH. Chronic cough and esomeprazole: A double-blind placebo-controlled parallel study. Respirology. 2011;16:1150–1156. doi: 10.1111/j.1440-1843.2011.02014.x. [DOI] [PubMed] [Google Scholar]
- 5.Shaheen NJ, Crockett SD, Bright SD, Madanick RD, Buckmire R, Couch M, et al. Randomised clinical trial: high-dose acid suppression for chronic cough – a double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2011;33:225–234. doi: 10.1111/j.1365-2036.2010.04511.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Irwin RS, Zawacki JK, Wilson MM, French CT, Callery MP. Chronic cough due to gastroesophageal reflux disease: failure to resolve despite total/near-total elimination of esophageal acid. Chest. 2002;121:1132–1140. doi: 10.1378/chest.121.4.1132. [DOI] [PubMed] [Google Scholar]
- 7.Poe RH, Kallay MC. Chronic cough and gastroesophageal reflux disease: experience with specific therapy for diagnosis and treatment. Chest. 2003;123:679–684. doi: 10.1378/chest.123.3.679. [DOI] [PubMed] [Google Scholar]
- 8.Vakil N, Veldhuyzen van Zanten S, Kahrilas P, et al. The Montreal definition and classification of gastro-esophageal reflux disease (GERD) – a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–1920. doi: 10.1111/j.1572-0241.2006.00630.x. [DOI] [PubMed] [Google Scholar]
- 9.Locke GR, 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ., 3rd Prevalence and clinical spectrum of gastro-oesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448–1456. doi: 10.1016/s0016-5085(97)70025-8. [DOI] [PubMed] [Google Scholar]
- 10.El-Serag HB, Sonnenberg A. Comorbid occurrence of laryngeal or pulmonary disease with esophagitis in United States military veterans. Gastroenterology. 1997;113:755–760. doi: 10.1016/s0016-5085(97)70168-9. [DOI] [PubMed] [Google Scholar]
- 11.Gislason T, Janson C, Vermeire P, et al. Respiratory symptoms and nocturnal gastro-esophageal reflux: a population based study of young adults in three European countries. Chest. 2002;121:158–163. doi: 10.1378/chest.121.1.158. [DOI] [PubMed] [Google Scholar]
- 12.Sackett DL, Straus SE, Richardson WS, et al. Evidence-based medicine: How to practice and teach EBM. 2. Churchill Livingstone; Edinburgh: 2000. [Google Scholar]
- 13.Ing AJ, Ngu MC, Breslin AB. Pathogenesis of chronic persistent cough associated with gastroesophageal reflux. Am J Respir Crit Care Med. 1994;149:160–167. doi: 10.1164/ajrccm.149.1.8111576. [DOI] [PubMed] [Google Scholar]
- 14.Irwin RS, French CL, Curley FJ, et al. Chronic cough due to gastroesophageal reflux. Clinical, diagnostic, and pathogenetic aspects. Chest. 1993;104:1511–1517. doi: 10.1378/chest.104.5.1511. [DOI] [PubMed] [Google Scholar]
- 15.Dicpinigaitis PV. Short- and long-term reproducibility of capsaicin cough challenge testing. Pulm Pharmacol Ther. 2003;16:61–65. doi: 10.1016/S1094-5539(02)00149-9. [DOI] [PubMed] [Google Scholar]
- 16.Javorkova N, Varechova S, Pecova R, et al. Acidification of the oesophagus acutely increases the cough sensitivity in patients with gastro-oesophageal reflux and chronic cough. Neurogastroenterol Motil. 2008;20:119–124. doi: 10.1111/j.1365-2982.2007.01020.x. [DOI] [PubMed] [Google Scholar]
- 17.Vaezi MF, Hicks DM, Abelson TI, et al. Laryngeal signs and symptoms and gastroesophageal reflux disease (GERD): a critical assessment of cause and effect association. Clin Gastroenterol Hepatol. 2003;1:333–344. doi: 10.1053/s1542-3565(03)00177-0. [DOI] [PubMed] [Google Scholar]
- 18.Irwin RS, Ownbey R, Cagle PT, et al. Interpreting the histopathology of chronic cough: a prospective, controlled, comparative study. Chest. 2006;130:362–370. doi: 10.1378/chest.130.2.362. [DOI] [PubMed] [Google Scholar]
- 19.Patterson N, Mainie I, Rafferty G, et al. Nonacid reflux episodes reaching the pharynx are important factors associated with cough. J Clin Gastroenterol. 2009;43:414–419. doi: 10.1097/MCG.0b013e31818859a3. [DOI] [PubMed] [Google Scholar]
- 20.Oelschlager BK, Quiroga E, Isch JA, Cuenca-Abente F. Gastroesophageal and pharyngeal reflux detection using impedance and 24-hour pH monitoring in asymptomatic subjects: defining the normal environment. J Gastrointest Surg. 2006;10:54–62. doi: 10.1016/j.gassur.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 21.Decalmer S, Stovold R, Houghton LA, et al. Chronic cough: relationship between microaspiration, gastroesophageal reflux, and cough frequency. Chest. 2012;142:958–964. doi: 10.1378/chest.12-0044. [DOI] [PubMed] [Google Scholar]
- 22.Bohman JK, Kor DJ, Kashyap R, Gajic O, Festic E, He Z, Lee AS. Airway pepsin levels in otherwise healthy surgical patients receiving general anesthesia with endotracheal intubation. Chest. 2013;143:1407–1413. doi: 10.1378/chest.12-1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kahrilas PJ. When proton pump inhibitors fail (editorial) Clin Gastroenterol Hepatol. 2008;6:482–483. doi: 10.1016/j.cgh.2008.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ing AJ, Ngu MC, Breslin AB. Chronic persistent cough and gastro-oesophageal reflux. Thorax. 1991;46:479–483. doi: 10.1136/thx.46.7.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ours TM, Kavuru MS, Schilz RJ, et al. A prospective evaluation of esophageal testing and a double-blind, randomized study of omeprazole in a diagnostic and therapeutic algorithm for chronic cough. Am J Gastroenterol. 1999;94:3131–3138. doi: 10.1111/j.1572-0241.1999.01504.x. [DOI] [PubMed] [Google Scholar]
- 26.Paterson WG, Murat BW. Combined ambulatory esophageal manometry and dual-probe pH-metry in evaluation of patients with chronic unexplained cough. Dig Dis Sci. 1994;39:1117–1125. doi: 10.1007/BF02087567. [DOI] [PubMed] [Google Scholar]
- 27.Blondeau K, Dupont LJ, Mertens V, et al. Improved diagnosis of gastro-oesophageal reflux in patients with unexplained chronic cough. Aliment Pharmacol Ther. 2007;25:723–732. doi: 10.1111/j.1365-2036.2007.03255.x. [DOI] [PubMed] [Google Scholar]
- 28.Sifrim D, Dupont L, Blondeau K, et al. Weakly acidic reflux in patients with chronic unexplained cough during 24 hour pressure, pH, and impedance monitoring. Gut. 2005;54:449–454. doi: 10.1136/gut.2004.055418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bogte A, Bredenoord AJ, Smout AJ. Diagnostic yield of oesophageal pH monitoring in patients with chronic unexplained cough. Scand J Gastroenterol. 2008;43:13–19. doi: 10.1080/00365520701580421. [DOI] [PubMed] [Google Scholar]
- 30.Smith JA, Decalmer S, Kelsall A, et al. Acoustic cough-reflux associations in chronic cough: potential triggers and mechanisms. Gastroenterology. 2010;139:754–62. doi: 10.1053/j.gastro.2010.06.050. [DOI] [PubMed] [Google Scholar]
- 31.Kunsch S, Gross V, Neesse A, et al. Combined lung-sound and reflux-monitoring: a pilot study of a novel approach to detect nocturnal respiratory symptoms in gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2011;33:592–600. doi: 10.1111/j.1365-2036.2010.04559.x. [DOI] [PubMed] [Google Scholar]
- 32.Chang AB, Lasserson TJ, Kiljander TO, et al. Systematic review and meta-analysis of randomised controlled trials of gastro-oesophageal reflux interventions for chronic cough associated with gastro-oesophageal reflux. BMJ. 2006;332:11–17. doi: 10.1136/bmj.38677.559005.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chang AB, Lasserson TJ, Gaffney J, Connor FL, Garske LA. Gastro-oesophageal reflux treatment for prolonged non-specific cough in children and adults. Cochrane Database Syst Rev. 2006;(4):CD004823. doi: 10.1002/14651858.CD004823.pub3. [DOI] [PubMed] [Google Scholar]
- 34.Kahrilas PJ, Howden CW, Hughes N, et al. Response of chronic cough to acid-suppressive therapy in patients with gastroesophageal reflux disease. Chest. 2013;143:605–612. doi: 10.1378/chest.12-1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kiljander TO, Salomaa ER, Hietanen EK, Terho EO. Chronic cough and gastro-oesophageal reflux: a double-blind placebo-controlled study with omeprazole. Eur Respir J. 2000;16:633–638. doi: 10.1034/j.1399-3003.2000.16d11.x. [DOI] [PubMed] [Google Scholar]
- 36.Noordzij JP, Khidr A, Evans BA, et al. Evaluation of omeprazole in the treatment of reflux laryngitis: a prospective, placebo-controlled, randomized, double-blind study. Laryngoscope. 2001;111:2147–2151. doi: 10.1097/00005537-200112000-00013. [DOI] [PubMed] [Google Scholar]
- 37.Ing AJ, Ngu MC, Breslin ABX. A randomised double blind placebo controlled cross-over study of ranitidine in patients with chronic persistent cough (CPC) associated with gastroesophageal reflux (GOR) [abstract] Am Rev Resp Dis. 1992;145 (4 pt 2):A11. [Google Scholar]
- 38.Vaezi MF, Richter JE, Stasney CR, et al. Treatment of chronic posterior laryngitis with esomeprazole. Laryngoscope. 2006;116:254–260. doi: 10.1097/01.mlg.0000192173.00498.ba. [DOI] [PubMed] [Google Scholar]
- 39.Francis DO, Goutte M, Slaughter JC, et al. Traditional reflux parameters and not impedance monitoring predict outcome after fundoplication in extraesophageal reflux. Laryngoscope. 2011;121:1902–1909. doi: 10.1002/lary.21897. [DOI] [PubMed] [Google Scholar]
- 40.Allen CJ, Anvari M. Gastro-oesophageal reflux related cough and its response to laparoscopic fundoplication. Thorax. 1998;53:963–968. doi: 10.1136/thx.53.11.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Allen CJ, Anvari M. Preoperative symptom evaluation and esophageal acid infusion predict response to laparoscopic Nissen fundoplication in gastroesophageal reflux patients who present with cough. Surg Endosc. 2002;16:1037–1041. doi: 10.1007/s00464-001-8330-4. [DOI] [PubMed] [Google Scholar]
- 42.Brouwer R, Kiroff GK. Improvement of respiratory symptoms following laparoscopic Nissen fundoplication. ANZ J Surg. 2003;73:189–193. doi: 10.1046/j.1445-1433.2002.02568.x. [DOI] [PubMed] [Google Scholar]
- 43.Ziora D, Jarosz W, Dzielicki J, et al. Citric acid cough threshold in patients with gastroesophageal reflux disease rises after laparoscopic fundoplication. Chest. 2005;128:2458–2464. doi: 10.1378/chest.128.4.2458. [DOI] [PubMed] [Google Scholar]
- 44.So JB, Zeitels SM, Rattner DW. Outcomes of atypical symptoms attributed to gastro-esophageal reflux treated by laparoscopic fundoplication. Surgery. 1998;124:28–32. [PubMed] [Google Scholar]
- 45.Faruqi S, Sedman P, Jackson W, Molyneux I, Morice AH. Fundoplication in chronic intractable cough. Cough. 2012;8:3. doi: 10.1186/1745-9974-8-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hoppo T, Komatsu Y, Jobe BA. Antireflux surgery in patients with chronic cough and abnormal proximal exposure as measured by hypopharyngeal multichannel intraluminal impedance. JAMA Surg. 2013;148:608–615. doi: 10.1001/jamasurg.2013.1376. [DOI] [PubMed] [Google Scholar]
- 47.Trinick R, Johnston N, Dalzell AM, McNamara PS. Reflux aspiration in children with neurodisability--a significant problem, but can we measure it? J Pediatr Surg. 2012;47:291–298. doi: 10.1016/j.jpedsurg.2011.11.019. [DOI] [PubMed] [Google Scholar]
- 48.Grabowski M, Kasran A, Seys S, Pauwels A, Medrala W, Dupont L, Panaszek B, Bullens D. Pepsin and bile acids in induced sputum of chronic cough patients. Respir Med. 2011;105:1257–1261. doi: 10.1016/j.rmed.2011.04.015. [DOI] [PubMed] [Google Scholar]
- 49.Pauwels A, Decraene A, Blondeau K, Mertens V, Farre R, Proesmans M, Van Bleyenbergh P, Sifrim D, Dupont LJ. Bile acids in sputum and increased airway inflammation in patients with cystic fibrosis. Chest. 2012;141:1568–1574. doi: 10.1378/chest.11-1573. [DOI] [PubMed] [Google Scholar]
- 50.Zerbib F, Roman S, Bruley Des Varannes S, Gourcerol G, Coffin B, Ropert A, Lepicard P, Mion F. Normal values of pharyngeal and esophageal twenty-four-hour ph impedance in individuals on and off therapy and interobserver reproducibility. Clin Gastroenterol Hepatol. 2013;11:366–372. doi: 10.1016/j.cgh.2012.10.041. [DOI] [PubMed] [Google Scholar]
- 51.Kawamura O, Shimoyama Y, Hosaka H, Kuribayashi S, Maeda M, Nagoshi A, Zai H, Kusano M. Increase of weakly acidic gas esophagopharyngeal reflux (epr) and swallowing-induced acidic/weakly acidic epr in patients with chronic cough responding to proton pump inhibitors. Neurogastroenterol Motil. 2011;23:411–418. e172. doi: 10.1111/j.1365-2982.2010.01658.x. [DOI] [PubMed] [Google Scholar]
- 52.Ummarino D, Vandermeulen L, Roosens B, Urbain D, Hauser B, Vandenplas Y. Gastroesophageal reflux evaluation in patients affected by chronic cough: Restech versus multichannel intraluminal impedance/ph metry. Laryngoscope. 2013;123:980–984. doi: 10.1002/lary.23738. [DOI] [PubMed] [Google Scholar]
- 53.Becker V, Graf S, Schlag C, Schuster T, Feussner H, Schmid RM, Bajbouj M. First agreement analysis and day-to-day comparison of pharyngeal ph monitoring with ph/impedance monitoring in patients with suspected laryngopharyngeal reflux. J Gastrointest Surg. 2012;16:1096–1101. doi: 10.1007/s11605-012-1866-x. [DOI] [PubMed] [Google Scholar]
- 54.Koch OO, Kaindlstorfer A, Antoniou SA, Asche KU, Granderath FA, Pointner R. Laparoscopic nissen versus toupet fundoplication: Objective and subjective results of a prospective randomized trial. Surg Endosc. 2012;26:413–422. doi: 10.1007/s00464-011-1889-5. [DOI] [PubMed] [Google Scholar]
- 55.Galmiche JP, Hatlebakk J, Attwood S, Ell C, Fiocca R, Eklund S, Langstrom G, Lind T, Lundell L. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic gerd: The lotus randomized clinical trial. JAMA. 2011;305:1969–1977. doi: 10.1001/jama.2011.626. [DOI] [PubMed] [Google Scholar]
- 56.Campos GM, Peters JH, DeMeester TR, Oberg S, Crookes PF, Tan S, DeMeester SR, Hagen JA, Bremner CG. Multivariate analysis of factors predicting outcome after laparoscopic nissen fundoplication. J Gastrointest Surg. 1999;3:292–300. doi: 10.1016/s1091-255x(99)80071-7. [DOI] [PubMed] [Google Scholar]
- 57.Novitsky YW, Zawacki JK, Irwin RS, French CT, Hussey VM, Callery MP. Chronic cough due to gastroesophageal reflux disease: Efficacy of antireflux surgery. Surg Endosc. 2002;16:567–571. doi: 10.1007/s00464-001-8328-y. [DOI] [PubMed] [Google Scholar]
- 58.Kirkby-Bott J, Jones E, Perring S, Hosking SW. Proximal acid reflux treated by fundoplication predicts a good outcome for chronic cough attributable to gastro-oesophageal reflux disease. Langenbecks Arch Surg. 2011;396:167–171. doi: 10.1007/s00423-010-0702-6. [DOI] [PubMed] [Google Scholar]
- 59.Mainie I, Tutuian R, Agrawal A, Hila A, Highland KB, Adams DB, Castell DO. Fundoplication eliminates chronic cough due to non-acid reflux identified by impedance ph monitoring. Thorax. 2005;60:521–523. doi: 10.1136/thx.2005.040139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thoman DS, Hui TT, Spyrou M, Phillips EH. Laparoscopic antireflux surgery and its effect on cough in patients with gastroesophageal reflux disease. J Gastrointest Surg. 2002;6:17–21. doi: 10.1016/s1091-255x(01)00013-0. [DOI] [PubMed] [Google Scholar]


