Abstract
Background
Infection with Streptococcus pneumoniae is a major cause of childhood morbidity and mortality worldwide, especially in low income countries where pneumococcal conjugate vaccines (PCVs) are still underused. In countries where PCVs have been introduced, much of their efficacy has resulted from their impact on nasopharyngeal carriage in vaccinated children. Understanding the epidemiology of carriage for S. pneumoniae and other common respiratory bacteria in developing countries is crucial for implementing appropriate vaccination strategies and evaluating their impact.
Methods and Findings
We have systematically reviewed published studies reporting nasopharyngeal or oropharyngeal carriage of S. pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, Staphylococcus aureus, and Neisseria meningitidis in children and adults in low and lower-middle income countries. Studies reporting pneumococcal carriage for healthy children <5 years of age were selected for a meta-analysis. The prevalences of carriage for S. pneumoniae, H. influenzae, and M. catarrhalis were generally higher in low income than in lower-middle income countries and were higher in young children than in adults. The prevalence of S. aureus was high in neonates. Meta-analysis of data from young children before the introduction of PCVs showed a pooled prevalence estimate of 64.8% (95% confidence interval, 49.8%–76.1%) in low income countries and 47.8% (95% confidence interval, 44.7%–50.8%) in lower-middle income countries. The most frequent serotypes were 6A, 6B, 19A, 19F, and 23F.
Conclusions
In low and lower-middle income countries, pneumococcal carriage is frequent, especially in children, and the spectrum of serotypes is wide. However, because data are limited, additional studies are needed to adequately assess the impact of PCV introduction on carriage of respiratory bacteria in these countries.
Introduction
Streptococcus pneumoniae (the pneumococcus) is a major cause of invasive diseases and respiratory tract infections and caused approximately 500,000 deaths in children <5 years of age in 2008, mostly in low income countries [1], [2]. Asymptomatic nasopharyngeal carriage, which plays an essential role in the transmission of S. pneumoniae, usually precedes invasive pneumococcal disease (IPD) [3].
Since 2000, the introduction of the 7-valent pneumococcal conjugate vaccine (PCV-7,) and second generation PCVs has significantly reduced the burden of IPD in vaccinated children [4]–[11]. PCVs have also reduced IPD in unvaccinated children and adults [5], [8], [10], [12]. The indirect (or herd) effects of PCVs against IPD are driven primarily by their impact on carriage of vaccine-type (VT) pneumococci in vaccinated children, preventing transmission to unvaccinated contacts [13]–[15].
Reduction in carriage of VT pneumococci due to PCV vaccination is often accompanied by an increase in the carriage of non-vaccine-type (NVT) pneumococci and, to a lesser extent, an increase in the incidence of IPD caused by NVT pneumococci [7], [8], [14], [16], [17]. However, the overall benefit of PCV-7 vaccination has not been substantially affected by replacement disease [7], [8], [18], [19] except in Alaska and possibly the United Kingdom [5], [20].
By reducing nasopharyngeal carriage of VT pneumococci, PCVs may also create ecological niches for colonization of alternative respiratory pathogens such as Staphylococcus aureus, Haemophilus influenzae, and Moraxella catarrhalis [21], bacteria that are frequently carried by children and are important causes of disease worldwide [22]–[24]. Introducing PCVs may also have modified carriage of Neisseria meningitidis in children, although the prevalence of meningococcal carriage is usually higher in adolescents and young adults [25]. Vaccination with PCV-7 has been associated with a shift in the etiology of acute otitis media (AOM) so that non-typeable H. influenzae has become the leading cause of AOM in place of S. pneumoniae in several studies [26], [27]. In addition, some studies have shown that carriage of S. pneumoniae is inversely related to carriage of S. aureus in healthy children [21], [28], [29]. Clarifying the interactions between these different pathogens is essential to assess overall impact on conjugate vaccines. H. influenzae type b (Hib) and N. meningitidis conjugate vaccines are also available and being introduced in low income countries, which may further influence global patterns of bacterial carriage [30].
Because the burden of IPD is high in young children in developing countries, second generation PCVs including more pneumococcal serotypes are being rapidly introduced into the Expanded Programme on Immunization of low and lower-middle income countries [2], [31]. Given the impact of PCV-7 childhood vaccination on carriage and the subsequent indirect benefits seen in industrialized countries, understanding the dynamics of pharyngeal carriage of pneumococci in developing countries is crucial to predict the potential public health implications of routine PCV use in these settings. Therefore, we have conducted a systematic literature review to evaluate nasopharyngeal and oropharyngeal carriage prevalence of S. pneumoniae in children and adults from low and lower-middle income countries, with a focus on children <5 years of age. We have also analyzed the prevalence of carriage of other common pathogenic respiratory bacteria that could be affected by the introduction of PCVs.
Methods
Search strategy and selection criteria
We systematically reviewed the literature on the carriage of S. pneumoniae, H. influenzae, M. catarrhalis, S. aureus, and N. meningitidis in low and lower-middle income countries, as defined by the World Bank (Text S1) [32]. We searched PubMed for articles published in English between January 1, 1990 and October 23, 2012 using a combination of search strings for microbiological agents, colonization and carriage, and low income and lower-middle income countries (Text S1). Websites of the World Health Organization (www.who.int), the United Nations International Children's Emergency Fund (www.unicef.org), and Google (www.google.com) were searched for additional data. The review is reported according to the PRISMA statement (Table S2) [33].
Two reviewers independently screened the titles and abstracts of all retrieved articles. Disagreements between the two reviewers were resolved by discussion. Articles that did not contain relevant information were excluded. In a second step, the full text of the selected articles was assessed for eligibility using pre-defined inclusion and exclusion criteria (Protocol S1).
All articles relevant to the objectives of the review and that reported prevalences of nasopharyngeal or oropharyngeal carriage of S. pneumoniae, H. influenzae, M. catarrhalis, S. aureus, or N. meningitidis in children or adults of all ages were included. Articles were excluded if they were letters (except those reporting results from studies that had a reasonable sample size and interpretable results), editorials, comments, or diagnostic articles; lacked methodology (e.g. no inclusion or exclusion criteria, setting not clearly described, or were biased); the location from which the swab was collected, the culture plate, or the method for identifying pathogens was unclear; reported phase II trials; reported randomized controlled trials with no usable intervention or placebo group (if only the placebo group was usable, the article was included but only the results of the placebo arm were considered); reported studies with a sample size <50 (except for articles on M. catarrhalis); were reviews that included only articles already covered by the current search.
Assessment of study quality
Reviewers assessed the quality of the studies reviewed by adapting the criteria of the Coordination of Cancer Clinical Practice Guidelines [34] for epidemiological studies. Specifically, the quality of the following were scored as - -, -, 0, +, or ++: study population clearly described and representative of the source population; outcome measures described; results applicable to the subject group targeted in the review; study design and setting described; main potential confounders identified and taken into account in the design and analysis; confidence intervals provided; type of sample collected and the typing method described clearly. This checklist was not designed to calculate a global quality score for each study. In case of doubt whether the quality of a study was sufficient for inclusion, the reviewer discussed the article with a second reviewer.
Data extraction and analysis
An EndNote (Thomson Reuters, New York, NY) database containing all the included and excluded articles was created. Extracted data included country, setting, study years, study design, population studied, type of swab obtained, culture and identification methods, number of subjects, number of swabs, definition of prevalence, and prevalence of carriage.
Prevalence of carriage (with 95% confidence interval [CI] if available) was reported for each pathogen for healthy, immunocompromised, and ill populations. Ill populations were defined as subjects with IPD, AOM, sinusitis, or respiratory tract infection (RTI). When subjects were swabbed once, point prevalence was defined as the number of positives per total samples or subjects. When subjects were swabbed several times, average prevalence was defined as the total number of positive samples divided by the total number of samples collected, without taking into account the number of samples taken per subject or the duration of the study. Period prevalence was defined as the percentage of subjects who were positive at some point during the study period. The serotype distribution (expressed as percentage of subjects or isolates) and the bacterial density (expressed as arbitrary units [35] or bacterial load calculated as genome equivalent/mL sample secretion [36]) were also analyzed when data were available.
Meta-analysis
Studies with a similar study design that reported S. pneumoniae carriage for healthy children <5 years of age were selected for a meta-analysis. Studies were included in the meta-analysis if the articles reported point prevalence estimates (with available number of subjects positive for carriage and sample size in the target age group) and if they included at least 100 subjects. Pooled prevalence estimates of carriage were computed when possible using the random-effects model of DerSimonian-Laird [37]. Heterogeneity between studies was assessed using the I2 statistic. Stata version 11 (StataCorp, College Station, TX) and Metalight (Metalight Systems, Round Rock, TX) were used for all analyses.
Results
Results of the literature search
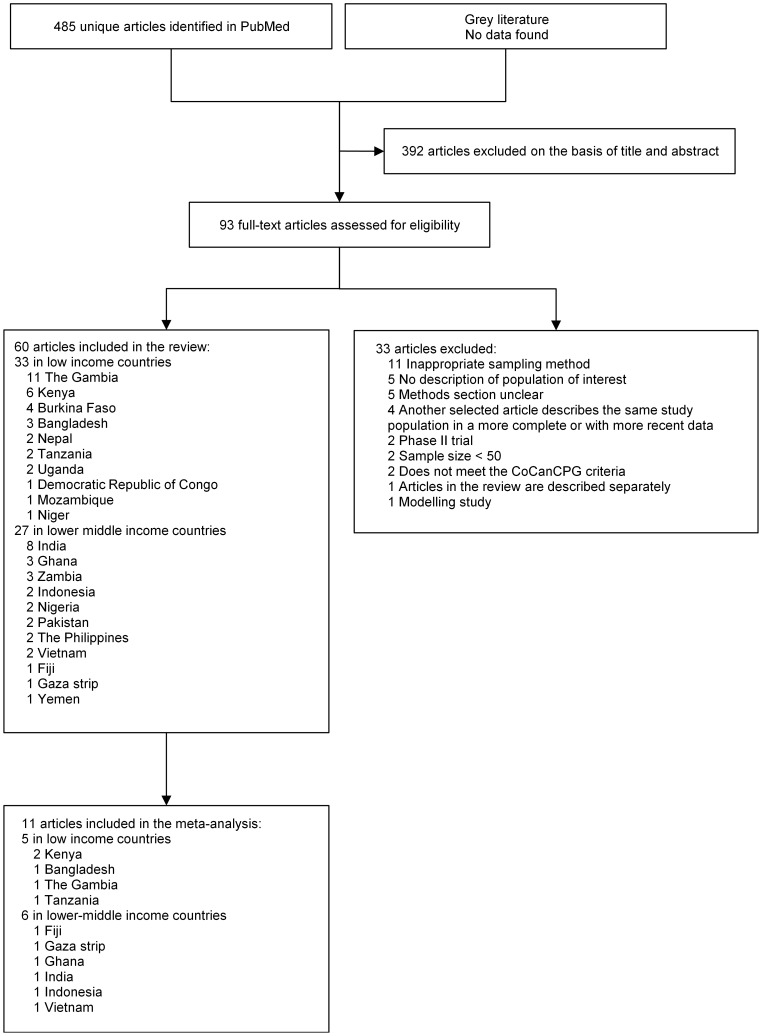
We identified 485 articles related to carriage of potentially pathogenic bacteria from PubMed; 93 were retrieved for assessment of the full text (Figure 1). Sixty of these articles were included in the systematic review, 33 of which were from low income countries and 27 from lower-middle income countries. These studies were most frequently performed in Africa (N = 38) and Asia (N = 21). One article was from Oceania. A total of 44 articles reported carriage results for S. pneumoniae, 12 for H. influenzae, three for M. catarrhalis, four for S. aureus, and nine for N. meningitidis. Eight articles reported prevalence of carriage for more than one pathogen.
Figure 1. Flowchart of study selection.
CoCanCPG, Coordination of Cancer Clinical Practice Guidelines.
Carriage of Streptococcus pneumoniae
Thirty-two of the 44 studies that reported prevalence of S. pneumoniae carriage were conducted in healthy populations, eight in immunocompromised populations, and six in populations with IPD, AOM, sinusitis, or RTI (Table 1, Table S2). Three articles reported prevalence of carriage in both healthy and ill populations [36], [38], [39].
Table 1. Summary table of studies reporting carriage of Streptococcus pneumoniae.
| Reference | Study period | Country | Sample size | Prevalence | Age group | Prevalence of carriage, % (95% CI) | |
| Low income countries | |||||||
| Healthy population | |||||||
| [65] | Saha et al. 2003 | 1999–2000 | Bangladesh | 2839 children | Point | Total | 46 |
| [49] | Granat et al. 2007 | 2000–2001 | Bangladesh | 98 families with 99 new-borns | Average | 4–12 months | 49.3 |
| 1–4 years | 50.9 | ||||||
| 5–9 years | 41.5 | ||||||
| 10–18 years | 32.4 | ||||||
| Mothers | 7.3 | ||||||
| Other adults | 8.2 | ||||||
| [116] | Coles et al. 2011 | 2005–2007 | Bangladesh | 225 children | Point | 12 weeks | 72.9 |
| [42] | Cheung et al. 2009 | 2003 and 2003–2004 | The Gambia | 2342 children and 675 of their younger siblings | Point and average | Median age: 12 months. Median age siblings: 3 | 86.2a |
| [53] | Roca et al. 2011 | 2003–2008 | The Gambia | 2094 individuals pre-vaccination | Point | 2–<5 years | 93.4a |
| 5–<15 years | 86.3 | ||||||
| ≥15 years | 60.6 | ||||||
| [43] | Kwambana et al. 2011 | NR | The Gambia | 30 infants | Average | 0–12 months | 78 (76–83) |
| [54] | Hill et al. 2010 | NR | The Gambia | 158 individuals | Period | Children | 97 (over study period) |
| Period | Adults | 85 (over study period) | |||||
| [50] | Hill et al. 2008 | NR | The Gambia | 236 infants | Period | 0–11 months | 20–90 (100 over study period) |
| [57] | Hill et al. 2006 | NR | The Gambia | 2972 individuals | Point | Median age: 15 years | 72 |
| [39] | Lloyd-Evans et al. 1996 | 1989–1991 | The Gambia | 113 children | Point | <5 years | 76.1 |
| [55] | Abdullahi et al. 2008 | 2004 | Kenya | 450 individuals | Average | 0–4 years | 57 |
| 5–9 years | 41 (32–51) | ||||||
| 10–85 years | 6.4 | ||||||
| [52] | Abdullahi et al. 2012 | 2006–2009 | Kenya | 2840 children | Point | 3–59 months | 65.8 |
| [51] | Tigoi et al. 2012 | 2006–2009 | Kenya | 1404 children, 1372 mothers, 221 fathers, and 1412 siblings | Average | Mean: 2.1 days. Mean age family members: NR | 63.2b |
| [64] | Valles et al. 2006 | 2003 | Mozambique | 285 children | Point | <5 years | 87 |
| [38] | Coles et al. 2008 | 2003–2005 | Nepal | 197 children | Point | 1–36 months | 78.7a |
| [63] | Moyo et al. 2012 | 2010 | Tanzania | 300 children | Point | <5 years | 35 |
| Immunocompromised population | |||||||
| [117] | Rusen et al. 1997 | 1990 | Kenya | 26 children with HIV | Point | <5 years | 86 |
| [58] | Abdullahi et al. 2012 | 2006–2008 | Kenya | 99 children with HIV | Point | 3–59 months | 76 (66–84) |
| [41] | Anthony et al. 2012 | 2008 | Tanzania | 142 children with HIV | Point | 1–4 years | 88 |
| 5–9 years | 77 | ||||||
| 10–14 years | 76 | ||||||
| [59] | Kateete et al. 2012 | 2001–2002 | Uganda | 81 children with homozygote sickle cell disease | Point | 8 months–6 years | 33 |
| [40] | Blossom et al. 2006 | 2004–2005 | Uganda | 600 individuals with HIV | Point | Adults (mean age 38.15 years) | 18 |
| Sick population | |||||||
| [39] | Lloyd-Evans et al. 1996 | 1989–1991 | The Gambia | 1152 children: 1071 sick (clinical diagnosis of pneumonia, meningitis, septicemia, or other serious bacterial infection) and 81 with IPD | Point | <5 years | Sick: 85.1. IPD: 90.1 |
| [38] | Coles et al. 2008 | 2003–2005 | Nepal | 197 children with ALRI | Point | 1–36 months | 80.2a |
| Lower-middle income countries | |||||||
| Healthy population | |||||||
| [68] | Russell et al. 2006 | 2003–2004 | Fiji | 774 children | Point | 3–13 months | 44.3 |
| [56] | Regev-Yochay et al. 2012 | 2009 | Gaza strip | 379 children | Point | 3 weeks–5.5 years | 50 |
| 379 parents | NR | 8 | |||||
| [66] | Denno et al. 2002 | 1996 | Ghana | 311 children | Point | 6–12 months | 51.4 |
| [118] | Donkor et al. 2010 | 2006–2007 | Ghana | 124 children | Point | <13 years | 15.3 |
| [119] | Coles et al. 2001 | 1998–1999 | India | 225 infants | Point | 2 months | 54.2 |
| 4 months | 67.9 | ||||||
| 6 months | 69.8 | ||||||
| [75] | Das et al. 2002 | 2000–2001 | India | 566 children | Point | 5–12 years | 29.1 |
| [120] | Devi et al. 2012 | 2009–2010 | India | 811 children | Point | 0–14 years | 12.8 |
| [67] | Rupa et al. 2012 | 2009–2010 | India | 210 children | Point | 0–1 years | Maximum: 46.3 |
| [121] | Wattal et al. 2007 | NR | India | 200 children | Point | 3 months–3 years | 6.5 |
| [69] | Soewignjo et al. 2001 | 1997 | Indonesia | 484 children | Point | 0–25 months | 48 (42–54)c |
| [122] | Adetifa et al. 2012 | NR | Nigeria | 1005 individuals | Point | All ages | 52.5 (49.4–55.7) |
| [36] | Vu et al. 2011 | 2007–2008 | Vietnam | 350 children | Point | <5 years | 50.3 |
| [123] | Gill et al. 2008 | 2003–2005 | Zambia | 132 children born to HIV+ mothers and 128 children born to HIV− mothers | Average | 6 weeks | 25.8 |
| Immunocompromised population | |||||||
| [70] | Bhattacharya et al. 2012 | 2008–2009 | India | 148 children with HIV | Point | 1–16 years | 28 |
| [71] | Mwenya et al. 2010 | 2002–2003 | Zambia | 439 children with HIV | Point | 6 months–14 years | 51 |
| [124] | Gill et al. 2008 | 2003–2005 | Zambia | 132 women with HIV | Average | Mean: 25.9 years | 11.4 |
| Sick population | |||||||
| [62] | Mastro et al. 1993 | 1989–1990 | Pakistan | 601 children with ARI | Point | Mean:14.5 months | 64.4 |
| [60] | Lankinen et al. 1994 | 1984 | The Philippines | 318 children with ALRI | Point | <5 years | 51 |
| [61] | Lupisan et al. 2000 | 1994 | The Philippines | 956 children with severe pneumonia, suspected meningitis, or clinical suspicion of sepsis. | Point | 0–59 months | 27.9 |
| [36] | Vu et al. 2011 | 2007–2008 | Vietnam | 274 children with radiologically confirmed pneumonia | Point | <5 years | 38.7 |
| 276 children with other LRTI | 43.3 | ||||||
ALRI, acute lower respiratory infection; ARI, acute respiratory infection; HIV, human immunodeficiency virus; IPD, invasive pneumococcal disease; LRTI, lower respiratory tract infection; NR, not reported.
Carriage rate is from the control group.
Overall carriage rate. Children, mothers, fathers, and siblings combined.
Age- and population-weighted carriage rate, adjusted for design effect.
One study included oropharyngeal rather than nasopharyngeal samples [40] and four studies used polymerase chain reaction (PCR) rather than conventional microbiology to detect carriage [36], [41]–[43]. Fourteen studies mentioned that sampling, storage, and culture procedures followed the WHO guidelines for detecting carriage of S. pneumoniae [44], [45]. Calcium alginate was the most frequent type of swab used (17/44 studies; 38.6%). Four articles did not report overall prevalence of pneumococcal carriage and are therefore not listed in Table 1, although they were included in the review for other outcomes. Three of these articles reported prevalence of pneumococcal carriage only by serotype [46]–[48], and one reported an overall carriage rate that had been published previously but reported a secondary analysis of bacterial density and impact of vaccination [35]. All the studies were performed before the introduction of PCV into the national childhood immunization program.
The prevalences of S. pneumoniae carriage in healthy children <5 years of age ranged from 20% to 93.4% in low income countries and were generally higher than reported in lower-middle income countries (range, 6.5%–69.8%). Two longitudinal studies undertaken in The Gambia and Bangladesh reported that all children carried S. pneumoniae at least once during their first year of life [49], [50]. In The Gambia, carriage rates increased from 20% within a week of birth to 80%–90% between 3 and 11 months of age [50]. A similar result was found using PCR [43]. The median age at first acquisition of S. pneumoniae was 24 days (95% CI, 21–28) in The Gambia and 38.5 days in Kenya [50], [51]. In Kenya, the acquisition rate of pneumococcal carriage was 0.0189 acquisitions/day (95% CI, 0.0177–0.0202 acquisitions/day) in newborns and 0.061 acquisitions/day (95% CI, 0.055–0.067) in children <5 years of age [51], [52]. In all the studies that included both children and adults, the prevalence of carriage was higher in children than in adults, with the highest rates found in children <5 years of age [49], [53]–[56]. The highest prevalence of carriage was in The Gambia [39], [42], [43], [50], [53], [54], [57]. No major difference in prevalence was seen between rural or urban settings in lower-middle income countries, but data were not available for urban areas in the low income countries.
All but one study that reported the prevalence of pneumococcal carriage in immunocompromised populations were conducted in Human Immunodeficiency Virus (HIV)-infected populations. S. pneumoniae carriage prevalence in HIV-infected subjects decreased with age (76%–88% in children <5 years of age vs. 11.4%–18% in adults). In Kenya, the prevalence of carriage in HIV-infected children 3–59 months of age was higher than in those uninfected (76% [95% CI, 66%–84%] vs. 65.8% [95% CI, 64.0%–67.5%], p = 0.04) [52], [58]. One study, from a low income country (Uganda), reported a 33% prevalence in children aged 8 months–6 years with homozygote sickle cell disease, a prevalence which was lower than in HIV-infected children in the same age category [59].
Six studies reported prevalence of S. pneumoniae carriage in ill subjects, all in children <5 years of age. Prevalence rates ranged from 80.2% to 90.1% in low income countries and from 27.9% to 64.4% in lower-middle income countries [36], [38], [39], [60]–[62]. The prevalence of carriage was generally lower in children with radiologically confirmed pneumonia (RCP, 38.7%) than in children with IPD (90.1%) or RTIs (43.3%–80.2%).
Serotype distribution
Overall serotype distributions were reported for 33 studies, 22 of which reported details of the particular serotypes or serogroups detected (Table S3). Overall, a wide spectrum of serotypes was detected, with up to 74 different serotypes isolated in one study [57]. Serotypes 6A, 6B, 19A, 19F, and 23F were the serotypes most commonly isolated. Serotypes 14 and 11A were also frequently isolated. A longitudinal study in The Gambia showed that serotypes 6B, 19F, 23F, and 6A were the most commonly isolated pneumococci at first acquisition, whereas serotypes 6B, 19F, 14, and 6A were the most common isolated in subsequent episodes of carriage [50]. In addition, NVT were acquired faster (median age at acquisition, 152 days vs. 174; p = 0.004) and had a shorter duration of carriage (median duration, 43 vs. 70 days; p<0.001) than PCV7-serotypes [50]. Between 36% and 56% of the pneumococcal isolates detected in unvaccinated healthy children <5 years of age in Africa were of PCV-7 serotypes [50], [51], [57], [63], [64], whereas the proportions were 37%–56% for PHiD-CV (10-valent pneumococcal Haemophilus influenzae protein D conjugate vaccine) and 50%–64% for PCV-13 (13-valent pneumococcal conjugate vaccine) [51], [63]. Non-typeable S. pneumoniae represented between 0.7% [55] and 20.6% [60] of the isolates. The highest percentage of non-typeable S. pneumoniae was in Filipino children with acute lower respiratory tract infection [60].
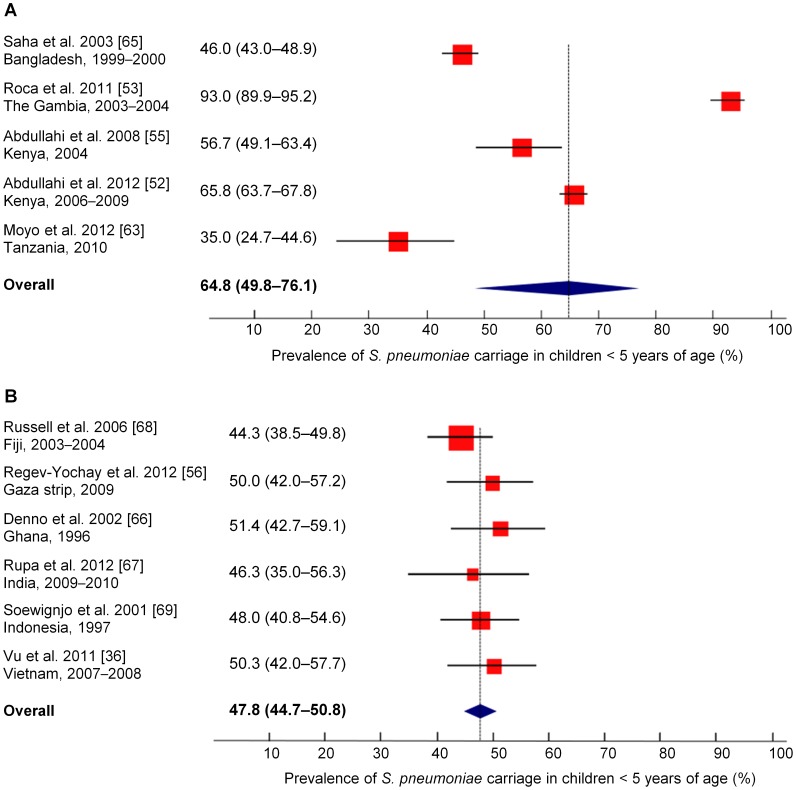
Meta-analysis of pneumococcal carriage
The pooled prevalence for carriage of S. pneumoniae in healthy children <5 years of age was 64.8% (95% CI, 49.8%–76.1%) for the five populations from low income countries [52], [53], [55], [63], [65] and 47.8% (95% CI, 44.7%–50.8%) for the six populations from lower-middle income countries (Figure 2) [36], [56], [66]–[69]. However, studies were highly heterogeneous in the low income countries (I2 = 98%), in contrast to those in the lower-middle income countries (I2 = 0%).
Figure 2. Meta-analysis of S. pneumoniae carriage in healthy children under 5 years of age.
(A) Low income countries. (B) Lower-middle income countries. The point prevalence estimate for each study is represented by a square. The 95% confidence interval (CI) for each study is represented by a horizontal line crossing the square. The size of the square corresponds to the weight of the study in the meta-analysis. All data were obtained before the introduction of the 7-valent pneumococcal conjugate vaccine.
Carriage of Haemophilus influenzae
The highest prevalence of H. influenzae carriage detected in a healthy population (70%) was recorded in a longitudinal study in infants in a rural setting in The Gambia (Table 2, Table S4) [43]. The study, which used PCR to detect respiratory pathogens, reported that carriage of H. influenzae was infrequent at birth (<20% within the first week of life) and increased steadily with age (>90% at 19 weeks), with a pattern similar to that of S. pneumoniae [43]. Another study in a post-Hib vaccination setting reported that H. influenzae carriage rates were lower in children aged ≥10 years and adults (1.1%–3.9%) than in children <10 years (21.0%–29.0%) [55]. The prevalence of H. influenzae carriage in HIV-infected children was reported for India (24%) [70] and Zambia (29%) [71], two lower-middle income countries. The prevalence of H. influenzae carriage in ill children from three lower-middle income countries ranged between 15.2% and 53.5% [36], [61], [62]. PCR generally yielded higher rates of H. influenzae carriage than microbiology in both healthy (31.4%–70% vs. 1.1%–28.6%) and ill (50%–53.5% vs. 15.2%–36.6%) subjects.
Table 2. Summary table of studies reporting carriage of Haemophilus influenzae.
| Reference | Study period | Country | Sample size | Prevalence | Age group | Prevalence of carriage, % (95% CI) | |
| Low income countries | |||||||
| Healthy population | |||||||
| [43] | Kwambana et al. 2011 | NR | The Gambia | 30 infants | Average | 0–12 months | 70 (65–74) |
| [72] | Adegbola et al. 1998 | NR | The Gambia | 3986 children | Point | 1–2 years | Urban: 5.6a Rural: 10.9 |
| [55] | Abdullahi et al. 2008 | 2004b | Kenya | 450 individuals | Point | 0–4 years | 26.0 |
| 5–9 years | 24.0 (16–33) | ||||||
| 10–85 years | 3.0 | ||||||
| [74] | Williams et al. 2011 | 2007 | Nepal | 2195 children | Point | 0–13 years | 5.0 (3.9–6.4) |
| Immunocompromised population | |||||||
| No data found | |||||||
| Sick population | |||||||
| No data found | |||||||
| Lower-middle income countries | |||||||
| Healthy population | |||||||
| [75] | Das et al. 2002 | 2000–2001 | India | 566 children | Point | 5–12 years | 28.6 |
| [76] | Sekhar et al. 2009 | 2005–2006 | India | 1000 children | Point | <2 years | 11.2 |
| [73] | Gessner et al. 1998 | NR | Indonesia | 484 children | Point | 0–24 months | 4.6 (3.7–5.5)c |
| [36] | Vu et al. 2011 | 2007–2008 | Vietnam | 350 children | Point | <5 years | 31.4 |
| Immunocompromised population | |||||||
| [70] | Bhattacharya et al. 2012 | 2008–2009 | India | 148 children with HIV | Point | 1–16 years | 24 |
| [71] | Mwenya et al. 2010 | 2002–2003 | Zambia | 439 children with HIV | Point | 6 months–14 years | 29 |
| Sick population | |||||||
| [62] | Mastro et al. 1993 | 1989–1990 | Pakistan | 601 children with ARI | Point | Mean:14.5 months | 36.6 |
| [61] | Lupisan et al. 2000 | 1994 | The Philippines | 956 children with severe pneumonia, suspected meningitis, or clinical suspicion of sepsis | Point | 0–59 months | 15.2 |
| [36] | Vu et al. 2011 | 2007–2008 | Vietnam | 274 children with radiologically confirmed pneumonia | Point | <5 years | 50 |
| 276 children with other LRTI | 53.5 | ||||||
ARI, acute respiratory infection; HIV, human immunodeficiency virus; LRTI, lower respiratory tract infection; NR, not reported.
All carriage rates are from the control group.
Post-vaccination data.
Age- and population-weighted carriage rate, adjusted for design effect.
Nine studies reported distributions for individual H. influenzae serotypes, including one conducted after introduction of the Hib vaccine [55]. Three focused on carriage of Hib [72]–[74]. The prevalence of Hib carriage was approximately 5% in these studies, with the highest prevalence (10.9%) in rural children [72]–[74]. The percentage of H. influenzae isolates that belonged to serotype b was 0.7%–69% in healthy children [43], [55], [73]–[76], 0.9%–18% in sick children [61], [62], [77], and 49% in immunocompromised children [70]. Non-typeable H. influenzae were isolated frequently in studies in which serotyping of H. influenzae was undertaken (31%–96.4% of all isolates) [55], [62], [76], except for one study in Nepalese children that reported a prevalence of non-typeable H. influenzae of only 1.5% based on oropharyngeal swabs [74].
Carriage of Moraxella catarrhalis
Only three studies reported prevalence of M. catarrhalis carriage (Table 3, Table S5) [36], [43], [78]. The highest carriage rate (71%) in healthy subjects was found in a longitudinal study in infants in The Gambia [43] which used PCR. In a study of M. catarrhalis carriage detected by microbiological methods in both nasopharyngeal and oropharyngeal samples, carriage prevalence was higher in children (31.4%–38.5%) than in adults (11.7%) [78]. Two of these studies also reported the prevalence of carriage of M. catarrhalis in an ill population [36], [78]. In Yemen, the prevalence in children with sinusitis was lower than in children with otitis media or tonsillitis/pharyngitis [78]. However, this study included only 64 ill children. In Vietnam, the prevalence of M. catarrhalis carriage in children <5 years of age with RCP was 28.1% compared to a prevalence of 42.2% in children with other lower RTIs (P = 0.001) [36].
Table 3. Summary table of studies reporting carriage of Moraxella catarrhalis.
| Reference | Study period | Country | Sample size | Prevalence | Age group | Prevalence of carriage, % (95% CI) | |
| Low income countries | |||||||
| Healthy population | |||||||
| [43] | Kwambana et al. 2011 | NR | The Gambia | 30 infants | Average | 0–12 months | 71 (67–75) |
| Immunocompromised population | |||||||
| No data found | |||||||
| Sick population | |||||||
| No data found | |||||||
| Lower-middle income countries | |||||||
| Healthy population | |||||||
| [36] | Vu et al. 2011 | 2007–2008 | Vietnam | 350 children | Point | <5 years | 58 |
| [78] | Sehgal et al. 1994 | 1992–1993 | Yemen | 35 children | Point | <3 years | 31.4 |
| 96 school children | 4–12 years | 38.5 | |||||
| 120 university students and staff | 20–40 years | 11.7 | |||||
| Immunocompromised population | |||||||
| No data found | |||||||
| Sick population | |||||||
| [36] | Vu et al. 2011 | 2007–2008 | Vietnam | 274 children with radiologically confirmed pneumonia | Point | <5 years | 28.1 |
| 276 children with other LRTI | 42.2 | ||||||
| [78] | Sehgal et al. 1994 | 1992–1993 | Yemen | 64 children with respiratory infections: | Point | 3–12 years | 21.9 |
| - OM | 26.9 | ||||||
| - Sinusitis | 9.1 | ||||||
| - Tonsillitis/Pharyngitis | 22.2 | ||||||
LRTI, lower respiratory tract infection; NR, not reported; OM, otitis media.
Carriage of Staphylococcus aureus
Four studies reported prevalence of S. aureus carriage (Table 4, Table S6) [43], [70], [79], [80]. All included nasopharyngeal samples. A longitudinal study in The Gambia found an average prevalence of nasopharyngeal S. aureus carriage of 20% in healthy infants [43]. The prevalence of carriage was highest in neonates and decreased with age (from 50% to 10%), in contrast to the prevalence of carriage of S. pneumoniae, H. influenzae, and M. catarrhalis, which increased with age during the first year of life [43]. In a second study in Pakistan, 14.8% of subjects of all ages carried S. aureus, without a statistically significant difference between age groups [80]. Similar prevalences of carriage of S. aureus were reported for two immunocompromised populations, HIV-infected adults in a low income country (27%) and HIV-infected children ≤16 years in a lower-middle income country (26%) [70], [79]. The prevalence of S. aureus carriage in an ill population (with IPD, AOM, RTI, or sinusitis) has not been reported.
Table 4. Summary table of studies reporting carriage of Staphylococcus aureus.
| Reference | Study period | Country | Sample size | Prevalence | Age group | Prevalence of carriage, % (95% CI) | |
| Low income countries | |||||||
| Healthy population | |||||||
| [43] | Kwambana et al. 2011 | NR | The Gambia | 30 infants | Average | 0–12 months | 20 (16–24) |
| Immunocompromised population | |||||||
| [79] | Amir et al. 1995 | 1992 | Kenya | 264 adults with HIV | Point | NR | 27 |
| Sick population | |||||||
| No data found | |||||||
| Lower-middle income countries | |||||||
| Healthy population | |||||||
| [80] | Anwar et al. 2004 | 2002–2003 | Pakistan | 1660 individuals | Point | All ages | 14.8 |
| Immunocompromised population | |||||||
| [70] | Bhattacharya et al. 2012 | 2008–2009 | India | 148 children with HIV | Point | 1–16 years | 26 |
| Sick population | |||||||
| No data found | |||||||
HIV, human immunodeficiency virus; NR, not reported.
Carriage of Neisseria meningitidis
Nine studies analyzed prevalence of N. meningitidis carriage, all in healthy populations (Table S7). Four studies used oropharyngeal samples, three used nasopharyngeal samples, one used both oropharyngeal and nasopharyngeal samples, and one used pharyngeal samples. Carriage rates ranged from 3.17% to 22% in low income countries [81]–[86] and from 1.64% to 6.2% in lower-middle income countries [87]–[89]. However, most studies included both children and adults, and only one described the prevalence of N. meningitidis carriage in young children (0.78% in children aged 3–24 months in western Democratic Republic of Congo) [81], the main target age group of this review. In addition, previous reviews suggest that infants and young children are unlikely to carry N. meningitidis [25], [90]. For these reasons, the results of the systematic search for this pathogen are not described further in this review.
Risk factors for carriage
Twenty-five studies evaluated possible risk factors for carriage of S. pneumoniae. Among healthy subjects, seasonality was identified as a risk factor for S. pneumoniae carriage in Kenya [51], [55], whereas day care attendance was identified as a risk factor in the Gaza strip [56]. Conflicting results were reported for several risk factors, including age, living in crowded conditions or a rural area, co-carriage with other pathogens, RTIs, or HIV infection. Co-carriage with H. influenzae was the only significant risk factor identified in an immunocompromised population [70], whereas an age >2 months and no previous antibiotic use were identified as risk factors for carriage in subjects with IPD, AOM, sinusitis, or RTI [60], [61].
For carriage of H. influenzae, risk factors were an age >2 months, co-colonization with S. pneumoniae, and the winter or rainy season [55], [76]. Risk factors reported for carriage with S. aureus were living in an urban setting and HIV infection [79], [80]. Risk factors for carriage of M. catarrhalis were not reported in any study.
Association between carriage and disease
An association between carriage and disease was analyzed in only two studies. One study, conducted in India, linked S. pneumoniae carriage to RTIs [67]. Children with six or more episodes of upper RTI had a higher percentage of pneumococcal-positive swabs than children who had less than three upper RTI episodes (60% vs. 17.2%; P<0.001). In multivariate analysis, significant risk factors for upper RTIs in the first year of life were nasopharyngeal carriage of S. pneumoniae, winter season, and a lower socioeconomic status of the parents [67]. The other study, conducted in The Gambia, linked serotype-specific carriage of S. pneumoniae to IPD [39]. In 43 of 56 (76.8%) children with IPD, pneumococci isolated from the nasopharynx and from the blood or other sterile site belonged to the same serotype.
Bacterial density
Only two studies analyzed the density of bacterial carriage [35], [36]. In a group of villages in which only children <30 months of age received PCV-7, the density of pneumococcal carriage (expressed as arbitrary units ranging from 1 to 4) decreased from 2.76 to 1.99 (p = 0.002) in children ≤5 years and from 2.44 to 1.75 (p = 0.001) in individuals >5 years, suggesting naturally acquired immunity [35].
The second study reported the density of S. pneumoniae, H. influenzae, and M. catarrhalis in healthy children, children with RCP, and children with other lower RTIs [36]. The bacterial load of S. pneumoniae in the nasopharynx, calculated as genome equivalent/mL sample secretion, was higher in children with RCP (7.8×106/mL) than in children with other lower RTIs (1.3×106/mL; p<0.0001) and healthy children (7.9×105/mL; p<0.0001). M. catarrhalis bacterial load was higher in children with RCP (2.5×107/mL) and other lower RTIs (3.3×107/mL) than in healthy children (5.5×106/mL; p<0.0001). H. influenzae bacterial load was lower in children with other lower RTIs than in children with RCP (p = 0.003) but there was no significant difference between healthy children and children with RCP [36].
Impact of vaccination on carriage
Five studies, all in The Gambia, analyzed the impact of pneumococcal vaccination on S. pneumoniae carriage rate and serotype distribution (Table S8) [35], [42], [46], [47], [53]. All of these studies were performed before PCV7 was introduced into the Gambian national childhood immunization program in 2009 [91]. Cheung et al. reported similar total carriage rates for children who had received the 9-valent PCV (PCV-9; 87.5%) and those who had received a placebo vaccine (86.2%) [42]. However, compared to placebo-vaccinated children, PCV-9-vaccinated children were less likely to carry a VT pneumococcus (22.6% vs. 40.0%; relative risk = 0.56; 95% CI, 0.49–0.65) and more likely to carry a NVT pneumococcus (42.7% vs. 26.9%, relative risk = 1.59; 95% CI, 1.41–1.79). Ota et al. analyzed S. pneumoniae carriage rates in 5-, 11-, and 15-month-old children who had received one, two, or three doses of PCV-7 [47]. Carriage rates were similar overall, although carriage rates tended to be higher in children who had received one dose of PCV-7 than in those who had received two or three doses. At 11 months of age, carriage of a VT pneumococcus was more common in children who had received one dose of PCV-7 than in children who had received three doses (20.2% vs. 10.0%, p = 0.005). In a cluster-randomized trial in which children <30 months of age were vaccinated with PCV-7, Roca et al. showed that the overall carriage rate in residents decreased from 71% in the pre-PCV-7 vaccination period to 44% following PCV-7 vaccination [35], [53]. Carriage rates increased with age (age groups: 2–4, 5–14, and ≥15 years), but they did not differ for any age group at any time point between the villages in which all residents received PCV-7 and those in which only children <30 months of age received PCV-7 [53]. The carriage rates of all age groups were lower at the first (4–6 months after vaccination) and second (12 months after vaccination) post-vaccination surveys than at the pre-vaccination survey. However, by the third post-vaccination survey, 22 months after vaccination, carriage rates were higher than at the second survey but still remained below pre-vaccination rates. Finally, Akinsola et al. compared the prevalence of S. pneumoniae carriage in children who had received primary vaccination with PCV-9 followed by a booster dose of PCV-7 and in age-matched children who received only a single dose of PCV-7 [46]. They found no significant differences between the carriage rates or serotype distributions of the two groups at any time point during a 16–18 month follow-up after vaccination. In conclusion, all five studies showed that the prevalence of VT carriage decreased after PCV vaccination, although the extent of the decrease varied between studies.
Two studies reported the impact of Hib vaccination on H. influenzae carriage. In one study, Hib carriage was 11% in fully vaccinated Gambian children who had received the diphtheria-tetanus-pertussis vaccine alone (control group) compared to only 4.4% for fully vaccinated children who had received diphtheria-tetanus-pertussis and an Hib conjugate vaccine (p<0.001) [72]. The prevalence of Hib carriage in children who had been partially vaccinated (either in the control or the vaccinated groups) was higher than in children who had received full vaccination. In the second study, conducted in Nepal, none of 27 children <13 years of age who had received at least one dose of the Hib vaccine carried Hib [74].
Discussion
This systematic review of the literature fills an important gap in knowledge on the carriage of five key pathogens in low and lower-middle income countries. The review found that nasopharyngeal carriage was frequent in these countries. The prevalences of carriage for S. pneumoniae, H. influenzae, and M. catarrhalis were generally higher in low income countries than in lower-middle income countries and were generally higher in children than in adults. The prevalence of S. aureus carriage was highest in neonates.
In low and lower-middle income countries, the prevalence of pneumococcal carriage was high in young children (up to 93.4% in children 2–4 years of age). Furthermore, carriage was acquired within the first months of life and persisted in older children and adults, although at lower levels [50], [51], [53], [54]. In contrast, in upper-middle and high income countries, the highest prevalence of pneumococcal nasopharyngeal carriage recorded was 58% (in healthy children <3 years of age) [92]. This difference could be due to the frequent overcrowded living conditions in developing countries. This view is supported by the high prevalence of carriage found among children living in orphanages or attending day-care centers in industrialized countries and among indigenous populations [93]–[96]. Malnutrition, more common in the developing countries, could also favor carriage and disease, as previously suggested [97].
In addition to a high prevalence of S. pneumoniae carriage, young children also have a higher pneumococcal density in the nasopharynx than older individuals [35]. This may partly explain why children are more efficient than adults at transmitting S. pneumoniae. The lower density in adults may be due to the progressive acquisition of immunity, less frequent close contact between individuals, better hygiene, or a combination of these factors. IPD is probably also a substantial public health problem for adults in many developing countries [98], particularly for countries with a high incidence of HIV [99]–[101], but this has not been well documented. As life expectancy increases in these countries, the proportion of the adult population with risk factors for IPD, such as diabetes, cardiovascular diseases, and chronic RTIs, is increasing [102]. It is hoped that an indirect effect of pediatric pneumococcal vaccination, through reduced carriage of VT pneumococci, will also be seen in these at risk populations, as it has occurred in the US and Europe [5], [8], [13] but this will occur only if the major route of pneumococcal transmission in these countries is from young children to adults. There is currently little information to support this expectation but longitudinal studies in Kenya and rural Gambia have suggested that intra-household transmission is more important than community transmission and that young children commonly introduce S. pneumoniae into the household, with subsequent spread to other children and adults [51], [54]. Vaccinations strategies against pneumococcal disease need to target young children, but a strong case can be made for catch-up campaigns in older children in developing countries because children up to nine years of age can effectively transmit S. pneumoniae [51].
The review has shown that residents of low and lower-middle income countries carry a wide variety of pneumococcal serotypes. Identifying clear trends in the serotype distributions was challenging due to the disparate geographic regions represented and to large variations in the types of studies reviewed and sets of serotypes analyzed in each study. Despite this, the five most common serotypes reported (6A, 6B, 14, 19F, and 23F) are among the seven serotypes that globally cause most IPD in children worldwide [103]. The two other serotypes, 1 and 5, are rarely isolated in carriage studies, although they have been found in epidemics of invasive pneumococcal disease [3], [104], [105]. All these serotypes are included in the two second generation PCVs – PHiD-CV and PCV-13.
Studies in industrialized countries have established a temporal association between pneumococcal carriage and disease, especially for AOM. We found only limited data on associations between disease and carriage in low and lower-middle income countries, although associations between S. pneumoniae and both IPD and RTIs have been described [39], [67].
Few carriage studies have analyzed more than one pathogen and the interactions between them. In The Gambia, approximately 90% of infants co-carried S. pneumoniae with at least one other pathogen, most often H. influenzae or M. catarrhalis [43]. Co-infections with multiple pathogens can subvert mucosal immune responses to carriage in the upper respiratory tract and can alter disease outcome [106]. In contrast, an inverse association has been found between S. pneumoniae and S. aureus [21], [28], [29], [106]. However, most studies do not consider that risk factors for these infections may be different and that bacterial interactions within the nasopharynx may influence the prevalence of carriage with individual bacteria.
Only five studies included PCV-vaccinated populations and two studies included Hib-vaccinated populations. Results were conflicting for the impact of PCV vaccination on the overall pneumococcal carriage, although all studies showed that the prevalence of VT carriage decreased after PCV vaccination and that the prevalence of Hib carriage decreased after Hib vaccination. A long-term follow-up of the village-randomized study of PCV-7 in The Gambia found that the decrease in VT carriage was sustained four years after vaccination and that carriage of NVT pneumococci did not significantly increase [107]. Also, PCV-7 indirectly reduced carriage of VT pneumococci in unvaccinated infants <8 weeks of age [108]. More data will be available on the long-term impact of PCV immunization as the use of these vaccines continues to increase in lower income countries.
The results of this review need to be interpreted in light of several considerations. S. pneumoniae was the only pathogen for which prevalence of carriage was available for all three subpopulations (healthy, immunocompromised, and ill). Heterogeneity between studies may also have hampered direct comparisons. For instance, differences were noted in study design, the definition of prevalence, sampling technique, laboratory methods, the type of sample, and the period between sample collection and vaccination. Notably, not all the studies of S. pneumoniae followed the WHO recommendations for measuring nasopharyngeal carriage [44], [45]. Nasopharyngeal and oropharyngeal swabs were used in the studies, both of which differ in sensitivity for detecting respiratory pathogens [109], [110]. Also, some standard methods for bacterial identification do not reliably distinguish H. influenzae from H. haemolyticus, a respiratory tract commensal [111]. In addition, variation between studies may be due in part to the type of settings where a study was done. Indeed, several studies included children from outpatient clinics, and selection bias is usually higher in these settings than in studies including children from the community. Studies in the low income countries were highly heterogeneous (I2 = 98%), so that the pooled estimate for pneumococcal carriage should be interpreted with caution, as it reflects only findings from countries where carriage studies have been published. In contrast, heterogeneity was low between studies from the lower-middle income countries (I2 = 0%). We were unable to perform a meta-analysis for H. influenzae, S. aureus, and M. catarrhalis because of the few studies available. Most studies included in this review had a cross-sectional design, which prevents assessing the effect of season on prevalence of carriage. Finally, because seasonality is a risk factor for carriage for S. pneumoniae and the other pathogens [51], [55], [76], it might be a confounding factor in comparisons of carriage rates between different studies.
None of the studies included in the review were from Central or South America, the Caribbean, or Europe due to the absence of any publications that met the inclusion criteria. In addition, we did not include upper-middle income countries in the analysis even though some populations within these countries may share characteristics with populations in low or lower-middle income countries. For instance, in one study in South Africa, prevalence of pneumococcal carriage was high (22.5%–61.0%) in children younger than five years of age [112], whereas a study in Costa Rica showed that infants acquire nasopharyngeal carriage of S. pneumoniae at a rate (3.1% at one month of age and 19.4% at one year of age) comparable to that seen in developed countries [113].
Conclusions
With support from the GAVI Alliance, PCVs of higher valencies are being rapidly introduced into the Expanded Programme on Immunization of low and lower-middle income countries [2], [31]. In the large number of countries where large-scale PCV vaccination is being introduced careful surveillance of IPD is needed. However, due to limited resources, population-based IPD surveillance systems similar to those in the industrialized countries will probably not be possible in most low and lower-middle income countries. Because carriage surveys are relatively cheap and possible compared to population-based IPD surveillance, carriage data could be used instead to indirectly monitor vaccine herd effects and serotype replacement after the introduction of PCVs [114] and in the process for future vaccine licensure [115]. However, the relevance of carriage studies for serotype replacement still needs to be properly assessed, because in many countries, although replacement in carriage is complete, the replacement in disease is small [7], [8], [14], [16], [17]. Because the dynamics of carriage within populations are complex, carefully designed multi-year, longitudinal carriage studies will be needed.
Our systematic review found high prevalences of bacterial carriage in children from low and lower-middle income countries. Although data were limited, we expect that the introduction of routine immunization programs against S. pneumoniae, H. influenzae, and N. meningitidis will help reduce the burden of infectious diseases in these countries and that studies of the effects on carriage may provide important data that can be used to understand overall vaccine effectiveness.
Supporting Information
PRISMA 2009 checklist.
(DOCX)
Details of studies reporting carriage of Streptococcus pneumoniae .
(DOCX)
Studies reporting carriage of individual pneumococcal serotypes or serogroups.
(DOCX)
Details of studies reporting carriage of Haemophilus influenzae .
(DOCX)
Details of studies reporting carriage of Moraxella catarrhalis .
(DOCX)
Details of studies reporting carriage of Staphylococcus aureus .
(DOCX)
Details of studies reporting carriage of Neisseria meningitidis .
(DOCX)
Impact of vaccination on Streptococcus pneumoniae carriage by age.
(DOCX)
Supplementary methods.
(DOCX)
Protocol of the systematic review.
(PDF)
Acknowledgments
The authors thank Pallas Health Research and Consultancy (The Netherlands) for assistance with the systematic review. Writing assistance was provided by Dr Julie Harriague (4Clinics, France) and manuscript coordination by Dr Abdelilah Ibrahimi (XPE Pharma & Science c/o GlaxoSmithKline Vaccines).
Funding Statement
GSK Biologicals SA paid for all costs associated with the development and the publishing of the present manuscript. The sponsor contributed to all stages of the study, including study design, data analyses, data interpretation, and the writing of this report.
References
- 1.World Health Organization (2012) Estimated Hib and pneumococcal deaths for children under 5 years of age, 2008.
- 2. O'Brien KL, Goldblatt D, Whitney CG (2014) Why do we need a systematic review of pneumococcal conjugate vaccine dosing schedules? Pediatr Infect Dis J 33 Suppl 2S107–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Simell B, Auranen K, Kayhty H, Goldblatt D, Dagan R, et al. (2012) The fundamental link between pneumococcal carriage and disease. Expert Rev Vaccines 11: 841–855. [DOI] [PubMed] [Google Scholar]
- 4. Whitney CG, Pilishvili T, Farley MM, Schaffner W, Craig AS, et al. (2006) Effectiveness of seven-valent pneumococcal conjugate vaccine against invasive pneumococcal disease: a matched case-control study. Lancet 368: 1495–1502. [DOI] [PubMed] [Google Scholar]
- 5. Miller E, Andrews NJ, Waight PA, Slack MP, George RC (2011) Herd immunity and serotype replacement 4 years after seven-valent pneumococcal conjugate vaccination in England and Wales: an observational cohort study. Lancet Infect Dis 11: 760–768. [DOI] [PubMed] [Google Scholar]
- 6. Kellner JD, Vanderkooi OG, MacDonald J, Church DL, Tyrrell GJ, et al. (2009) Changing epidemiology of invasive pneumococcal disease in Canada, 1998–2007: update from the Calgary-area Streptococcus pneumoniae research (CASPER) study. Clin Infect Dis 49: 205–212. [DOI] [PubMed] [Google Scholar]
- 7. Isaacman DJ, McIntosh ED, Reinert RR (2010) Burden of invasive pneumococcal disease and serotype distribution among Streptococcus pneumoniae isolates in young children in Europe: impact of the 7-valent pneumococcal conjugate vaccine and considerations for future conjugate vaccines. Int J Infect Dis 14: e197–209. [DOI] [PubMed] [Google Scholar]
- 8. Pilishvili T, Lexau C, Farley MM, Hadler J, Harrison LH, et al. (2010) Sustained reductions in invasive pneumococcal disease in the era of conjugate vaccine. J Infect Dis 201: 32–41. [DOI] [PubMed] [Google Scholar]
- 9.Martinelli D, Pedalino B, Cappelli MG, Caputi G, Sallustio A, et al.. (2013) Towards the 13-valent pneumococcal conjugate universal vaccination: Effectiveness in the transition era between PCV7 and PCV13 in Italy, 2010–2013. Hum Vaccin Immunother 10. [DOI] [PMC free article] [PubMed]
- 10.Steens A, Bergsaker MA, Aaberge IS, Ronning K, Vestrheim DF (2013) Prompt effect of replacing the 7-valent pneumococcal conjugate vaccine with the 13-valent vaccine on the epidemiology of invasive pneumococcal disease in Norway. Vaccine. [DOI] [PubMed]
- 11. De Wals P, Lefebvre B, Defay F, Deceuninck G, Boulianne N (2012) Invasive pneumococcal diseases in birth cohorts vaccinated with PCV-7 and/or PHiD-CV in the province of Quebec, Canada. Vaccine 30: 6416–6420. [DOI] [PubMed] [Google Scholar]
- 12. Whitney CG, Farley MM, Hadler J, Harrison LH, Bennett NM, et al. (2003) Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. N Engl J Med 348: 1737–1746. [DOI] [PubMed] [Google Scholar]
- 13. Millar EV, Watt JP, Bronsdon MA, Dallas J, Reid R, et al. (2008) Indirect effect of 7-valent pneumococcal conjugate vaccine on pneumococcal colonization among unvaccinated household members. Clin Infect Dis 47: 989–996. [DOI] [PubMed] [Google Scholar]
- 14. Flasche S, Slack M, Miller E (2011) Long term trends introduce a potential bias when evaluating the impact of the pneumococcal conjugate vaccination programme in England and Wales. Euro Surveill 16: 19868. [PubMed] [Google Scholar]
- 15. Davis SM, Deloria-Knoll M, Kassa HT, O'Brien KL (2013) Impact of pneumococcal conjugate vaccines on nasopharyngeal carriage and invasive disease among unvaccinated people: review of evidence on indirect effects. Vaccine 32: 133–145. [DOI] [PubMed] [Google Scholar]
- 16. Huang SS, Platt R, Rifas-Shiman SL, Pelton SI, Goldmann D, et al. (2005) Post-PCV7 changes in colonizing pneumococcal serotypes in 16 Massachusetts communities, 2001 and 2004. Pediatrics 116: e408–413. [DOI] [PubMed] [Google Scholar]
- 17. O'Brien KL, Millar EV, Zell ER, Bronsdon M, Weatherholtz R, et al. (2007) Effect of pneumococcal conjugate vaccine on nasopharyngeal colonization among immunized and unimmunized children in a community-randomized trial. J Infect Dis 196: 1211–1220. [DOI] [PubMed] [Google Scholar]
- 18. Choi YH, Jit M, Gay N, Andrews N, Waight PA, et al. (2011) 7-Valent pneumococcal conjugate vaccination in England and Wales: is it still beneficial despite high levels of serotype replacement? PLoS One 6: e26190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Feikin DR, Kagucia EW, Loo JD, Link-Gelles R, Puhan MA, et al. (2013) Serotype-specific changes in invasive pneumococcal disease after pneumococcal conjugate vaccine introduction: a pooled analysis of multiple surveillance sites. PLoS Med 10: e1001517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wenger JD, Zulz T, Bruden D, Singleton R, Bruce MG, et al. (2010) Invasive pneumococcal disease in Alaskan children: impact of the seven-valent pneumococcal conjugate vaccine and the role of water supply. Pediatr Infect Dis J 29: 251–256. [DOI] [PubMed] [Google Scholar]
- 21. Dunne EM, Smith-Vaughan HC, Robins-Browne RM, Mulholland EK, Satzke C (2013) Nasopharyngeal microbial interactions in the era of pneumococcal conjugate vaccination. Vaccine 31: 2333–2342. [DOI] [PubMed] [Google Scholar]
- 22. Verduin CM, Hol C, Fleer A, van Dijk H, van Belkum A (2002) Moraxella catarrhalis: from emerging to established pathogen. Clin Microbiol Rev 15: 125–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Agrawal A, Murphy TF (2011) Haemophilus influenzae infections in the H. influenzae type b conjugate vaccine era. J Clin Microbiol 49: 3728–3732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wertheim HF, Melles DC, Vos MC, van Leeuwen W, van Belkum A, et al. (2005) The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect Dis 5: 751–762. [DOI] [PubMed] [Google Scholar]
- 25. Christensen H, May M, Bowen L, Hickman M, Trotter CL (2010) Meningococcal carriage by age: a systematic review and meta-analysis. Lancet Infect Dis 10: 853–861. [DOI] [PubMed] [Google Scholar]
- 26. Casey JR, Adlowitz DG, Pichichero ME (2010) New patterns in the otopathogens causing acute otitis media six to eight years after introduction of pneumococcal conjugate vaccine. Pediatr Infect Dis J 29: 304–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wiertsema SP, Kirkham LA, Corscadden KJ, Mowe EN, Bowman JM, et al. (2011) Predominance of nontypeable Haemophilus influenzae in children with otitis media following introduction of a 3+0 pneumococcal conjugate vaccine schedule. Vaccine 29: 5163–5170. [DOI] [PubMed] [Google Scholar]
- 28. Regev-Yochay G, Dagan R, Raz M, Carmeli Y, Shainberg B, et al. (2004) Association between carriage of Streptococcus pneumoniae and Staphylococcus aureus in Children. JAMA 292: 716–720. [DOI] [PubMed] [Google Scholar]
- 29. Bogaert D, van Belkum A, Sluijter M, Luijendijk A, de Groot R, et al. (2004) Colonisation by Streptococcus pneumoniae and Staphylococcus aureus in healthy children. Lancet 363: 1871–1872. [DOI] [PubMed] [Google Scholar]
- 30. Pollard AJ, Perrett KP, Beverley PC (2009) Maintaining protection against invasive bacteria with protein-polysaccharide conjugate vaccines. Nat Rev Immunol 9: 213–220. [DOI] [PubMed] [Google Scholar]
- 31. Centers for Disease Control and Prevention (2013) Progress in introduction of pneumococcal conjugate vaccine - worldwide, 2000–2012. MMWR Morb Mortal Wkly Rep 62: 308–311. [PMC free article] [PubMed] [Google Scholar]
- 32.The World Bank (2012) Country and lending groups.
- 33. Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Fervers B, Remy-Stockinger M, Mazeau-Woynar V, Otter R, Liberati A, et al. (2008) CoCanCPG. Coordination of cancer clinical practice in Europe. Tumori 94: 154–159. [DOI] [PubMed] [Google Scholar]
- 35. Roca A, Bottomley C, Hill PC, Bojang A, Egere U, et al. (2012) Effect of age and vaccination with a pneumococcal conjugate vaccine on the density of pneumococcal nasopharyngeal carriage. Clin Infect Dis 55: 816–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Vu HT, Yoshida LM, Suzuki M, Nguyen HA, Nguyen CD, et al. (2011) Association between nasopharyngeal load of Streptococcus pneumoniae, viral coinfection, and radiologically confirmed pneumonia in Vietnamese children. Pediatr Infect Dis J 30: 11–18. [DOI] [PubMed] [Google Scholar]
- 37. DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7: 177–188. [DOI] [PubMed] [Google Scholar]
- 38. Coles CL, Sherchand JB, Khatry SK, Katz J, Leclerq SC, et al. (2008) Zinc modifies the association between nasopharyngeal Streptococcus pneumoniae carriage and risk of acute lower respiratory infection among young children in rural Nepal. J Nutr 138: 2462–2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lloyd-Evans N, O'Dempsey TJ, Baldeh I, Secka O, Demba E, et al. (1996) Nasopharyngeal carriage of pneumococci in Gambian children and in their families. Pediatr Infect Dis J 15: 866–871. [DOI] [PubMed] [Google Scholar]
- 40. Blossom DB, Namayanja-Kaye G, Nankya-Mutyoba J, Mukasa JB, Bakka H, et al. (2006) Oropharyngeal colonization by Streptococcus pneumoniae among HIV-infected adults in Uganda: assessing prevalence and antimicrobial susceptibility. Int J Infect Dis 10: 458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Anthony L, Meehan A, Amos B, Mtove G, Mjema J, et al. (2012) Nasopharyngeal carriage of Streptococcus pneumoniae: prevalence and risk factors in HIV-positive children in Tanzania. Int J Infect Dis 16: e753–757. [DOI] [PubMed] [Google Scholar]
- 42. Cheung YB, Zaman SM, Nsekpong ED, Van Beneden CA, Adegbola RA, et al. (2009) Nasopharyngeal carriage of Streptococcus pneumoniae in Gambian children who participated in a 9-valent pneumococcal conjugate vaccine trial and in their younger siblings. Pediatr Infect Dis J 28: 990–995. [DOI] [PubMed] [Google Scholar]
- 43. Kwambana BA, Barer MR, Bottomley C, Adegbola RA, Antonio M (2011) Early acquisition and high nasopharyngeal co-colonisation by Streptococcus pneumoniae and three respiratory pathogens amongst Gambian new-borns and infants. BMC Infect Dis 11: 175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Satzke C, Turner P, Virolainen-Julkunen A, Adrian PV, Antonio M, et al. (2013) Standard method for detecting upper respiratory carriage of Streptococcus pneumoniae: updated recommendations from the World Health Organization Pneumococcal Carriage Working Group. Vaccine 32: 165–179. [DOI] [PubMed] [Google Scholar]
- 45. O'Brien KL, Nohynek H (2003) World Health Organization Pneumococcal Vaccine Trials Carraige Working G (2003) Report from a WHO working group: standard method for detecting upper respiratory carriage of Streptococcus pneumoniae. Pediatr Infect Dis J 22: 133–140. [DOI] [PubMed] [Google Scholar]
- 46. Akinsola AK, Ota MO, Enwere GC, Okoko BJ, Zaman SM, et al. (2012) Pneumococcal antibody concentrations and carriage of pneumococci more than 3 years after infant immunization with a pneumococcal conjugate vaccine. PLoS One 7: e31050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ota MO, Akinsola A, Townend J, Antonio M, Enwere G, et al. (2011) The immunogenicity and impact on nasopharyngeal carriage of fewer doses of conjugate pneumococcal vaccine immunization schedule. Vaccine 29: 2999–3007. [DOI] [PubMed] [Google Scholar]
- 48. Bogaert D, Ha NT, Sluijter M, Lemmens N, De Groot R, et al. (2002) Molecular epidemiology of pneumococcal carriage among children with upper respiratory tract infections in Hanoi, Vietnam. J Clin Microbiol 40: 3903–3908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Granat SM, Mia Z, Ollgren J, Herva E, Das M, et al. (2007) Longitudinal study on pneumococcal carriage during the first year of life in Bangladesh. Pediatr Infect Dis J 26: 319–324. [DOI] [PubMed] [Google Scholar]
- 50. Hill PC, Cheung YB, Akisanya A, Sankareh K, Lahai G, et al. (2008) Nasopharyngeal carriage of Streptococcus pneumoniae in Gambian infants: a longitudinal study. Clin Infect Dis 46: 807–814. [DOI] [PubMed] [Google Scholar]
- 51. Tigoi CC, Gatakaa H, Karani A, Mugo D, Kungu S, et al. (2012) Rates of acquisition of pneumococcal colonization and transmission probabilities, by serotype, among newborn infants in Kilifi District, Kenya. Clin Infect Dis 55: 180–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Abdullahi O, Karani A, Tigoi CC, Mugo D, Kungu S, et al. (2012) Rates of acquisition and clearance of pneumococcal serotypes in the nasopharynges of children in Kilifi District, Kenya. J Infect Dis 206: 1020–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Roca A, Hill PC, Townend J, Egere U, Antonio M, et al. (2011) Effects of community-wide vaccination with PCV-7 on pneumococcal nasopharyngeal carriage in the Gambia: a cluster-randomized trial. PLoS Med 8: e1001107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Hill PC, Townend J, Antonio M, Akisanya B, Ebruke C, et al. (2010) Transmission of Streptococcus pneumoniae in rural Gambian villages: a longitudinal study. Clin Infect Dis 50: 1468–1476. [DOI] [PubMed] [Google Scholar]
- 55. Abdullahi O, Nyiro J, Lewa P, Slack M, Scott JA (2008) The descriptive epidemiology of Streptococcus pneumoniae and Haemophilus influenzae nasopharyngeal carriage in children and adults in Kilifi district, Kenya. Pediatr Infect Dis J 27: 59–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Regev-Yochay G, Abullaish I, Malley R, Shainberg B, Varon M, et al. (2012) Streptococcus pneumoniae carriage in the Gaza strip. PLoS One 7: e35061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hill PC, Akisanya A, Sankareh K, Cheung YB, Saaka M, et al. (2006) Nasopharyngeal carriage of Streptococcus pneumoniae in Gambian villagers. Clin Infect Dis 43: 673–679. [DOI] [PubMed] [Google Scholar]
- 58. Abdullahi O, Karani A, Tigoi CC, Mugo D, Kungu S, et al. (2012) The prevalence and risk factors for pneumococcal colonization of the nasopharynx among children in Kilifi District, Kenya. PLoS One 7: e30787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Kateete DP, Kajumbula H, Kaddu-Mulindwa DH, Ssevviri AK (2012) Nasopharyngeal carriage rate of Streptococcus pneumoniae in Ugandan children with sickle cell disease. BMC Res Notes 5: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lankinen KS, Leinonen M, Tupasi TE, Haikala R, Ruutu P (1994) Pneumococci in nasopharyngeal samples from Filipino children with acute respiratory infections. J Clin Microbiol 32: 2948–2952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Lupisan SP, Herva E, Sombrero LT, Quiambao BP, Capeding MR, et al. (2000) Invasive bacterial infections of children in a rural province in the central Philippines. Am J Trop Med Hyg 62: 341–346. [DOI] [PubMed] [Google Scholar]
- 62. Mastro TD, Nomani NK, Ishaq Z, Ghafoor A, Shaukat NF, et al. (1993) Use of nasopharyngeal isolates of Streptococcus pneumoniae and Haemophilus influenzae from children in Pakistan for surveillance for antimicrobial resistance. Pediatr Infect Dis J 12: 824–830. [DOI] [PubMed] [Google Scholar]
- 63. Moyo SJ, Steinbakk M, Aboud S, Mkopi N, Kasubi M, et al. (2012) Penicillin resistance and serotype distribution of Streptococcus pneumoniae in nasopharyngeal carrier children under 5 years of age in Dar es Salaam, Tanzania. J Med Microbiol 61: 952–959. [DOI] [PubMed] [Google Scholar]
- 64. Valles X, Flannery B, Roca A, Mandomando I, Sigauque B, et al. (2006) Serotype distribution and antibiotic susceptibility of invasive and nasopharyngeal isolates of Streptococcus pneumoniae among children in rural Mozambique. Trop Med Int Health 11: 358–366. [DOI] [PubMed] [Google Scholar]
- 65. Saha SK, Baqui AH, Darmstadt GL, Ruhulamin M, Hanif M, et al. (2003) Comparison of antibiotic resistance and serotype composition of carriage and invasive pneumococci among Bangladeshi children: implications for treatment policy and vaccine formulation. J Clin Microbiol 41: 5582–5587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Denno DM, Frimpong E, Gregory M, Steele RW (2002) Nasopharyngeal carriage and susceptibility patterns of Streptococcus pneumoniae in Kumasi, Ghana. West Afr J Med 21: 233–236. [PubMed] [Google Scholar]
- 67. Rupa V, Isaac R, Manoharan A, Jalagandeeswaran R, Thenmozhi M (2012) Risk factors for upper respiratory infection in the first year of life in a birth cohort. Int J Pediatr Otorhinolaryngol 76: 1835–1839. [DOI] [PubMed] [Google Scholar]
- 68. Russell FM, Carapetis JR, Ketaiwai S, Kunabuli V, Taoi M, et al. (2006) Pneumococcal nasopharyngeal carriage and patterns of penicillin resistance in young children in Fiji. Ann Trop Paediatr 26: 187–197. [DOI] [PubMed] [Google Scholar]
- 69. Soewignjo S, Gessner BD, Sutanto A, Steinhoff M, Prijanto M, et al. (2001) Streptococcus pneumoniae nasopharyngeal carriage prevalence, serotype distribution, and resistance patterns among children on Lombok Island, Indonesia. Clin Infect Dis 32: 1039–1043. [DOI] [PubMed] [Google Scholar]
- 70. Bhattacharya SD, Niyogi SK, Bhattacharyya S, Arya BK, Chauhan N, et al. (2012) Associations between potential bacterial pathogens in the nasopharynx of HIV infected children. Indian J Pediatr 79: 1447–1453. [DOI] [PubMed] [Google Scholar]
- 71. Mwenya DM, Charalambous BM, Phillips PP, Mwansa JC, Batt SL, et al. (2010) Impact of cotrimoxazole on carriage and antibiotic resistance of Streptococcus pneumoniae and Haemophilus influenzae in HIV-infected children in Zambia. Antimicrob Agents Chemother 54: 3756–3762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Adegbola RA, Mulholland EK, Secka O, Jaffar S, Greenwood BM (1998) Vaccination with a Haemophilus influenzae type b conjugate vaccine reduces oropharyngeal carriage of H. influenzae type b among Gambian children. J Infect Dis 177: 1758–1761. [DOI] [PubMed] [Google Scholar]
- 73. Gessner BD, Sutanto A, Steinhoff M, Soewignjo S, Widjaya A, et al. (1998) A population-based survey of Haemophilus influenzae type b nasopharyngeal carriage prevalence in Lombok Island, Indonesia. Pediatr Infect Dis J 17: S179–182. [DOI] [PubMed] [Google Scholar]
- 74. Williams EJ, Lewis J, John T, Hoe JC, Yu L, et al. (2011) Haemophilus influenzae type b carriage and novel bacterial population structure among children in urban Kathmandu, Nepal. J Clin Microbiol 49: 1323–1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Das BK, Arora NK, Mathur P, Ostwal P, Mandal S, et al. (2002) Nasopharyngeal carriage of Haemophilus influenzae . Indian J Pediatr 69: 775–777. [DOI] [PubMed] [Google Scholar]
- 76. Sekhar S, Chakraborti A, Kumar R (2009) Haemophilus influenzae colonization and its risk factors in children aged <2 years in northern India. Epidemiol Infect 137: 156–160. [DOI] [PubMed] [Google Scholar]
- 77. Utsunomiya Y, Ahmed K, Rikitomi N, Ruhulamin M, Hanif M, et al. (1998) Isolation of pathogenic bacteria from induced sputum from hospitalized children with pneumonia in Bangladesh. J Trop Pediatr 44: 338–342. [DOI] [PubMed] [Google Scholar]
- 78. Sehgal SC, al Shaimy I (1994) Moraxella catarrhalis in upper respiratory tract of healthy Yemeni children/adults and paediatric patients: detection and significance. Infection 22: 193–196. [DOI] [PubMed] [Google Scholar]
- 79. Amir M, Paul J, Batchelor B, Kariuki S, Ojoo J, et al. (1995) Nasopharyngeal carriage of Staphylococcus aureus and carriage of tetracycline-resistant strains associated with HIV-seropositivity. Eur J Clin Microbiol Infect Dis 14: 34–40. [DOI] [PubMed] [Google Scholar]
- 80. Anwar MS, Jaffery G, Rehman Bhatti KU, Tayyib M, Bokhari SR (2004) Staphylococcus aureus and MRSA nasal carriage in general population. J Coll Physicians Surg Pak 14: 661–664. [PubMed] [Google Scholar]
- 81. Cheesbrough JS, Morse AP, Green SD (1995) Meningococcal meningitis and carriage in western Zaire: a hypoendemic zone related to climate? Epidemiol Infect 114: 75–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Kristiansen PA, Diomande F, Ba AK, Sanou I, Ouedraogo AS, et al. (2013) Impact of the serogroup A meningococcal conjugate vaccine, MenAfriVac, on carriage and herd immunity. Clin Infect Dis 56: 354–363. [DOI] [PubMed] [Google Scholar]
- 83. Kristiansen PA, Diomande F, Wei SC, Ouedraogo R, Sangare L, et al. (2011) Baseline meningococcal carriage in Burkina Faso before the introduction of a meningococcal serogroup A conjugate vaccine. Clin Vaccine Immunol 18: 435–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Mueller JE, Sangare L, Njanpop-Lafourcade BM, Tarnagda Z, Traore Y, et al. (2007) Molecular characteristics and epidemiology of meningococcal carriage, Burkina Faso, 2003. Emerg Infect Dis 13: 847–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Mueller JE, Yaro S, Madec Y, Somda PK, Idohou RS, et al. (2008) Association of respiratory tract infection symptoms and air humidity with meningococcal carriage in Burkina Faso. Trop Med Int Health 13: 1543–1552. [DOI] [PubMed] [Google Scholar]
- 86. Nicolas P, Djibo S, Tenebray B, Castelli P, Stor R, et al. (2007) Populations of pharyngeal meningococci in Niger. Vaccine 25 Suppl 1A53–57. [DOI] [PubMed] [Google Scholar]
- 87. Ichhpujani RL, Mohan R, Grover SS, Joshi PR, Kumari S (1990) Nasopharyngeal carriage of Neisseria meningitidis in general population and meningococcal disease. J Commun Dis 22: 264–268. [PubMed] [Google Scholar]
- 88. Leimkugel J, Hodgson A, Forgor AA, Pfluger V, Dangy JP, et al. (2007) Clonal waves of Neisseria colonisation and disease in the African meningitis belt: eight- year longitudinal study in northern Ghana. PLoS Med 4: e101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Odugbemi T, Ademidun O, Agbabiaka A, Banjo T (1992) Nasopharyngeal carriage of Neisseria meningitidis among school children at Ijede, Lagos State, Nigeria. Ethiop Med J 30: 33–36. [PubMed] [Google Scholar]
- 90. Trotter CL, Greenwood BM (2007) Meningococcal carriage in the African meningitis belt. Lancet Infect Dis 7: 797–803. [DOI] [PubMed] [Google Scholar]
- 91. Mackenzie GA, Plumb ID, Sambou S, Saha D, Uchendu U, et al. (2012) Monitoring the introduction of pneumococcal conjugate vaccines into West Africa: design and implementation of a population-based surveillance system. PLoS Med 9: e1001161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Bogaert D, De Groot R, Hermans PW (2004) Streptococcus pneumoniae colonisation: the key to pneumococcal disease. Lancet Infect Dis 4: 144–154. [DOI] [PubMed] [Google Scholar]
- 93. Raymond J, Le Thomas I, Moulin F, Commeau A, Gendrel D, et al. (2000) Sequential colonization by Streptococcus pneumoniae of healthy children living in an orphanage. J Infect Dis 181: 1983–1988. [DOI] [PubMed] [Google Scholar]
- 94. Millar EV, O'Brien KL, Zell ER, Bronsdon MA, Reid R, et al. (2009) Nasopharyngeal carriage of Streptococcus pneumoniae in Navajo and White Mountain Apache children before the introduction of pneumococcal conjugate vaccine. Pediatr Infect Dis J 28: 711–716. [DOI] [PubMed] [Google Scholar]
- 95. Jacoby P, Carville KS, Hall G, Riley TV, Bowman J, et al. (2011) Crowding and other strong predictors of upper respiratory tract carriage of otitis media-related bacteria in Australian Aboriginal and non-Aboriginal children. Pediatr Infect Dis J 30: 480–485. [DOI] [PubMed] [Google Scholar]
- 96. Bogaert D, Engelen MN, Timmers-Reker AJ, Elzenaar KP, Peerbooms PG, et al. (2001) Pneumococcal carriage in children in The Netherlands: a molecular epidemiological study. J Clin Microbiol 39: 3316–3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Caulfield LE, de Onis M, Blossner M, Black RE (2004) Undernutrition as an underlying cause of child deaths associated with diarrhea, pneumonia, malaria, and measles. Am J Clin Nutr 80: 193–198. [DOI] [PubMed] [Google Scholar]
- 98. Fedson DS, Scott JA (1999) The burden of pneumococcal disease among adults in developed and developing countries: what is and is not known. Vaccine 17 Suppl 1S11–18. [DOI] [PubMed] [Google Scholar]
- 99. World Health Organization (2008) 23-valent pneumococcal polysaccharide vaccine. WHO position paper. Wkly Epidemiol Rec 83: 373–384. [PubMed] [Google Scholar]
- 100. Feikin DR, Feldman C, Schuchat A, Janoff EN (2004) Global strategies to prevent bacterial pneumonia in adults with HIV disease. Lancet Infect Dis 4: 445–455. [DOI] [PubMed] [Google Scholar]
- 101. Gilks CF (1997) Royal Society of Tropical Medicine and Hygiene meeting at Manson House, London, 12 December 1996. HIV and pneumococcal infection in Africa. Clinical, epidemiological and preventative aspects. Trans R Soc Trop Med Hyg 91: 627–631. [DOI] [PubMed] [Google Scholar]
- 102. Pradeepa R, Prabhakaran D, Mohan V (2012) Emerging economies and diabetes and cardiovascular disease. Diabetes Technol Ther 14 Suppl 1S59–67. [DOI] [PubMed] [Google Scholar]
- 103.Johnson HL, Deloria-Knoll M, Levine OS, Stoszek SK, Freimanis Hance L, et al.. (2010) Systematic evaluation of serotypes causing invasive pneumococcal disease among children under five: the pneumococcal global serotype project. PLoS Med 7. [DOI] [PMC free article] [PubMed]
- 104. Dagan R, Gradstein S, Belmaker I, Porat N, Siton Y, et al. (2000) An outbreak of Streptococcus pneumoniae serotype 1 in a closed community in southern Israel. Clin Infect Dis 30: 319–321. [DOI] [PubMed] [Google Scholar]
- 105. Brueggemann AB, Griffiths DT, Meats E, Peto T, Crook DW, et al. (2003) Clonal relationships between invasive and carriage Streptococcus pneumoniae and serotype- and clone-specific differences in invasive disease potential. J Infect Dis 187: 1424–1432. [DOI] [PubMed] [Google Scholar]
- 106. Lijek RS, Weiser JN (2012) Co-infection subverts mucosal immunity in the upper respiratory tract. Curr Opin Immunol 24: 417–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Roca A, Dione MM, Bojang A, Townend J, Egere U, et al. (2013) Nasopharyngeal Carriage of Pneumococci Four Years after Community-Wide Vaccination with PCV-7 in The Gambia: Long-Term Evaluation of a Cluster Randomized Trial. PLoS One 8: e72198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Egere U, Townend J, Roca A, Akinsanya A, Bojang A, et al. (2012) Indirect effect of 7-valent pneumococcal conjugate vaccine on pneumococcal carriage in newborns in rural Gambia: a randomised controlled trial. PLoS One 7: e49143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Greenberg D, Broides A, Blancovich I, Peled N, Givon-Lavi N, et al. (2004) Relative importance of nasopharyngeal versus oropharyngeal sampling for isolation of Streptococcus pneumoniae and Haemophilus influenzae from healthy and sick individuals varies with age. J Clin Microbiol 42: 4604–4609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Odutola A, Antonio M, Owolabi O, Bojang A, Foster-Nyarko E, et al. (2013) Comparison of the prevalence of common bacterial pathogens in the oropharynx and nasopharynx of gambian infants. PLoS One 8: e75558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Murphy TF, Brauer AL, Sethi S, Kilian M, Cai X, et al. (2007) Haemophilus haemolyticus: a human respiratory tract commensal to be distinguished from Haemophilus influenzae. J Infect Dis 195: 81–89. [DOI] [PubMed] [Google Scholar]
- 112. Usuf E, Bottomley C, Adegbola RA, Hall A (2014) Pneumococcal carriage in sub-Saharan Africa–a systematic review. PLoS One 9: e85001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Vives M, Garcia ME, Saenz P, Mora MA, Mata L, et al. (1997) Nasopharyngeal colonization in Costa Rican children during the first year of life. Pediatr Infect Dis J 16: 852–858. [DOI] [PubMed] [Google Scholar]
- 114. Weinberger DM, Bruden DT, Grant LR, Lipsitch M, O'Brien KL, et al. (2013) Using Pneumococcal Carriage Data to Monitor Postvaccination Changes in Invasive Disease. Am J Epidemiol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Goldblatt D, Ramakrishnan M, O'Brien K (2013) Using the impact of pneumococcal vaccines on nasopharyngeal carriage to aid licensing and vaccine implementation; a PneumoCarr meeting report March 27–28, 2012, Geneva. Vaccine 32: 146–152. [DOI] [PubMed] [Google Scholar]
- 116. Coles CL, Labrique A, Saha SK, Ali H, Al-Emran H, et al. (2011) Newborn vitamin A supplementation does not affect nasopharyngeal carriage of Streptococcus pneumoniae in Bangladeshi infants at age 3 months. J Nutr 141: 1907–1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Rusen ID, Fraser-Roberts L, Slaney L, Ombette J, Lovgren M, et al. (1997) Nasopharyngeal pneumococcal colonization among Kenyan children: antibiotic resistance, strain types and associations with human immunodeficiency virus type 1 infection. Pediatr Infect Dis J 16: 656–662. [DOI] [PubMed] [Google Scholar]
- 118. Donkor ES, Newman MJ, Oliver-Commey J, Bannerman E, Dayie NT, et al. (2010) Invasive disease and paediatric carriage of Streptococcus pneumoniae in Ghana. Scand J Infect Dis 42: 254–259. [DOI] [PubMed] [Google Scholar]
- 119. Coles CL, Rahmathullah L, Kanungo R, Thulasiraj RD, Katz J, et al. (2001) Vitamin A supplementation at birth delays pneumococcal colonization in South Indian infants. J Nutr 131: 255–261. [DOI] [PubMed] [Google Scholar]
- 120. Devi U, Ayyagari A, Devi KR, Narain K, Patgiri DK, et al. (2012) Serotype distribution & sensitivity pattern of nasopharyngeal colonizing Streptococcus pneumoniae among rural children of eastern India. Indian J Med Res 136: 495–498. [PMC free article] [PubMed] [Google Scholar]
- 121. Wattal C, Oberoi JK, Pruthi PK, Gupta S (2007) Nasopharyngeal carriage of Streptococcus pneumoniae . Indian J Pediatr 74: 905–907. [DOI] [PubMed] [Google Scholar]
- 122. Adetifa IM, Antonio M, Okoromah CA, Ebruke C, Inem V, et al. (2012) Pre-vaccination nasopharyngeal pneumococcal carriage in a Nigerian population: epidemiology and population biology. PLoS One 7: e30548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Gill CJ, Mwanakasale V, Fox MP, Chilengi R, Tembo M, et al. (2008) Effect of presumptive co-trimoxazole prophylaxis on pneumococcal colonization rates, seroepidemiology and antibiotic resistance in Zambian infants: a longitudinal cohort study. Bull World Health Organ 86: 929–938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Gill CJ, Mwanakasale V, Fox MP, Chilengi R, Tembo M, et al. (2008) Impact of human immunodeficiency virus infection on Streptococcus pneumoniae colonization and seroepidemiology among Zambian women. J Infect Dis 197: 1000–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA 2009 checklist.
(DOCX)
Details of studies reporting carriage of Streptococcus pneumoniae .
(DOCX)
Studies reporting carriage of individual pneumococcal serotypes or serogroups.
(DOCX)
Details of studies reporting carriage of Haemophilus influenzae .
(DOCX)
Details of studies reporting carriage of Moraxella catarrhalis .
(DOCX)
Details of studies reporting carriage of Staphylococcus aureus .
(DOCX)
Details of studies reporting carriage of Neisseria meningitidis .
(DOCX)
Impact of vaccination on Streptococcus pneumoniae carriage by age.
(DOCX)
Supplementary methods.
(DOCX)
Protocol of the systematic review.
(PDF)