Abstract
Residential characteristics influence opportunities, life chances and access to health services in the United States but what role does residential segregation play in differential access and mental health service utilization? We explore this issue using secondary data from the 2006 Medical Expenditure Panel Survey, 2006 American Medical Association Area Research File and the 2000 Census. Our sample included 9737 whites, 3362 African Americans and 5053 Latinos living in Metropolitan Statistical Areas. Using logistic regression techniques, results show respondents high on Latino isolation and Latino centralization resided in psychiatrist shortage areas whereas respondents high on African American concentration had access to psychiatrists in their neighborhoods. Predominant race of neighborhood was associated with the type of mental health professional used where respondents in majority African American neighborhoods were treated by non-psychiatrists and general doctors whereas respondents in majority Latino neighborhoods saw general doctors. Respondents high on Latino Isolation and Latino Centralization were more likely to utilize non-psychiatrists. These findings suggest that living in segregated neighborhoods influence access and utilization of mental health services differently for race/ethnic groups which contradicts findings that suggest living in ethnic enclaves is beneficial to health.
Keywords: Residential segregation, Race/ethnicity, Mental health, Access, Use, Disparities
Introduction
Limited access to mental health services is regarded as a major barrier for individuals needing care. The U.S. Surgeon General's report estimates that two thirds of Americans suffering from mental illness do not receive care and many that receive medical treatment do so in the primary care setting (Young, Klap, Sherbourne, & Wells, 2001). Under-treatment and inappropriate treatment occur in this setting despite the existence of effective interventions, including pharmacological therapy, psychotherapy, and practice guidelines for specific diagnoses (Ronzio, Guagliardo, & Persaud, 2006). The problems associated with limited access and inappropriate treatment are particularly problematic for race/ethnic groups since they have less access to mental health services than whites, are less likely to receive needed care, and are more likely to receive poor quality of care (U.S. Department of Health and Human Services, 2001).
The majority of literature elucidating the relationship between access and utilization of mental health services has attributed race/ethnic disparities to cultural beliefs about the origins, stigma and treatment of mental health conditions, patient–ephysician racial concordance and individual enabling factors, such as socioeconomic status and insurance coverage (Cook, 2007; Lillie-Blanton & Hoffman, 2005). However, researchers who have decomposed race/ethnic disparities found these individual enabling and predisposing factors do not fully account for the observed differences (Hargraves & Hadley, 2003; Weinick, Zuvekas, & Cohen, 2000) but “place” characteristics are also possible sources of race/ethnic disparities (Smedley, Stith, & Nelson, 2003). Recently, residential segregation has been considered an important “place” characteristic since it is associated with social forces that shape culture and preferences regarding health care utilization, inequalities in health care marketplaces across communities and disparities in environmental risk factors that affect health needs and outcomes (Gaskin, Dinwiddie, Chan, & McCleary, 2012).
The literature investigating the relationship between residential segregation and mental health is inconclusive. Some report either a detrimental effect (Acevedo-Garcia, 2001; Jackson, Anderson, Johnson, & Sorlie, 2000) while others show a buffering effect (LeClere, Rogers, & Peters, 1997). Using Fundamental Cause theory (Link & Phelan, 1995) as a basis for understanding race/ethnic disparities in health, Williams and Collins (2001) suggest residential segregation can be regarded as a “fundamental cause” of disease since groups that reside in these types of neighborhoods often lack the health resources needed to circumvent disease (i.e. fewer physician offices, innovative technologies necessary for treatment and limitations in accessing alternative forms of transportation which in turn affect utilization and continuity of care). Specifically for Latinos, some research shows Latino neighborhood concentration operates to lower mortality, disease prevalence and overall health (Eschbach, Ostir, Patel, Markides, & Goodwin, 2004; Lee & Ferraro, 2007).
In the present article, we focus on one aspect of the health delivery system that may affect limited access and utilization of mental health services, such as residential segregation. We are interested in geographic availability of mental health services not only because it is amenable to policy solutions, but also because geographic disparity in provider location may be an explanatory factor in disparities of mental services utilization by race/ethnicity (Ronzio et al., 2006). Research that adequately measures disparities in the geography of mental health providers by residential segregation is limited. Since few studies examine geographic proximity of providers in relation to where people live, we investigate if residential segregation influences access and utilization by mapping the location of mental health care professionals (MHCP's) for African Americans and Latinos in the United States (U.S.).
Factors driving residential segregation for race/ethnic groups
Residential segregation is the degree to which two or more groups live separately from one another, in different parts of the urban environment (Massey & Denton, 1988). Sociological research has underscored the role of residential segregation as a primary institutional mechanism of racism and a fundamental cause of racial disparities in health (Massey & Denton, 1993; Williams & Collins, 2001). Residential segregation of race/ethnic groups is not only endemic to the U.S., but widely observed throughout the world (Burholt, 2004; Johnston, Poulsen, & Forrest, 2007). For example, South Africa mirrored their Apartheid system after U.S. racial segregation and as a result, Blacks and Coloreds suffer higher rates of all-cause mortality, infant mortality, chronic disease and the social problems associated with inadequate health care in segregated communities (Christopher, 1993; Myer, Ehrlich, & Susser, 2004). In the U.S., residential segregation remains much higher than economic segregation (Darden & Bagaka, 1997). African Americans are the most segregated racial group even when various factors such as neighborhood preferences (Zubrinsky & Bobo, 1996), racial attitudes and stereotyping (Bobo & Massagli, 2001) and preferred educational level of neighbors (Cutler & Glaeser, 1997)are taken into account. Although suburban areas have more African American residents than in the past, only about one-fourth live in suburbs. Moreover, African Americans living in the suburbs are segregated in areas with lower income levels and higher crime rates (Alba, Logan, & Bellair, 1994; Timberlake, Howell, & Straight, 2011).
Trends in residential segregation vary for Latinos compared to African Americans. Latinos are moderately segregated from whites, although their levels of segregation are increasing as a result of continuous, high-volume immigration since 1970 (Charles, 2003). Latino segregation has been attributed to immigrant preferences for settling in “ethnic enclaves” to ease their adjustment to U.S. society (Alba & Logan, 1991; Logan, Alba, & Leung, 1996). In a study investigating the spatial assimilation of Latinos and Latino immigrants, South, Crowder, and Chavez (2005) found that higher SES Latinos and those with greater English language proficiency were more likely to move into neighborhoods with non-Latino whites than were low SES Latinos with less English proficiency.
Residential segregation, availability, and utilization of mental health care professionals
Much of the literature on residential segregation, access and utilization of mental health services has been mixed. Some show communities with high proportions of African American and Latino residents are 4 times more likely than non-Latino whites to have a shortage of specialists, regardless of community income (Gaskin et al., 2012; Morales, Lara, Kington, Valdez, & Escarce, 2002). Other studies suggest residential segregation might place African Americans at an advantage because of their closer proximity to inner city hospitals and academic medical centers (Kahn et al., 1994). Moreover, some report that mentally distressed African Americans and Latinos residing in segregated areas are forced to rely on hospital emergency rooms and churches for support because they are less likely to have private health insurance (Chow, Jaffe, & Snowden, 2003). Allegria et al. (2002) found that predominantly Latino communities and the surrounding areas are often limited in the quality and number of available mental health services and for individuals with subsidized insurance such as Medicaid, there is less access to mental health specialty services.
The disparity in geographic availability of MHCP's may constitute an important barrier for persons seeking mental health services. Residential segregation influences utilization because of its impact on the supply of MHCP's. Research has shown fewer providers locate in minority neighborhoods because of lower reimbursement rates particularly when higher proportions of African Americans and Latinos are covered by Medicaid or are uninsured (Gaskin et al., 2012). Since many minorities residing in residentially segregated neighborhoods are less likely to receive treatment from a specialist (Ronzio et al., 2006), they are forced to visit other types of MHCP's. Research suggests patients with mental health problems who do not visit a psychiatrist are less likely to receive a proper DSM-IV diagnosis and/or referral to psychotherapy (Pingitore, Snowden, Sansone, & Klinkman, 2001).
In addition to limitations in the supply of health care providers, other individual factors are believed to influence differences in utilization. In a study examining the determinants of utilization for Latinos, Allegria et al. (2002) found language fluency, cultural differences, access to Medicaid specialty services, differences in recognition of mental health problems and lower quality of mental health care were major contributors to disparities. Other studies found African Americans who were not poor were less likely to use specialty services compared to whites even when demographic, insurance status and psychiatric morbidity were taken into account (Snowden & Thomas, 2000). Pingitore et al. (2001) found African Americans and other minorities were more likely to visit a primary care physician when seeking treatment for depression, but the study measured race/ethnic differences and SES as major barriers, not residential segregation.
New contribution: residential segregation, access and utilization of mental health care professionals
To date, we found no studies examining which dimensions of residential segregation might influence access to psychiatrists and the type of MHCP's utilized in residentially segregated neighborhoods. We are interested in exploring five dimensions in order to test multiple specific pathways linking residential segregation to access and utilization of mental health services. This is noteworthy because our analysis provides a methodological advantage over previous studies that only use segregation measures such as dissimilarity, isolation, or predominant race of neighborhood. Previous research has provided a strong theoretical justification for linking dissimilarity and isolation dimensions to health (Shihadeh & Flynn, 1996) and others have used population composition at the neighborhood level as a proxy for segregation (Fang, Madhavan, Bosworth, & Alderman, 1998). However, not much is known whether other segregation dimensions, such as centralization and clustering relate to health (Acevedo-Garcia, Lochner, Osypuk, & Subramanian, 2003). Since segregation is a multidimensional construct where a group can experience segregation on more than one dimension simultaneously, these dimensions can be highly correlated. However, segregation investigates how these groups are situated or positioned in the MSA where each dimension has different implications for access to essential mental health resources. We examine multiple dimensions of segregation for African Americans and Latinos since it is unknown whether segregation varies across race/ethnic groups in their effects on access to mental health care (Acevedo-Garcia, 2001). Studies that examine African American segregation in comparison to Latino segregation may also shed light on the various mechanisms causing race/ethnic specific segregation since, historically, African American segregation is largely a function of institutionalized discriminatory practices in the housing market whereas Latino segregation is considered a result of preferences for immigrants to settle in “ethnic enclaves” with high visibility of social networks (Williams & Collins, 2001). Therefore the present study: 1) examines which dimensions of residential segregation are most relevant for understanding geographic availability of psychiatrists and 2) investigates the segregation dimensions associated with race/ethnic differences in utilization of MHCP's for a subpopulation seeking treatment. Information derived from this analysis will provide insight into the patterns of mental health services availability by specialty and treatment by MHCP characteristics. We hypothesize residentially segregated areas would have fewer psychiatrists. In addition, respondents residing in residentially segregated areas would be more likely to use primary care physicians for their mental health problems rather than psychiatrists.
Methods
Data
We combine data from three sources. The first is the 2006 Medical Expenditure Panel Survey (MEPS), a national survey of health care utilization, providers, insurance coverage and cost of health care services in the U.S. We use the Household (HC) and Medical Provider Components (MPC). The HC component collects data from a sample of families and individuals in selected communities, drawn from a nationally representative subsample of households that participated in the prior year's National Health Interview Survey (NHIS). The MPC covers hospitals, physicians, home health care providers and pharmacies identified by HC respondents. We used office-based, outpatient, and emergency event files from the MEPS. The second dataset is the 2006 American Medical Association Master File (AMAMF), which lists the addresses of community mental health care centers, physicians, psychiatrists, psychologists, social workers and other certified health care providers that service mental health problems. The third dataset is the 2000 Census Summary File 1 and 3, which contain housing patterns data for metropolitan statistical areas (MSA's). MSA's are geographic regions normally centered on a single large city with high population density and close economic resources. We obtained counts of MHCP's for each zip code located fully or partially in MSA's. We used all provider locations as well as the total population within a 3 to 5 mile radius to ensure that the supply (provider) and demand (population) influences on the periphery of the city were properly captured in the estimations of provider accessibility (Ronzio et al., 2006). We linked data from MEPS and the AMAARF to demographic and SES information from 2000 Census Summary File 1 and 3. Only respondents that could be matched with census data were included in the analysis.
Our sample started with 34,145 person level observations from the 2006 MEPS HC survey. After dropping 10,354 people under the age of 18 and 4375 people that did not match with Census data, we were left with the current sample of 19,048. The 2000 Census Bureau Summary File 1 and 3 was merged with the MEPS on the Zip Code Tabulation Areas (ZCTA) level. A ZCTA is “a statistical geographic entity” that approximates the delivery areas for a U.S. Postal Service five-digit or three-digit ZIP Code. We further narrowed the population to 16,025 by dropping 2027 zip codes without 5 numbers and also dropping 96 zip codes that did not link to MSA's.
The 2000 Census Bureau Housing Patterns Residential Segregation Data that was linked to the Census zip code level data was downloaded on the MSA level for African Americans and Latinos. Before merging the census data containing the segregation measures to the MEPS, the 2006 American Medical Association Area Research File was added. Finally data from the 2006 MEPS office based, outpatient, and emergency event files was merged to the data. The 2006 Medical Conditions File (HC-104) was merged to the event file then collapsed on the person level file in order to merge to the person level data to the larger dataset.
Measures
Dependent variables: specialists and mental health care professionals
To create the variable for psychiatrist shortage, we computed the population to psychiatrist ratio for each zip code. Consistent with the Bureau of Health Professions definition (see http://bhpr.hrsa.gov/shortage/mental.htm), we defined psychiatrist shortage areas as those zip codes where the population to psychiatrist ratio was greater than 3500 or those zip codes that did not have a psychiatrist. A dichotomous variable was created to indicate whether the respondent lived in a shortage area (0 = no; 1 = yes).
To measure which type of MHCP was seen for a mental health problem in the past 12 months, we constructed a mutually exclusive categorical variable that included four values: 0 = no visit, 1 = psychiatrist, 2 = general doctor and 3 = non-psychiatrist/non-general doctor. Psychiatrist included child and adult psychiatry, excluding psychoanalysis. General doctor included primary care physicians such as family and general practice, internal medicine, obstetrics–gynecology and pediatrics. Non-psychiatrist/non-general doctor included certified mental health care professionals such as social workers, psychologists, therapists or counselors. A mental health problem was determined using ICD-9 codes for mental disorders that were validated by a certified mental health care professional. Based on the fact that no more than 10% and probably closer to 6% of the U.S. population are estimated to meet criteria for serious mental illness in a given year (Kessler et al., 2001), serious biologically based schizophrenic disorders were excluded. These disorders were removed since research suggests clinicians over diagnose schizophrenia and under diagnose mood disorders in African Americans (Strakowski, McElroy, Keck, & West, 1996). For respondents with multiple visits to MHCP's, the first encounter with a specific MHCP (i.e. general doctor then referred to a psychiatrist) is counted as one visit and put into the category of the professional seen non-psychiatrist on the first encounter.
Ecological variables
To measure residential segregation, we linked zip code level data to MSA measures of segregation published by the Census Bureau for each minority group. Residential segregation is a multidimensional construct consisting of five dimensions: dissimilarity, isolation, clustering, centralization, and concentration (Massey & Denton, 1993). These dimensions are conceptually and empirically different measuring distinct forms of how groups are distributed within a MSA. Each of these distributional characteristics has different social and behavioral implications and represents a different facet of what researches have referred to as “segregation” (Massey & Denton, 1988). Dissimilarity measures evenness, i.e. the proportion of minority residents who would have to change census tracts for the population to be evenly distributed. Various studies have used dissimilarity since it measures the degree of integration in neighborhoods. A score over 60 is interpreted as extreme segregation between two groups indicating the percentage of either group that would have to move to achieve an even population distribution. Although research using the dissimilarity dimension has provided the least clear conceptualization regarding its relationship to health, theoretically, scholars believe the unequal distribution of minorities within a geographic space many have a negative impact on access to health resources (Acevedo-Garcia et al., 2003). Isolation measures exposure. This is the probability of contact of one minority group in relation to whites. Isolation has been employed in a number of health studies because it is the dimension that severely limits life chances for social mobility by combining poverty, joblessness, welfare dependency, teenage childbearing and other indicators of social malaise in minority neighborhoods (Wilson, 1993). Isolation is the percentage of same race in the average group member's neighborhood where scores of 70 and over are considered extreme. Clustering measures the degree to which minorities and whites reside in proximity to one another. It is also known as ghettoization, the degree to which minority neighborhoods are close to one another as opposed to spread across the MSA. Clustering further constrains social and economic opportunities for the segregated group making it more difficult for residents to access other parts of the metropolitan area in search of health services (Morenoff & Sampson, 1997; Sampson, Morenoff, & Earls, 1999). We measured the association between clustering, access and utilization for African Americans because Latinos in the MEPS were not high on this dimension. Centralization measures if minorities live in the urban center as opposed to the suburbs. In residential segregation studies, scholars regard this dimension as pivotal in the spread of infectious disease from inner city disease epicenters to the surrounding suburbs because of the lack of essential health resources necessary to mitigate the spread of disease (Wallace et al., 1997). Lastly, concentration measures the degree to which minority residents are densely populated within a small geographic area relative to the density experienced by other groups. Similar to centralization, in terms of infectious disease transmission, concentration of marginalized populations might increase contact between infectious and susceptible individuals within the MSA. High degrees of concentration may also facilitate geographic targeting on the part of anti-public health entities such as the tobacco and alcohol industries since it is the dimension most clearly linked to indicators of lower SES among African Americans (Acevedo-Garcia, 2001). Scores above 60 for clustering, 80 for centralization and 70 for concentration imply the existence of a large enclave containing mostly one racial/ethnic group (Massey & Denton, 1988). We transformed each residential segregation dimension into a dichotomous variable based on cut off points indicating high segregation for that respective racial/ethnic group. Dichotomization of segregation dimensions has been done in previous studies showing its relationship to access to health resources, utilization and health outcomes (Chan, Gaskin, Dinwiddie, & McCleary, 2012; Gaskin et al., 2012).
Neighborhood composition
We designated zip codes as predominantly African American or Latino if more than 50 percent of the residents were a racial/ethnic minority. Research has shown racial composition of neighborhoods influences the availability of specialists (Reschovsky & O'Malley, 2007). Integrated neighborhoods were defined as zip codes between 30% and 49% of one racial/ethnic group. Recent demographic studies suggest a small proportion of minorities have moved to suburban neighborhoods surrounding central cities that are characteristically low income signaling a “tipping” of poor populations toward the suburbs (Berube & Kneebone, 2006). Dichotomous variables were created for African Americans and Latinos for both measures of neighborhood composition.
Pre-disposing factors
Research suggests mental health disparities are embedded within persistent SES differences, so we chose educational attainment as our SES indicator. Levels of schooling are considered a better indicator of SES because individuals may or may not have a steady source of income but have had some exposure to schooling (Dinwiddie, 2010) and educational attainment is unaffected by health impairments that may emerge in adulthood (Elo & Preston, 1996). We measure educational attainment with a categorical variable indicating levels of schooling (1 = less than 8 years, 2 = less than 11 years, 3 = some college training, 4 = bachelor's degree and 5 = advanced degree). We include race/ethnicity as a categorical variable (1 = African American, 2 = Latino and 3 = whites) to examine whether race/ethnicity effects are independent of residential segregation since African Americans and Latinos tend to have less access to mental health services and are more likely to receive poor quality of care (Miranda, McGuire, Williams, & Wang, 2008).
Control variables
Individual level control variables include age, sex, health insurance, income and a Kessler Index of Non-Specific Psychological Distress (K6) (Kessler et al., 2002). Age is a categorical variable measured by four stages of the life course (1 = 18−24 years, 2 = 25−44 years, 3 = 45−64 years and 4 = 65 + years). Sex is a dichotomous variable for male (0) or female (1). Health Insurance is a categorical variable indicating type of coverage (1 = private, 2 = public insurance and 3 = uninsured). The categorical variable income was constructed by dividing family income by the poverty line based on family size and composition provided in the U.S. Census summary file 1 & 3 (1 = poor (less than 100%), 2 = near poor (100% to less than 125%), 3 = low income (125% to less than 200%), 4 = middle income (200% to less than 400%), and 5 = high income (greater than or equal to 400%). The K(6) is a community based validated epidemiological measure of non-specific psychological distress consisting of six variables which asks respondents “How much of the time did you feel”: 1) so sad nothing could cheer you up, 2) nervous, 3) restless or fidgety, 4) hopeless, 5) that everything was an effort, and 6) worthless. Each was measured by a categorical variable (0 = none of the time, 1 = a little of the time, 2 = some of the time, 3 = most of the time, 4 = all of the time). An index was created where the higher the value, the greater the person's tendency toward mental distress. We use the K(6) as a proxy for severity of mental illness since were not able to control for severity directly.
Community level control variables include percent owner occupied and percent renter occupied in the zip code. Percent owner and percent renter occupied, provided by the Census summary file, were calculated at the neighborhood level based on percentages of these characteristics in the zip code.
Methods
We analyzed these data using logistic regression techniques in SAS 9.1 (2009). We estimated three sets of logistic regression analyses to compute the odds of residing in a psychiatrist shortage area based on residential segregation dimensions. We used state level random effects to control for unobserved state level factors (i.e. Medical licensing policies, presence of medical school and academic medical centers). The first set of regressions is our base model estimating psychiatrist shortage by residential segregation controlling for age, sex, insurance coverage, income, percent home owners in the zip code, percent renters in the zip code and the K(6). In the base model, whites were the reference group and the odds ratios of interest were the race/ethnic specific segregation measures. The second set of models adds neighborhood composition to the base specification. In this model, the objective was to examine if predominantly African American or predominantly Latino neighborhoods and/or integrated neighborhoods were associated with psychiatrist shortage areas. Our intension was to also examine if measures of neighborhood composition attenuate the residential segregation dimension in the base model with controls. The third set of models incorporates enabling factors such as educational attainment, indicator variables for African American and Hispanic race/ethnic identity and nine interactions (i.e. segregation*race/ethnicity) to examine individual and concomitant associations with psychiatrist shortage areas. The interactions test whether the association of segregation was uniform across race and ethnic groups. All analyses were weighted using the “person weight” variable provided by the MEPS.
For the utilization analysis, we employed relative risk ratios (RR's) to examine differential utilization of services by residential segregation based on the MHCP seen on the first visit. We estimated a model predicting whether respondents saw a psychiatrist, general doctor or non-psychiatrist for a mental health problem in the past year. Since empirical evidence shows racial/ethnic groups more often use other sources rather than psychiatrists for their mental health problems (Pingitore et al., 2001), psychiatrist was set as the reference group. Our goal was to explore the RR of visiting a non-psychiatrist or general doctor over the probability of choosing a psychiatrist given residential segregation patterns. This analysis controls for age, sex, insurance coverage, income, percent home owners in the zip code, percent renters in the zip code and the K(6).
Results
Descriptive statistics
Table 1 shows descriptive statistics for the independent and control variables with Pearson's chi-square and t-tests of significance for whites, African Americans and Latinos. Nearly half of whites and the majority of African Americans and Latinos lived in MSA's with high African American dissimilarity. Almost a quarter of Latinos were high on Latino isolation in contrast to the smallest percent of whites (4%), and African Americans (10%) high on this segregation dimension. The lowest percentage of African Americans (14%) was high on African American clustering and no MSA demonstrated segregation based on clustering for Latinos. Interestingly, a sizeable percentage of Whites (42%) were high on African American centralization. Lastly, the majority of Whites (54%) and African Americans (51%) were high on African American centralization. Over a quarter of Latinos were high on Latino concentration.
Table 1.
Weighted descriptive statistics of the independent and control variables by race/ethnicity.
| Variables | White (N = 9737) | African Americans (N = 3362) | Latino (N = 5053) |
|---|---|---|---|
| Independent variables | |||
| African American dissimilarity | 48.61%*** | 66.94%*** | 51.14%*** |
| Latino dissimilarity | 13.46%*** | 19.87%*** | 23.30%*** |
| African American isolation | 10.54%*** | 25.85%*** | 14.92%*** |
| Latino isolation | 3.71%*** | 10.40%*** | 26.73%*** |
| African American clustering | 9.74%*** | 14.15%*** | 6.29%*** |
| African American centralization | 42.19%*** | 28.59%*** | 29.07%*** |
| Latino centralization | 21.07% | 22.26% | 25.03% |
| African American concentration | 54.35%*** | 51.64%*** | 36.89%*** |
| Latino concentration | 20.75%** | 25.52%** | 27.27%** |
| Neighborhood composition | |||
| Predominately African American | 1.96%*** | 37.92%*** | 3.40%*** |
| Predominately Latino | 1.68%*** | 4.23%*** | 30.94%*** |
| Integrated African American | 2.72%*** | 17.6%*** | 7.29%*** |
| Integrated Latino | 3.68%*** | 7.4%*** | 19.54%*** |
| Education | |||
| 8th grade or below | 2.08%*** | 4.04%*** | 22.5%*** |
| Some high school | 8.01%*** | 16.95%*** | 20.42%*** |
| High school diploma or GED | 32.58%*** | 36.57%*** | 29.22%*** |
| Some college | 24.92%*** | 25.49%*** | 16.72%*** |
| Bachelors degree | 21.28%*** | 11.72%*** | 8.12%*** |
| Advanced degree | 11.12%*** | 5.22%*** | 3.03%*** |
| Control variables | |||
| Age | |||
| 18–24 | 11.18%*** | 15.92%*** | 17.9%*** |
| 25–44 | 33.58%*** | 40.39%*** | 49.46%*** |
| 45–64 | 36.58%*** | 31.97%*** | 24.37%*** |
| 65+ | 18.66%*** | 11.72%*** | 8.27%*** |
| Sex | |||
| Male | 48.40%*** | 44.96%*** | 51.55%*** |
| Female | 51.60%*** | 55.04%*** | 48.45%*** |
| Health insurance | |||
| Private | 79.05%*** | 60.93%*** | 46.39%*** |
| Public | 11.37%*** | 22.64%*** | 18.49%*** |
| Uninsured | 9.58%*** | 16.43%*** | 35.12%*** |
| Income | |||
| Poor | 7.02%*** | 19.51%*** | 17.05%*** |
| Near poor | 3.15%*** | 5.27%*** | 7.03%*** |
| Low income | 9.45%*** | 16.68%*** | 21.93%*** |
| Middle income | 29.12%*** | 31.93%*** | 34.31%*** |
| High income | 51.27%*** | 26.61%*** | 19.68%*** |
| Percent owner-occupied housing units | 70.5%*** | 59.4%*** | 58.8%*** |
| Percent renter-occupied housing units | 29.5%*** | 40.6%*** | 41.2%*** |
| Kessler index (mean) | 3.362* | 3.324* | 3.693* |
Note: Pearson's Chi-Square two tailed test of significance of racial/ethnic group in relation to whites at
p ≤ .05,
p ≤ .01,
p ≤ .001.
There were no Latinos in the sample high on clustering. Source: Medical Expenditure Panel Survey (MEPS) HC-105: 2006 Full Year; 2000 Census; 2006 AMAARF.
Neighborhood composition (Table 1) showed that 38% of African Americans and 31% of Latinos resided in same race/ethnic neighborhoods. Nearly 18% of African Americans and 20% of Latinos resided in integrated neighborhoods. The distribution of important SES indicators, provide evidence for educational stratification along race/ethnicity. Close to one third of whites, African Americans and Latinos had a high school diploma or GED. However, a quarter of whites and African Americans had some college training whereas 23% of Latinos had 8th grade or below educational attainment.
For control variables, the age distribution was relatively younger with over half of African Americans (56%), and Latinos (67%), between 18 and 44 years of age. The majority of whites (52%) and African Americans (55%) were female whereas Latinos (52%) were male. Most whites, African Americans and Latinos were covered by private health insurance. As for income, the majority of African Americans and Latinos were in the middle income category whereas nearly half of whites had high incomes. A sizeable percent of whites (71%) large percents of African Americans and Latinos (59%) owned their homes but 41% of African Americans and Latinos rented. The mean on the K(6) did not differ for racial/ethnic groups where each group had low levels of non-specific psychological distress.
Role of racial residential segregation in access to psychiatrists
Table 2 displays the odds ratios assessing the association between psychiatrist shortage and race/ethnic specific residential segregation dimensions controlling for age, sex, health insurance, poverty status, income, percent home owner in the zip code, percent renter in the zip code and the K(6). The first model tests the association between shortage area and residential segregation. Model 2 includes neighborhood composition and model 3 adds educational attainment, race/ethnicity and interactions.
Table 2.
Weighted odds ratios for no psychiatrist in zip code and residential segregation measures.
| Variables | Odds ratio (CI) | Odds ratio (CI) | Odds ratio (CI) |
|---|---|---|---|
|
|
|
|
|
| Model 1 | Model 2 | Model 3 | |
| Residential segregation | |||
| AfAm dissimilarity | 1.12 (0.847, 1.49) | 1.21 (0.924, 1.59) | 1.23 (0.928, 1.63) |
| Latino dissimilarity | 0.750 (0.443, 1.27) | 0.727 (0.443, 1.19) | 0.854 (0.532, 1.37) |
| AfAm isolation | 0.744 (0.357, 1.55) | 0.784 (0.409, 1.50) | 0.987 (0.579, 1.68) |
| Latino isolation | 2.30** (1.27, 4.18) | 2.30** (1.37, 3.85) | 7.54*** (2.71, 20.96) |
| AfAm clustering | 1.92 (0.849, 4.35) | 1.86 (0.873, 4.00) | 1.51 (0.764, 2.98) |
| AfAm centralization | 1.03 (0.760, 1.41) | 0.944 (1.02, 1.26) | 0.881 (0.653, 1.19) |
| Latino centralization | 1.30 (0.870, 1.95) | 1.36 (0.924, 1.99) | 1.42+ (0.977, 2.08) |
| AfAm concentration | 0.619** (0.457, 0.839) | 0.707** (0.513, 0.941) | 0.681** (0.506, 0.917) |
| Latino concentration | 1.10 (0.699, 1.75) | 1.40 (0.906, 2.18) | 1.38 (0.913, 2.09) |
| Neighborhood composition | |||
| Predominantly AfAm | 0.295*** (0.193, 0.450) | 0.209*** (0.102, 0.425) | |
| Predominantly Latino | 0.313*** (0.206, 0.476) | 0.570* (0.314, 0.954) | |
| Integrated AfAm | 0.460***(0.296, 0.716) | 0.486**(0.309, 0.762) | |
| Integrated Latino | 0.722 (0.463, 1.12) | 0.626 (0.395, 0.994) | |
| Education | |||
| <8th grade | 0.832 (0.667, 1.03) | ||
| <11th grade | 0.891 (0.764, 1.03) | ||
| Some college | 1.33*** (1.16, 1.53) | ||
| Bachelor's degree | 2.10*** (1.75, 2.51) | ||
| Advanced degree | 2.57*** (1.98, 3.35) | ||
| Race | |||
| African American | 1.22 (0.934, 1.67) | ||
| Latino | 1.08 (0.826, 1.43) | ||
| White (reference) | − | ||
| Interactions (significant) | |||
| AfAm * isolation | 0.148*** (0.048, 0.459) | ||
| Latino * isolation | 0.173** (0.056, 0.532) | ||
| AfAm * clustering | 0.217* (0.051, 0.917) |
Note: AfAm = African American; OR = Odds Ratio; CI = Confidence Interval; Significance
p ≤ .05,
p ≤ .01,
p ≤ .001:
All models control for age, sex, health insurance, income, percent owner occupied housing units, percent renter occupied housing units and K(6). There were no Latinos in the sample high on clustering. Source: Medical Expenditure Panel Survey (MEPS) HC-105: 2006 Full Year: 2000 Census; 2006 AMAARF.
Latino isolation was positively associated with psychiatrist shortage areas were the predicted odds were 2.30 times higher relative to whites (Model 1). However living in a shortage area was 31% lower for African American concentration. Model 2 incorporates racial composition of the neighborhood to further test whether a critical mass of one race/ethnic group was associated with limited access to psychiatrists. Although both predominantly one race and integrated neighborhoods had lower odds of not having a psychiatrist in the neighborhood, Latino isolation and African American concentration dimensions remained significant and the odds ratios did not change much from the first model. This finding suggests that how racial/ethnic groups are situated within a geographical space has explanatory power for access to mental health care beyond racial composition of neighborhoods.
In the final model, higher levels of schooling were associated with living in a psychiatrist shortage area. When observing how education influences the strength of the odds ratios, we found that Latino isolation increased substantially and Latino centralization became modestly significant. The predicted odds of living in psychiatrist shortage areas were 32% lower for concentrated African Americans which slightly increased from the previous model. Of the significant interactions, results indicate the effect of predominantly African American neighborhoods depends on the value of the Isolation and Clustering indexes. The effect for predominantly Latino neighborhoods depends on the Isolation index.
To further test the effects of residential segregation on access to psychiatrists, we performed sensitivity analysis estimating availability within a 3-mile and 5-mile radius around the zip code. Results (not shown) indicate African Americans that are clustered were more likely to have access to a psychiatrist within 3 miles (OR 1.94; CI 1.11–3.38; p ≤ .01) and 5 miles (OR 2.05; CI 1.18–3.57; p ≤ .01) of their residences. However, access to psychiatrists within a 5 mile radius of their residences was 49% lower for isolated Latinos (OR 0.519; CI 0.319–0.845; p ≤ .01).
Racial/ethnic differences in utilization
Although it is plausible that people living in residentially segregated communities with a mental health problem do not seek treatment since they may reside in shortage areas, it is difficult to discern their specific mental health needs and estimate prevalence rates. Therefore our next analysis focused on the subpopulation that initiated care in order to investigate whether residential segregation had any bearing on the type of MHCP seen on their first visit. In the sample, 976 Whites (9.4%), 217 African Americans (7%) and 301 Latinos (6%) indicated they were treated by an MHCP for a problem within the past 12 months. Results show (Fig. 1) the RR of seeing a non-psychiatrist/non-general doctor over a psychiatrist for isolated Latinos was 4.72 times higher relative to whites. Moreover, Latinos centrally located in the urban center had higher RR of seeing a non-psychiatrist/non-general doctor rather than a psychiatrist. In contrast, neighborhood composition was a determinant of utilization for respondents residing in predominantly African American neighborhoods. The RR for seeing a non-psychiatrist over a psychiatrist was 2.32 times higher and 1.67 times higher for seeing a general doctor over a psychiatrist. Similar to predominantly African American neighborhoods, a critical mass of respondents residing in Latino neighborhoods (RR = 2.0) were treated by a general doctor over a psychiatrist compared to whites.
Fig. 1.
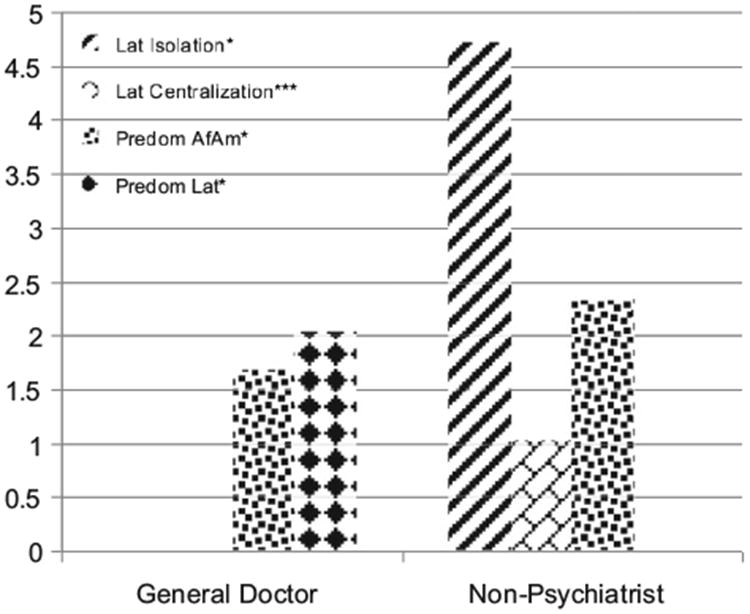
Weighted relative risk ratios for type of mental health care professional by residential segregation. Source: Medical Expenditure Panel Survey (MEPS) HC-105: 2006 Full Year; 2000 Census; 2006 AMAARF. Note: Lat = Latino, AfAm = African American, Predom = Predominant. All models control for age, sex, health insurance, income, percent owner occupied housing units, percent renter occupied housing units and K(6). Significance at *p ≤ .05, **p ≤ .01, ***p ≤ .001.
Discussion
Despite extensive research investigating how characteristics of neighborhoods are linked to the availability of mental health services (Osypuk & Acevedo-Garcia, 2010), much remains to be seen how racial/ethnic representation in those communities is an underlying factor driving disparities across mental health services. We explored this issue by asking questions linking 3 secondary datasets to determine 1) whether the availability of psychiatrists is contingent on how racial/ethnic groups are situated in MSA's and 2) if segregation has any bearing on the type of MHCP available for a subpopulation seeking care. We know nationally, there is a shortage of MHCP's and our results suggest isolated Latino neighborhoods are disproportionally affected by this shortage. Our findings support previous studies finding residential proximity to mental health care services an important factor in differential access and utilization of services (Fortney, Rost, Zhang, & Warren, 1999; Ronzio et al., 2006; Shannon, Bashshur, & Lovett, 1986). Our hypothesis, residentially segregated areas would have fewer psychiatrists, was supported for only two dimensions of segregation. Respondents residing in isolated Latino neighborhoods and high on Latino centralization (although marginally significant) had limited geographical access to psychiatrists. Research on the benefits of living in ethnically homogenous neighborhoods has shown mixed results for Latinos. Some report Latino concentration protects against the deleterious effects of disadvantaged environments showing Mexicans having a mortality advantage, better self-rated health and lower disease prevalence (Eschbuch et al., 2004). Others have shown living in ethnic enclaves limit access to outside resources needed to circumvent disease where high ethnic density is less beneficial to health compared to moderate ethnic density (Fagg, Curtis, Stansfeld, & Congdon, 2006; Portes, 1998). In addition, Lee (2009) provides enlightening findings on the impact of residential segregation on affective disorders showing Latino isolation was a stronger predictor of depression than individual level characteristics for Mexicans. The present study extends this research adding that respondents residing in isolated Latino neighborhoods and are centrally located in the central city have limited access to psychiatrists that can adequately treat them for their mental health problems, which is a major public health concern. Theoretically, isolation is the segregation dimension that limits access to health care resources because the “social conditions in which people live” (i.e. exposure to excess violence, crime, limitations to upward mobility, and low SES) not only increase health vulnerability but also influence the reluctance of health care providers to practice in these types of neighborhoods (Gaskin et al., 2012). In addition, centralization normally confines minorities to declining central city areas with fewer health care resources, older medical facilities, more community health centers and hospital outpatient departments (Gaskin et al., 2007; Lee, Spain, & Umberson, 1985; Lillie-Blanton, Martinez, & Salganicoff, 2001; Massey, 1985).
Although our findings show positive (but not statistically significant) associations between psychiatrist shortage areas and African American dissimilarity, clustering and centralization, we were not able to reinforce, with confidence, that respondents residing in these types of neighborhoods had limited access to psychiatrists. However, other studies have found significant associations with African American dissimilarity, homogeneous African American neighborhoods and shortages of primary care physicians (Gaskin et al., 2012; Greene, Blustein, & Weitzman, 2006). We did find respondents high on African American concentration were at an advantage and did have access to psychiatrists in their neighborhoods. Denton (1994) provides the best theoretical explanation for the effect of concentration on access to resources by suggesting concentration is the segregation dimension most clearly linked to indicators of lower SES among African Americans. Although less likely to have medical facilities with newer health related technologies, lower SES communities are more likely to have community mental health centers, hospital outpatient departments, and teaching hospitals with providers receiving federal and state subsidies to finance indigent care. Perhaps more psychiatrists are practicing in hospital based facilities since reimbursement policies vary by cite and care with hospital-based providers typically receiving faster reimbursement and more generous uncompensated care payments compared to office based providers.
We did find evidence that respondents with higher educational attainment were living in psychiatrist shortage areas. However, living in shortage areas may not be as detrimental for this population because they have access to resources necessary to circumvent disease that are not readily available in residentially segregated neighborhoods. Educational attainment increases income potential to purchase health enhancing goods such as health care services, nutritious food, live in cleaner environments, reduce stress and reduce the likelihood of practicing health risk-behaviors (Dinwiddie, 2010). The issue of great concern is “concentrated poverty” and its implications for health since segregated communities tend to have concentrated low SES and environmental disadvantage.
Our second research question was supported by evidence showing African Americans and Latinos utilize different types of MHCP's from whites which have been shown in other studies (Pingitore et al., 2001). African Americans may experience barriers that prohibit using specialty mental health services in their neighborhoods. We found racial make-up of neighborhoods has a significant bearing on the type of MHCP available where African Americans residing in majority homogenous communities more often were treated by social workers, therapists, and other certified MHCP's rather than psychiatrists. Respondents residing in predominantly Latino communities were treated by general doctors, a consistent finding with empirical studies suggesting Latinos generally seek care from a primary care physician or member of the clergy (U.S. Department of Health and Human Services, 2001). This can be problematic because general doctors face problems in understanding and treating some mental disorders, consequently leaving mental disorders in many people unrecognized or inadequately treated since the screening instruments used are often nonspecific for psychiatric disorders and general psychiatric morbidity (Hirschfield et al., 1997).
Major implications from our findings suggest that not race/ethnicity, per se, but racial stratification and racial processes that have created separate “place” characteristics for minority groups matter for understanding disparities in access and utilization patterns. Residential segregation has been regarded as a “fundamental cause” of disease since the racial and social organization of communities dictates availability of health resources in neighborhoods. “Fundamental Cause” theory (Link & Phelan, 1995) contends that disadvantaged environments have a persistent association with disease despite changes in intervening mechanisms (i.e. sanitation) since fundamental causes involve access to resources that can be used to avoid risk or to minimize the consequences of disease once it occurs. “Fundamental Causes,” such as residential segregation, are tied to resources like money, power, prestige and social connectedness where those with the most access and control over resources are in a better position to avoid risks, disease and the consequences of disease. Using “Fundamental Cause” theory to understand why essential health resources, such as psychiatrists, are limited in Latino neighborhoods has been unexplored in the literature. Our findings suggest this theoretical framework might be more appropriate for understanding disparities in mental health access, utilization and outcomes for Latinos since our data challenge existing hypotheses of the protective environments of “ethnic enclaves.” We suggest that future research investigate the impact of “place” characteristics on access and utilization of mental health services for Latinos with emphasis on variations by Latino subgroup.
Our findings also reinforce that African Americans and Latinos residing in racially homogenous neighborhoods are at a “double” disadvantage, since residential segregation and a “critical mass” of a racial/ethnic group in the neighborhood operate as stratifying agents limiting the availability of essential MHCP's. We have proven this point in our results and regard this as another major contribution to the literature.
Our study had a number of limitations that warrant consideration. First, we did not include Asians because their small numbers prohibited proper examination of segregation's impact on the availability of MHCP's located in their neighborhoods. Only 3 percent lived in predominantly Asian neighborhoods which were not a large enough sample for adequate comparison. Second, we were not able to discern if psychiatrists or other certified MHCP's were practicing in private offices, hospitals, community mental health centers or general health centers in neighborhoods. Disaggregation by type of facility would have allowed for a more nuanced analysis of where racial/ethnic groups were receiving care and the organizational structures that facilitate differential use. However, we found a consistent pattern of racial/ethnic disparities in utilization for African Americans and Latinos when examining the MHCP's located in their neighborhoods. Third, we did not address severity of mental health conditions (i.e. hospitalizations), which might prompt respondents to seek a specialist outside of their neighborhoods. We did, however, exclude respondents that were diagnosed with schizophrenia since they would more likely have differential access to MHCP's through federally sponsored health insurance and/or use community health services to assist with activities of daily living. We attempted to control for severity by using the K6 in our models. Lastly, although there is a wealth of literature indicating that African American and Latinos do not seek help for mental health conditions because of differences in the etiological beliefs about mental illness (Schnittker, Freeze, & Powell, 2000), stigma, distrust, religious and cultural preferences (Dupree, Watson, & Schneider, 2005), we chose not to include members of the clergy since most are not certified mental health professionals.
Conclusion
In conclusion, the present study extends research that seeks to understand the association between residential segregation, access and utilization of mental health services. Our findings have major implications for the 2010 Patient Protection and Affordability Care Act (PPACA) and the future of reducing health disparities. If the goal of the PPACA is to increase access to doctors for the most vulnerable population, policy makers must make a concerted effort to provide qualified psychiatrists in underserved areas that are segregated and predominantly African American and Latino. Our findings point to one tangible approach to improving access to psychiatrists and other MHCP's by reinforcing the need for a diverse workforce by increasing the pool of minority MHCP's that aspire to practice psychiatry as their primary profession. Also, providing incentives such as loan forgiveness, improvements in working conditions in the facilities located in minority communities, updated technology and quicker reimbursement for Medicare/Medicaid are a few cost effective solutions that might entice psychiatrists to locate their practices in segregated communities. We provided empirical evidence that residential segregation and racial composition of neighborhoods matter and we suggest that future research further examine the influence of geography in medical practice and availability of mental health services in order to accurately identify and design reforms to reduce racial/ethnic health disparities.
Acknowledgments
This paper was written with support from the National Institutes of Health Division of Health Disparities LRP 2009−2011 and grant# 1P60MD00214-07 from the National Institute of Minority Health and Health Disparities (NIMHD) of the National Institutes of Health (NIH). A version of the article was originally presented at the American Sociological Association meetings in Las Vegas, NV August 2011. The authors would like to thank William Falk, Thomas LaVeist and three anonymous reviewers for their comments.
References
- Acevedo-Garcia D. Zip code-level risk factors for tuberculosis: neighborhood environment and residential segregation in New Jersey, 1985–1992. American Journal of Public Health. 2001;91:734–741. doi: 10.2105/ajph.91.5.734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future directions in residential segregation and health research: a multilevel approach. American Journal of Public Health. 2003;93(2):215–221. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alba R, Logan J. Variations on two themes: racial and ethnic patterns in the attainment of suburban residence. Demography. 1991;28:431–453. [PubMed] [Google Scholar]
- Alba R, Logan J, Bellair P. Living with crime: the implications of racial/ethnic differences in suburban location. Social Forces. 1994;73:394–434. [Google Scholar]
- Alegria M, Canino G, Rios R, Vera M, Calderon J, Rusch D, et al. Inequalities in the use of specialty mental health services among Latinos, African Americans and non-Latino whites. Psychiatric Services. 2002;53:1547–1555. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- Berube A, Kneebone E. Two steps back: City and suburban poverty trends. Washington: Brookings Institute; 2006. pp. 1999–2005. [Google Scholar]
- Bobo L, Massagli M. Stereotypes and urban inequality. In: O'Connor A, Tilly C, Bobo L, editors. Urban inequality: Evidence from four cities. New York: Russell Sage Foundation; 2001. pp. 89–162. [Google Scholar]
- Burholt V. The settlement patterns and residential histories of older Gujaratis, Punjabis and Sylhetis in Birmingham, England. Ageing and Society. 2004;24:383–409. [Google Scholar]
- Chan KS, Gaskin DJ, Dinwiddie GY, McCleary R. Do diabetic patients living in racially segregated neighborhoods experience different access and quality of care? Medical Care. 2012;50(8):692–699. doi: 10.1097/MLR.0b013e318254a43c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles C. The dynamics of racial residential segregation. Annual Review of Sociology. 2003;29:167–207. [Google Scholar]
- Chow J, Jaffe K, Snowden L. Racial/ethnic disparities in the use of mental health services in poverty areas. American Journal of Public Health. 2003;93:792–797. doi: 10.2105/ajph.93.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christopher A. Segregation levels in the late-apartheid city 1985–1991. Tijdschrift Voor Econonische en Sociale Geografie. 1993;82:15–24. doi: 10.1111/j.1467-9663.1994.tb00670.x. [DOI] [PubMed] [Google Scholar]
- Cook BL. Measuring trends in mental health care disparities 2000–2004. Psychiatric Services. 2007;55:1533–1540. doi: 10.1176/ps.2007.58.12.1533. [DOI] [PubMed] [Google Scholar]
- Cutler D, Glaeser E. Are Ghettos good or bad? Quarterly Journal of Economics. 1997;112:827–872. [Google Scholar]
- Darden J, Bagaka J. Residential segregation and the concentration of lowand high-income households in the 45 largest U.S. metropolitan areas. Journal of Developed Societies. 1997;13:171–194. [PubMed] [Google Scholar]
- Denton N. Are African Americans still hyper segregated? In: Bullard RD, Grigsby JE, Lee C, Feagin JR, editors. Residential apartheid: The American legacy. Los Angeles: CAAS Publications; 1994. pp. 49–81. [Google Scholar]
- Dinwiddie G. The health advantages of educational attainment. In: Peterson P, Baker E, McGraw B, editors. International encyclopedia of education. Oxford: Elsevier; 2010. pp. 667–672. [Google Scholar]
- Dupree L, Watson M, Schneider M. Preferences for mental health care: a comparison of older African Americans and older Caucasians. Journal of Applied Gerontology. 2005;24:196–210. [Google Scholar]
- Elo IT, Preston SH. Educational differentials in mortality: United States, 1979–85. Social Science & Medicine. 1996;42(1):47–57. doi: 10.1016/0277-9536(95)00062-3. [DOI] [PubMed] [Google Scholar]
- Eschbach K, Ostir G, Patel K, Markides K, Goodwin J. Neighborhood context and mortality among older Mexican Americans: is there a barrio advantage? American Journal of Public Health. 2004;94(10):1807–1812. doi: 10.2105/ajph.94.10.1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagg J, Curtis S, Stansfeld S, Congdon P. Psychological distress among adolescents and its relationship to individual, family and area characteristics in east London. Social Science & Medicine. 2006;63:636–648. doi: 10.1016/j.socscimed.2006.02.012. [DOI] [PubMed] [Google Scholar]
- Fang J, Madhavan S, Bosworth W, Alderman M. Residential segregation and mortality in New York city. Social Science & Medicine. 1998;47:469–476. doi: 10.1016/s0277-9536(98)00128-2. [DOI] [PubMed] [Google Scholar]
- Fortney J, Rost K, Zhang M, Warren J. The impact of geographic accessibility on the intensity and quality of depression treatment. Medical Care. 1999;37:884–893. doi: 10.1097/00005650-199909000-00005. [DOI] [PubMed] [Google Scholar]
- Gaskin DJ, Arbelaez JJ, Brown J, Petras H, Wagner F, Cooper LA. Examining racial and ethnic disparities in site of usual source of care. Journal of the National Medical Association. 2007;99:22–30. [PMC free article] [PubMed] [Google Scholar]
- Gaskin D, Dinwiddie G, Chan K, McCleary R. Residential segregation and disparities in health care services utilization. Medical Care Research and Review. 2012;69(2):158–175. doi: 10.1177/1077558711420263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene J, Blustein J, Weitzman B. Race, segregation and physicians participation in Medicaid. Milbank Quarterly. 2006;84:239–272. doi: 10.1111/j.1468-0009.2006.00447.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hargraves L, Hadley J. The contributions of insurance coverage and community resources in reducing racial/ethnic disparities in access to care. Health Services Research. 2003;38:809–829. doi: 10.1111/1475-6773.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschfield R, Keller MB, Panico S. The national depressive and manic-depressive association consensus statement on the under treatment of depression. Journal of the American Medical Association. 1997;277:333–340. [PubMed] [Google Scholar]
- Jackson S, Anderson R, Johnson N, Sorlie PD. The relation of residential segregation to all-cause mortality: a study in black and white. American Journal of Public Health. 2000;90:615–617. doi: 10.2105/ajph.90.4.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston R, Poulsen M, Forrest J. The geography of ethnic residential segregation: a comparative study of five countries. Annals of the Association of American Geographers. 2007;97(4):713–738. [Google Scholar]
- Kahn KL, Pearson ML, Harrison ER, Desmond KA, Rogers WH, Rubenstein LV, et al. Health care for Black and poor hospitalized medicare patients. Journal of the American Medical Association. 1994;271(15):1169–1174. [PubMed] [Google Scholar]
- Kessler R, Andrews G, Colpe L, Hiripi E, Mroczek D, Normand S, et al. Short screening scales to monitor population prevalence's and trends in nonspecific psychological distress. Psychological Medicine. 2002;32:959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Bruce ML, Koch JR, Laska EM, Laska EM, et al. The prevalence and correlates of untreated serious mental illness. Health Services Research. 2001;36(6 pt 1):987–1007. [PMC free article] [PubMed] [Google Scholar]
- LeClere FB, Rogers RG, Peters KD. Ethnicity and mortality in the United States: individual and community correlates. Social Forces. 1997;76:169–198. [Google Scholar]
- Lee M. Neighborhood residential segregation and mental health: a multilevel analysis on Hispanic Americans in Chicago. Social Science & Medicine. 2009;68:1975–1984. doi: 10.1016/j.socscimed.2009.02.040. [DOI] [PubMed] [Google Scholar]
- Lee M, Ferraro KF. Neighborhood residential segregation and physical health among Hispanic Americans: good, bad or benign? Journal of Health and Social Behavior. 2007;48:131–148. doi: 10.1177/002214650704800203. [DOI] [PubMed] [Google Scholar]
- Lee BA, Spain D, Umberson DJ. Neighborhood revitalization and racial change: the case of Washington, D.C. Demography. 1985;22:581–602. [PubMed] [Google Scholar]
- Lillie-Blanton M, Hoffman C. The role of health insurance coverage in reducing racial/ethnic disparities in health care. Health Affairs. 2005;24:398–408. doi: 10.1377/hlthaff.24.2.398. [DOI] [PubMed] [Google Scholar]
- Lillie-Blanton M, Martinez RM, Salganicoff A. Site of medical care: do racial and ethnic differences persist? Yale Journal of Health Policy, Law and Ethics. 2001;1:15–32. [PubMed] [Google Scholar]
- Link B, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995;35:80–94. [PubMed] [Google Scholar]
- Logan JR, Alba R, Leung SY. Minority access to white suburbs: a multiregional comparison. Social Forces. 1996;74:851–881. [Google Scholar]
- Massey DS. Ethnic residential segregation: a theoretical synthesis and empirical review. Sociology and Social Research. 1985;69:315–350. [Google Scholar]
- Massey D, Denton N. The dimensions of residential segregation. Social Forces. 1988;67:281–315. [Google Scholar]
- Massey D, Denton N. American apartheid: Segregation and the making of the underclass. Cambridge, MA: Harvard University Press; 1993. [Google Scholar]
- Miranda J, McGuire TG, Williams DR, Wang P. Mental health in the context of health disparities. American Journal of Psychiatry. 2008;165(9):1102–1107. doi: 10.1176/appi.ajp.2008.08030333. [DOI] [PubMed] [Google Scholar]
- Morales L, Lara M, Kington R, Valdez R, Escarce J. Socioeconomic, cultural and behavioral factors affecting Hispanic health outcomes. Journal of Health Care for the Poor and Underserved. 2002;1:477–503. doi: 10.1177/104920802237532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morenoff JD, Sampson R. Violent crime and the spatial dynamics of neighborhood transition: Chicago 1970–1990. Social Forces. 1997;76:31–64. [Google Scholar]
- Myer L, Ehrlich R, Susser E. Social epidemiology in South Africa. Epidemiologic Reviews. 2004;26:112–123. doi: 10.1093/epirev/mxh004. [DOI] [PubMed] [Google Scholar]
- Osypuk T, Acevedo-Garcia D. Beyond individual neighborhoods: a geography of opportunity perspective for understanding racial/ethnic health disparities. Health & Place. 2010;16:1113–1123. doi: 10.1016/j.healthplace.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pingitore D, Snowden L, Sansone R, Klinkman M. Persons with depressive symptoms and the treatments they receive: a comparison of primary care physicians and psychiatrists. International Journal of Psychiatry in Medicine. 2001;31:41–60. doi: 10.2190/6BUL-MWTQ-0M18-30GL. [DOI] [PubMed] [Google Scholar]
- Portes A. Social capital: its origins and applications in modern sociology. Annual Review of Sociology. 1998;24:1–24. [Google Scholar]
- Reschovsky J, O'Malley A. Do primary care physicians treating minority patients report problems delivering high-quality care? Health Affairs. 2007;26(3):w222–w231. doi: 10.1377/hlthaff.27.3.w222. [DOI] [PubMed] [Google Scholar]
- Ronzio C, Guagliardo M, Persaud N. Disparity in location of urban mental service providers. American Journal of Orthopsychiatry. 2006;76:37–43. doi: 10.1037/0002-9432.76.1.37. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Morenoff JD, Earls F. Beyond social capital: spatial dynamics of collective efficacy for children. American Sociological Review. 1999;64:633–660. [Google Scholar]
- SAS. User's guide, version 9.2. Cary, NC: SAS Institute Inc; 2009. [Google Scholar]
- Schnittker J, Freeze J, Powell B. Nature, nurture, neither, nor: black/White differences in beliefs about the causes and appropriate treatment of mental illness. Social Forces. 2000;78:1101–1132. [Google Scholar]
- Shannon G, Bashshur R, Lovett J. Distance and the use of mental health services. Milbank Quarterly. 1986;64:302–330. [PubMed] [Google Scholar]
- Shihadeh ES, Flynn N. Segregation and crime: the effect of black social isolation on the rates of black urban violence. Social Forces. 1996;74:1325–1352. [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. Unequal treatment: Confronting racial and ethnic disparities in healthcare. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- Snowden L, Thomas K. Medicaid and African American outpatient mental health treatment. Mental Health Services Research. 2000;2:115–120. doi: 10.1023/a:1010161222515. [DOI] [PubMed] [Google Scholar]
- South S, Crowder K, Chavez E. Migration and spatial assimilation among U.S. Latinos: classic versus segmented trajectories. Demography. 2005;42:497–521. doi: 10.1353/dem.2005.0025. [DOI] [PubMed] [Google Scholar]
- Strakowski S, McElroy S, Keck P, West S. Racial influence on diagnosis in psychotic mania. Journal of Affective Disorders. 1996;39:157–162. doi: 10.1016/0165-0327(96)00028-6. [DOI] [PubMed] [Google Scholar]
- Timberlake J, Howell A, Straight A. Trends in thesuburbanization of racial/ethnic groups in U.S. metropolitan areas, 1970 to 2000. Urban Affairs Review. 2011;47:218–255. [Google Scholar]
- U.S. Departmentof Health and Human Services. Mental health: Culture, race and ethnicity – A supplement to “mental health: A report of the surgeon general”. Washington, DC: U.S. Department of Health and Human Services; 2001. [PubMed] [Google Scholar]
- Wallace R, Huang YS, Gould P, Wallace D. The hierarchical diffusion of AIDS and violent crime among U.S. metropolitan regions: inner-city decay, stochastic resonance and reversal of the mortality transition. Social Science & Medicine. 1997;44:935–947. doi: 10.1016/s0277-9536(96)00197-9. [DOI] [PubMed] [Google Scholar]
- Weinick RM, Zuvekas SH, Cohen JW. Racial and ethnic differences in access to and use of health care services. Medical Care Research and Review. 2000;57(Suppl. 1):36–54. doi: 10.1177/1077558700057001S03. [DOI] [PubMed] [Google Scholar]
- Williams D, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Reports. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson W. The underclass: issues, perspectives and public policy. In: Wilson WJ, editor. The Ghetto underclass. California: Sage Publications; 1993. pp. 1–24. [Google Scholar]
- Young AS, Klap R, Sherbourne CD, Wells KB. The quality of care for depressive and anxiety disorders in the United States. Archives of General Psychiatry. 2001;58:655–675. doi: 10.1001/archpsyc.58.1.55. [DOI] [PubMed] [Google Scholar]
- Zubrinsky C, Bobo L. Prismatic metropolis: race and residential segregation in the city of angels. Social Science Research. 1996;25:335–374. doi: 10.1006/ssre.1996.0016. [DOI] [PubMed] [Google Scholar]


